Abstract
Rationale:
Obesity has become a worldwide health challenge. In elderly patients, obesity induces a decrease in skeletal muscle strength and mass, which is linked to age-related sarcopenia. These are important predictors of hospitalization and death. Herein, we report on 2 elderly male patients who were treated by pharmacopuncture with wild ginseng complex (WGC).
Patient concerns:
Case 1 was that of a 62-year-old man who was mainly concerned about his appearance as his abdominal fat was steadily increasing, without any changes to his body weight. He also had an aversion to any type of modern Western medicine. In addition, the patient was averse to changing his eating habits or exercise style. Case 2 was that of a 66-year-old man who was concerned about his appearance due to an increase in abdominal fat accumulation. Furthermore, he had gained 1.5 inches in waist circumference over the past 2 years. The patient wanted to lose fat in the abdomen, but not in other parts of the body.
Diagnoses:
In this study, we examined 2 elderly male patients (aged 60 years and above) with abdominal obesity and excessive visceral fat mass. Abdominal obesity is defined as a waist circumference of ≥ 90 cm for men and ≥ 80 cm for women.
Interventions:
The patients received pharmacopuncture with WGC 5 times over 3 weeks on their abdomen without controlling diet and exercise.
Outcome:
After 3 weeks of pharmacopuncture with WGC and at a follow-up appointment 3 weeks later, we detected an increase in muscle mass, protein content, and basal metabolic rate in both cases.
Lessons:
Although we observed only 2 cases, our results indicated that pharmacopuncture with WGC can be used as a new alternative treatment to prevent and improve abdominal obesity in elderly individuals, as well as age-related sarcopenic obesity.
Keywords: clinical study, elderly patients, Korean medicine, obesity, pharmacopuncture, wild-ginseng complex
1. Introduction
Obesity has become a worldwide health challenge as its prevalence has increased globally in recent decades. The World Health Organization (WHO) defines “obesity” as abnormal or excessive fat accumulation that may have an adverse effect on health, and it is reported that the global prevalence of obesity doubled between 1980 and 2014.[1] Obesity due to increased body fat is a major risk factor for the deterioration of health, dysfunction, and a decrease in the quality of life.[2] Besides young people, obesity in the elderly population is increasing globally, which has significant public health consequences.[3–6]
Obesity in elderly patients induces a decrease in skeletal muscle strength and mass, which is linked to age-related sarcopenia, and is one of the important predictors of hospitalization and death.[7] Obesity caused by aging is characterized by changes in body composition with increased visceral body fat that accumulates more in the abdominal area, and a reduction in skeletal muscle mass. Thus, several longitudinal studies have reported that body fat mass increases with age, and reaches a maximum at 60 to 75 years of age.[8] Furthermore, muscle mass declines more rapidly after age 60.[9] Recently, a combination of diet and exercise has been considered as the most effective method of weight loss. However, there are disadvantages such as it can be difficult to achieve the weight loss required within a short time frame, and it can be difficult to manage partial obesity. Therefore, it appears that a new paradigm is needed for the treatment of obesity.
Alternative and complementary therapeutics such as herbal medicines and acupuncture are used for obesity treatments. The acupuncture treatment method involves needling on the meridian points. Pharmacopuncture, which is one of the acupuncture methods, involves injecting pharmaceutical agents such as herbal medicines into acupuncture points or fat areas based on pharmacology and meridian theories.[10,11] In Korean medicine, it is believed that pharmacopuncture therapy is one of the top candidates for time-effective treatment of obesity in the elderly. Wild ginseng complex (WGC) is composed of Panax Quinquefolius (Ginseng Radix Alba: wild American ginseng), Bos Taurus Linné var. domesticus (Bovis Calculus, ox bezoar), Ursus arctos Linné (Fel Ursi, gall bladder of a bear), and Ondatra zibethicus (Moschus, musk). Pharmacopuncture using WGC is commonly used to treat obesity. It has been reported to have antiobesity and anti-inflammatory effects in 3T3-L1 adipocytes and RAW264.7 macrophages when a high fat diet is induced in obese mice.[12] The benefits of this treatment have also been clinically studied in young female patients with obesity, which showed that there was an improvement in the regulation of cholesterol, insulin, and leptin levels.[13–17] In most clinical studies, pharmacopuncture with WGC has shown that it has therapeutic effects in obese female patients, but the effect in the elderly is currently unknown. Therefore, in this study we evaluated the therapeutic effects of pharmacopuncture with WGC in obese elderly patients who were treated in Korean clinics.
