Abstract
Suicide is the outcome of the interaction of biological, personal, and social risk factors. The purpose of this study was to verify the effects of strain due to individual risk factors and social risk factors on suicidality, and the mediating effect of depressive symptoms in relationship between strain related to individual risk factors and social risk factors and suicidality. The data from sociopsychological anxiety survey of Korea society conducted by the Korea Institute for Health and Social Affairs in 2015 were used in verifying the model. We analyzed the data of 7000 adults aged 19 to 79 years using Structural Equation Modeling. Strain due to individual risk factors was positively related to depressive symptoms and suicidality. Interestingly, strain induced by social risk factors was positively associated with depressive symptoms and suicidality. Social support is significantly associated with depressive symptoms and suicidality. Depressive symptoms directly affected suicidality. In addition, strain due to individual risk factors and social risk factors indirectly affected suicidality mediating depressive symptoms. These findings suggest that not only individual efforts such as social interaction and depression prevention but also government efforts such as preparation for aging may be needed to decrease suicide rate.
Keywords: depression, individual risk factors, KIHASA, population-based study, social risk factors, structural sequence modeling, suicidality
1. Introduction
Numerous studies have focused on individual risk factors in understanding suicide.[1–3] However, suicide is the result of interactions of biological, individual, and social risk factors in addition to absence of protective factors such as social support.[4] On the basis of this assumption, Zhang[5] suggested that various strain factors influence directly suicide, and that strain factors affect indirectly suicide-mediating psychiatric disorders such as depression. In addition, the author emphasized that social and psychological protective factors involve in the process of strain factors inducing suicide.
Psychiatric disorders such as depression and anxiety disorder are important predictors of suicide and reflect the biological vulnerability of suicide.[6,7] In particular, depression was the most proximal and the strongest predictor of adult suicide in many studies.[8–10]
Individual risk factors such as interpersonal problems and economic difficulties along with depression are major predictors of suicide. Persistent stress due to individual risk factors may increase depressive symptoms and, as a result, may lead to suicidal thoughts and suicide attempts.[3] Previous studies have tended to focus on individual risk factors such as economic difficulties, health problems, and interpersonal conflicts.[11,12] However, in order to claim the effects of individual risk factors on depression and suicide more clearly, additional factors such as unemployment, family conflicts, conflicts in the workplace, aging, life safety, and physical health need to be considered.
Previous studies have regarded social risk factors as relatively less important than individual risk factors as predictors of suicide.[13,14] However, social risk factors such as low fertility, population aging, and youth unemployment may increase the strain (or stress) of the social members, and may affect suicidal ideation and suicide attempt.[13] The social risk theory of Taylor-Gooby[15] emphasized the importance of social risk factors in understanding suicide. They divide social risk factors into old social risk factors and new social risk factors. The former assumes that loss of labor related to illness, unemployment, industrial disaster, and poverty in industrial society are the main factors in relation to suicide, whereas the latter focuses on social phenomena after the postindustrial society. In other words, social factors such as changes in family structure, increase in the number of related to female workers, self-employed, temporary position workers, reduction in governmental welfare policy, and population aging are important variables affecting suicide.
In Korea, after the financial crisis in 1997, the unstable working environment of male workers, the increase in the number of female workers with temporary position, the increase of elderly retirement, and youth unemployment rate are becoming social problems. These social risk factors may decrease life satisfaction,[16] which in turn, may affect mental health such as depression and suicide.[17] Indeed, since 2000, the life satisfaction of Korean adults is the lowest among Organization for Economic Cooperation and Development (OECD) member countries,[18] which may be related to maintaining the highest suicide rate among OECD members’ countries.
A few studies have examined the effects of social risk factors on depression and suicide, and they focused on social risk factors such as economic crisis[19,20] and national disaster.[21,22] However, in order to argue for the effects of social risk factors on depression and suicide, various social risk factors such as social safety net, population aging, and conflicts between generations should be considered together.
