Abstract
To evaluate the effect of the social support on adherence of highly active antiretroviral therapy (HAART) of people living with human immunodeficiency virus/acquired immune deficiency syndrome (PLWHA). Participants of PLWHA at Beijing, China were intervened by 1-year social support program intervention. Difference of social support scale and medication adherence scale before and after the intervention were evaluated. Our results showed that there were statistically significant difference for total score and subjective score, medication adherence between before and after intervention (t = −3.62, −2.81, 5.75, P < .05), and there were statistically significant correlation between the difference of total social support score and that of social support utilization score, and the difference of medication adherence score (r = 0.14, 0.12, all P < .05). Multifactor linear regression showed that the medication adherence score was influenced by the insurance status, the residential status, and the difference in the social support utilization score (β = −0.14, 0.17, 0.16, all P < .05). Social support and care-giving can exert some influence and facilitate PLWHAs adherence of HAART.
Keywords: AIDS, intervention study, medication adherence, social support
1. Introduction
Acquired immune deficiency syndrome (AIDS) is a major public health concern for the entire world, especially for China. Data from May of 2017 show that the number of reported people living with human immunodeficiency virus (HIV)/AIDS (PLWHA) in China has reached 708,158.[1] In order to achieve an improvement in life expectancy as well as in quality of life, more PLWHAs need to be placed on life-long highly active antiretroviral therapy (HAART).[2] However, incomplete adherence to HAART is common in all groups of treated individuals, which may eventually undermine the dramatic improvements in HIV-related health parameters expected with the rising availability of HAART in developing countries.[3–5]
Consistent associations are found between certain psychosocial factors and adherence behavior. Since PLWHAs often face stigma in their communities and among family and friends, social support has been shown to play an important role in PLWHAs’ medication adherence.[6–8] Social support refers to spiritual and material help and support from parents, relatives, friends, and communities.[9] Since, in Beijing China, the overwhelming majority of PLWHAs have been infected by male-to-male sexual behavior, the means of developing a social support model suitable for this community are vital for China's AIDS control.
One possible solution is to use peer educators who have the same cultural background and emotional experience as members of the PLWHA community.[10,11] Therefore, an interventional model integrating peer educators into medical facility and faculty to strengthen and consolidate peer's social support for PLWHAs’ medication adherence should be studied. However, most studies regarding the influence of social support on medication adherence have not studied the impact of a comprehensive package of psychosocial interventions in improving medication adherence.[12–14] Therefore, our study aims to evaluate the interventional effect of the social support on adherence of HAART of PLWHAs, to further develop an appropriate model of social support and care-giving, and to provide policy makers with reference materials of nursing and care in the PLWHA community.
2. Methods
2.1. Study design
A nonrandomized community intervention study was conducted.
2.2. Participants
Inclusion criteria for participants include meeting the standard antiviral treatment of AIDS in China (an adult PLWHA will begin treatment when CD4+ T lymphocytes ≤350/mm3 and early treatment is recommended when CD4+ T lymphocytes is in 350–500/mm3 range).[15] Age over 18 years; currently receiving HAART; and voluntarily entering into the “Love Home” social support institute (further described below).
Exclusion criteria include PLWHA with communication difficulties; PLWHA with severe diseases incapable of completing the study; and PLWHA who refuses to take part in the study.
2.3. Intervention
At baseline, 277 eligible participants were diagnosed and referred to the Love Home social support institute. Love Home was founded by Beijing You-An Hospital in 1998, being the first social support institute for PLWHA in China. The staff consist of several nurses as its chief constituents who work alongside with 5 full-time volunteers, and with 50 part-time volunteers from the PLWHA community. The Love Home community is divided into several well-operated small groups and each small group is further divided into subgroups composed of 9 core individuals, including 1 nurse, 1 fellow volunteer, and 1 social volunteer. In this manner, it provides a comprehensive service, including health education, stress management, and social interactions, with the intention of providing PLWHAs with therapeutic support.
