Abstract
Background:
In the current meta-analysis, we aim to assess the effect of high-sensitive C-reactive protein (hs-CRP) on in-stent restenosis (ISR) outcome in patients receiving stent implantation.
Methods:
Embase, PubMed, and Cochrane databases were searched through October 2016 using the keywords “high-sensitive C-reactive protein,” “in-stent restenosis.” An odds ratio (OR) of on ISR endpoints among patients receiving stent implantation was calculated using random-effects models.
Results:
In the meta-analysis of 6 prospective observational studies, there are 1156 coronary heart disease (CHD) patients, a total of 885 stents were implanted and 194 ISR events had been followed up for 6 to 12 months; high-sensitive C-reactive protein levels are associated with the prediction of in-stent restenosis among patients receiving stent implantation. The OR of hs-CRP for ISR was 1.16 [95% confidence interval (CI), 1.01–1.30, P < .05].
Conclusions:
This meta-analysis shows that higher levels of hs-CRP are associated with an increased risk of ISR and indicate a poorer prognosis in CHD patients after stent implantation.
Keywords: coronary heart disease, high-sensitive C-reactive protein, in-stent restenosis, prognosis
1. Introduction
The treatment methods and techniques of coronary heart disease (CHD) were improved in recent decades due to its high morbidity and incidence. One of the most important treatment methods is peripheral percutaneous interventions (PPI), which can reduce the occurrence of death, heart failure (HF), malignant arrhythmias, and other severe complications. However, this new technique has some side effects. In-stent restenosis (ISR) is still a serious complication, especially, associated with stent insertion in percutaneous coronary intervention (PCI),[1,2] despite the great improvement of interventional technology and interventional materials these years. Some studies indicated that ISR had reduced from 40% to 50% in the era of percutaneous transluminal coronary angioplasty (PTCA) to 20% to 40% in the era of bare-metal stent (BMS). Although the advent of drug-eluting stents (DES) had greatly reduced the incidence of ISR, the incidence rate was still 5% to 10%.[3] It is found that antiplatelet agents such as aspirin and clopidogrel can significantly reduce the incidence of early thrombosis after interventional therapy, but there is no significant role of ISR in late stage.
The specific mechanism of ISR is not clear, but it is generally believed that the formation includes 3 links that are independent and interrelated. The essence of ISR is an excessive healing response of the body to arterial injury and it is a complex biological process mediated by a series of inflammatory substances and growth factors. Studies found that there are many clinical and angiographic factors contributed to ISR among patients received stent implantation including platelet deposition, diabetes, drug therapy, thrombosis, the length of their coronary artery, the degree of artery stenosis, plasma tissue factor, and other remnants of vascular repair response.[4–6] Besides, several biomarkers of inflammation and coagulation were reported as of ISR such as high-sensitivity C-reactive protein (hs-CRP).[7] While some studies indicated that the association of hs-CRP with PCI for ISR, was still a controversial issue.[8] Therefore, we conducted this systematic review and meta-analysis to evaluate the long-term prognostic significance of hs-CRP to ISR inpatients of CHD receiving stent implantation.
2. Materials and methods
2.1. Search strategy
Two authors (LX and YC) independently searched the PubMed, Embase, and Cochrane databases to identify relevant studies published up to October 30, 2016, using the keywords “in-stent restenosis,” “high-sensitivity C-reactive protein.” A manual search of the reference of retrieved studies for additional relevant publications was also performed. Ethical approval was not necessary because this is a meta-regression analysis.
2.2. Inclusion criteria
Studies were included if they met the following criteria: used a well-defined case–control design or cohort design; clearly stated hs-CRP as a major exposure in ISR among patients of CHD receiving stent implantation; and presented odds ratios (OR) for mortality with a 95% confidence interval (CI) or reported sufficient data to calculate these parameters.
2.3. Statistical analysis
Dichotomous data were analyzed by using an OR or hazard rate (HR) with 95% CI. Heterogeneity among studies was assessed by using Cochrane Q test and I2 test. Sensitivity analysis and meta-regression analysis was performed to determine the influence of each study on the overall results by excluding studies sequentially when considerable heterogeneity was indicated by I2 > 30% or P < .05, otherwise, the fixed-effects model was used to attain the summary estimates. Funnel plots and the Egger test were adopted to evaluate the potential publication bias. Statistical analyses were performed using Stata software version 11 (StataCorp LP, College Station, TX), and a 2-sided P-value ≤.05 was considered statistically significant.