Another important thing in understanding the effects of individual and social risk factors on depression and suicide is that individual and social risk factors do not have the same impact on all individuals. Previous researches showed that social support may moderate the effects of individual and social risk factors on depressive symptoms and suicide attempt.[11,23] In addition, social support may alleviate strain associated with individual and social risk factors.[9,24] Indeed, in numerous studies, emotional support from family members or interaction support from acquaintance has been found to alleviate stress induced by individual and social risk factors as well as to reduce depressive symptoms and suicidality.[25]
According to previous studies, among sociodemographic variables, gender was clearly associated with depression, and the prevalence of depression in adult women was more than twice that in adult men.[26] On the contrary, the relationship between suicide and gender is complex. Some studies have shown that women experience suicidal ideation more than men.[9] In other studies, suicide attempts rates in male were higher than females.[27]
On the basis of empirical studies and suicide-related theories, this study tested the effects of strain due to individual and social risk factors on suicidality, the indirect effects of strain induced by individual, and social risk factors on suicidality via depressive symptoms.
2. Methods
2.1. Survey and Participants
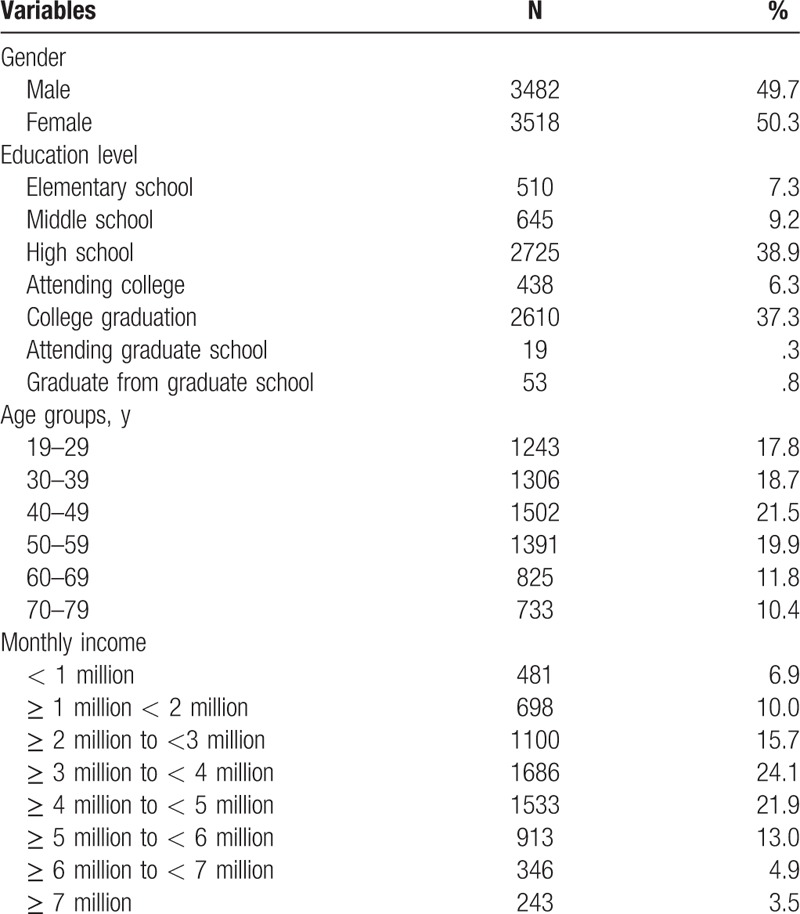
The data from the sociopsychological anxiety survey of Korean society conducted by the Korea Institute for Health and Social Affairs (KIHASA) were used for analysis. The survey was performed in August and September 2015. Two hundred districts were selected from 17 cities and 3552 districts in South Korea by Probabilities Proportional to Size (PPS) method. Sample households were selected through system extraction based on 200 residents’ centers. Considering the ratio of gender, age, and residence area, 7000 people aged 19 to 79 years were sampled using the proportional allocation method. The survey was conducted on a one-on-one basis by trained interviewers visiting the households. The mean age of the participants was 46.55 years (SD = 15.29), and there are 3518 men (50.3%) and 3482 women (49.7%). The specific sociodemographic characteristics of the participants are summarized in Table 1. All participants were informed of the purpose of the survey and signed a consent form. IRB of KIHASA approved the present study.