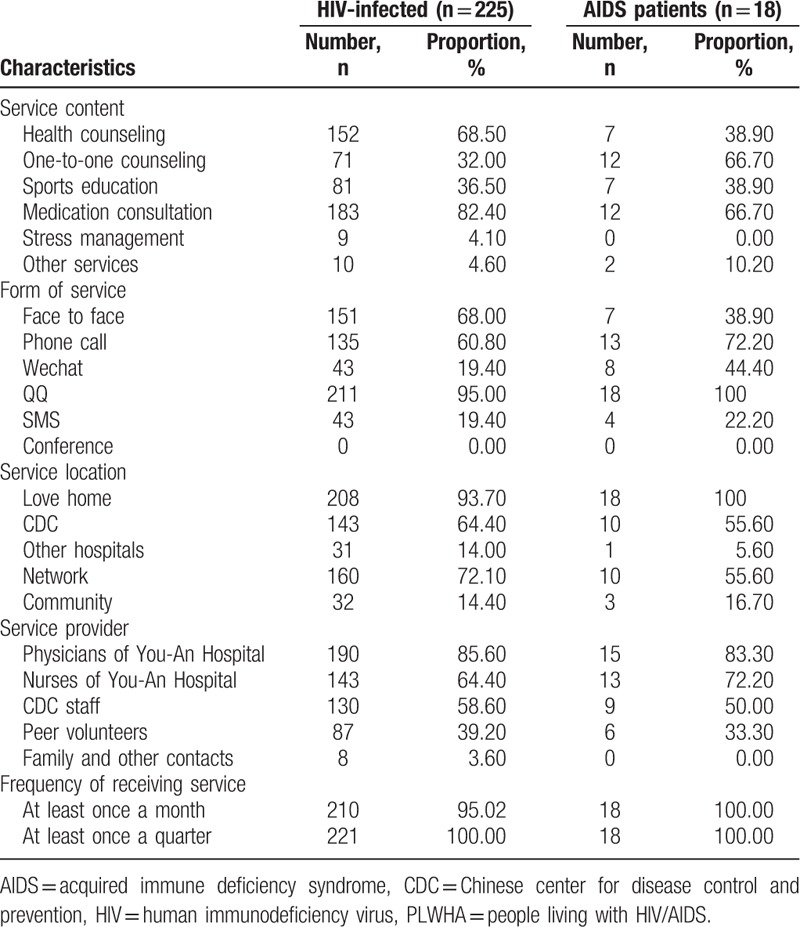
After recruiting participants, collecting baseline information, conducting risk evaluation, and classifying into HIV or AIDS group based on CD4 count, the intervention was carried out in succession from December 2013 to December 2014. Subsequently, a second survey was conducted in December 2014 to evaluate the effect of social support and care-giving on their medication adherence. The social support and care-giving intervention protocols are further described in Tables 1 and 2.
Table 1.
Social support and care model for PLWHA.
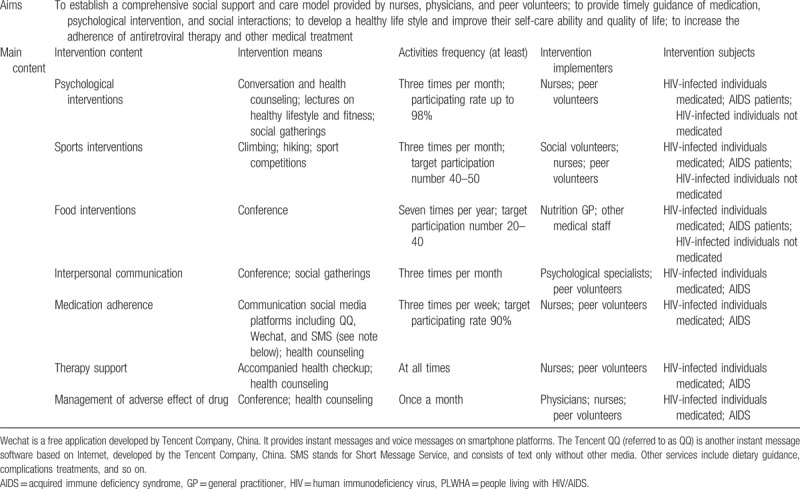
Table 2.