3. Results
3.1. Search results and study characteristics
The workflow of identifying eligible studies is shown in Fig. 1. There were 567 studies identified through database searches, including 153 from PubMed, 204 from Embase, and 210 from Cochrane. After reviewing titles, excluding the duplicates or irrelevant studies and reviewing abstracts, 37 full-text articles entered the detailed review. Subsequent full-text review helped to exclude 31 studies that did not report the relation between hs-CRP and ISR or indicated the prognostic significance of hs-CRP to ISR. Finally, we included 6 published studies with full text in this meta-analysis. The characteristics of each study are displayed in Table 1.[9–14] There were 1156 CHD patients, a total of 885 stents were implanted and 194 ISR events during follow up 6 to 12 months of follow-up.
Figure 1.
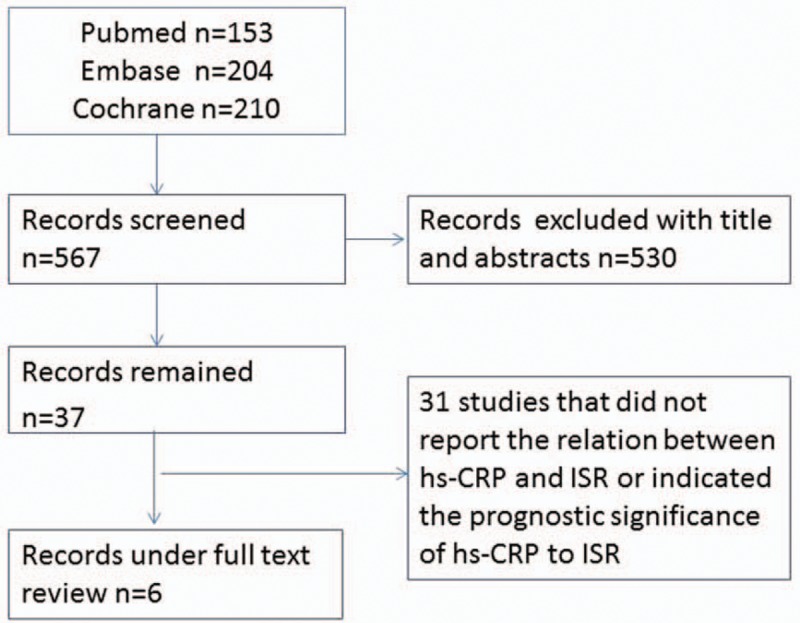
Flow diagram of eligible studies included in the meta-analysis.
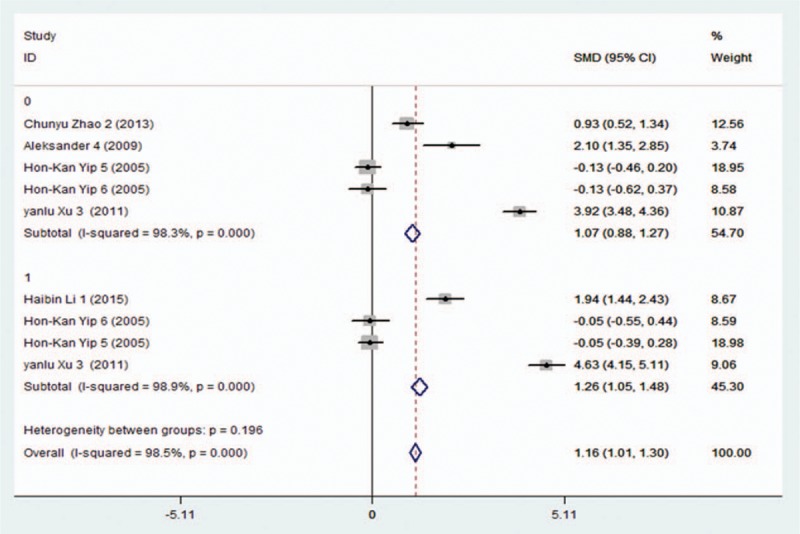
Table 1.
Baseline characteristics of included studies.