Table 1.
Sociodemographic characteristics N = 7000.
2.2. Measures
2.2.1. Strain induced by individual risk factors
In order to measure strain due to individual risk factors during the past year, 12 questions of 11-points scale (not at all anxious = 0 to very anxious = 10) developed by KIHASA[28] were used. Twelve questions were asked about employment and income (e.g., unemployment, debt, poverty), preparation for old age (e.g., pensions, savings, assets), life safety (e.g., public security, adult entertainment, unpleasant facilities), physical health (e.g., chronic illnesses, severe illnesses), mental health (e.g., stress, addiction), family relations and dissolution (e.g., family conflict, divorce, separation), child education, family support and care (e.g., education for children, nursing), conflicts in the workplace (e.g., interpersonal relationships, poor working conditions), relationships with neighbors (e.g., conflicts with neighbors, floor noise, parking problems), physical and emotional problems related to aging (e.g., loss of memory, dementia, generation gap, loneliness), invasion of privacy and leakage of private information online (e.g., privacy exposure online, voice phishing), and anxiety about other personal problems. Higher total score is related to higher strain due to individual risk factors. Cronbach alpha for this scale was 0.87.
2.2.2. Strain induced by social risk factors
In order to measure strain due to social risk factors during the past year, 13 items of 11-points scale (not at all anxious = 0 to very anxious = 10) developed by KIHASA[28] were used. Thirteen questions were asked about new infectious diseases (e.g., MERSC, SARS), economic recession and economic stagnation (e.g., lack of jobs, decreased income), safety problems (e.g., nuclear accident, bridge collapse), environmental destruction and natural disasters (e.g., climate change, natural disasters, energy shortages), politics and diplomacy (e.g., North Korea's threats, political instability), mental health problems (e.g., suicide, gambling, alcohol addiction), crime (e.g., sexual violence, murder, robbery), vulnerability to social safety net (e.g., family cosuicide), low fertility and aging (e.g., aging problem and welfare burden), stratum, group and generational conflicts (e.g., conflict between employers and workers, massive strikes, violent protests), frequent changes in education policy and college entrance system (e.g., change in college entrance examinations), leakage of private information online, and anxiety from other social problems. Higher total score is related to greater strain due to social risk factors. Cronbach alpha for this scale was 0.88.
2.2.3. Social support
Five items of 11-point scale (very few = 0 to very many = 10) developed by KIHASA[28] were used. The specific questions are as follows. “How often do you communicate with your family (including social networking and telephone communication)?”, “How often do you communicate with people outside your family (including social networking and telephone communication)?”, “How much do you think you receive social support?”, “How much do you think you can get help if you are in a difficult situation?”, “How many people do you think you can talk with trust?”. Higher total score is associated with greater social support. Cronbach alpha for this scale was 0.85. A confirmatory factor analysis indicated that 2-factor model was superior to 1-factor model. The fit of 2-factor model was good [Chi-square = 39.41, df = 3, P < .001, Goodness of fit index (GFI) = 0.998, Tucker–Lewis Index (TLI) = 0.991, Comparative Fit Index (CFI) = 0.997, root mean squared error of approximation (RMSEA) = 0.042]. First factor is named social interaction support and the other is called emotional support.
