Abstract
This retrospective study investigated the effect and safety of extracorporeal shockwave therapy (ESWT) for treatment of knee osteoarthritis (KOA).
In this retrospective study, 105 patients with KOA were included. Of those, 60 patients underwent ESWT, whereas 45 patients received laser therapy. Effect was measured by the Numeric Rating Scale (NRS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). In addition, adverse events (AEs) were also recorded in this study. All outcome measurements were evaluated at the end of weeks 1, 6, and 12.
Compared with the laser therapy, ESWT showed greater effect in KOA symptoms relief with regard to NRS, WOMAC total, and its subscores at week 6 (P < .05) and week 12 (P < .01) after treatment. No AE, however, occurred in both groups.
The results of this retrospective study found that ESWT may be efficacious and safe for the treatment of patients with KOA. It, however, had an intrinsic limitation as a retrospective study. Prospective study with larger sample size is still needed to warrant the result of this study in the future.
Keywords: effect, extracorporeal shockwave therapy, knee osteoarthritis, safety
1. Introduction
Knee osteoarthritis (KOA) is one of the disabling joint disease of advanced age.[1–3] It often results in the knee pain, stiffness, restricted movement, sleep disturbance, and even poor quality of life and psychological disability.[4–6] The progressive aging of the population has also caused to the increase in the incidence and prevalence of KOA, and such condition has become a major public health issue.[7,8] It has been reported that 9.6% of men and 18% of women have symptomatic KOA at the age of 60 years and above.[9] In addition, approximately 25% population older than 55 years have reported at least 1 attack of knee pain each year,[10] and approximately 13% of older population have diagnosed as having KOA over the 7 years.[11]
As for treatment, pharmacological therapy often has limited benefit for KOA pain relief.[12] Furthermore, the use of pharmacological drugs is often associated with serious adverse events (AEs), including bleeding and gastrointestinal ulcers.[13] Complementary therapies, such as local injection,[14,15] acupuncture,[16,17] moxibustion,[18] cupping therapy,[19] exercise,[20] and laser therapy[21] are also used to treat KOA. They are, however, not sufficient to control chronic, severe KOA pain. Although surgery is generally effective for the treatment of patients with advanced KOA,[22] some older patients with limiting comorbidities may not be able to undergo such intervention appropriately. In such conditions, extracorporeal shockwave therapy (ESWT) might be a successful alternative treatment in patients with KOA with few complications.[23] ESWT is a nonsurgical and noninvasive intervention by using shock waves outside the body, especially for patients who cannot be treated by anti-inflammatory or immobilization devices. This quick effective intervention is often used to treat many chronic painful orthopedic conditions.
It has been reported that ESWT can be used to treat patients with KOA.[23] Limited data on the ESWT for the treatment of KOA are, however, available. Thus, more studies are still needed to explore the effect and safety of ESWT on the treatment of KOA. In this retrospective study, we investigated the effect and safety of ESWT for the treatment in patients with KOA, compared with laser therapy.
2. Materials and methods
2.1. Ethics
This study was formally approved by the ethics committee of The First Hospital of Harbin City, The First Affiliated Hospital of Harbin Medical University, and The Fourth Affiliated Hospital of Harbin Medical University. All patients provided the informed consent.
2.2. Design
This retrospective study included 105 patients with KOA. They were assigned to an ESWT therapy group and a laser therapy group according to the different interventions they received. Sixty patients underwent ESWT and were assigned to the ESWT therapy group, whereas 45 patients received laser therapy and were assigned to the laser therapy group. Patients in both groups were treated for 12 weeks. All outcomes were measured at the end of 1-, 6-, and 12-week treatment.
2.3. Eligibility criteria
This retrospective study was also conducted at these 3 hospitals between January 2015 and December 2016. All 105 patients were diagnosed with KOA. In addition, the inclusion criteria included the following: patients had >6 months history of KOA and pain intensity was >4, measured by Numeric Rating Scale (NRS). The exclusion criteria included patients had history of knee surgery, tumors, or they received ESWT or laser therapy 1 month before this study.
2.4. Interventions
Sixty patients with KOA underwent ESWT with 3000 pulses of 0.11 mJ/mm2 at a frequency of 15 Hz by using the Pain Treatment System of Radial Shockwave Device (Sonothera, Hanil TM Co. Ltd, Wonju-si, Gangwon-do, Korea). All patients presented in a supine position with affected knee unbent. The shockwave probe was applied to the trigger point around the attacked knee. All patients were treated for 5 sessions with an interval of 3 days for a total of 12 weeks. Forty-five patients received laser therapy. The calibrated laser device (Standard Class 3B; Stockholm, Sweden) was used to treat patients with KOA. It applied over the joint line with 5 points of synovial region of the medial side. In addition, 4 points at the lateral side were also applied. The measurement output energy was 0.2 J/point for a total dose of 20 J each treatment per knee.
