Supplemental Digital Content is available in the text
Keywords: bupivacaine, ibuprofen, intracutaneous injection, lidocaine, methylprednisolone, neck pain
Abstract
Acute nonspecific neck pain is one of the major public health problems lacking efficient treatments. The present study was designed to observe the analgesic effect of intracutaneous injection of local anesthestics and steroids on acute nonspecific neck pain.
Thirty-six newly diagnosed with acute nonspecific neck pain patients were randomized to receive ibuprofen (IPB group) or intracutaneous injection of local anesthetics (lidocaine and bupivacaine) and steroid (methylprednisolone) (MLB group). The pain intensity was the primary outcome and evaluated with visual analog scale (VAS). Neck disability index (NDI) and patient global impression of changes (PGIC) were monitored for overall outcomes.
Following treatments, patients from the 2 groups have decreased VAS scores and NDI when compared with their baseline level at 3 hours, day 1, and day 3 time points. Interestingly, the MLB group patients have lower VAS scores and NDI than IPB group. MLB patients also had a greater PGIC than IPB group.
This study indicates that single intracutaneous injection of local anesthetics and steroids is sufficient to alleviate acute nonspecific neck pain.
1. Introduction
Neck pain is a major public health problem with high prevalence and costs in terms of health care expenditures and productivity loss.[1–3] In the general population, lifetime prevalence of neck pain varies widely, from 14% to 71%.[4] Acute neck pain, if not appropriately controlled, may lead to persistent pain, which will last for months, even years. There are currently nonsurgical managements available for neck pain treatment, for example, local massage, physical exercise, and trigger point injection of local anesthetics.[5–10] These physical and minimal invasive therapies are widely used around the world; however, these therapies have shown incomplete or conflicting outcomes[11–17] on neck pain, as there are no standard protocols. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, is widely used for acute neck pain control, though some of the patients do not respond to NISAIDS.[11,12] There has been a pursuit for novel drugs or for more information regarding novel techniques to alleviate acute neck pain.
We recently reported that intracutaneous injections of local anesthetics and steroids were useful interventional strategies to effectively control acute thoracic herpes zoster pain.[13] In the present study, we proposed that intracutaneous injection of local anesthetics and steroids are also effective to alleviate acute nonspecific neck pain by using oral ibuprofen as a positive control.
2. Methods and materials
This study was approved by the Institutional Medical Ethics Committee of the First People's Hospital of Lianyungang and was carried out in accordance with the approved guidelines. Informed consent was obtained from all the subjects. This study was designed as a prospective, randomized, positive-controlled clinical trial from July 2014 to December 2016.
Participants in the study met the following criteria: 18 to 65 years old, experiencing nonspecific neck pain within 72 hours, pain intensity ≥ 4 on the visual analog scale (VAS). Patients were excluded if the neck pain was induced by fracture, carcinoma, infection, neuropathy, or spinal cord diseases; the neck pain was experienced after spinal cord surgery; there is infection at the injection sites; the patient has coagulopathy; the patient has an opioid addiction; the patient is obese [body mass index (BMI) > 30]; the patient has neuropsychiatric diseases or a related treatment history; the patient is pregnant. Patients were instructed in the use of the visual analogue scale (VAS; 0, no pain, to 10, worst possible pain). Post-treatment VAS score is the primary outcome of the study. No important changes to the methods were made after trial commencement.
A total of 42 patients were enrolled into the study; after excluding 6 of them, 36 patients were divided into 2 groups at random using a computer-generated randomized table (Fig. 1): Ibuprofen control (IPB) group and intracutaneous injection of local anesthetics and steroid (MLB) group (Fig. 1). Patients from the 2 groups received oral ibuprofen (oral ibuprofen, 400 mg/day) or intracutaneous injection of local anesthetics and steroid (Methylprednisolone 20 mg, 2 mL of 0.5% bupivacaine, and 2 mL of 2% lidocaine in 0.9% saline solution) into the ipsilateral paravertebral skin and the affected areas (Fig. 2). Six out of these 36 patients reported sitting for a long period of time during the night before treatment, and the rest patients reported no reasons. Pain intensity evaluation and Neck Disability Index were recorded on admission as baselines, and at time-points of 3 hours, 1 day and 3 days following first oral administration of ibuprofen or intracutaneous injection. Patient Global Impression of Change (PGIC) was determined by patient self-evaluation on a 7-point scale (1 = very much improved, 2 = much improved, 3 = minimally improved, 4 = no change, 5 = minimally worse, 6 = much worse, and 7 = very much worse). Positive response was determined by a 50% reduction of baseline VAS.