2.2.4. Depressive symptoms
Center for Epidemiologic Studies-Depression Scale 11 (CESD-11), which is an abbreviated version of the CESD, was used to measure depressive symptoms. CESD was developed by Radloff[29] and this inventory was commonly used in studies of nonclinical depression. This inventory consists of 11 items of 4-point scale (very rare = 0 to mostly = 3). Higher scores are related to higher level of depression. People with higher score than 16 out of a total 33 are likely to be diagnosed with depression.[30] A confirmatory factor analysis indicated that 4-factor model was superior to 2 and 3-factor model.[31] The fit of 4-factor model was good (Chi-square = 253.68, df = 36, P < .001, GFI = 0.993, TLI = 0.984, CFI = 0.989, RMSEA = 0.029). Each factor was named. Depressed mood was first factor, somatic symptom was second factor, happy emotion was third factor, and interpersonal problem was fourth factor.
2.2.5. Suicidality
Two questions were used to assess suicidal ideation and suicide attempt. “Have you ever thought about death in the last year? (yes or no)”. “Have you ever actually attempted suicide? (yes or no)”. For the analysis, yes was coded as “1” and, no was coded as “0.” These questions were widely used in previous studies.[10,25,32]
2.3. Analysis
Using AMOS 20.0 (AMOS Development Corporation, Crawfordville, FL), we conducted The Confirmatory Factor Analysis of measurement model to verify whether the indicators adequately measured latent construct. Structural equation modeling (SEM) was performed by AMOS 20.0 to verify the fit of the model (Fig. 1). SEM is a strong method of multivariate regression to examine the relationship between variables considering the measurement errors.[33] Dependent variable was suicidality (latent variable), including suicidal ideation and suicide attempt, and predictors include strain due to individual risk factors (observed indicator), strain due to social risk factors with single indicator (observed indicator), social support with two observed indicators (emotional support, social interaction support), and depression with four observed indicators (depressed mood, physical symptoms, happy emotion, interpersonal problem). The normality test showed that SKEW is below 3. Therefore, we used the maximum likelihood estimation. We used the Chi-square GFI, TLI, CFI, RMSEA to verify the fit of the model. Chi-square is likely to accept the null hypothesis because it is very sensitive to sample size.[34] Thus, researchers should consider other indices such as GFI, TLI, CFI, and RMSEA together. GIF, TLI, and CFI are recognized as good if they are higher than 0.95.[35] RMSEA less than 0.08 is acceptable, and 0.05 is considered good.[34] We performed Bootstrap with 200 bootstrap samples to verify the mediating effects of depression between predictors (strain due to individual risk factor and social risk factors) and suicide. Indirect effects are significant if their 95% confidence interval (95% CI) does not include zero.[36]
Figure 1.
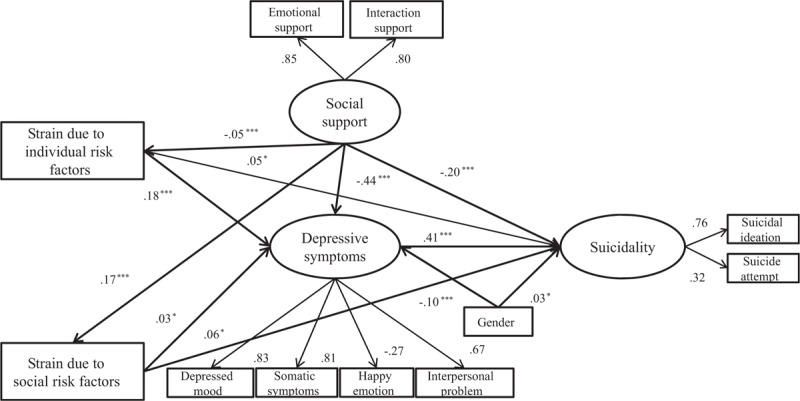
Structural equation modeling.
3. Results
3.1. Confirmatory Factor Analysis
The fit of the measurement model was good: Chi-square (26, N = 7000) = 187.07, P < .001, GFI = 0.995, TLI = 0.985, CFI = 0.991, RMSEA = 0.030 (95% CI 0.026–0.034). This result showed that all indicators adequately measured their latent construct.