2. Case description
We studied 2 elderly male patients (aged 60 years and above) who had abdominal obesity, with excessive visceral fat mass. Abdominal obesity is defined as a waist circumference ≥ 90 cm for men or ≥ 80 cm for women.
2.1. Case 1
Case 1 was that of a 62-year-old man (163 cm, 70.7 kg) who works with machinery and other heavy equipment. He was mainly concerned about his appearance as his abdominal fat steadily increased without there being any change to his body weight. His family history was normal. His minor complaints included chronic rhinitis, severe snore, and low back pain with spinal stenosis (L4–5). He has an aversion to any type of modern Western medicine, and has difficulties with his eating habits and exercise style. Therefore, we suggested pharmacopuncture treatment with WGC, which he agreed to.
2.2. Case 2
Case 2 was that of a 66-year-old man (173 cm, 71 kg) who is a professor. He was concerned about his appearance as his abdominal fat had increased. Furthermore, over the past 2 years his waist circumference had increased by 1.5 inches. His previous medical history included an enlarged prostate which was diagnosed 2 years ago. In addition, his family history was normal. For treatment we suggested pharmacopuncture with WGC as he didn’t want to lose fat in other parts of the body, except for the abdomen. The patient agreed to these treatment methods.
3. Intervention
The patients were not forced to strictly comply with diet and exercise therapies; instead, they were allowed to follow their regular diet and exercise. Pharmacopuncture was conducted on the subjects 5 times over 3 weeks. At baseline, upon completion of the 5 treatments, and at a follow-up appointment 3 weeks later, the subjects’ anthropometric measurements and body composition were analyzed.
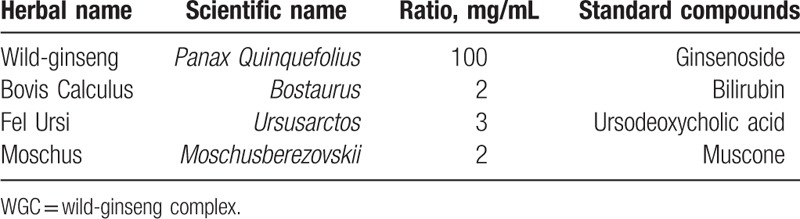
3.1. Preparation of the pharmacopuncture with WGC
WGC is composed of 4 herbs (Table 1). Wild ginseng was purchased from a herbal materials company (Woomin, Ontario, Canada). Bovis Calculus, Fel Ursi, and Moschus were purchased from another herbal materials company (WooriSY, Gyeonggido, Korea). The WGC extract was manufactured under a Good Manufacturing Practice (GMP)-compliant facility (Korea Immuno-Pharmacopuncture Association: KIPA, Seoul, Korea) in water and alcohol (v/v = 1:1). For this study, the final product of WGC extract (107 mg/mL in a sealing vial) was provided by KIPA.
Table 1.
Composition of WGC.
3.2. Treatment using pharmacopuncture with WGC
The locations of the pharmacopuncture treatment were the left and right sides of 4 points inferior to and 4 points superior to the navel points on the meridians of the stomach, the spleen, and the gall bladder. The total number of points was 20. The points were spaced about 2 cm apart, and about 0.2 mL of the pharmacopuncture therapy solution was injected into each point. A total of 4 mL WGC extract was injected into each subject at each visit. Besides the pharmacopuncture therapy on their abdomen, we also treated the patients with acupuncture, cupping, and moxibustion on other parts of the body due to other minor complaints that the patients had. After the treatment was finished, we did not give any medications.
