Abstract
Background
Access to neurology consultation is limited by high demand and urgency of the presentation. Champlain BASETM (Building Access to Specialists through eConsultation) (eConsult service) aims to increase access through direct communication between primary care providers (PCPs) and specialists. Rapid responses to PCP questions can guide management and sometimes relieve the need for a formal consultation. We reviewed which topics were frequently addressed, the types of questions asked, and the effect on primary care for the patient.
Methods
This is a retrospective review of 387 consecutive questions submitted to the Champlain BASETM service between May 2011 and January 2015 and the data generated from routine use and PCP exit surveys. Questions were categorized by topic and type and analyzed quantitatively. This included time required to answer each question and effect on plans for traditional referral and clinical course of action.
Results
The top 5 topics were headache (17%), incidental imaging findings (11%), numbness/tingling (11%), seizure (9%), and cerebrovascular disease (CVD) (9%). Fifty-one percent were related to diagnosis (choice of test, imaging interpretation, symptom interpretation), 23% to drug treatment (choice, adverse effects, prescribing instructions), and 17% to management (general, need for referral). Eighty-eight percent of questions took less than 10 minutes of specialist time to answer, and 80% were answered within 1 day. eConsults decreased face-to-face referrals by 50%. In 54% of cases, the PCP received information for a new course of action.
Conclusions
We found that an eConsult service provides timely access to neurologists and can divert half of intended face-to-face consultations. The most common questions posed by PCPs regarded diagnosis and drug therapy for headaches, seizures, altered sensation, and CVD. eConsult services could provide guidance for continuing medical education planning in neurology.
The median wait time for patients in Ontario to see a neurologist is 96 days1 and is expected to worsen given the aging demographic. Delays in diagnosis and treatment of neurologic conditions can worsen patient care and quality of life.
The Champlain BASETM (Building Access to Specialists through eConsultation) service was developed to increase access and direct communication between primary care providers (PCPs) and specialists.1 Using this service, PCPs can ask a neurologist a patient-specific question, determine whether the patient would benefit from neurologic assessment, and receive immediate advice on issues that do not require formal consultation. Advice can also be provided in cases that still need formal consultation, including initial workup. Specialists are paid a prorated hourly rate based on their self-reported time taken to answer the eConsult.
Since this service has been running (2011), several analyses of its use have been published.2-5 In the initial review of 406 eConsults, neurology eConsults made up 11% of the total eConsults across all specialties, and neurology was among the top 3 specialties in which eConsult resulted in a new or additional course of action by PCPs (57% of cases).2 The clinical content of these questions has never been described, and there is only one existing report of such a service used for neurology eConsults.6
This retrospective review describes the topics and questions prompting eConsult request by PCPs, and resulting effect on the need for formal referrals to neurology. Secondarily, we looked at the value of this service to patients and PCPs, the time requirements of neurologists, and ultimate effect on the PCPs’ course of action.
Methods
Our study took place in the Champlain region of Eastern Ontario, which has a population of 1.2 million.
Standard protocol approvals, registrations, and patient consents
This study was approved by the Ottawa Health Science Network Research Ethics Board. As this was a chart review of submitted eConsults, individual patient consent was not required. Providers participating in the eConsult service sign a consent.
eConsults were submitted via a web-based tool that allows PCPs to upload imaging reports and investigations along with their question. eConsults were then assigned to specialists, preferentially based on their subspecialty. A secure database was used to store all eConsult questions as well as the replies, which were completed by 1 of 3 independent staff neurologists. Neurologists participating had subspecialties in headache, neuromuscular disease, and multiple sclerosis. When eConsults could not be answered based on the information provided, there was an opportunity to ask for further information. If the neurologist believed he or she could not answer the question safely without a formal consultation, he or she had an opportunity to request one. In some cases, a formal consultation has already been requested, and the eConsult is asking about tests that should be ordered while waiting. After completion of the eConsult, the neurologist entered the amount of time spent on each case. PCPs received the response and filled out a mandatory survey consisting of 5 questions on the outcome of the consult, the ultimate decision on formal referral, the value of the eConsult service to themselves and the patient, and any additional feedback. The PCP can refer the patient for formal consultation at any point regardless of the neurologist's recommendations. No contact between the patient and specialist occurred during the eConsult process.