3.2. Structural Equation Modeling
SEM was conducted to test the relationship between strain due to individual risk factors, strain due to social risk factors, social support, depressive symptoms, and suicidality. The fit of the model (Fig. 1) was good: Chi-square (26, N = 7000) = 76.473, P < .001, GFI = 0.991, TLI = 0.977, CFI = 0.987, RMSEA = 0.034 (95% CI 0.012–0.021). The final model accounted for 27.6% of the variance in suicidality (Table 2).
Table 2.
Coefficient estimates and standard error of path model.
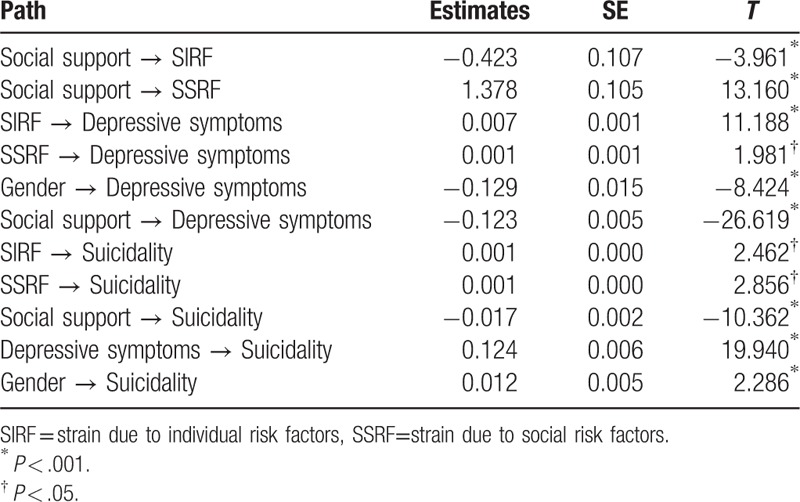
Strain induced by individual risk factors was significantly related to depressive symptoms (β = 0.007, P < .001, 95% CI 0.148–0.213), and strain induced by social risk factors was significantly associated with depressive symptoms (β = 0.001, P < .05, 95% CI 0.004–0.065). Strain due to individual risk factors was positively associated with suicidality (β = 0.001, P < .05, 95% CI −0.093 to −0.015), and strain due to social risk factors was positively related to more suicidality (β = 0.001, P < .05, 95% CI 0.010–0.097).
Social support was negatively related to strain due to individual risk factors (β = -0.423, P < .001, 95% CI −0.081 to −0.024), but social support was positively associated with strain due to social risk factors (β = 1.378, P < .001, 95% CI 0.146–0.201). In addition, social support was negatively associated with depressive symptoms (β = -0.123, P < .001, 95% CI −0.473 to −0.416) and social support was negatively related to suicidality (β = -0.017, P < .001, 95% CI −0.259 to −0.152).
Depressive symptoms were positively related to suicidality (β = 0.124, P < .001, 95% CI 0.348–0.505). In addition, male reported greater suicidality than female (β = 0.012, P < .05, 95% CI −0.010 to 0.058), and female reported more depressive symptoms than male (β = −0.129, P < .001, 95% CI −0.125 to −0.079).
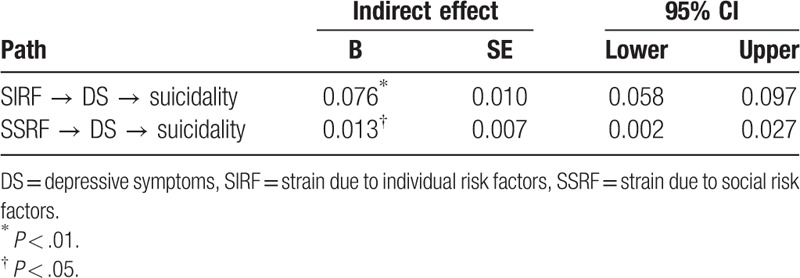
The results (Table 3) showed that strain related to individual risk factors had indirectly an impact on suicidality mediating depressive symptoms (indirect = 0.076, P < .01, 95% CI 0.058–0.097). In addition, strain associated with social risk factors had indirect effects on suicidality mediating depressive symptoms (indirect = 0.013, P < .05, 95% CI 0.002–0.027).
