Abstract
Rationale:
Parathyroid hormone PTH) levels are the main parameters to differentiate primary hyperparathyroidism (PHPT) from non-PTH-dependent hypercalcemia. We report a case of hypercalcemia with normal PTH levels due to a parathyroid adenoma.
Patient concerns:
A 52-year-old female patient presented with 2-year history of documented sustained high-normal serum calcium and hypercalcemia (2.51–3.03 mmol/L) with normal serum intact PTH levels (21.95–40.15 pg/ mL).
Diagnoses:
A parathyroid tumor was localized by ultrasonography and 99mTc-sestamibi dual-phase fusion imaging with single-photon emission computed tomography/computed tomography.
Interventions:
Parathyroidectomy was performed to excise the tumor completely.
Outcomes:
A 1.2-cm-sized parathyroid adenoma was removed surgically. The serum calcium was declined to normal level immediately after resection, as well as in 4- month follow-ups. The immunohistological diagnosis proved to be a PTH positive parathyroid adenoma.
Lessons:
In case of hypercalcemia, serum intact PTH and parathyroid imaging should be monitored to evaluate the presence of parathyroid adenoma with care because PHPT could present with inappropriate normal PTH.
Keywords: hypercalcemia, parathyroid adenoma, parathyroid hormone, primary hyperparathyroidism
1. Introduction
Primary hyperparathyroidism (PHPT) is usually considered by the occasional findings of hypercalcemia and confirmed by an elevated serum parathyroid hormone (PTH) concentration, mostly due to parathyroid adenoma. However, a few patients with PHPT exhibiting low normal serum PTH levels were reported global wide within recent decades,[1–5] but rarely in China. To our knowledge, this report first presents a case of PTH producing parathyroid adenoma with normal levels of serum PTH and hypercalcemia in China.
2. Case report
A 54-year-old female was referred twice to our inpatient department due to hypercalcemia in 2017. Hypercalcemia was first detected in February 2015. Her history revealed weakness, depression, loss of vitality, and endoscopically visible multiple gastric ulcers. She was diagnosed of coronary atherosclerosis by coronary computed tomographic angiography. The patient had no history of bone disease, hematuria, renal colic, urolithiasis, dyspepsia, or constipation. She had been treated for diabetes for 8 years, dyslipidemia for 1 year, and hypertension for 7 years, with medication of acarbose, metformin, pioglitazone, fenofibrate, omeprazole, clopidogrel, and valsartan-amlodipine at the present time. The onset of menopause was at the age of 52 and the patient opted to take calcium supplements since 2010 but quitted before the first hospitalization in 2017. Physical examination indicated no abnormalities. The patient was 160 cm in height and 60 kg in weight with a normal blood pressure of 122/72 mmHg and normal pulse rate of 78 per minute.
Laboratory data revealed sustained hypercalcemia, occasionally high-normal serum calcium (2.51–3.03 mmol/L, normal reference range: 2.0–2.60 mmol/L), and normal level of PTH (intact-PTH: 21.95–40.15 pg/mL, Roche Elysees PTH assays, normal reference range: 15.00–65.00 pg/mL) since 2015 (Table 1). There was no abnormality in the hormonal levels of the thyroid gland, gonadal gland, and corticosteroids. Urinalysis and blood chemistry were also normal. Tumor markers (including alpha-fetoprotein, carcinoembryonic antigen, carbohydrate antigen [CA]-125, CA-199, CA-242, CA-50, and CA-153) were within the normal range. Bone densitometry revealed the good preserved anteroposterior spine (T score, 0.6), total hip (T score, 0.9), and femoral neck (T score, 0.2). Chest computed tomography (CT) suggested tiny chronic inflammatory pulmonary nodules (maximum 5 mm) at bilateral lower lobes. Pituitary magnetic resonance imaging indicated suspected microadenomas (2 mm). There were no positive findings of parathyroid gland by ultrasound in 2015 (once) and 2017 (twice). During the latest admission, ultrasound of the cervical region indicated a well-demarcated tumor located behind the right upper lobe of the thyroid gland (Fig. 1). Using 99mTc-sestamibi dual-phase fusion imaging by single-photon emission computed tomography/computed tomography (SPECT/CT) revealed an area of increased uptake in the same region depicted by ultrasonography, which indicated a functional parathyroid adenoma (Fig. 2).
Table 1.
The level of serum calcium, serum phosphorus, serum 25-hydroxyvitamin D3, serum PTH, urine calcium, and urine phosphorus.