We reviewed all 387 consecutive eConsults submitted to the Champlain BASETM service between May 2011 and January 2015. The questions were de-identified and uploaded to a secure private server. They were then individually reviewed and categorized based on topic and question type. Descriptive statistics were the only statistics compiled. To ensure agreement on the categorization of consults, this initial subset of 30 questions was analyzed by 2 authors (A.C.B. and L.S.). Disagreements in the first 20 cases analyzed were discussed further with a third reviewer (L.A.) until agreement was reached. The last 10 consults reviewed had no disagreements. The remainder were completed by 1 reviewer (A.B.). Question types are outlined in table 1. Importantly, questions were categorized based on the information provided by the PCP in the question rather than based on the recommendation/diagnosis contained in the neurologists' response.
Table 1.
Neurology eConsult question categories
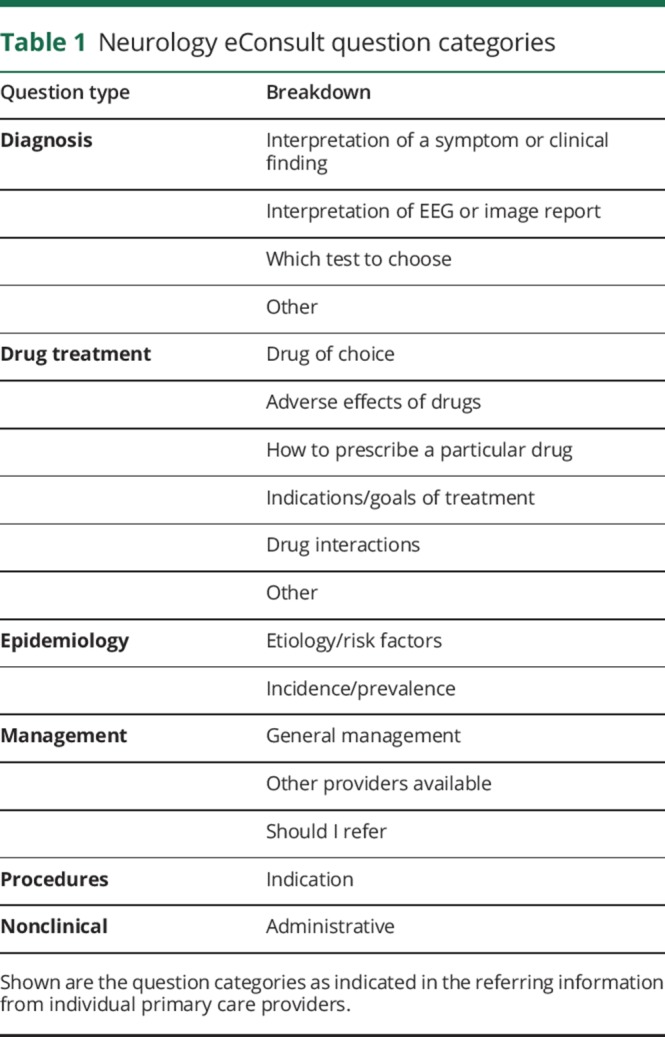
In some cases there were 2 question types and these were coded accordingly. If more than 2 questions were asked, the eConsult was deemed too complex to categorize. If no specific question was asked, this was also noted. The distribution of these questions was then analyzed quantitatively.
Data availability
Anonymized data not published within this article will be made available by request from any qualified investigator if approved by our Research Ethics Board.
Results
There were 387 eConsults directed to neurology during the study period, which represented 6.9% of the total number of eConsults submitted (n = 5,597). All were included in the analysis. These came from physicians in 92% of cases and nurse practitioners in 8% of cases.