The acceptance of social support and care-giving of the PLWHA population in the past 3 months from 2014 to 2015 (n = 243).
2.4. Data collection
2.4.1. Demographic indicators
Data on gender, age, marital status, education level, medical insurances, residence, and registration status were collected.
2.4.2. Social support scale
The Scale of Social Support was adopted to evaluate the individuals’ subjective feelings about social support and care provided by the Love Home social support institute for PLWHA. This scale included 3 dimensions: subjective support, objective support, and social usefulness. Among them, objective support means objective, visible, and applicable support, including material support, social networks, and interpersonal relationships. Subjective support is defined as an emotional experience whenever they are respected, supported, and understood in the social interactions. Usage of social support indicates the extent, to which individuals use social support. When adding the above dimensions together, we got a total score for social support, in which higher scores correlate with higher levels of social support. This scale has been verified with good reliability and validity.[16] To evaluate the impact of social support and social care model on PLWHAs’ score of social support, our study analyzed the difference of total and 3 dimensions of scores before and after the intervention (net benefit value).
2.4.3. Evaluation of medication adherence
Medication adherence was determined through face-to-face interview and by asking the following question: “In the past 30 days, how many times did you take your medications within 1 hour of the set time.” Participants’ answers were categorized according to the following scores: “never” = 1, “seldom” = 2, “less than half of the time” = 3, “around half of the time” = 4, “more than half of the time” = 5, and “always within 1 hour of the set time” = 6.[15] When adding the above numbers together, we got a total score for medication adherence correlating between higher scores and higher level of medication adherence. The net benefit value of adherence was calculated by the methods described above. In addition, the correlation between social support scale and medication adherence was evaluated.
2.5. Statistical methods
Data were entered twice to the statistical program of Epidata 3.0 to ensure accuracy. SPSS 19.0 was adopted for data analysis, and the chi-squared test was used to compare the distribution of the social demographic indicators between infected individuals and AIDS patients. The paired t test or nonparametric test was conducted to compare the difference of total score and each dimension score of social support scale and the medication adherence scale before and after intervention. Pearson or Spearman correlation test was used to analyze the correlation between net benefit value of social support and adherence. Multifactor linear regression was adopted to evaluate the influence of medication adherence score exerted by social support score by controlling the demographic indicators. All P value < .05 was considered statistically significant difference.
2.6. Ethics review
The study followed the principles outlined in the Declaration of Helsinki. The patients received both written and oral information about the study before they gave their informed consent. In the information, it was emphasized that participation was voluntary and could be terminated at any time during the study. The patients were also assured about confidentiality. Permission for the study was obtained from the Ethical Review Board in You-An Hospital Ethics Committee (Reg. No. Jingyoukelunzi [2014] No.7).
3. Results
3.1. Participant characteristics
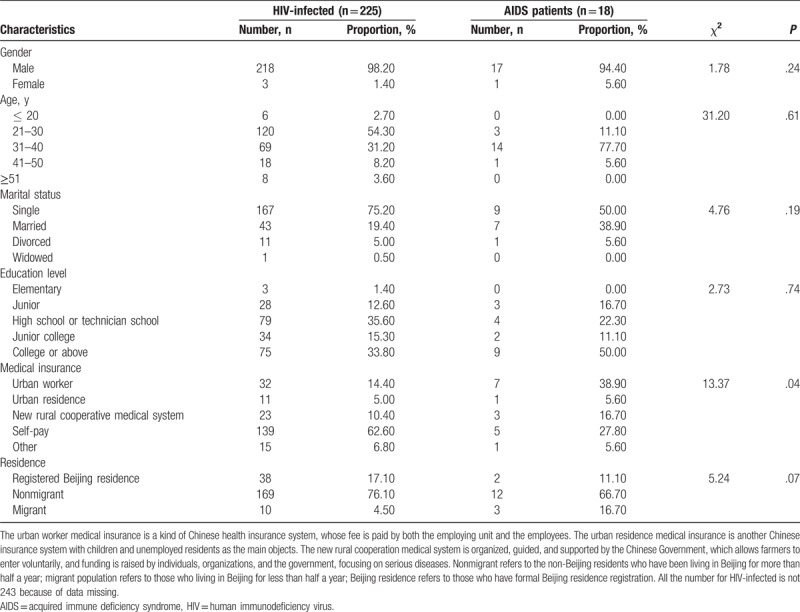
In the study, 243 eligible PLWHAs were finally selected and recruited into intervention group. At the baseline survey, 7.6% of the 243 eligible participants were classified as having AIDS. Most patients were men. Patients with HIV were mostly between the ages of 21 to 30 years, while AIDS patients were generally between the ages of 31 to 40. PLWHAs were mostly single, with a college level of education, obtained medical insurance through their work, and were nonmigrants (Table 3).