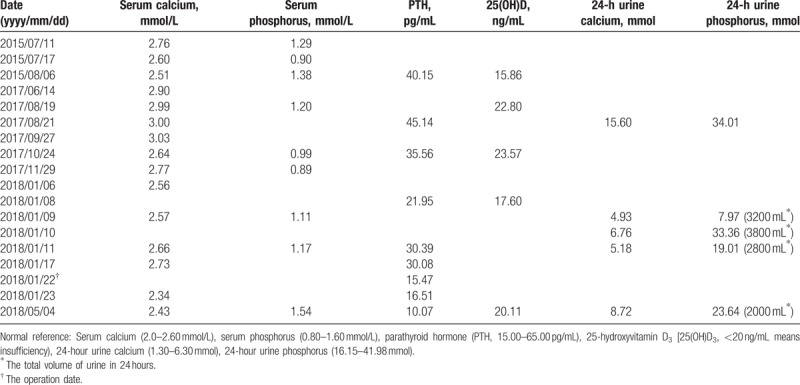
Figure 1.

Neck ultrasonography. Findings suggested that the proliferated solidly tumor was located in the right upper lobe of thyroid gland. The boundary with the surroundings was relatively well demarcated and a low-echoic area with a partially uneven echo level was noted.
Figure 2.
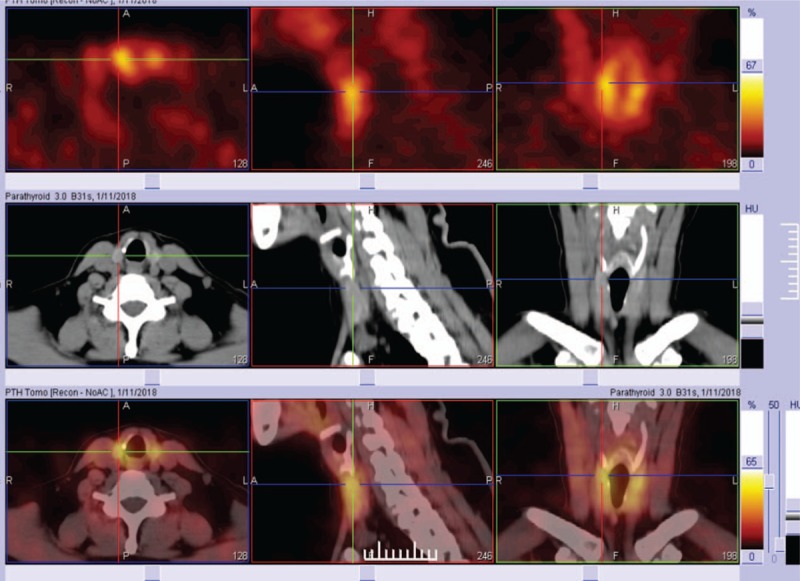
99mTc-sestamibi scintigraphy with SPECT/CT fusion imaging. Dual-phase 99mTc-sestamibi parathyroid scintigraphy showed focal radioactivity retention at the superior pole of the right thyroid lobe in the delayed phase which was consistent with parathyroid adenoma while complete washout of the radioactivity was seen throughout the thyroid gland.
A 1.2-cm-sized parathyroid adenoma was removed on January 22, 2018. The diagnosis of adenoma was histologically confirmed by the pathologist (Fig. 3). The adenoma was separated from the uninvolved parathyroid parenchyma by a thin and intact edematous capsule. Hematoxylin and eosin (H&E) staining indicated that the adenoma was full of chief cells and a small percentage of oxyphils, with an absence of fibroadipose tissue. The tumor cells were immunohistochemically positive for PTH (mouse antihuman PTH monoclonal antibody; Maxim Biotechnology). Low molecular weight cytokeratins and chromogranin A were also immune-reactive.
Figure 3.