4. Examination
The 2 subjects underwent examination before their pharmacopuncture therapy and upon completion of the 5 treatments. Anthropometric measurements and body composition analysis were carried out on the subjects. This case report is one of retrospective chart reviews and approved by the Institutional Review Board (IRB) of Gachon University Gil, Korean Medical Hospital (IRB No. 18-107). The patients signed informed consent for the publication of this case report.
4.1. Anthropometric measurements
The height was measured using a height meter (Neo GM Tech, Korea) up to 0.1 cm, after the subjects were instructed to remove their socks and stand in an upright position. The body weight (BW) was measured with a bio-impedance body mass analyzer (InBody, Seoul, Korea). The waist circumference (WC) was measured midway between the lower margin of the last rib and the top of the pelvic bone in a horizontal plane using plastic tape. The hip circumference (HC) was measured at the horizontal level of the widest part of the hip. Body mass index (BMI) is calculated by dividing weight in kilograms by height in square meters.
4.2. Body composition analysis
Each subject was asked to visit the hospital at set times, during which body fat mass (BFM), skeletal muscle mass (SMM), body fat percentage (BFP), fat free mass (FFM), bone mineral content (BMC), waist-hip ratio (WHR), protein content, mineral content, and basal metabolic rate (BMR) were measured. Measurements were made using a body mass analyzer (InBody) based on bioelectrical impedance analysis (BIA). The measurements were taken while the individuals were scantily clad. The subjects were also instructed to remove their socks and metals that they might be wearing such as glasses, necklaces, and watches.
5. Clinical outcomes
As the treatment progressed, the 2 patients felt that their body became lighter and their pants become looser around the waist. In addition, at follow-up, these changes continued.
5.1. Measurement of abdominal obesity based on WC and WHR
Regarding changes to the abdominal obesity, we analyzed WC and WHR. We also analyzed BMI so that it could be compared with WC and WHR. WC in case 1 decreased from 91 to 89 cm after 5 treatments of WGC pharmacopuncture. These changes continued until the follow-up (F/U) appointment 3 weeks after treatment. WC in case 2 decreased from 95 to 86 cm after WGC pharmacopuncture, and these changes continued until the F/U appointment 3 weeks after treatment (Fig. 1). WHR in case 1 decreased from 0.95 to 0.90 after WGC pharmacopuncture and decreased to 0.88 at the F/U appointment 3 weeks after treatment. WHR in case 2 decreased from 0.90 to 0.85 after WGC pharmacopuncture, and decreased further (0.84) at the F/U appointment 3 weeks after treatment (Fig. 2). BMI in case 1 decreased from 26.6 to 26.2 kg/m2 after WGC pharmacopuncture and these changes continued until the F/U appointment 3 weeks after treatment. BMI in case 2 decreased from 23.7 to 23.1 kg/m2 after WGC pharmacopuncture and increased to 23.2 kg/m2 at the F/U appointment 3 weeks after treatment (Fig. 3).
Figure 1.
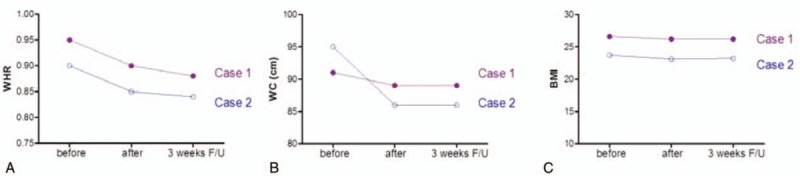
Effects of pharmacopuncture with WGC on changes to the levels of WHR (A), WC (B), and BMI (C) as markers of abdominal fat accumulation in elderly patients with obesity. The pharmacopuncture with WGC was conducted on the subjects, on their abdomen 5 times over 3 weeks. At the baseline, upon completion of the 5 treatments and at a follow-up appointment 3 weeks after these treatments began, the body composition and anthropometric measurements of the patients were analyzed. BMI = body mass index, WC = waist circumference, WHR = waist-hip ratio.
Figure 2.