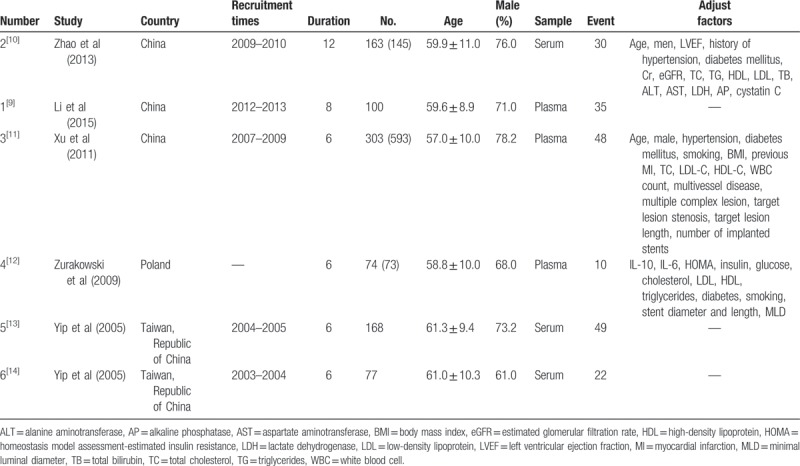
3.2. The risk of higher hs-CRP to ISR
There are 2 dates of hs-CRP in study 3, 5, and 6, which indicated on-admission and follow-up, but the level of hs-CRP only included the front in the other papers. We conducted a random-effects meta-analysis and found that the presence of the higher hs-CRP level in patients with CHD was associated with a significantly increased risk for ISR who had received stent implantation (OR: 1.16; 95% CI: 1.01–1.30). In accordance, I2 was 98.5% (P < .001) (Fig. 2), indicating considerable heterogeneity across included studies.
Figure 2.
Forest plot showing in-stent restenosis risk in patients who had received stent implantation.
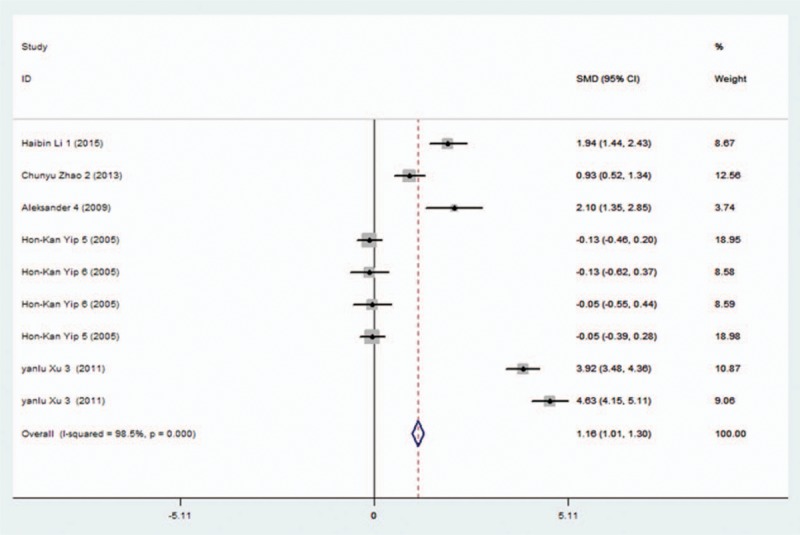
3.3. Subgroup analyses
We performed subgroup analysis subject to the hs-CRP level of on admission and follow-up. The higher hs-CRP level of follow-up (OR: 1.26; 95% CI: 1.05–1.48, P < .001) were shown to be significantly associated with increased risk for ISR events, while the results showed that there was no statistical significance on admission (OR: 1.07, 95% CI: 0.88–1.27, P < .001) (Fig. 3). Considerable heterogeneity was observed (up to 98.9%) in follow-up hs-CRP subgroups, and tests for heterogeneity between subgroups were likely to be invalid.
Figure 3.
Forest plot of subgroup analysis subject to the hs-CRP level of on admission and follow-up.
When we performed subgroup analysis subject to hs-CRP level of plasma and serum, the result showed the prognostic significance of hs-CRP in plasma (OR: 3.38, 95% CI: 3.12–3.63, P < .001) to ISR among patients after stent implantation, while in serum does not have statistical significance (OR: 0.10; 95% CI: −0.08 to 0.27, P < .001) (Fig. 4). This heterogeneity still could not be resolved by the aforementioned subgroup analysis.
Figure 4.