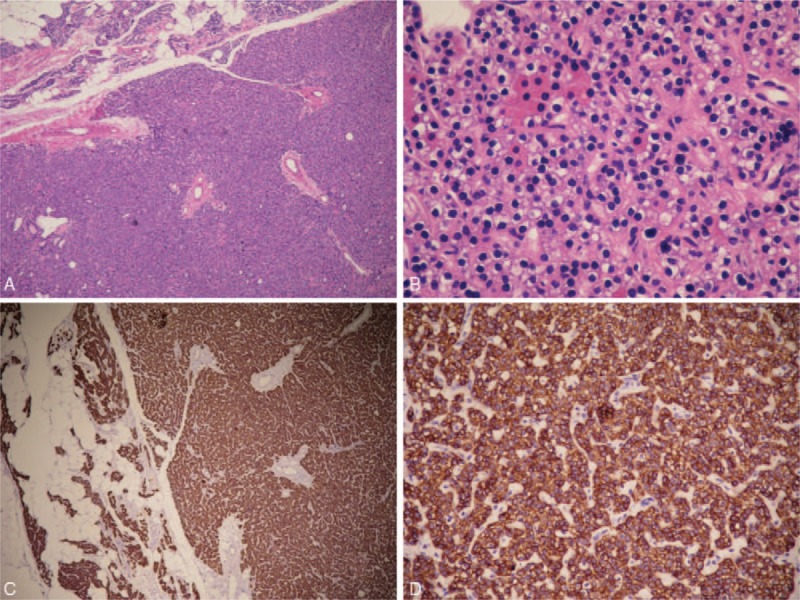
H&E staining and PTH staining. Histological sections of H&E staining showed the parathyroid gland was composed of medullary tumor with atrophic paranchyma at the periphery (A–B). The adenoma was consisted mostly of chief cells, including a small number of eosinophilic cells. The tumor cells were strongly positive for PTH immunostaining (C–D). (A, C) 60 × original magnification; (B, D) 600 × original magnification.
Serum calcium decreased to normal level of 2.34 mmol/L and PTH level was lowered to a more normal level (15.47 pg/mL right after resection and 16.51 pg/mL 1-day postoperatively). In a 4-month follow-up on May 4, 2018, the patient still presented with normal serum calcium (2.43 mmol/L) and normal PTH level (10.07 pg/mL).
This case report was approved by the ethics committee of Shanghai Jiaotong University Affiliated Sixth People's Hospital, Shanghai, China, and written informed consent was obtained.
3. Discussion
The level of PTH is inversely and tightly regulated by the level of serum calcium. Hypercalcemia leads to cessation of PTH production, except for the presence of hyperparathyroidism. The level of PTH distinguishes parathyroid disease-dependent hypercalcemia from malignancy-related hypercalcemia. However, the female patient we reported here presented as mild-to-moderate hypercalcemia and normal PTH level without an underlying malignancy. The incidental localization of parathyroid adenoma by the latest ultrasound led to the determination of a rare case of PHPT-related hypercalcemia, proved both by surgery and pathology.
The most common cause of PHPT is the adenoma in parathyroid gland composed mainly of chief cells producing PTH. However, the frequency of inappropriately “normal” serum PTH levels was estimated to be 5% to 20% in the occurrence of PHPT,[1] although it has been rarely reported in China. A few cases had been reported for functional adenoma with normal PTH levels,[2–5] but there is no consensus on the unexplained biochemical presentation of hypercalcemia, normal PTH levels, and histological features of parathyroid adenoma. Some literature suggested that patients with normal PTH were younger and less symptomatic in terms of hypercalcemia compared with overt patients.[4] Oxyphil parathyroid adenoma was reported to be an uncommon cause of hypercalcemia while exhibiting normal PTH[5–7]; however, immunohistostaining excluded such possibility for our case.
Therefore, PHPT is recommended to be defined as hypercalcemia with increased or inappropriately normal plasma PTH according to a Canadian and international consensus in 2017.[8] The mechanism of inappropriately low PTH level in PHPT remains unknown and might be caused by multiple reasons: a hook effect generated by a circulating autoantibody against the PTH, or the pulsatile secretion of PTH by adenoma, or an increased biologic activity by abnormal PTH, or increased tissue sensitivity to PTH due to postreceptor gene mutation, or an intragenic mutation producing an abnormal PTH, or hemorrhage and necrosis inside the tumor, or other mediator of hypercalcemia (e.g., parathyroid hormone-related protein [PTHrp], fibroblast growth factor-23). Normocalcemic PHPT with high level of PTH has been recognized for the initial stages of overt PHPT. However, there is no case of PHPT with inappropriate normal PTH level to be reported in the published literatures from China.[9–11] Infusion imaging with SPECT/CT is valuable for identification of functional parathyroid adenoma,[12] especially for such cases of PHPT with inappropriate normal PTH.
PTHrp belongs to the PTH family and is the main cause of the malignancy-related hypercalcemia with the presentation of the “normal” level of PTH. As PTHrp detection is not available in our clinical laboratory, we could not exclude the possibility of PTHrp-related hypercalcemia, even if malignant tumors were ruled out in the patient.