Mean age of patients was 50 years. Sixty-seven percent of patients were women.
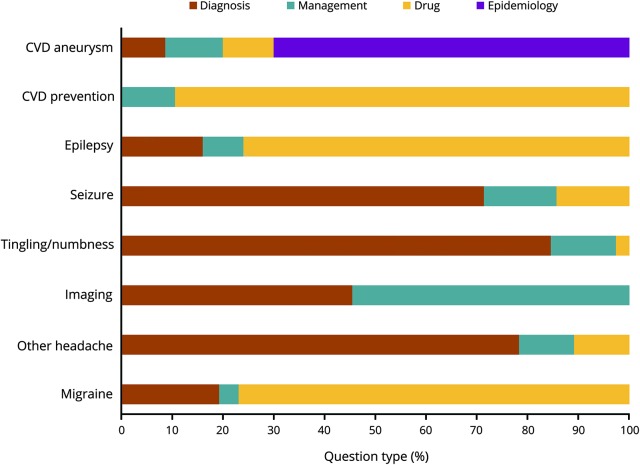
The topics most commonly addressed are listed in table 2. The top 5 topics addressed were headache, imaging findings, tingling/numbness, seizure, and cerebrovascular disease, which together made up 57% of eConsults. Analysis of the distribution of primary question type showed that 51% were related to diagnosis, 23% to drug treatment, and 17% to management.
Table 2.
Neurology content topics encountered
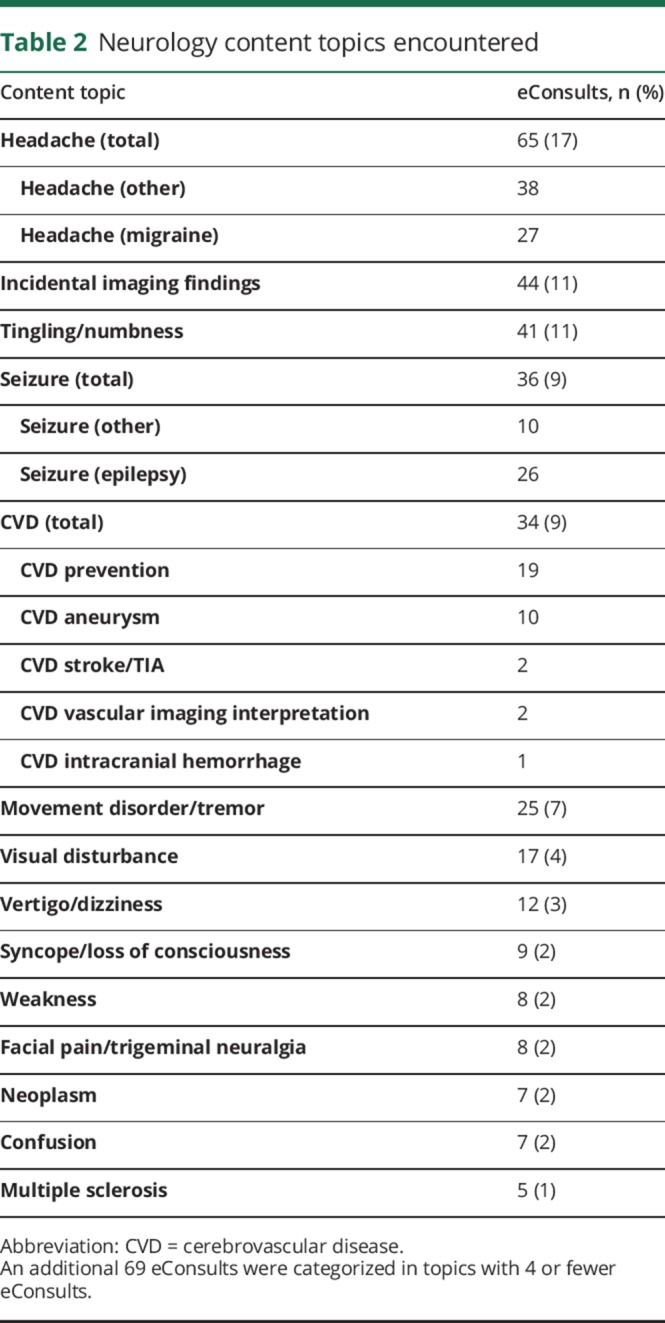
Figure 1 shows the breakdown of question type by topic for the top 5 topics.