Table 3.
Indirect effects of final model.
4. Discussion
Main findings of this study were that strain induced by individual risk factors and social risk factors were positively associated with suicidality, and affected indirectly suicidality mediating depressive symptoms.
Strain due to individual risk factors was significantly associated with depressive symptoms and suicidality. These results are in line with previous studies in which negative life events had direct effects on suicidal ideation.[9,37] This study complemented a methodological limitation of previous studies by including various individual risk factors. Furthermore, our evidence showed that suicidality is likely to increase when individual risk factors are combined with social risk factors.
This assumption is the core of “The strain theory of suicide.” The theory proposes that strains precede suicide.[5] Strain may induce negative emotions such as hopelessness, anger, and frustration, and heightened tensions, which may lead to mental problems such as depression and suicide. More importantly, strain does not refer to a single stressor or pressure, but distress is composed of at least 2 stressors.[3] In other words, the theory emphasizes that experiencing more than 2 different stressors at the same time significantly increases intent of suicide.
It is necessary to grasp key individual factors related to depression and suicide. Therefore, we conducted a hierarchical regression analysis to identify the independent effects of each individual risk factor on suicidality. Results showed that physical/emotional problem due to aging and family dissolution had a great effect on suicidality. In addition, in the sociopsychological anxiety survey of Korea society of KIHASA,[28] participants reported preparation for old age (35.3%) as the most important factor that government should provide to reduce strain induced by individual risk factors. The second important factor was improvement and support of medical system for physical health (19.8%). These results may be related to the phenomenon that the speed of aging in Korean society is the fastest in the world. It is suggested that strain due to preparation for aging and health problems may be key predictors of depression and suicide in Korea society.[38,39]
It is interesting to note that strain related to social risk factors had a great effect on depressive symptoms and suicidality. Evidences suggest that social risk factors may affect individual's mental health.[40] A few studies have identified the effects of the national economic crisis on depressive symptoms and suicide rate,[20] but no studies have examined the effects of social risk factors on depression and suicide considering various social risk factors. These findings suggest that researchers and clinicians should consider social risk factors as direct factors rather than secondary factors in understanding suicide in adults. In particular, Korean society is in a special external situation including tensions between North and South Korea, as well as low fertility, and very rapid aging. These situations may increase people's psychological distress, and consequently in mental health.
The results of a hierarchical regression analysis indicate that strain associated with new infectious disease, economic recession and economic stagnation, and low fertility/population aging had a great effect on suicidality. In addition, in the sociopsychological anxiety survey of Korean society of KIHASA,[28] participants answered that economic stimulation and growth promotion (43.0%) is the most important factor when asked “what do you think the government should do to decrease the strain induced by social risk factors?”. The next was strengthening management of new infectious diseases (19.6%). These results mean that economic recession may affect the mental health such as depression and suicide in the Korean society like other societies.[41,42] More importantly, low fertility and population aging, one of the representative social issues in Korean society, may have a strong impact on one's mental health from a long-term perspective. The members of the Korean society seem less satisfied with the government reaction when new infectious diseases or national disasters occur. This result may reflect the MERSC (Middle East respiratory syndrome coronavirus) incident in 2015.
Social support plays an important role in the relationship between individual and social risk factors and depressive symptoms/suicidality. Social support was negatively related to depressive symptoms and suicidality. It is plausible that emotional bond and emotional support through interaction with family members and friends may alleviate negative emotions such as loneliness, and consequently in prevention of depression and suicide. Furthermore, these results reinforce the claim that suicide attempts are associated with limited social networks and social interactions.[43,44]
Social support was negatively associated with strain related to individual risk factors, but contrary to expectations, social support positively affected strain associated with social risk factors. These results suggest that information shared through interactions with others can help to find solutions for individual problems, which might reduce strain induced by individual risk factors. On the contrary, as social interaction through the offline and online networks increases, more specific information about the social risk factors is shared, which could induce strain due to social risk factors temporarily.[45] However, these results may be because this study used cross-sectional design. Therefore, further work should extend this study utilizing longitudinal design.