Figure 1.
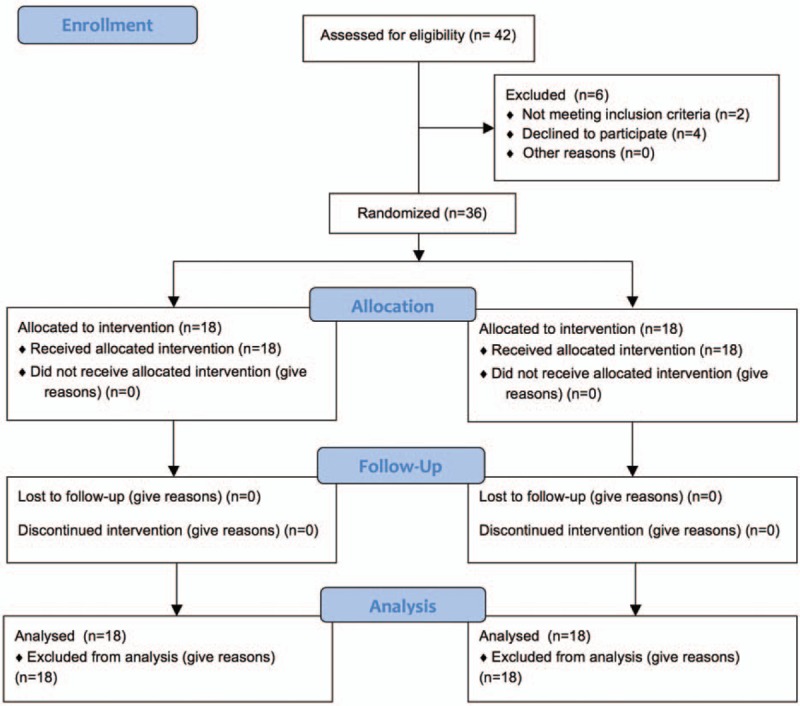
Flow diagram of this study.
Figure 2.

Sample photos showing intracutaneous injections in the paravertebral and affected areas from a 27-year-old male patient and a 22-year-old female patient.
2.1. Statistical analysis
All of the data in the present study were analyzed with the GraphPad Prism software, version 7.0, (GraphPad Software Inc., San Diego, CA). Parameters such as age and onset time were compared between the 2 groups using the unpaired t test. Normality of the scoring data was statistically tested by the D’Agostino-Pearson omnibus normality test. Scoring data at different time points within 1 group were compared with between the 2 groups by 1-way or 2-way analysis of variance (ANOVA), followed by Bonferroni post-test. These data were also presented as median along with the first (Q25) and third (Q75) quartiles followed by the [minimum, maximum] in the supplementary file, and were compared by using a Wilcoxon rank sum test. Adverse effects were analyzed with Fisher test. All data with P < .05 were considered statistically significant.
3. Results
3.1. Demographic characteristics
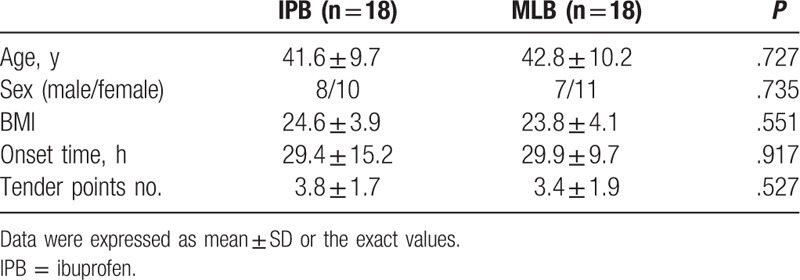
Both groups were similar with respect to demographic data and baseline pain statement (P > .05). These data are presented in Table 1 in details.
Table 1.
Demographic data.
3.2. Pain intensity measurement
On admission, the baseline VAS scores of patients from both groups were comparable (Table 1). Patients receiving oral ibuprofen and intracutaneous injection of local anesthetics and steroid both shown reduced VAS score at all of the selected time-points (Fig. 3 A and B, at time point of 3-hour, 1-day, and 3-day time-points, ∗∗∗P < .001; and also see supplementary table 1, 2); however, those from the MLB group had a lower VAS than their control patients from IPB group (Fig. 3C, at time point of 3-hour, 1-day, and 3-day time-points, ∗∗∗P < .001, ∗P < .05; and also see supplementary table 3).