Figure 1. Breakdown of question type by topic for the top 5 topics.
CVD = cerebrovascular disease.
From the total database, when complex questions were analyzed separately, 142/387 eConsults contained 2 questions but only 4 were too complex to categorize.
Of 387 eConsults, 34% still required a face to face consultation, but in another 34% a face to face consultation was avoided. This represents a 50% reduction in intended consultation. In 3% of cases, the neurologist requested a consult when one was not originally intended. This breakdown is shown in figure 2.
Figure 2. Breakdown of consultation results after eConsult.
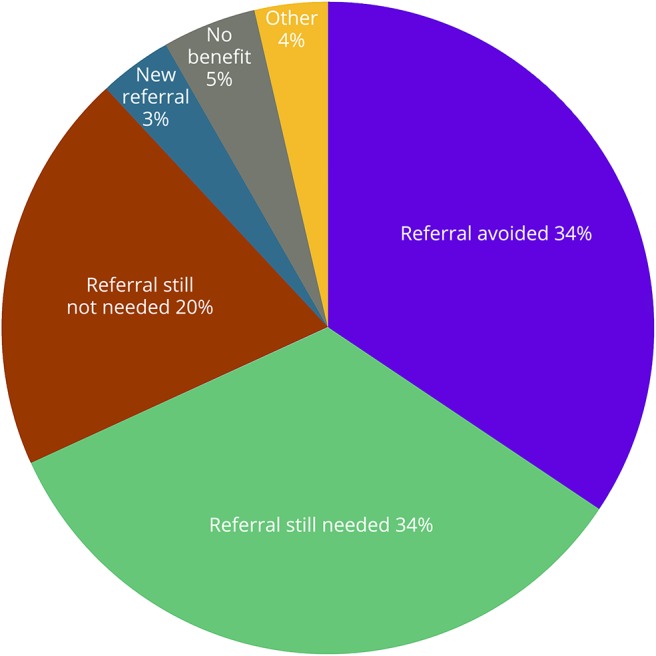
In 54% of the total cases, the PCP received information for a new course of action, and in 38% the intended course of action was confirmed. PCPs who were planning to send a formal referral received suggestions for a new course of action in 58% of cases, while those not intending to send formal referrals received this in 53% of cases. The highest rate of new additional course of action occurred in eConsults that generated a formal consult where it had not been intended (92%), followed by those eConsults where a formal consult was no longer needed (62%).
Only 6% of responses were deemed to be not useful by the PCP. When asked to rate the value of the eConsult service for the patient, 87% rated it as excellent or very good. When asked to rate the value of the eConsult service to the PCP, 89% thought it was excellent or very good.