2.5. Outcome measurements
The outcomes measured by the 11-point NRS[24] and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).[25] The NRS tool ranges from 0 to 10, with 0 as no pain, and 10 as the worst pain. The WOMAC tool includes 24 items, and it is divided into 3 subscales to evaluate the pain, stiffness, and physical function. The subscale of pain with 5 items ranges from 0 to 20, with 0 as no pain, and 20 as the worst pain. The subscale of stiffness with 2 items varies from 0 to 8, with 0 as no pain, and 20 as the worst pain. The subscale of physical function with 17 items ranges from 0 to 68. In addition, AEs were also recorded in this study. We assessed and analyzed the outcome data of NRS and WOMAC at the end of 1, 6, and 12 weeks. In addition, we analyzed the data of AEs at the end of 12-week treatment.
2.6. Statistical analysis
All data were analyzed using the Statistical Package for the Social Sciences software v.19.0 (SPSS Inc, Chicago, IL). The continuous variable data at baseline, and NRS and WOMAC scores were analyzed by t test (normally distributed data) or Mann-Whitney rank sum test (not normally distributed data) at the end of 1-, 6-, and 12-week treatment. The categorical data at baseline were analyzed by Pearson chi-square test. Two-sided P values of <.05 were regarded as the statistical significance.
3. Results
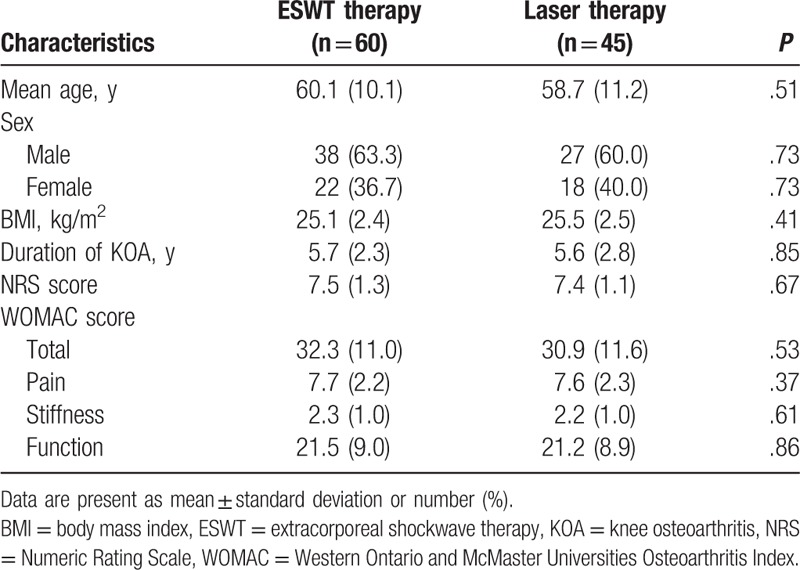
The characteristics of 105 included patients with KOA are summarized in Table 1. No significant differences of characteristic values were found at baseline between 2 groups (Table 1). These characteristics consisted of age, sex, body mass index, duration of KOA, NRS score, WOMAC total, and its subscores.
Table 1.
Characteristics of included patients.
At baseline, the NRS scores by ESWT therapy and laser therapy were 7.5 ± 1.3 and 7.4 ± 1.1, respectively (Table 1). After 1 week, the NRS scores by each therapy were 6.9 ± 1.5 and 7.0 ± 1.4, respectively (Fig. 1). After 6 weeks, they were 5.0 ± 1.7 and 6.7 ± 1.8, and after 12 weeks, they were 2.8 ± 1.4 and 6.4 ± 1.6, respectively (Fig. 1). There were significant differences between the 2 therapies at weeks 6 (P < .01) and weeks 12 (P < .01) (Fig. 1).
Figure 1.