Figure 3.
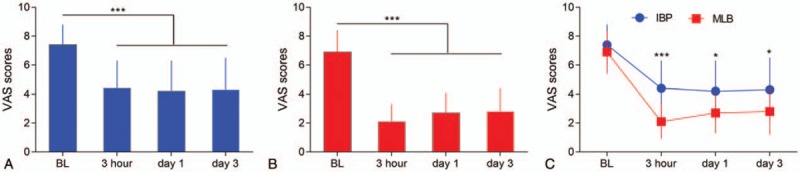
VAS scores from the 2 groups at different time points. (A) IBP group: VAS scores comparison between the baseline value and that at time point of 3-h, 1-day, and 3-day time-points, ∗∗∗P < .001. (B) MLB group: VAS scores comparison between baseline value and that at 3-h, 1-day, and 3-day time-points, ∗∗∗P < .001. (C) VAS scores comparison between the IBP and MLB groups at different time points (at time point of 3-h, 1-day, and 3-day time-points, ∗∗∗P < .001, ∗P < .05).
3.3. NDI measurement
On admission, the baseline NDI of patients from both groups were comparable (Table 1). Patients receiving oral ibuprofen and intracutaneous injection of local anesthetics and steroid both shown reduced NDI at all of the selected time-points (Fig. 4 A and B, at time point of 3-hour, 1-day, and 3-day time-points, ∗∗∗P < .001; and also see supplementary table 4, 5), and those from the MLB group had a lower NDI than their control patients from IPB group (Fig. 4C, at time point of 3-hour, 1-day, and 3-day time-points, ∗∗∗P < .001, ∗P < .05; and also see supplementary table 6).
Figure 4.
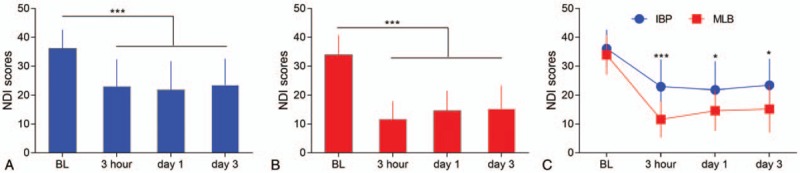
NDI scores from the 2 groups at different time points. (A) IBP group: NDI scores comparison between baseline value and that at time point of 3-h, 1-day, and 3-day time-points, ∗∗∗P < .001. (B) MLB group: NDI scores comparison between baseline value and that at 3-h, 1-day, and 3-day time-points, ∗∗∗P < .001. (C) NDI scores comparison between the IBP and MLB groups at different time points (at time point of 3-h, 1-day, and 3-day time-points, ∗∗∗P < .001, ∗P < .05).
3.4. Responsive rates and PGIC measurements
A responsive rate was determined by a 50% reduction of baseline VAS. More patients from the MLB group respond to the treatment they received (Fig. 5A, ∗∗P < .01). Patients self-evaluation on day 3 indicated a lower PGIC in patients from the MLB group when compared with those from the IPB group (Fig. 5B, ∗∗P < .01, and also see supplementary table 7).
Figure 5.
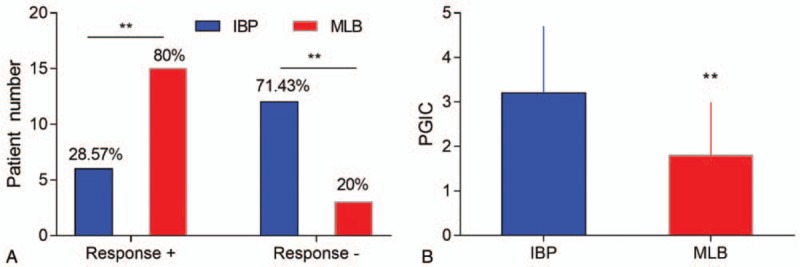
Responsive rates and patient global impression of changes. (A) Responsive rates comparison between the 2 groups (∗∗P < .01). (B) PGIC comparison between the 2 groups (∗∗P < .01).
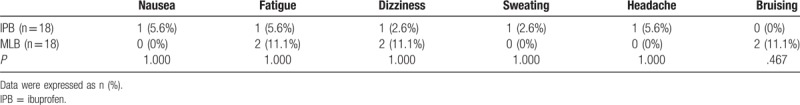
3.5. Adverse effects
With respect to the adverse effect, no significant difference was observed between the 2 groups (Table 2).