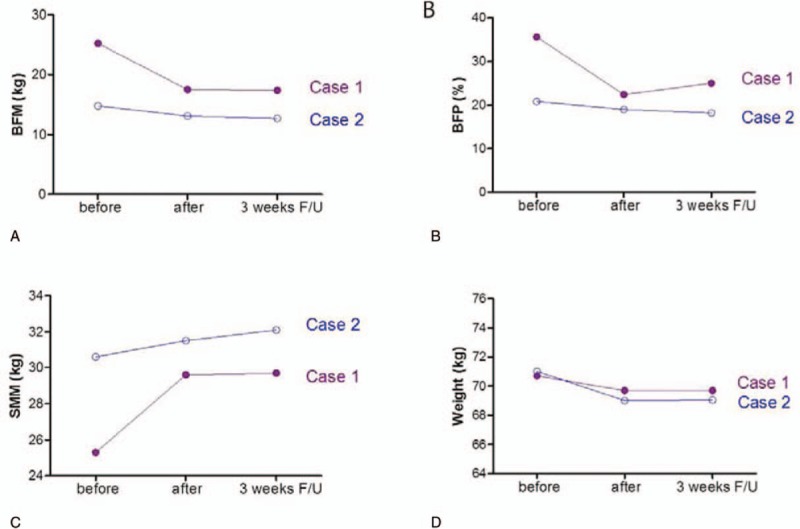
Effects of pharmacopuncture with WGC on changes to the levels of markers that indicate body composition, BFM (A), BFP (B), SMM (C) and body weight (D). Pharmacopuncture with WGC was conducted on the subjects 5 times over 3 weeks. At the baseline, upon completion of the 5 treatments and a follow-up appointment after the 5 treatments, the anthropometric measurements and body composition of the patients were analyzed. BFM = body fat mass, BFP = body fat percentage, SMM = skeletal muscle mass, WGC = wild-ginseng complex.
Figure 3.
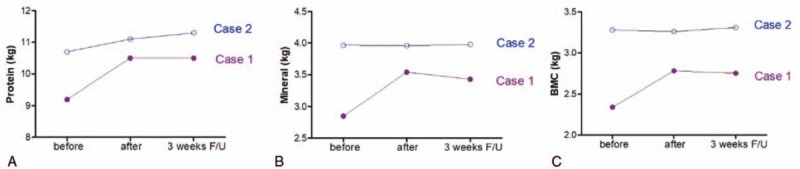
Effects of pharmacopuncture with WGC on changes to protein content (A), mineral content (B) and BMC (C) in the body. Pharmacopuncture with WGC was conducted on the subjects 5 times over 3 weeks. At the baseline, upon completion of the 5 treatments and at a follow-up appointment 3 weeks after the 5 treatments, body composition analysis of the patients was analyzed using BIA (Inbody 520). BMC = bone mineral content, WGC = wild-ginseng complex.
5.2. Analysis of the ratio of muscle and fat
To evaluate the level of obesity in detail, the ratio of muscle to fat was analyzed by comparing BFM, BFP, and SMM in each subject. In this study, BFM in case 1 decreased from 25.2 to 17.5 kg after WGC pharmacopuncture treatment. At the F/U appointment 3 weeks later, BFM decreased to 17.4 kg. BFM in case 2 decreased from 14.8 to 13.1 kg after WGC pharmacopuncture and decreased further to 12.7 kg when measured at the F/U appointment 3 weeks after treatment had finished (Fig. 2A). BFP in case 1 decreased from 35.6% to 22.4% after WGC pharmacopuncture and increased to 25.0% when measured at the F/U appointment 3 weeks after treatment. BFP in case 2 decreased from 20.8% to 19.05% after WGC pharmacopuncture and decreased to 18.2% when measured at the F/U appointment 3 weeks after treatment (Fig. 2B). SMM in case 1 increased from 25.3 to 29.6 kg after WGC pharmacopuncture and increased to 29.7 kg when measured at the F/U appointment 3 weeks later. SMM in case 2 decreased from 30.6 to 31.5 kg after WGC pharmacopuncture and increased to 32.1 kg at the F/U appointment 3 weeks after treatment (Fig. 2C). However, both patients had no noticeable difference in body weight (Fig. 2D).