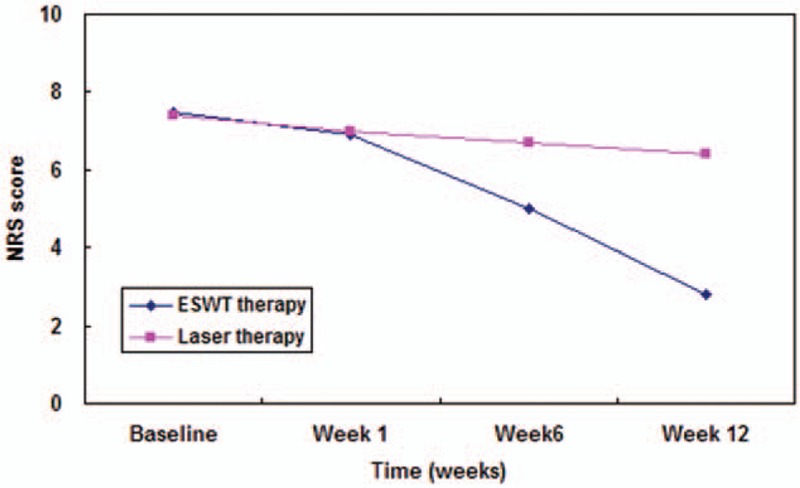
Comparison of NRS scores between 2 therapies. ESWT = extracorporeal shockwave therapy, NRS = Numeric Rating Scale.
At baseline, the WOMAC total scores by ESWT therapy and laser therapy were 32.3 ± 11.0 and 30.9 ± 11.6, respectively (Table 1). After 1 week, the total WOMAC scores by the 2 therapies were 29.5 ± 11.3 and 29.7 ± 11.8, respectively; after 6 weeks, they were 21.5 ± 10.5 and 28.6 ± 12.1, respectively; and after 12 weeks, they were 16.9 ± 9.1 and 27.2 ± 10.9, respectively (Fig. 2). There were also significant differences between the 2 therapies at week 6 (P < .01) and week 12 (P < .01) (Fig. 2).
Figure 2.
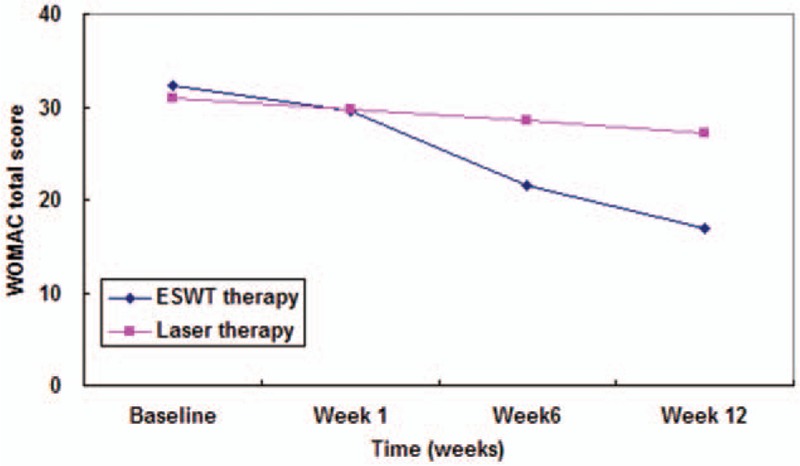
Comparison of WOMAC total scores between 2 therapies. ESWT = extracorporeal shockwave therapy, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
The WOMAC subscores of pain, stiffness, and function by 2 therapies were 7.7 ± 2.2, 2.3 ± 1.0, 21.5 ± 9.0 and 7.6 ± 2.3, 2.2 ± 1.0, 21.2 ± 8.9, respectively (Table 1). After 1 week, WOMAC subscores for the 2 therapies were 7.1 ± 2.3, 2.1 ± 0.9, 20.3 ± 9.4 and 7.2 ± 2.3, 2.1 ± 1.0, 20.6 ± 9.1, respectively (Figs. 3–5). After 6 weeks, they were 1.4 ± 0.8, 2.3 ± 1.0, 15.1 ± 8.3 and 6.8 ± 2.5, 2.0 ± 0.9, 19.9 ± 9.4, respectively (Figs. 3–5); after 12 weeks, they were 3.0 ± 2.1, 1.0 ± 0.7, 12.8 ± 6.9 and 6.5 ± 2.4, 1.8 ± 0.8, 19.6 ± 8.0, respectively (Figs. 3–5).
Figure 3.