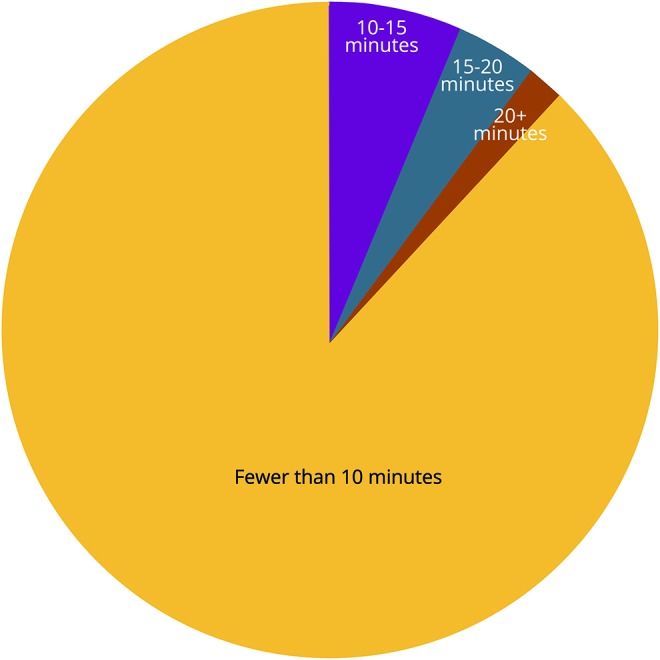
The median time it took for PCPs to receive their response from the neurologist was under 1 day, with 96% receiving them within 7 days (the expectation). The neurologists indicated they required less than 10 minutes to answer 87% of the eConsults. Further breakdown of specialist time required is shown in figure 3.
Figure 3. Breakdown of specialist time required.
Discussion
This analysis shows that the eConsult service was successful in facilitating direct contact between PCPs and specialists, which allowed for rapid advice and guidance for the PCPs. The majority of the time, a response deemed helpful was received within 24 hours of consultation. Often there was new information received that altered the PCPs’ plans for the patient (for example, initiation of a diagnostic workup or initial treatment while the patient waits for face to face consult). Overall, the neurologists spent 10 minutes or less on each case. We postulate that by reducing the intended referrals by 50%, more rapid access may also be available to those patients who required formal consultation, though this was not studied.
The most frequently addressed topics were headache, imaging findings, numbness/tingling, seizure, and cerebrovascular disease, which reflects in large part the most common neurologic presentations to primary care. We were surprised to find that interpretation of incidental imaging findings was among the most frequent topics addressed. This may reflect difficulty on the PCPs’ part with recognizing which findings require further action, or alternatively unclear imaging reporting. Consults about diagnosed chronic neurologic conditions more often asked about alternative management options.
Based on our findings, future CME events could focus on diagnostic guidelines/interpretation of tests and considerations for headache and tingling/numbness presentations, and on drug treatment guidelines for migraine, seizure, and cerebrovascular disease.
There is currently only one other report on the use of eConsults in neurology, published in Ireland in 2012.6 Those authors reviewed 662 eConsults and describe a response time of 19 hours on average for response, with a consult deferral rate of 19%. We found a higher rate of deferred consults (50%) in our review. Their top 5 topics were “unknown,” epilepsy, migraine, multiple sclerosis, and paresthesias. Another publication from 2016 reviewed the questions asked of neurologists who were collocated within a primary care medical home through electronic consult, “hallway consult,” or face to face consult.7 In this review, only 19% of consultations were electronic. Similar to our findings, their top 5 topics were headache, seizure, cerebrovascular disease, movement disorders, and radiculopathy. This article also analyzed the resources used by patients involved in these consults, and found a reduction in both imaging and neurophysiologic tests. There was a reduction in formal consultations to neurology as well. Of the 68 eConsults, only 11 were converted to formal consultation. Taken together, these 2 articles seem to support our findings that eConsults can help deliver appropriate and timely care for those patients requiring it, and may in some cases relieve the need for formal consultation. Another study showed that 80%–91% of patients prefer the idea of having an early neurology opinion through their PCP, potentially negating the need for a consult, rather than waiting longer for a guaranteed neurology visit.8
We recognize several limitations of this system. There is inherent uncertainty and risk associated with providing advice about a patient one did not assess oneself. There are likely different levels of risk tolerance among specialists using the eConsults system, which can affect the generalizability of our results. Of note, however, the duty of care for performing an eConsult is no different than performing a telephone or hallway consult and is clearly documented, which provides protection.9 We were also unable to follow up on outcomes after deferred consults, as this information was not collected in the initial database. Also, we are not able to track how many patients ultimately did end up having formal referrals or how many patients attended these appointments. A previous survey of 222 patients whose formal neurology consultation request was answered without patient contact found that there was only an 11% re-referral rate over a 6-month period, and 1.3% delayed diagnosis rate.10
Further research could be helpful to address whether referral wait time has changed over the time period since eConsults have been introduced, whether initially deferred consults remain deferred, and whether targeted PCP medical education talks on the identified topics influence the volume of referrals.