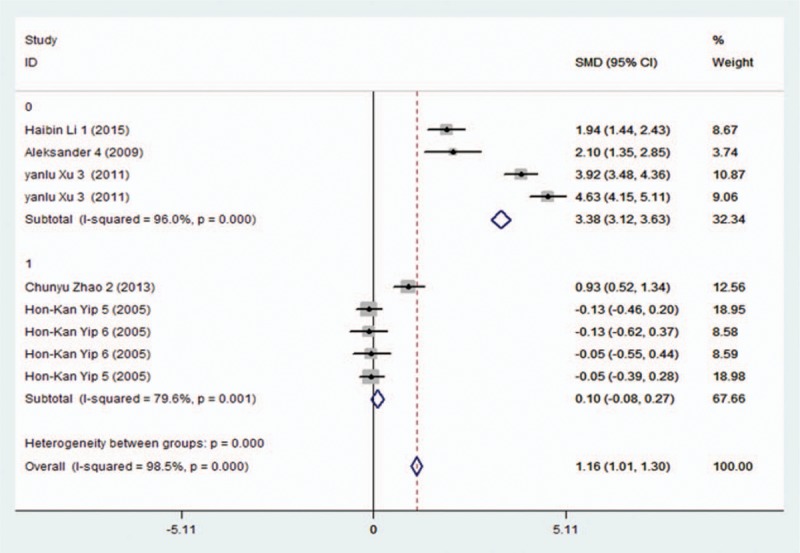
Forest plot of subgroup analysis subject to the hs-CRP level of plasma and serum.
3.4. Publication bias
A funnel plot for the 6 eligible studies showed that balanced diffusion is shown in Fig. 1, suggesting no considerable publication bias across included studies. Egger's regression was used for confirmation and yielded a similar result (z = 0.63, probability > |z| = 0.532) (Fig. 5).
Figure 5.
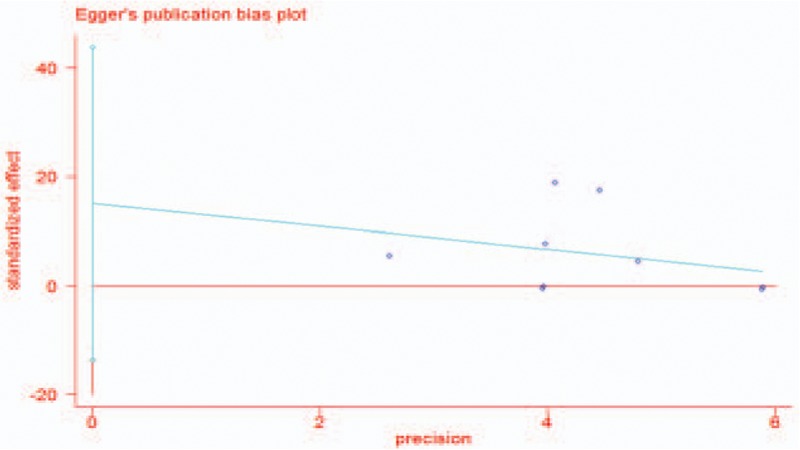
Egger's publication bias plot of the meta-analysis.
3.5. Sensitivity analysis
The results of a sensitivity analysis showed that when exclusion of study 3, the 95% CI changed to 0.66 to 1.01, when exclusion of study 5, the 95% CI changed to 1.30 to 1.62 (Fig. 6).
Figure 6.
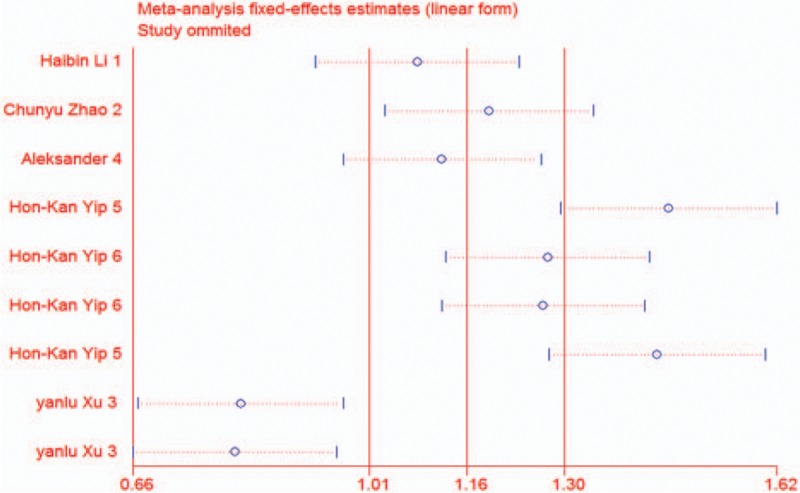
Sensitivity analysis of the meta-analysis.