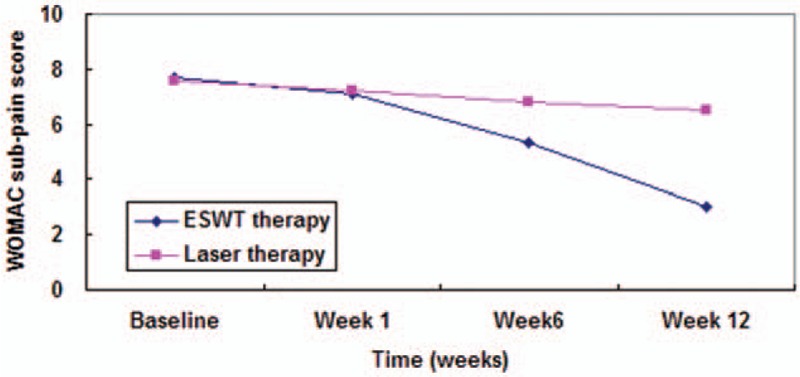
Comparison of WOMAC subpain scores between 2 therapies. ESWT = extracorporeal shockwave therapy, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
Figure 5.
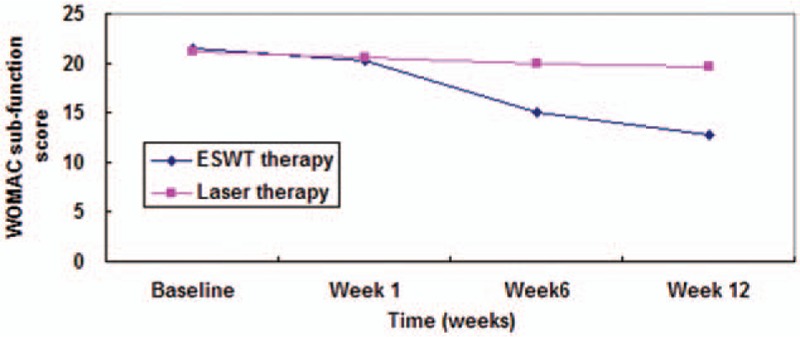
Comparison of WOMAC subfunction scores between 2 therapies. ESWT = extracorporeal shockwave therapy, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
Figure 4.
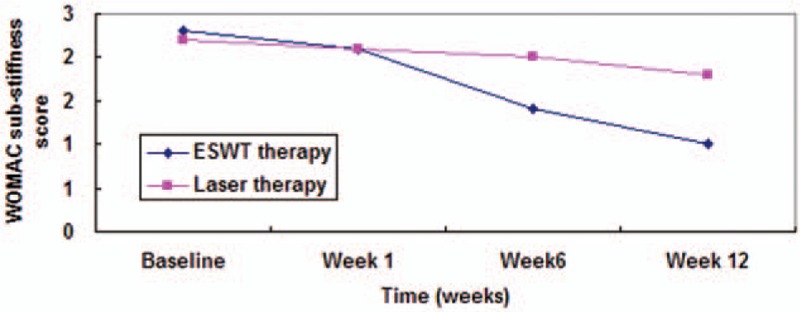
Comparison of WOMAC substiffness scores between 2 therapies. ESWT = extracorporeal shockwave therapy, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
As for safety, no AE was recorded by any of the therapies during the study period.
4. Discussion
Several animal studies and clinical studies investigated the mechanism, efficacy, and safety of ESWT for the KOA. Ochiai et al[26] explored the effect ESWT on KOA in a rat knee model. The results showed that the enhancement in walking ability and the decreased expression of calcitonin gene-related peptide in dorsal root ganglion neurons indicating that ESWT is an useful intervention for KOA.[26] Zhao et al[27] investigated the mechanism of ESWT for KOA in rabbits by reducing nitric oxide (NO) level and chondrocyte apoptosis. Its results demonstrated that ESWT can significantly reduce the level of NO in the synovial cavity of knee joints, and can decrease the chondrocyte apoptosis in rabbits with KOA.[27] It indicates that ESWT can decrease the progression of KOA in rabbits, and may be used as a useful treatment for KOA.[27] Zhao et al[23] also evaluated the efficacy of ESWT for patients with KOA during 12 weeks when compared with placebo. They found that ESWT is efficacious in decreasing pain and enchaining knee function during the 12-week treatment.[23] Kim et al[28] investigated the dose-related effects of ESWT in Korean patients with KOA. Their results showed that medium-energy ESWT had greater improvement in pain relief and function restoration than the low-energy ESWT.[28] Imamura et al[29] explored the efficacy and safety of radial ESWT (rESWT) for Brazilian patients with disabling pain due to the primary KOA. Its results demonstrated that rESWT is not efficient for the treatment in patients with disabling pain due to the primary KOA.[29] The data indicate that higher energy of rESWT may be useful for treating patients with such condition.[29]
Although several previous studies have investigated the efficacy and safety of ESWT for treating patients with KOA, 2 of them focused on the animal studies, and only 1 study included Chinese patients with small sample size. To our best knowledge, this study is the first retrospective research to explore the effect and safety of ESWT in patients with KOA among Chinese population. The results of this study found that ESWT showed promising effect and satisfied safety for the treatment of patients with KOA, compared with the laser therapy.