Table 3.
Baseline characteristics of participants, in 2014 (n = 243).
3.2. Net benefit value of social support and medication adherence
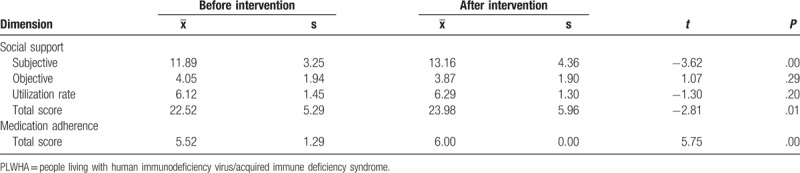
Our results showed that there were significant differences in the total score and the subjective support score after the intervention (t = −3.62, −2.81, P < .05). Before the intervention, the total social support score was 22.52 ± 5.29 points, while after intervention the score increased to 23.98 ± 5.96 points, which indicated that total social support score and subjective support were significantly higher than that before the intervention. This signified in depth that the mode of social support and care-giving could probably exert influence to improve the total score and subjective support score. Conversely, objective support and support utilization scores showed that there were no statistically significant changes (all P > .05). Medication adherence was increased with statistical significance after the intervention (t = 5.75, P < .05), from 5.52 ± 1.29 points before the intervention to 6.00 ± 0.00 points afterward (Table 4).
Table 4.
Comparison of social support scores and medication adherence before and after social care intervention for PLWHA from 2014 to 2015 (n = 243).
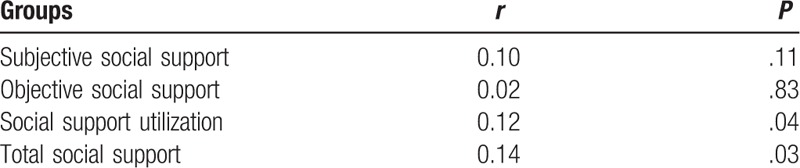
3.3. Correlation analysis between medication adherence and social support
The results of linear correlation analysis showed that there was a statistically significant correlation between the net benefit value of total social support score and that of social support utilization score, and that of medication adherence (r = 0.14, 0.12, all P < .05), with a weak correlation revealing that the net benefit value of total social support score and social support utilization score would affect the improvement of medication adherence to some extent. The net benefit value of subjective and objective support score and the difference of medication adherence score, however, showed no statistically significant correlation (all P > .05) (Table 5).
Table 5.
Correlation analysis between the difference of medication adherence scores and the difference of various dimensions of social support scores from 2014 to 2015 (n = 243).