5.3. Changes to protein and mineral levels in the body
For the elderly, a lack of protein or mineral content in the body can induce sarcopenic obesity.[16] In this study, protein in case 1 increased from 9.2 to 10.5 kg after pharmacopuncture with WGC, which was found to be increased further when measured at the F/U appointment 3 weeks later. Protein in case 2 increased from 10.7 to 11.0 kg after pharmacopuncture with WGC. Furthermore, it increased further to 11.3 kg when measured at the F/U appointment 3 weeks after treatment (Fig. 3A). Mineral content of the patient in case 1 increased from 2.85 to 3.54 kg after pharmacopuncture with WGC. When measured at the F/U appointment 3 weeks after treatment, the mineral mass decreased to 3.43 kg. Mineral content of the patient in case 2 decreased from 3.97 to 3.96 kg after pharmacopuncture with WGC, which then increased to 3.98 kg at the F/U appointment 3 weeks later (Fig. 3B). BMC in case 1 increased from 2.34 to 2.78 kg after WGC pharmacopuncture and decreased to 2.75 kg at the F/U appointment after 3 weeks. BMC in case 2 decreased from 3.28 to 3.26 kg after WGC pharmacopuncture and increased to 3.31 kg at the F/U appointment 3 weeks after treatment had ceased (Fig. 3C).
5.4. The changes of basal metabolic rate and fat free mass
BMR indicates the minimum energy required to sustain vital functions while at rest and is measured by a body mass analyzer. FFM is a known indicator closely related to BMR.[18] In this study, BMR in case 1 increased from 1353 to 1538 kcal after WGC pharmacopuncture, which then decreased to 1499 kcal when measured at the F/U appointment 3 weeks after treatments had stopped. BMR in case 2 decreased from 1582 to 1577 kcal after WGC pharmacopuncture and increased to 1599 kcal when measured at the F/U appointment 3 weeks after treatment (Fig. 4A).
Figure 4.
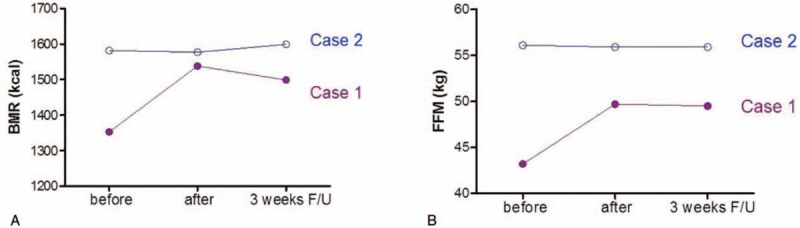
Changes in the basal metabolic rate. Pharmacopuncture with WGC was conducted on the subjects 5 times over 3 weeks. At the baseline, upon completion of the 5 treatments and a follow-up a follow-up appointment 3 weeks after the 5 treatments, the body composition analysis of the patients was analyzed using BIA. BMR, basal metabolic rate (A); and FFM, fat free mass (B). BIA = bioelectrical impedance analysis, BMR = basal metabolic rate, FFM = free fat mass, WGC = wild-ginseng complex.
In case 1, FFM increased from 43.2 to 49.7 kg after WGC pharmacopuncture and decreased to 49.5 kg at the F/U appointment after 3 weeks. In case 2, FFM decreased from 56.1 to 55.9 kg after WGC pharmacopuncture and continued to decrease until the F/U appointment 3 weeks after treatment (Fig. 4B).
6. Discussion
In recent years, there has been a sharp increase in the number of elderly people worldwide.[19] The proportion of people aged 60 and over in the population is also growing each year and is expected to double by 2050.[20] In the elderly, obesity is characterized by a greater mass of fat in the abdomen and a decrease in skeletal muscle mass. One of the major problems in the obese elderly population, is a progressive loss of skeletal muscle mass, muscle strength, and/or functionality, which can be described as age-related sarcopenia.[21–23] The elderly who suffer from this multifactorial pathological condition are at risk of adverse outcomes such as physical disability, injuries, frailty, social exclusion, hospitalization and increased mortality.[24] In this study, we introduced the effectively managed cases of 2 elderly patients who have abdominal obesity and skeletal muscle mass loss. The subjects were treated by pharmacopuncture with WGC in a Korean clinic.