eConsults are a helpful medium for providing rapid access to neurologists for PCPs, and advice and guidance for management of their patients. The process requires much less specialist time than formal consultation and was rated positively by PCPs. With increased use, it has the potential to increase access to neurologists, by improving triage of those patients who do not require formal consultation. In this way, all 3 parties benefit from the use of this service.
Acknowledgment
The authors thank Lesley Ananny for assisting with the coordination of statistical analysis.
Footnotes
Editorial Page 177
Podcast: NPub.org/NCP/podcast8-3a
Author contributions
A.C. Bradi performed data collection and interpretation of data and is the primary author. L. Sitwell performed data collection, edited the manuscript, and provided study supervision. C. Liddy co-developed the Champlain BASE eConsult service, contributed to study concept and design, and critically reviewed this manuscript. A. Afkham edited the manuscript. E. Keely contributed to study concept and design, manuscript editing, and study supervision.
Study funding
Study funded by the Department of Medicine, University of Ottawa, and The Royal College of Physicians and Surgeons of Canada.
Disclosure
A.C. Bradi and L. Sitwell report no disclosures. C. Liddy serves as a consultant for Ministry of Health and Long Term Care of Ontario. A. Afkham reports no disclosures. E. Keely serves as an Associate Editor of Obstetric Medicine and receives research support from CIHR (Partnerships for Health System Improvement), Stemmler Medical Education Research Fund, and National Board of Medical Examiners Physicians' Services Incorporated Foundation. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Liddy C, Nawar N, Moroz I, et al. Understanding patient referral wait times for specialty care in Ontario: a retrospective chart audit. Healthc Policy 2017;13:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keely E, Liddy C, Afkham A. Utilization, benefits and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health 2013;19:733–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tran C, Liddy C, Pinto N, Keely E. Impact of question content on e-consultation outcomes. Telemed J E Health 2016;22:216–222. [DOI] [PubMed] [Google Scholar]
- 4.Liddy C, Drosinis P, Fogel A, Keely E. Prevention of delayed referrals through the Champlain BASE eConsult service. Can Fam Physician 2017;63:e381–e386. [PMC free article] [PubMed] [Google Scholar]
- 5.Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Med 2013;7:e1. [PMC free article] [PubMed] [Google Scholar]
- 6.Williams L, O'Riordan S, McGuigan C, Hutchinson M, Tubridy N. A web-based electronic neurology referral system: a solution for an overburdened healthcare system? Irish Med J 2012;105:301–303. [PubMed] [Google Scholar]
- 7.Young NP, Elrashidi MY, Crane SJ, Ebbert JO. Pilot of integrated colocated neurology in a primary care medical home. J Eval Clin Pract 2016;23:548–553. [DOI] [PubMed] [Google Scholar]
- 8.Patterson V, Donaghy C. Email triage for new neurological outpatient referrals: what the customers think. J Neurol Neurosurg Psychiatry 2006;77:1295–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CMPA, Duty of care, in: is that eConsultation or eReferral service right for your medical practice? Available at: cmpa-acpm.ca/en/advice-publications/browse-articles/2017/is-that-econsultation-or-ereferral-service-right-for-your-medical-practice. Accessed December 3, 2017.
- 10.Cariga P, Huang WH, Ranata A. Safety and efficiency of non-contact first specialist assessment in neurology. N Z Med J 2011;124:48–52. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator if approved by our Research Ethics Board.