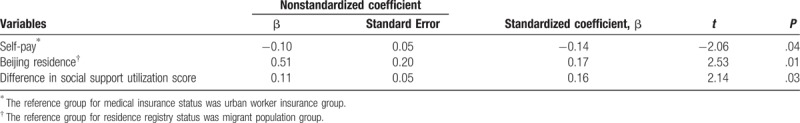
3.4. Multifactor analysis on factors related to effectiveness of mediation adherence
The multifactor linear regression results showed that self-paid status of medical insurance (reference group as urban worker insurance), Beijing nonmigrant status of residence registry (reference group as migrant population) and the net benefit value of social support utilization score had statically significant influence on that of medication adherence score (standardized β = −0.14, 0.17, 0.16, all P < .05), which indicated that the net benefit value of medication adherence of the self-paid PLWHAs was 0.14 times lower than that of those participants with urban worker insurance, and the net benefit value of medication adherence score of the registered Beijing residence population has a 0.17 times higher than that of those migrant PLWHAs, with the medication adherence rate rising 0.16 times for each 1 point rise in net benefit value of social support utilization score. However, our results showed that there was no statistically significant relation between other factors and the net benefit value of medication adherence (all P > .05) (Table 6).
Table 6.
The result of social support and other factors that affect mediation adherence by linear regression analysis (n = 243).
4. Discussion
In countries with broad access to effective antiretroviral therapy (HAART), HIV/AIDS has transformed from an acute disease often lethal in the first 2 years after AIDS illness to a chronic disease with life expectancy now measured in decades.[17] For the PLWHA population, the adherence to the antiviral medication is crucial for survival and mostly depends on influences from the various support, including material and mental support from community, family, and friends. Hence, it is of great importance to explore the social support, social care pattern, and implement strategy toward PLWHAs.[18–21] Therefore, we designed and implemented our social support and care-giving intervention model according to the characteristics of Beijing community residence and the Love Home social support institute.[22] Also, we have further evaluated the relationship between medication adherence and the social support level to provide more evidence to AIDS patients nursing and care.
The intervention population was composed of highly educated single young male adults with HIV infection who were predominantly native residents (nonmigrants) and had their medication covered by themselves. The social support and care-giving interventions mainly included one-on-one consultation on medication by care-givers consisting of nurses, physicians, and peer volunteer. Our results revealed good levels of intervention coverage and participation.
Our study examined a package of interventions utilizing social support to improve medication adherence. We found the intervention had a significant and positive effect on the sense of social support, as perceived by the participants. The medication adherence was positively related to the presence of the social support. This supports the role of social support and care-giving on medication adherence, although a relative weak correlation was identified, which could probably be attributed to the lack of comprehensive social care and support as well as other relevant factors not under consideration in our study. Therefore, we recommend further study to be conducted in this field.[23,24]
The multivariable linear analysis showed that the main factors related to the medication adherence were the net benefit value of utilization of social support, possession of medical insurance, and residential status, which is consistent with previous reports globally that the implementation of social support and care-giving proved to be a successful strategy that influences PLWHAs’ health.[13,14,23] Under the support and guidance of trained peer volunteers, who were HIV-infected with similar background as the participants, but with good medical adherence rates, PLWHAs’ medication adherence could effectively improve. In our study, this improvement was achieved by intermediate variables such as self-efficacy that transfers the influence of the implementation of social support to the medication adherence. The more the PLWHAs made use of the social support, the higher his/her self-efficacy was, which led to a better medication adherence.[12,25]
Our findings also suggest that except for providing proper social support, more attention should be given to encourage the PLWHA community to further utilize their social support and care-giving network. Therefore, we highly recommend a beneficial social environment should be created to encourage a higher participation for PLWHA community, in order to improve their medication adherence. As another influencing factor, the residence status should be taken into consideration, as the migrant population's medication adherence is often altered by their frequent change of treatment location, compared with the fixed registered Beijing residence. Our results further indicate that this discriminative medical insurance policy also prevents the migrant population from getting local prompt medical care. Those whose treatment is not covered by insurance have a comparatively lower medication adherence compared to the registered Beijing residence.
In summary, the article reveals that our social support and care-giving model and status of medical insurance as well as residence registry can exert multiple benefits in facilitating PLWHAs’ adherence of HAART. To further ameliorate this situation, attentions should also be paid to various social characteristics, such as medical insurance of the PLWHA population. However, limitations of this study also exist. Since the study was not a randomized community intervention trial with a parallel control group, its scientific sense was inevitably compromised to some extent. Moreover, the intervention interval was relatively short, leading to masked intervention factors that could only be accessed through a longer study period.