Depressive symptom was a major predictor of suicidality. In addition, strain due to individual risk factors and social risk factors affected suicidality mediating depressive symptoms. These results further strengthen that depression is proximal predictor of suicide, and a mediator in suicide.[9,25] More importantly, this study expanded the previous model that shows individual risk factors had direct effects on suicide, and indirect effect on suicide via depression including social risk factors.[46]
Among sociodemographic variables, gender is an important variable related to depression and suicide. In this study, women reported more depressive symptoms than men, and these results are in line with higher prevalence of depression in women.[47] On the contrary, men may be more vulnerable to suicide than women. Although numerous studies have shown that women are more likely to experience suicidal ideation, the rate of attempted suicide is known to be higher in males.[48]
Finally, substance abuse may be an important risk factor for suicidality. A recent study of meta-analysis[49] showed that people with alcohol use disorder and other substance use disorders are likely to attempt suicide compared with control groups. Thus, in future studies, researchers need to test the independent influence of substance abuse on suicidality.
Several limitations apply to the present study. First, the measurement of suicidal ideation and suicide attempt through 2 questions may not accurately measure the suicidality. Second, this study is cross-sectional in nature. Thus, there is a limit to clarify the relationships between the variables. Despite these limitations, there are several implications from this study's findings in suicide. It is important to consider individual risk factors and social risk factors together in establishing suicide prevention policies. In other words, in order to decrease suicidal ideation and suicide attempt, not only the individual efforts but also government efforts such as providing extensive health insurance are needed to reduce strain associated with social risk factors.
Author contributions
Writing – original draft: Bae Sung-Man.
Footnotes
Abbreviations: CESD-11 = Center for Epidemiologic Studies-Depression Scale 11, KIHASA = Korea Institute for Health and Social Affairs, MERSC = Middle East Respiratory Syndrome Coronavirus, OECD = Organization for Economic Co-operation and Development, SARS = severe acute respiratory syndrome.
Funding/support: The data from the sociopsychological anxiety survey of Korean society conducted by the Korea Institute for Health and Social Affairs (KIHASA) in 2015 were used for analysis.
There are no conflicts of interest.
References
- [1].Conner KR, Phillips MR, Meldrum SC. Predictors of low-intent and high-intent suicide attempts in rural China. Am J Public Health 2007;97:1842–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Stack S, Wasserman I. Economic strain and suicide risk: a qualitative analysis. Suicide Life Threat Behav 2007;37:103–12. [DOI] [PubMed] [Google Scholar]
- [3].Zhang J, Liu Y, Sun L. Life satisfaction and degree of suicide intent: a test of the strain theory of suicide. Compr Psychiatry 2017;74:1–8. [DOI] [PubMed] [Google Scholar]
- [4].Moscicki EK. Epidemiology of ners: initial evaluation. Epidemiology of completed and attempted suicide: toward a framework for prevention. Clin Neurosci Res 2001;1:310–23. [Google Scholar]
- [5].Zhang J. From psychological strain to disconnectedness: a two-factor model theory of suicide. Crisis 2016;37:169–75. [DOI] [PubMed] [Google Scholar]
- [6].Crump C, Sundquist K, Sundquist J, et al. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med 2014;44:279–89. [DOI] [PubMed] [Google Scholar]
- [7].Nock MK, Hwang I, Sampson N, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med 2009;6:e1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Cheng JKY, Fancher TL, Ratanasen M, et al. Lifetime suicidal ideation and suicide attempts in Asian Americans. Asian Am J Psychol 2010;1:18–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gong Y, Zhang L, Wang Z, et al. Pathway analysis of risk factors for severe suicidal ideation: a survey in rural China. Can J Public Health 2011;102:472–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kuroki Y. Risk factors for suicidal behaviors among Filipino Americans: a data mining approach. Am J Orthopsychiatry 2015;85:34–42. [DOI] [PubMed] [Google Scholar]