3.6. Meta-regression analysis
By using the survival regression analysis of the original paper as a variable, the result of meta-regression analysis shows that the result of study 5 and 6 was due to heterogeneity. The proportion of between-study variance explained with Knapp–Hartung modification (P = .009).
4. Discussion
ISR was defined as in-stent narrowing of at least 50% or within 5 mm proximal or distal to the stent, which is more occurred in 2 months after stent implantation. The rate can be even high to 15% to 35% despite the advancement of stent, drugs, and technology of PCI, which can reduce the occurrence of restenosis to a certain extent.[9] Once ISR happened, it means the probable occurrence of angina, acute myocardial infarction (AMI), malignant arrhythmia, acute left HF, stroke, etc. All of these could lead to death without timely rescue. Hence, it is extremely urgent to find the high-risk population and predict the occurrence of ISR among people after stent implantation. As a result, mortality will be reduced and medical resources will be saved through early found and intervention.
The study[15,16] indicated that ISR was largely related to diabetes, long lesions, multivessel diseases, and bifurcation lesions. Among the biological factors, high plasma levels of hs-CRP and IL-6 had been found to predict the risk of restenosis for a long time and it was published in J Am Coll Cardiol, Am J Cardiol Heart.[17–20] On the other hand, there were some different findings reveal that hs-CRP did not predict restenosis in patients undergoing PCI with stenting despite it was significantly increased in these people.[13,14,21] Some studies even reported that ISR was observed with similar rates in patients with elevated hs-CRP levels compared to normal levels.[21] We designed this meta-analysis including 6 studies and 1156 patients and exposed the long-term prognostic significance of hs-CRP to ISR among patients receiving stent implantation.
Hs-CRP, a landmark for oxidative stress, has been used as a reference for inflammatory diseases for a long time.[22] Compared to other biomarkers such as Cys C, total cholesterol (TC), and triglyceride (TG), the hs-CRP level is higher in patients with CHD and in ISR patients although no differences in terms of medication were present after stent implantation.[10,23] Hoshida et al[24] reported that there was a persistent increase in hs-CRP associated with the risk of restenosis in patients with stable angina but not receiving statins. Gaspardone et al indicated that inflammation plays an important role in complications of PCI. It was related to arterial injury, he explained it, both after balloon dilation and after stent implantation. Apart from this, multiple inflammatory factors such as cytokines and chemokines were involved in the neointimal tissue response at the site of coronary stenting.[25] Therefore, recent reports have shown hs-CRP can be used to predict not only early stent thrombosis but also long-term ISR including 6, 8, and 12 months.[8,10,26]
Hon-Kan Yip et al[13,14] reported that circulating concentrations of hs-CRP were elevated preprocedure distinctly in patients with unstable angina and declined thereafter. Nonetheless, it was not useful in predicting late restenosis after coronary stent implantation. This study, which is associated with a different outcome, has been included in our study, leading to our study with considerable heterogeneity, despite this, hs-CRP still can be used to predict ISR in patients with CHD after stent implantation through our analysis. If we took these 2 articles out, it would be observed that the predictor value became much higher. Apart from study 5 and 6, the sensitivity analysis showed exclusion of study 3 results became lower because it had a much higher sample size of China almost half of all the studies and the recruitment times from 2007 to 2009, that is just why we cannot exclude it from the meta-analysis.
Niccoli et al[27] evaluated the association of optical coherence tomograph (OCT) characteristics of neointimal with systemic concentrations of hs-CRP which was measured when ISR occurred. They did not find significant differences between patients with high and low levels of hs-CRP according to stent type and time from stent implantation while patients with high hs-CRP levels had a higher restenosis tissue symmetry ratio compared to patients with low hs-CRP levels. The differential distribution of shear stress and its effects on neointimal tissue shape mediated by hs-CRP release can explain the association between the high levels of hs-CRP and the growth of restenotic tissue. Indeed, coronary stent implantation changes vessel geometry and, consequently, under disturbed flow and or low endothelial shear stress, increasing the risk of ISR.[28,29]
As a result, we can identify the mechanism of ISR and select appropriate treatment strategies to prevent the occurrence of ISR through measuring hs-CRP level.[27]
Some studies have demonstrated the association of hs-CRP with ISR both on admission and during follow-up in a large number of patients.[30] While Zairis et al[31] showed that hs-CRP on admission was not related to restenosis in patients with stable unstable coronary diseases at 1-year follow-up. The next year, Dibra et al[21] indicated the same opinion at 6-month follow-up in SA patients. In the subgroup analysis of our study, we also found that hs-CRP level follow-up (6–12 months) may be used to predict the occurrence of ISR after patients with CHD undergone PCI therapy while hs-CRP expression on admission or basic level cannot.