Table 2.
Adverse events.
4. Discussion
The present study demonstrates that intracutaneous injection of local anesthetics and steroid into the affected skin area and the paravertebral area is sufficient to relieve acute nonspecific neck pain. And the analgesic effect is more potent than that generated from oral administration of ibuprofen.
Neck pain is a major public health problem with a high lifetime prevalence[1–3] varying widely from 14% to 71%.[4] Early control of this acute neck pain will prevent its development into a long-lasting persistent pain. Local massage and physical exercise are 2 currently used treatments for neck pain[5–8]; however, these therapies have shown incomplete or conflicting outcomes as a result of a lack of standard protocols. Trigger point injection, such as local intramuscular injection of local anesthetics or saline, was also used for neck pain treatment. For our experience, neck pain affects a vague area, and it is hard to locate all of the trigger points. Some patients need a second injection because of insufficient analgesia. Oral analgesic, such as NSAIDs, is another widely accepted strategy for acute neck pain control, though some of the patients do not respond to NSAIDs.[11,12] In clinical practice, a combined strategy has been employed to treat acute neck pain for the ineffectiveness of a single treatment alone. Meanwhile, there is an urgent pursuit for novel techniques to alleviate acute neck pain.
Intracutaneously injecting a mixture of local anesthetics and/or steroid has been implicated in controlling hyperalgesia in in previous clinical studies.[13–15] We recently reported that intracutaneous injection of local anesthetics and steroids was a useful interventional strategy to potently control acute thoracic herpes zoster pain.[13] In the present study, we further found that intracutaneous injection of local anesthetics and steroids was also effective to alleviate acute neck pain, by using oral ibuprofen as a positive control. Together with this study, we believe that intracutaneous injection of local anesthetics and steroids can be a novel strategy for different kinds of acute pain control, and our future study will employ and generalize this treatment in acute pain management. Moving disability induced by neck pain greatly impacts daily life quality.[16] We also observed that this intracutaneous injection robustly improved neck disability, even when compared with their positive control patients. Our data showed on the first 1 to 2 days following the injection, acute neck pain was remarkably alleviated; then, the patients would experience a 1 to 2 weeks slow recovery. However, we only observed the analgesic effects for 3 days but did not monitor the long-term effects.
To evaluate the overall effect of intracutaneous injection of local anesthetics and steroid mixture on acute neck pain, 2 separate methods were used to measure the responding rate of analgesic effects by anesthesiologist, and general impression on the treatment by patients themselves. These objective and subjective evaluations further confirmed the analgesic and overall effects of intracutaneous injection of local anesthetics and steroid on acute neck pain. These data indicated that intracutaneous injection of local anesthetics and steroid mixture was sufficient to control acute nonspecific neck pain.
A concern should be taken in consideration is that controlling acute pain without accurate diagnosis is dangerous because this will cover up the real pain reason, for example, in patients with abdominal pain as well as those with neck pain though at a lower incidence. Although we believe that, not like abdominal pain, the reasons of specific acute neck pain could be easily found, sufficient physical and radiological examinations are needed before application of this treatment.
Local intracutaneous injections, including sterile saline, local anesthetics, steroids, or combinations of drugs, have been implicated in treating different kinds of chronic or acute pain state[17–20]; however, the underlying mechanisms remained largely unknown. In this study, we injected less than 0.5 mL into each injection site. This small volume may not able to diffuse to the affected areas far away from the injection site. It has been reported that more sensory neural fibers were distributed in the skin than in deep tissues, so it could be a blockade of local sensory C-fiber terminals and anti-inflammatory effects of the mixture.[13] And the exact mechanisms underlying this potent and long-lasting analgesic effect also need further investigations.
There are limitations in the present study. This is a single-center study; it is hard to generalize the findings; and it holds a small sample size; as the technique is invasive, it is difficult to accept for some of the patients. The present study recorded the analgesic effect of the treatment for only 3 days. Further observation is needed to see whether this effect could last for an even longer period, although 3 days is considered a long-term effect for single injection.
Overall, this randomized controlled clinical study reported that intracutaneous injection of local anesthetics and steroid is effective to treat acute neck pain. This study will provide useful information and potential guidance for future control of acute nonspecific neck pain.
Author contributions
Conceptualization: Xiao-Na Yang, Zhu-Sheng Geng, Yun-Hai Zhang.
Data curation: Zhu-Sheng Geng, Yun-Hai Zhang.