In pharmacopuncture therapy for obesity treatment, direct injections into areas with a high fat-accumulation are frequently used to eliminate local cellulite and to treat internal problems with systemic manifestations. WGC extract containing wild ginseng is frequently used as a pharmacopuncture medicine for the treatment of obesity in Korean clinical practice. It is reported to have antiobesity effects in 3T3-L1 adipocytes through the inhibition of fat accumulation.[12] In these cells, it also increases PPARγ expression and adiponectin production.[12] It also has anti-inflammatory effects in LPS-stimulated RAW264.7 macrophages by inhibiting NO production and expression of iNOS, COX-2, and NF-κB.[12] In vivo studies have also reported antiobesity effects of pharmacopuncture with WGC in high fat diet-induced obese mice. The effects of this treatment on the mice included a decrease of AST, ALT, γ-GTP, BUN, total cholesterol, LDL-cholesterol, leptin, and increased HDL-cholesterol.[12] From this study the treatment was also deemed to be safe to use in the mice.[12] In clinical studies, pharmacopuncture with WGC induced weight loss as well as a decrease in cholesterol, insulin, and leptin levels in young female patients.[13] In our study, pharmacopuncture with WGC also improved the symptoms of the elderly obese patients by decreasing the abdominal fat accumulation, increasing protein content and BMR, and improving the ratio of muscle to fat.
Wild ginseng, a main active component of WGC, is a representative herb used to strongly tonify source qi in traditional medicines, which can be beneficial for elderly people who lack energy. The herb has also been reported to have many pharmacological effects such as anticancer properties, anti-inflammatory properties, and antidiabetic activities.[25] Due to the various biological properties of the herb, it can be considered as a vital component for the treatment of age-related obesity and sarcopenic obesity. Previous studies have shown that Bovis Calculus, Ursi Fel, and Moschus have various positive effects such hepaprotection, anti-inflammatory properties, antioxidant properties, immune regulation, anticancer properties, and antiobesity.[25] Therefore, it is believed that the antiobesity effects of pharmacopuncture with WGC may be derived from the effects of each component of the herb. However, there have been very few studies investigating the use of the pharmacopuncture with WGC on elderly patients with obesity. In this study, we found that 2 elderly patients with obesity, treated using pharmacopuncture with WGC, showed an improvement in their appearance through changes to body composition. These changes included a decrease in fat mass and an increase of muscle mass after the 3 week treatment period.
Obesity caused by aging is characterized by changes in body composition such as an increase in visceral body fat, which accumulates more in the abdominal area, and a reduction in skeletal muscle mass.[26] In this study, we analyzed the degree of abdominal obesity in 2 elderly obese patients, based on WC and WHR. According to WHO guidelines, WC and WHR are superior indicators of abdominal obesity to BMI, especially for elderly and Asian populations.[26,27] We also measured the ratio of muscle to fat using BFM, BFP, and SMM from BIA. As a result, the levels of WC, WFR, BFM, and BFP were decreased after pharmacopuncture with WGC, and the SMM levels were increased in elderly patients with obesity. However, there was no change to the body weight of the patients. This result indicates that pharmacopuncture with WGC extract can be beneficial for elderly patients who suffer with abdominal obesity and have a poor body composition.
The lack of protein or mineral content in the body can induce sarcopenia.[17,28] Furthermore, the amount of protein in the body is hugely important, especially for the elderly. It was reported that increasing the amount of protein in the body by 1 kg, reduced the risk of sarcopenia-related obesity in the elderly to 1 in 50.[17] In our study, the level of protein in elderly patients with obesity, increased after pharmacopuncture treatment with WGC. In addition, protein levels were maintained even after 3 weeks. Meanwhile, mineral levels in the patients showed different results. However the mineral levels in both patients increased when measured at the F/U appointment after 3 weeks. From these results, we believe that the use of pharmacopuncture with WGC for increasing protein and mineral levels in elderly obese patients is much more beneficial than other potential treatments.