Another subgroup data analysis subject to the hs-CRP level of plasma and serum, then found the prognostic significance of hs-CRP in plasma to ISR among patients after stent implantation while in serum does not have the same outcome. It means that we should use plasma hs-CRP rather than serum hs-CRP to predict the ISR.
Among the included articles, only the 2nd, 3rd, and 4th study adjusted factors when analyzing the prognostic of hs-CRP to ISR. Zhao et al[10] indicated that only higher level of TB (total bilirubin) and TC, cystatin C, and hs-CRP have the prognostic significance. Xu et al[11] indicated that apart from hs-CRP, only diabetes and number of implanted stents had the prognostic significance. While in the number 4 study, hs-CRP, IL-10, IL-6, glucose, triglycerides, diabetes, stent length, and minimal luminal diameter (MLD) (poststent implantation) were significantly predicted the ISR.[12]
To our knowledge, this is the first meta-analysis to demonstrate the association of hs-CRP with ISR that is probably explained as an inflammatory reactor. Through further subgroup analysis, we indicated that we should measure plasma hs-CRP and not only depend on hs-CRP on admission but also remeasure its follow-up. However, the underlying mechanism remains to be elucidated, and further large-scale observational studies can help confirm the prognostic value of hs-CRP to ISR.
4.1. Limitations
There were several limitations in our study. First, our selection criteria for studies, which were restricted to those published in English, might produce language bias. Second, among the 6 included studies, there are 5 studies come from Asia and only 1 study comes from European which brings the difference in race and population. Third, high heterogeneity was observed in the analysis of the prognostic value of hs-CRP to ISR in patients after stent implanting in the long-term. Subsequent meta-regression of hs-CRP derived from serum or plasma and hs-CRP derived from on admission or follow-up failed to identify significant sources of heterogeneity. Since we use SMD as pooled effects for the continuous data as hours, the discrepancies in the acquisition of outcomes among different studies may affect the homogeneity of the results. Apart from this, we are not able to delineate the different laboratory testing methods on the current finding in our meta-analysis due to insufficient data. All of these may contribute to heterogeneity and bias among the studies and affect the quality of the meta-analysis.
5. Conclusions
In summary, our study is the first meta-analysis demonstrating that the presence of hs-CRP in patients with CHD after stent implantation is associated with an increased risk for ISR, which makes it a potential marker of prognosis in ISR both on admission and in follow up. Findings from the present study may reinforce the knowledge of practical predictive methods for ISR to reduce the risk of sudden death in patients with CHD.
Author contributions
Data curation: Li Xiang, Yuqi Chen, Jianchang Chen.
Formal analysis: Li Xiang, Yuqi Chen, Tao You.
Funding acquisition: Li Xiang, Yang Jiao.
Investigation: Li Xiang, Yuqi Chen, Xinyi Zhu, Tao You, Yang Jiao.
Methodology: Li Xiang, Yuqi Chen, Xinyi Zhu, Tao You, Yang Jiao, Weiting Xu.
Resources: Li Xiang, Yuqi Chen, Xinyi Zhu.
Writing – original draft: Li Xiang.
Writing – review & editing: Li Xiang, Yuqi Chen, Xinyi Zhu, Tao You, Jianchang Chen, Weiting Xu.
Footnotes
Abbreviations: ALT = alanine aminotransferase, AMI = acute myocardial infarction, AP = alkaline phosphatase, AST = aspartate aminotransferase, BMI = body mass index, BMS = bare-metal stent, CHD = coronary heart disease, CI = confidence interval, DES = drug-eluting stent, eGFR = estimated glomerular filtration rate, HDL = high-density lipoprotein, HF = heart failure, HOMA = homeostasis model assessment-estimated insulin resistance, HR = hazard rate, hs-CRP = high-sensitive C-reactive protein, ISR = in-stent restenosis, LDH = lactate dehydrogenase, LDL = low-density lipoprotein, LVEF = left ventricular ejection fraction, MI = myocardial infarction, MLD = minimal luminal diameter, OR = odds ratio, PCI = percutaneous coronary intervention, PPI = peripheral percutaneous interventions, PTCA = percutaneous transluminal coronary angioplasty, TB = total bilirubin, TC = total cholesterol, TG = triglyceride, WBC = white blood cell.