Based on the findings of this study, we would like to put forward the following suggestions:
-
1.
A more integrative social support and care-giving system should be provided to the PLWHA community. The government should take more responsibility to remove stigmatization and discrimination toward the HIV/AIDS population by using social activities and media publications to promote acceptance by society. More people should be motivated to join the social support system.
-
2.
Strong measures should be taken to motivate the PLWHA population to join and utilize the social support system. The medical care personnel and volunteers should operate on the community level, making use of available network platforms to inspire more PLWHAs to join and improve their medication adherence.
-
3.
Effective policy measures should be taken to improve the medical insurance coverage for the migrant population, which would improve their access to diagnosis and treatment services, lower the economical burden on the migrant PLWHA population, and encourage usage of antiviral treatment in this community.
5. Conclusion
Our article reveals that our social support and care-giving model, status of medical insurance and residence registry can exert multiple benefits in facilitating PLWHAs’ adherence of HAART. To further ameliorate this situation, attentions should also be paid to various social backgrounds as medical insurance of the PLWHA population.
Acknowledgments
The authors would like to extend our appreciation to the 243 participants of this survey. The authors would also like to thank the Office of Beijing Traditional Medicine who sponsored us for the survey. Especially we would extend our thanks to those social volunteers, nurses, physician, and peer volunteers who contributed dramatically to the process of data collection and social support and care-giving to PLWHAs.
Author contributions
Xing-Ming Li conceived the study design, conceptualized the ideas, and supervised the whole analytical procedure. Scottie Bussell contributed to this writing during his fellowship. Xiao-Qing Yuan conducted the study design and the data collection and supervised the manuscript writing. Jun-Jie Wang, Wan-Ying Zhang and Alon Rasooly provided technical support for drafting and revising the manuscript.
Conceptualization: Xiao-Qing Yuan, Alon Rasooly, Jun-Jie Wang.
Data curation: Xiao-Qing Yuan, Alon Rasooly.
Formal analysis: Xing-Ming Li, Xiao-Qing Yuan.
Methodology: Xing-Ming Li, Xiao-Qing Yuan, Scottie Bussell, Jun-Jie Wang.
Project administration: Xing-Ming Li, Xiao-Qing Yuan.
Supervision: Scottie Bussell.
Writing – original draft: Alon Rasooly, Wan-Ying Zhang.
Writing – review and editing: Xing-Ming Li, Alon Rasooly, Scottie Bussell.
Footnotes
Abbreviations: HAART = highly active antiretroviral therapy, PLWHA = people living with human immunodeficiency virus/acquired immune deficiency syndrome.
Capital Chinese Medicine and Nursing Important Health Research Project in 2013 (No. 13HL02).
The authors have no conflicts of interest to disclose.
References
- [1].NCADS, NCSTD, China CDC. Update on ADS/HIV epidemic in China and main response in control and prevention in May, 2017. Chin J AIDS STD 2017;23:581–583. [Google Scholar]
- [2].Tao LL, Liu M, Li SM, et al. Impact of Antiretroviral Therapy on the Spread of Human Immunodeficiency Virus in Chaoyang District, Beijing, China: Using the Asian Epidemic Model. Chin Med J 2017;130:32–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Xiao-Hua X, Qing-Yan W, Meng-Xin C. A systematical review of peer support in elevating drug adherence among HIV/AIDS patients. J Nurs Adm 2016;16:847. [Google Scholar]
- [4].Garcia de Olalla P, Knobel H, Carmona A, et al. Impact of adherence and highly active antiretroviral therapy on survival in HIV-infected patients. J Acquir Immune Defic Syndr 2002;30:105–10. [DOI] [PubMed] [Google Scholar]