One of the characteristics of aging, is the degradation of metabolic function that is observed in metabolic syndromes including systemic hypertension, obesity, and type 2 diabetes mellitus.[29] BMR indicates the minimum energy required to sustain vital functions and it is reported that fat mass stored in the body can decrease as a result of increased BMR through effective treatments for obesity.[30] In our study, BMR in case 1 increased after 5 pharmacopuncture treatments with WGC over 3 weeks compared to the baseline measurement. In addition, this change was maintained even after 3 weeks. BMR in case 2 increased only at the F/U appointment 3 weeks after the treatments were administered. These results indicate that pharmacopuncture with WGC is beneficial for increasing metabolic function in elderly patients with obesity. We believe this occurs due to the activating effects of wild ginseng complex on body metabolism.[31]
In summary, pharmacopuncture with WGC 5 times over 3 weeks improved abdominal obesity with an increase to the muscle/fat ratio, muscle mass, protein contents, and BMR. There was also a decrease of WC and fat mass in the 2 elderly patients with obesity. Although only 2 cases, our study indicates that pharmacopuncture with WGC can be used as a new alternative treatment method to prevent and improve abdominal obesity in the elderly as well as age-related sarcopenic obesity. In further studies, we plan to carry out a clinical trial with a larger sample size, conduct follow-up appointments over a longer period of time, and in addition, utilize various evaluation methods to verify the therapeutic effects of pharmacopuncture with WGC in the long term.
Acknowledgments
The authors thank the patients for agreeing with our report and for providing a detailed medical history.
Author contributions
Conceptualization: Ji Hye Hwang, Hyo Won Jung.
Data curation: Ji Hye Hwang.
Formal analysis: Ji Hye Hwang.
Investigation: Ji Hye Hwang.
Methodology: Ji Hye Hwang.
Resources: Ji Hye Hwang.
Supervision: Hyo Won Jung.
Visualization: Ji Hye Hwang, Hyo Won Jung.
Writing – original draft: Ji Hye Hwang.
Writing – review & editing: Hyo Won Jung.
Footnotes
Abbreviations: BFP = body fat percentage, BMC = bone mineral content, BMR = basal metabolic rate, BW = body weight, F/U = follow-up, FFM = free fat mass, HC = hip circumference, SMN = skeletal muscle mass, TKM = Traditional Korean Medicine, WC = waist circumference, WGC = wild-ginseng complex, WHR = waist-hip ratio.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP: Ministry of Science, ICT & Future Planning) (No. NRF-2017R1C1B5076224).
Competing interests: The authors declare no conflicts of interest regarding the publication of this paper.
References
- [1].World Health Organization. Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- [2].Alley DE, Chang VW. The changing relationship of obesity and disability, 1988–2004. JAMA 2007;298:2020–7. [DOI] [PubMed] [Google Scholar]
- [3].Amarya S, Singh K, Sabharwal M. Health consequences of obesity in the elderly. J Clin Gerontol 2014;5:63–7. [Google Scholar]
- [4].Case A, Menendez A. Sex differences in obesity rates in poor countries: evidence from South Africa. Econ Hum Biol 2009;7:271–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Han T, Tajar A, Lean M. Obesity and weight management in the elderly. Br Med Bull 2011;97:169–96. [DOI] [PubMed] [Google Scholar]
- [6].Han T, Wu F, Lean M. Obesity and weight management in the elderly: a focus on men. Best Pract Res Clin Endocrinol Metab 2013;27:509–25. [DOI] [PubMed] [Google Scholar]
- [7].Newman AB, Kupelian V, Visser M, et al. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci 2006;61:72–7. [DOI] [PubMed] [Google Scholar]
- [8].Ding J, Kritchevsky SB, Newman AB, et al. Effects of birth cohort and age on body composition in a sample of community-based elderly. Am J Clin Nutr 2007;85:405–10. [DOI] [PubMed] [Google Scholar]