Funding: This work was supported in part by grants from the Suzhou Science and Technology Project Foundation of China (SYS201721 to LX).
XZ and YC contributed equally to this article.
The authors have no conflicts of interest to disclose.
References
- [1].Bennett MR. In-stent stenosis: pathology and implications for the development of drug eluting stents. Heart 2003;89:218–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lowe HC, Oesterle SN, Khachigian LM. Coronary in-stent restenosis: current status and future strategies. J Am Coll Cardiol 2002;39:183–93. [DOI] [PubMed] [Google Scholar]
- [3].Hao PP, Chen YG, Wang XL, et al. Efficacy and safety of drug eluting stents in patients with acute ST-segment-elevation myocardial infarction: a meta-analysis of randomized controlled trials. Tex Heart Inst J 2010;37:516–24. [PMC free article] [PubMed] [Google Scholar]
- [4].Toutouzas K, Colombo A, Stefanadis C. Inflammation and restenosis after percutaneous coronary interventions. Eur Heart J 2004;25:1679–87. [DOI] [PubMed] [Google Scholar]
- [5].Liu W, Liu Y, Jiang H, et al. Plasma levels of interleukin 18, interleukin 10, and matrix metalloproteinase-9 and -137G/C polymorphism of interleukin 18 are associated with incidence of in-stent restenosis after percutaneous coronary intervention. Inflammation 2013;36:1129–35. [DOI] [PubMed] [Google Scholar]
- [6].Christopoulos G, Karmpaliotis D, Alaswad K, et al. The efficacy of “hybrid” percutaneous coronary intervention in chronic total occlusions caused by in-stent restenosis: insights from a US multicenter registry. Catheter Cardiovasc Interv 2014;84:646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Blum A, Schneider DJ, Sobel BE, et al. Endothelial dysfunction and inflammation after percutaneous coronary intervention. Am J Cardiol 2004;94:1420–3. [DOI] [PubMed] [Google Scholar]
- [8].Roghani F, Mehrabi Koushki A, Nezarat N, et al. The correlation between early complications of percutaneous coronary intervention and high sensitive C-reactive protein. ARYA Atheroscler 2013;9:263–7. [PMC free article] [PubMed] [Google Scholar]
- [9].Li H, Jiang Z, Liu X, et al. Higher plasma level of STIM1, OPG are correlated with stent restenosis after PCI. Int J Clin Exp Med 2015;8:21089–97. [PMC free article] [PubMed] [Google Scholar]
- [10].Zhao C, Yang L, Mao L, et al. Cystatin C associates with the prediction of in-stent restenosis among patients receiving stent implantation: results of the 1-year follow-up. Coron Artery Dis 2013;24:357–60. [DOI] [PubMed] [Google Scholar]
- [11].Xu YL, Li JJ, Xu B, et al. Role of plasma C-reactive protein in predicting in-stent in patients with stable angina after coronary stenting. Chin Med J 2011;124:845–50. [PubMed] [Google Scholar]
- [12].Zurakowski A, Wojakowski W, Dzielski T, et al. Plasma levels of C-reactive protein and interleukin-10 predict late coronary in-stent restenosis 6 months after elective stenting. Kardiol Pol 2009;67:623–30. [PubMed] [Google Scholar]
- [13].Yip HK, Hung WC, Yang CH, et al. Serum concentrations of high-sensitivity C-reactive protein predict progressively obstructive lesions rather than late restenosis in patients with unstable angina undergoing coronary artery stenting. Circ J 2005;69:1202–7. [DOI] [PubMed] [Google Scholar]
- [14].Yip HK, Wu CJ, Yang CH, et al. Serial changes in circulating concentrations of soluble CD40 ligand and C-reactive protein in patients with unstable angina undergoing coronary stenting—role of inflammatory mediators in predicting late restenosis. Circ J 2005;69:890–5. [DOI] [PubMed] [Google Scholar]
- [15].Natarajan MK, Strauss BH, Rokoss M, et al. Randomized trial of insulin versus usual care in reducing restenosis after coronary intervention in patients with diabetes. the STent Restenosis And Metabolism (STREAM) study. Cardiovasc Revasc Med 2012;13:95–100. [DOI] [PubMed] [Google Scholar]