- [5].Hogg RS, Heath K, Bangsberg D, et al. Intermittent use of triple-combination therapy is predictive of mortality at baseline and after 1 year of follow-up. AIDS 2002;16:1051–8. [DOI] [PubMed] [Google Scholar]
- [6].Wenyu Z, Hailiang Y, Shaodong Y, et al. Factors associated with adherence of highly active antiretroviral therapy among 386 HIV/AIDS patients in 3 provinces of China. Chin J Prev Med 2016;50:335–7. [DOI] [PubMed] [Google Scholar]
- [7].Lifson AR, Workneh S, Hailemichael A, et al. Perceived social support among HIV patients newly enrolled in care in rural Ethiopia. AIDS Care 2015;27:1382–6. [DOI] [PubMed] [Google Scholar]
- [8].Lan KE, Kui H, Shanfang T, et al. Multiple regression analysis of influencing factors related to AIDS drug treatment adherence. Mod J Integr Trad Chin West Med 2011;20:432–3. [Google Scholar]
- [9].Jianzhuo L, Yan J, Hui Y, et al. Influencing factors of drug treatment adherence among patients with HIV /AIDS in Jinan city of China. J Shandong Univ (Health Sci) 2014;52:107–9. [Google Scholar]
- [10].Rui G, Jian-Yong L, Xu W-X. Study on HAART adherence and related influencing factors among HIV/AIDS patients in Jiaxing City. Chin J Dis Control Prev 2015;19:206–7. [Google Scholar]
- [11].Yanxia C, Zhongying L, Xingming L, et al. Medication adherence and influence factors for taking medicine among people living with HIV/AIDS. Chi J AIDS STD 2015;21:268–9. [Google Scholar]
- [12].Jones DL, McPherson-Baker S, Lydston D, et al. Efficacy of a group medication adherence intervention among HIV positive women: the SMART/EST women's project. AIDS Behav 2007;11:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zhoulin L, Guilan C, Wei S, et al. Promote the adherence of the treatment of HIV/AIDS in the treatment of HIV/AIDS. Soft Sci Health 2007;21:414–5. [Google Scholar]
- [14].Raja S, McKirnan D, Glick N. The treatment advocacy program—Sinai: a peer-based HIV prevention intervention for working with African American HIV-infected persons. AIDS Behav 2007;11(suppl):S127–37. [DOI] [PubMed] [Google Scholar]
- [15].China CDC Group. National Free Antiretroviral Treatment for HIV/AIDS. 2012;Beijing: People's Health Publishing House, 141–157. [Google Scholar]
- [16].Shuiyuan X. The theoretical foundation and research applications of “social support scale”. J Clin Psychiatry 1994;4:98–100. [Google Scholar]
- [17].Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet 2013;382:1525–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Remien R, Sturratt M, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS 2005;19:807–14. [DOI] [PubMed] [Google Scholar]
- [19].Jing-Fang C, Hui-Zhen W. Correlation between social supports and medication adherence of AIDS patients. J Nurs 2014;21:1–3. [Google Scholar]
- [20].Yan-Xia C, Zhong-Ying L, Xing-Ming L, et al. Medication adherence and influence factors for taking medications among people living with HIV/AIDS. Chin J AIDS STD 2015;21:268–72. [Google Scholar]
- [21].Aidala AA, Wilson MG, Shubert V, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health 2016;106:e1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Li XM, Yuan XQ, Wang JJ, et al. Evaluation of impact of social support and care on HIV-positive and AIDS individuals’ quality of life: a non randomised community trial. J Clin Nurs 2017;26:369–78. [DOI] [PubMed] [Google Scholar]
- [23].Xiao-Yun S, Yu-Hua R, Hui X. HIV/AIDS patients with highly effective antiretroviral treatment adherence factors. Chin J AIDS STD 2008;14:302–3. [Google Scholar]
- [24].Caifang P. The influence factors and intervention measures of anti viral treatment adherence of AIDS patients. Intern Med China 2014;9:440–1. [Google Scholar]
- [25].Luszczynska A, Sarkar Y, Knoll N. Received social support, self-efficacy, and finding benefits in disease as predictors of physical functioning and adherence to antiretroviral therapy. Patient Educ Couns 2007;66:37–42. [DOI] [PubMed] [Google Scholar]