- [9].Frontera WR, Hughes VA, Fielding RA, et al. Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol 2000;88:1321–6. [DOI] [PubMed] [Google Scholar]
- [10].Kim JH. Korean Acupuncture, MoxibutionSoc. Pharmacopuncture therapy. Hanmi Medical Publishing Co, Acupuncture Medicine. Paju, Korea:2016. [Google Scholar]
- [11].Jung C, Jung JH, Lee MS. Jung C. Pharmacopuncturemedines. Kyungrak Medical Publishing Co, A Clinical Study of Immune Pharmacopuncturology. Chungnam, Korea:2011. [Google Scholar]
- [12].Kim MW, Lim HH, Song YK. Anti-obesity effect of wild ginseng complex pharmacopuncture on adipocyte and high fat diet-induced obese C57BL/6J mice. J Oriental Rehab Med 2012;22:67–90. [Google Scholar]
- [13].Lim JY. Efficacy and safety of wild ginseng complex pharmacopuncture on the abdominal fat: randomized, double blinded, placebo-controlled trial. Seongnam, Korea: Gachon University; 2013. [Google Scholar]
- [14].Yoo JE, Chon YJ. A case report for the effects of pharmacopuncture combined thread implantation therapy to improve localized obesity. J Korean Med Obes Res 2015;15:144–8. [Google Scholar]
- [15].Shin M. A case series: the effects of cultivated wild ginseng pharmacopuncture and thread implantation therapy on abdominal obesity. J Korean Med Obes Res 2013;13:46–50. [Google Scholar]
- [16].Yoo JE. The effects of wild ginseng complex pharmacopuncture combined with hyperthermia on abdominal obesity in post-menopause women: case report. J Korean Med Obes Res 2016;16:133–7. [Google Scholar]
- [17].Lee MH, Park YH. Prevalence and factors related to sarcopenic obesity among community-dwelling elderly women. J Korean Biol Nurs Sci 2017;19:30–7. [Google Scholar]
- [18].Harris JA, Benedict FG. A biometric Study of Basal Metabolism in Man. Washington: Carnegie Institution of Washington; 1919. [Google Scholar]
- [19].Hafez G, Bagchi K, Mahaini R. Caring for the elderly: a report on the status of care for the elderly in the Eastern Mediterranean Region. East Mediterr Health J 2000;6:636–443. [PubMed] [Google Scholar]
- [20].World Population Prospects. The 2002 Revision, Highlights. New York: United Nations Population Division; 2003. [Google Scholar]
- [21].Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol 2014;2:819–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Marcell TJ. Sarcopenia: causes, consequences, and preventions. J Gerontol A Biol Sci Med Sci 2003;58:M911–6. [DOI] [PubMed] [Google Scholar]
- [23].Dalle S, Rossmeislova L, Koppo K. The role of inflammation in age-related sarcopenia. Front Physiol 2017;8:1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Batsis JA, Mackenzie TA, Barre LK, et al. Sarcopenia, sarcopenic obesity and mortality in older adults: results from the National Health and Nutrition Examination Survey III. Eur J Clin Nutr 2014;68:1001–7. [DOI] [PubMed] [Google Scholar]
- [25].Kim MW, Song YK, Lim HH. The analysis of study trends of wild ginseng, Bovis Calculus, Ursi Fel, Moschus and the study on applied possibility as obesity medications. J Korean Med Obes Res 2011;11:41–68. [Google Scholar]
- [26].Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev 2007;8:41–59. [DOI] [PubMed] [Google Scholar]
- [27].Janssen I, Katzmarzyk PT, Ross R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. J Am Geriatr Soc 2005;53:2112–8. [DOI] [PubMed] [Google Scholar]
- [28].Breen L, Phillips SM. Skeletal muscle protein metabolism in the elderly: interventions to counteract the anabolic resistance of ageing. Nutr Metab (Lond) 2011;8:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 2005;365:1415–28. [DOI] [PubMed] [Google Scholar]
- [30].Sadiya A, Ahmed S, Siddieg HH, et al. Effect of Ramadan fasting on metabolic markers, body composition, and dietary intake in Emiratis of Ajman (UAE) with metabolic syndrome. Diabetes Metab Syndr Obes 2011;4:409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Park EY, Kim MH, Kim EH, et al. Efficacy comparison of Korean ginseng and American ginseng on body temperature and metabolic parameters. Am J Chin Med 2014;42:173–87. [DOI] [PubMed] [Google Scholar]