In this study, the knee pain associated with KOA, measured by the NRS score, and subscale of WOMAC, was significantly relieved by utilizing ESWT, compared with laser therapy. The knee stiffness and function, both measured by the subscales of WOMAC also improved greatly in patients among Chinese population. Moreover, no treatment-related AEs were recorded in both groups in our study.
This study has the following limitations: sample size was relative small in this study, which affected its results; only single dose of ESWT was used in this study; therefore, optimal doses of ESWT should be focused in further study; this study did not evaluate the quality of life in patients with KOA, because it just analyzed the outcome data based on the available completed cases of the included patients; and this study had an intrinsic limitation because it is a retrospective study, which may affect the results of this study. Thus, future studies should include comprehensive outcome measurements, including quality of life measurement.
5. Conclusion
This study found that ESWT may be efficacious and safety for patients with KOA. It, however, suffered from an intrinsic limitation as a retrospective study. Thus, future prospective study with larger sample size should further warrant the results of this study.
5.1. Uncited reference
[3]
Author contributions
Conceptualization: Qinggang Meng, Wei Li, Yu Pan, Zheng-gui Guo, Qi Yue.
Data curation: Wei Li, Zheng-gui Guo.
Formal analysis: Yu Pan, Qi Yang.
Investigation: Qi Yang, Qi Yue.
Methodology: Yu Pan, Qi Yang.
Project administration: Yu Pan.
Resources: Qinggang Meng, Wei Li.
Software: Qi Yang, Qi Yue.
Supervision: Qi Yue.
Validation: Wei Li, Zheng-gui Guo.
Visualization: Zheng-gui Guo.
Writing – original draft: Qinggang Meng, Wei Li, Yu Pan, Qi Yang, Zheng-gui Guo, Qi Yue.
Writing – review and editing: Qinggang Meng, Wei Li, Yu Pan, Qi Yang, Zheng-gui Guo, Qi Yue.
Footnotes
Abbreviations: AE = adverse events, ESWT = extracorporeal shockwave therapy, KOA = knee osteoarthritis, NO = nitric oxide, NRS = Numeric Rating Scale, rESWT = radial ESWT, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
WL and YP contributed equally to this work.
This study was funded by grants from the Science and Technology Talents Program of Harbin (2017RAQXJ179, 2017RAXQJ043), Post Doctoral Fund (160780), and Heilongjiang Natural Science Foundation (QC2016102, H2016002).
The authors have no conflicts of interest to disclose.
References
- [1].Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil 2006;85:S2–14. [DOI] [PubMed] [Google Scholar]
- [2].Deveza LA, Melo L, Yamato TP, et al. Knee osteoarthritis phenotypes and their relevance for outcomes: a systematic review. Osteoarthritis Cartilage 2017;25:1926–41. [DOI] [PubMed] [Google Scholar]
- [3].Xing F, Lu B, Kuang MJ, et al. A systematic review and meta-analysis into the effect of lateral wedge arch support insoles for reducing knee joint load in patients with medial knee osteoarthritis. Medicine (Baltimore) 2017;96:e7168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Herrero-Beaumont G, Roman-Blas JA, Bruyère O, et al. Clinical settings in knee osteoarthritis: pathophysiology guides treatment Maturitas 2017;96:54–7. [DOI] [PubMed] [Google Scholar]
- [5].Sliepen M, Brandes M, Rosenbaum D. Current physical activity monitors in hip and knee osteoarthritis: a review. Arthritis Care Res (Hoboken) 2017;69:1460–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ondrésik M, Azevedo Maia FR, Da Silva Morais A, et al. Management of knee osteoarthritis. Current status and future trends. Biotechnol Bioeng 2017;114:717–39. [DOI] [PubMed] [Google Scholar]
- [7].Silverwood V, Blagojevic-Bucknall M, Jinks C, et al. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage 2015;23:507–15. [DOI] [PubMed] [Google Scholar]
- [8].Nicolson PJA, Bennell KL, Dobson FL, et al. Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: a systematic review and meta-analysis. Br J Sports Med 2017;51:791–9. [DOI] [PubMed] [Google Scholar]