- [16].Takagi K, Ielasi A, Basavarajaiah S, et al. The impact of main branch restenosis on long term mortality following drug-eluting stent implantation in patients with de novo unprotected distal left main bifurcation coronary lesions: the Milan and New-Tokyo (MITO) Registry. Catheter Cardiovasc Interv 2014;84:341–8. [DOI] [PubMed] [Google Scholar]
- [17].Walter DH, Fichtlscherer S, Sellwig M, et al. Preprocedural C-reactive protein levels and cardiovascular events after coronary stent implantation. J Am Coll Cardiol 2001;37:839–46. [DOI] [PubMed] [Google Scholar]
- [18].Gaspardone A, Crea F, Versaci F, et al. Predictive value of C-reactive protein after successful coronary artery stenting in patient with stable angina. Am J Cardiol 1998;82:515–8. [DOI] [PubMed] [Google Scholar]
- [19].Dibra A, J Mehilli SB, Hadamitzky H, et al. Inflammatory response after intervention assessed by serial C-reactive protein measurements correlates with restenosis in patients treated with coronary stenting. Am Heart J 2005; 150: 344–350. [DOI] [PubMed] [Google Scholar]
- [20].Hojo Y, Ikeda U, Katsuki T, et al. Interleukin 6 expression in coronary circulation after coronary angioplasty as a risk factor for restenosis. Heart 2000;84:83–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dibra A, Mehilli J, Braun S, et al. Association between C-reactive protein levels and subsequent cardiac events among patients with stable angina treated with coronary artery stenting. Am J Med 2003;114:715–22. [DOI] [PubMed] [Google Scholar]
- [22].Mega JL, Morrow DA, De Lemos JA, et al. B-type natriuretic peptide at presentation and prognosis in patients with ST-segment elevation myocardial infarction: an ENTIRE-TIMI-23 substudy. J Am Coll Cardiol 2004;44:335–9. [DOI] [PubMed] [Google Scholar]
- [23].Lamblin N, Mouquet F, Hennache B, et al. High-sensitivity C-reactive protein: potential adjunct for risk stratification in patients with stable congestive heart failure. Eur Heart J 2005;26:2245–50. [DOI] [PubMed] [Google Scholar]
- [24].Hoshida S, Nishino M, Takeda T, et al. A persistent increase in C-reactive protein is a risk factor for restenosis in patients with stable angina who are not receiving statins. Atherosclerosis 2004;173:285–90. [DOI] [PubMed] [Google Scholar]
- [25].Gaspardone A, Crea F, Versaci F, et al. Predictive value of C-reactive protein after successful coronary-artery stenting in patients with stable angina. Am J Cardiol 1998;82:515–8. [DOI] [PubMed] [Google Scholar]
- [26].Delhaye C, Sudre A, Lemesle G, et al. Preprocedural high-sensitivity C-reactive protein predicts death or myocardial infarction but not target vessel revascularization or stent thrombosis after percutaneous coronary intervention. Cardiovasc Revasc Med 2009;10:144–50. [DOI] [PubMed] [Google Scholar]
- [27].Niccoli G, Dato I, Imaeva AE, et al. Association between inflammatory biomarkers and in-stent restenosis tissue features: an Optical Coherence Tomography Study. Eur Heart J Cardiovasc Imaging 2014;15:917–25. [DOI] [PubMed] [Google Scholar]
- [28].Chatzizisis YS, Coskun AU, Jonas M, et al. Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: molecular, cellular, and vascular behavior. J Am Coll Cardiol 2007;49:2379–93. [DOI] [PubMed] [Google Scholar]
- [29].Wentzel JJ, Krams R, Schuurbiers JC, et al. Relationship between neointimal thickness and shear stress after Wallstent implantation in human coronary arteries. Circulation 2001;103:1740–5. [DOI] [PubMed] [Google Scholar]
- [30].Versaci F, Gaspardone A. Prevention of restenosis after stenting: the emerging role of inflammation. Coron Artery Dis 2004;15:307–11. [DOI] [PubMed] [Google Scholar]
- [31].Zairis MN, Ambrose JA, Manousakis SJ, et al. The impact of plasma levels of C-reactive protein, lipoprotein (a) and homocysteine on the long-term prognosis after successful coronary stenting: the Global Evaluation of New Events and Restenosis After Stent Implantation Study. J Am Coll Cardiol 2002;40:1375–82. [DOI] [PubMed] [Google Scholar]