The quick recovery from hypercalcemia of the patient and decline in half of PTH level after resection suggested it to be a successful parathyroidectomy. However, whether the patients with the “normal” preoperative PTH level could benefit from the surgery in terms of risk reduction for hypercalcemia-related mortality and morbidity from cardiovascular disease or bone turnover remains a long-term follow-up.
In conclusion, we reported a case of hypercalcemia with “normal” level of intact PTH due to surgical and immunostaining proved parathyroid adenoma, which is rarely reported in China. In case of hypercalcemia, serum calcium, serum intact PTH, and parathyroid imaging should be monitored with care even if initial PTH assay indicates normal or imaging evidence is negative.
Author contributions
Conceptualization: Can Pang, Yuqian Bao.
Data curation: Can Pang, Haoyong Yu.
Formal analysis: Can Pang, Youben Fan, Yuqian Bao.
Investigation: Can Pang, Youben Fan, Haoyong Yu, Yuqian Bao.
Methodology: Huizhen Zhang, Boming Guo, Jie Kang, Xianzhao Deng.
Resources: Yuqian Bao.
Validation: Youben Fan, Huizhen Zhang, Haoyong Yu, Boming Guo, Jie Kang, Xianzhao Deng.
Writing – original draft: Can Pang.
Writing – review and editing: Can Pang, Youben Fan, Huizhen Zhang, Yuqian Bao.
Footnotes
Abbreviations: CA = carbohydrate antigen, CT = computed tomography, H&E = hematoxylin and eosin, PTH = parathyroid hormone, PHPT = primary hyperparathyroidism, SPECT = single-photon emission computed tomography.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Mischis-Troussard C, Goudet P, Verges B, et al. Primary hyperparathyroidism with normal serum intact parathyroid hormone levels. QJM 2000;93:365–7. [DOI] [PubMed] [Google Scholar]
- [2].Lafferty FW, Hamlin CR, Corrado KR, et al. Primary hyperparathyroidism with a low-normal, atypical serum parathyroid hormone as shown by discordant immunoassay curves. J Clin Endocrinol Metab 2006;91:3826–9. [DOI] [PubMed] [Google Scholar]
- [3].Gulcelik NE, Bozkurt F, Tezel GG, et al. Normal parathyroid hormone levels in a diabetic patient with parathyroid adenoma. Endocrine 2009;35:147–50. [DOI] [PubMed] [Google Scholar]
- [4].Bergenfelz A, Lindblom P, Lindergard B, et al. Preoperative normal level of parathyroid hormone signifies an early and mild form of primary hyperparathyroidism. World J Surg 2003;27:481–5. [DOI] [PubMed] [Google Scholar]
- [5].Gurrado A, Marzullo A, Lissidini G, et al. Substernal oxyphil parathyroid adenoma producing PTHrP with hypercalcemia and normal PTH level. World J Surg Oncol 2008;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Matsushita H, Hara M, Nakazawa H, et al. The presence of immunoreactive parathyroid hormone-related protein in parathyroid adenoma cells. Acta Pathol Jpn 1992;42:35–41. [DOI] [PubMed] [Google Scholar]
- [7].Bleier BS, LiVolsi VA, Chalian AA, et al. Technetium Tc 99m sestamibi sensitivity in oxyphil cell-dominant parathyroid adenomas. Arch Otolaryngol Head Neck Surg 2006;132:779–82. [DOI] [PubMed] [Google Scholar]
- [8].Khan AA, Hanley DA, Rizzoli R, et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int 2017;28:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Zhao L, Liu JM, He XY, et al. The changing clinical patterns of primary hyperparathyroidism in Chinese patients: data from 2000 to 2010 in a single clinical center. J Clin Endocrinol Metab 2013;98:721–8. [DOI] [PubMed] [Google Scholar]
- [10].Wang W, Kong J, Nie M, et al. Primary hyperparathyroidism in Chinese children and adolescents: a single-centre experience at Peking Union Medical College Hospital. Clin Endocrinol (Oxf) 2017;87:865–73. [DOI] [PubMed] [Google Scholar]
- [11].Hu Y, Cui M, Sun Z, et al. Clinical Presentation, Management, and Outcomes of Primary Hyperparathyroidism during Pregnancy. Int J Endocrinol 2017;2017:3947423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wong KK, Fig LM, Gross MD, et al. Parathyroid adenoma localization with 99mTc-sestamibi SPECT/CT: a meta-analysis. Nucl Med Commun 2015;36:363–75. [DOI] [PubMed] [Google Scholar]