- [9].Bedson J, Jordan K, Croft P. The prevalence and history of knee osteoarthritis in general practice: a case-control study. Fam Pract 2015;22:103–8. [DOI] [PubMed] [Google Scholar]
- [10].Peat G, McCarney RP, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001;60:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jordan KP, Joud A, Bergknut C, et al. International comparisons of the consultation prevalence of musculoskeletal conditions using population-based healthcare data from England and Sweden. Ann Rheum Dis 2014;73:212–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Manjhi J, Gupta M, Sinha A, et al. Effects of Balsamodendron mukul gum resin extract on articular cartilage in papain-induced osteoarthritis. Altern Ther Health Med 2016;22:50–8. [PubMed] [Google Scholar]
- [13].Gutthann SP, Garcia Rodriguez LA, Raiford DS. Individual nonsteroidal antiinflammatory drugs and other risk factors for upper gastrointestinal bleeding and perforation. Epidemiology 1997;8:18–24. [DOI] [PubMed] [Google Scholar]
- [14].Bhandari M, Bannuru RR, Babins EM, et al. Intra-articular hyaluronic acid in the treatment of knee osteoarthritis: a Canadian evidence-based perspective. Ther Adv Musculoskelet Dis 2017;9:231–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nguyen C, Rannou F. The safety of intra-articular injections for the treatment of knee osteoarthritis: a critical narrative review. Expert Opin Drug Saf 2017;16:897–902. [DOI] [PubMed] [Google Scholar]
- [16].Zhang Q, Yue J, Sun Z, et al. Acupuncture for chronic knee pain: aprotocol for an updated systematic review. BMJ Open 2016;6:e008027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Huh JE, Seo BK, Lee JW, et al. Analgesic effects of diluted bee venom acupuncture mediated by (-opioid and (2-adrenergic receptors in osteoarthritic rats. Altern Ther Health Med 2018;24:28–35. [PubMed] [Google Scholar]
- [18].Li A, Wei ZJ, Liu Y, et al. Moxibustion treatment for knee osteoarthritis: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Li JQ, Guo W, Sun ZG, et al. Cupping therapy for treating knee osteoarthritis: the evidence from systematic review and meta-analysis. Complement Ther Clin Pract 2017;28:152–60. [DOI] [PubMed] [Google Scholar]
- [20].Zhang Y, Huang L, Su Y, et al. The effects of traditional Chinese exercise in treating knee osteoarthritis: a systematic review and meta-analysis. PLoS One 2017;12:e0170237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Huang Z, Chen J, Ma J, et al. Effectiveness of low-level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 2015;23:1437–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Steinhaus ME, Christ AB, Cross MB. Total knee arthroplasty for knee osteoarthritis: support for a foregone conclusion? HSS J 2017;13:207–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zhao Z, Jing R, Shi Z, et al. Efficacy of extracorporeal shockwave therapy for knee osteoarthritis: a randomized controlled trial. J Surg Res 2013;185:661–6. [DOI] [PubMed] [Google Scholar]
- [24].Bellamy N, Carette S, Ford PM, et al. Osteoarthritis antirheumatic drug trials: III, setting the delta for clinical trials: results of a consensus development (Delphi) exercise. J Rheumatol 1992;19:451–7. [PubMed] [Google Scholar]
- [25].Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain 2002;100:55–64. [DOI] [PubMed] [Google Scholar]
- [26].Ochiai N, Ohtori S, Sasho T, et al. Extracorporeal shock wave therapy improves motor dysfunction and pain originating from knee osteoarthritis in rats. Osteoarthritis Cartilage 2007;15:1093–6. [DOI] [PubMed] [Google Scholar]
- [27].Zhao Z, Ji H, Jing R, et al. Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Arch Orthop Trauma Surg 2012;132:1547–53. [DOI] [PubMed] [Google Scholar]
- [28].Kim JH, Kim JY, Choi CM, et al. The dose-related effects of extracorporeal shock wave therapy for knee osteoarthritis. Ann Rehabil Med 2015;39:616–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Imamura M, Alamino S, Hsing WT, et al. Radial extracorporeal shock wave therapy for disabling pain due to severe primary knee osteoarthritis. J Rehabil Med 2017;49:54–62. [DOI] [PubMed] [Google Scholar]