Project administration: Xin-Ling Wang, Xiao-Bao Zhang.
Supervision: Ji-Zheng Cui.
Validation: Xiao-Bao Zhang.
Writing – original draft: Xiao-Na Yang, Zhu-Sheng Geng, Xiu-Li Zhang.
Writing – review & editing: Ji-Zheng Cui.
Supplementary Material
Footnotes
Abbreviations: IPB = ibuprofen, NDI = Neck disability index, NSAIDs = nonsteroidal anti-inflammatory drugs (NSAIDs), PGIC = patient global impression of changes, VAS = visual analog scale.
XY, ZSG, and XLZ contributed equally to the present study.
Funding/support: This work was funded by Youth Talent Haosen Fund Project (NQ150201).
All authors declared that there was no conflict of interest exists.
The author(s) of this work have nothing to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [DOI] [PubMed] [Google Scholar]
- [2].Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hansson EK, Hansson TH. The costs for persons sick-listed more than one month because of low back or neck problems. A two-year prospective study of Swedish patients. Eur Spine J 2005;14:337–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J 2006;15:834–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sherman KJ, Cook AJ, Wellman RD, et al. Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain. Ann Fam Med 2014;12:112–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sherman KJ, Cherkin DC, Hawkes RJ, et al. Randomized trial of therapeutic massage for chronic neck pain. Clin J Pain 2009;25:233–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Goode AP, Freburger J, Carey T. Prevalence, practice patterns, and evidence for chronic neck pain. Arthritis Care Res (Hoboken) 2010;62:1594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Harvey N, Cooper C. Physiotherapy for neck and back pain. BMJ 2005;330:53–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Liu L, Huang QM, Liu QG, et al. Effectiveness of dry needling for myofascial trigger points associated with neck and shoulder pain: a systematic review and meta-analysis. Arch Phys Med Rehabil 2015;96:944–55. [DOI] [PubMed] [Google Scholar]
- [10].Xie P, Qin B, Yang F, et al. Lidocaine injection in the intramuscular innervation zone can effectively treat chronic neck pain caused by MTrPs in the Trapezius muscle. Pain Physician 2015;18:E815–26. [PubMed] [Google Scholar]
- [11].Peloso PM, Khan M, Gross AR, et al. Pharmacological interventions including medical injections for neck pain: an overview as part of the ICON Project. Open Orthop J 2013;7:473–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].McCarberg B, D’Arcy Y. Options in topical therapies in the management of patients with acute pain. Postgrad Med 2013;125:19–24. [DOI] [PubMed] [Google Scholar]
- [13].Cui JZ, Zhang XB, Zhu P, et al. Effect of repetitive intracutaneous injections with local anesthetics and steroids for acute thoracic herpes zoster and incidence of postherpetic neuralgia. Pain Med 2017;18:1566–72. [DOI] [PubMed] [Google Scholar]
- [14].Savastano M, Ferraro SM, Marioni G. Perichondritis with or without external otitis and intradermal injection: a new therapeutic approach. J Otolaryngol Head Neck Surg 2009;38:568–72. [PubMed] [Google Scholar]
- [15].Tschopp KP, Gysin C. Local injection therapy in 107 patients with myofascial pain syndrome of the head and neck. ORL J Otorhinolaryngol Relat Spec 1996;58:306–10. [DOI] [PubMed] [Google Scholar]
- [16].Billeci D, Coluzzi F. Tapentadol extended release for the management of chronic neck pain. J Pain Res 2017;10:495–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cui JZ, Geng ZS, Zhang YH, et al. Effects of intracutaneous injections of sterile water in patients with acute low back pain: a randomized, controlled, clinical trial. Braz J Med Biol Res 2016;49:pii: S0100-879X2016000300704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sim HL, Tan KY. Randomized single-blind clinical trial of intradermal methylene blue on pain reduction after open diathermy haemorrhoidectomy. Colorectal Dis 2014;16:O283–7. [DOI] [PubMed] [Google Scholar]
- [19].Kankel J, Obreja O, Kleggetveit IP, et al. Differential effects of low dose lidocaine on C-fiber classes in humans. J Pain 2012;13:1232–41. [DOI] [PubMed] [Google Scholar]
- [20].Oman KS, Fink R, Kleiner C, et al. Intradermal lidocaine or bacteriostatic normal saline to decrease pain before intravenous catheter insertion: a meta-analysis. J Perianesth Nurs 2014;29:367–76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