- [11].Compton MT, Thompson NJ, Kaslow NJ. Social environment factors associated with suicide attempt among low-income African Americans: the protective role of family relationships and social support. Soc Psychiatry Psychiatr Epidemiol 2005;40:175–85. [DOI] [PubMed] [Google Scholar]
- [12].Song YY, Lu Y. Decision tree methods: applications for classification and prediction. Shanghai Arch Psychiatry 2015;27:130–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Amitai M, Apter A. Social aspects of suicidal behavior and prevention in early life: a review. Int J Environ Res Public Health 2012;9:985–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Diez-Roux AV. Neighborhoods and health: where are we and were do we go from here? Rev Epidemiol Sante Publique 2007;55:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Taylor-Gooby P. New Risk, New Welfare. Oxford: Oxford University Press; 2004. [Google Scholar]
- [16].Isikli E, Ustundag A, Cevikcan E. The effects of environmental risk factors on city life cycle; a link analysis. Hum Ecol Risk Assess 2015;21:1379–94. [Google Scholar]
- [17].Fergussion DM, McLeod GFH, Horwood LJ, et al. Life satisfaction and mental health problems. Psychol Med 2015;45:2427–36. [DOI] [PubMed] [Google Scholar]
- [18].Organization Economic Co-operation Development. Better Life Index. 2017. Available at: http://www.oecdbetterlifeindex.org/#/11111111111. [Google Scholar]
- [19].Coope C, Donovan J, Wilson C, et al. Characteristics of people dying by suicide after job loss, financial difficulties and other economic stressors during a period of recession (2010–2011): a review of corners’ records. J Affect Disord 2015;183:98–105. [DOI] [PubMed] [Google Scholar]
- [20].Madianos M, Economou M, Alexiou T, et al. Depression and economic hardship across Greece in 2008 and 2009: two cross-sectional surveys nationwide. Soc Psychiatry Psychiatr Epidemiol 2011;46:943–52. [DOI] [PubMed] [Google Scholar]
- [21].Bromet EJ, Cloustion S, Gonzalez A, et al. Hurricane Sandy exposure and the mental health of World Trade Center responders. J Trauma Stress 2017;30:107–14. [DOI] [PubMed] [Google Scholar]
- [22].Bell CJ, Boden JM, Horwood LJ, et al. The role of peri-traumatic stress and disruption distress in predicting symptoms of major depression following exposure to a natural disaster. Aust N Z J Psychiatry 2017;51:711–8. [DOI] [PubMed] [Google Scholar]
- [23].Jeong AS, An JY. The moderating role of social support on depression and anxiety for gastric cancer patients and their family caregivers. PLoS One 2017;12:e0189808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Sherbourne CD. The role of social support and life stress events in use of mental health services. Soc Sci Med 1988;27:1393–400. [DOI] [PubMed] [Google Scholar]
- [25].Cheng ST, Chan AC. Multiple pathways from stress to suicidality and the protective effect of social support in Hong Kong adolescents. Suicide Life Threat Behav 2007;37:187–96. [DOI] [PubMed] [Google Scholar]
- [26].Lamis D, Lester D. Gender differences in risk and protective factors for suicidal ideation among college students. J Coll Stud Psychother 2013;27:62–77. [Google Scholar]
- [27].Kumar RS, Hashim U. Gender differences among suspected suicide attempts in a rural tertiary care hospital in South India. Psychiatr Rehab J 2018;9:59–65. [Google Scholar]
- [28].Korea Institute for Health and Social Affairs. Social and Psychological Anxiety Survey of Korean Society, 2015. Available at: https://data.kihasa.re.kr/db/subject_view.jsp?project_seq=370. [Google Scholar]
- [29].Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measur 1977;1:385–401. [Google Scholar]
- [30].Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D Depression Symptoms Index. J Aging Health 1993;5:179–93. [DOI] [PubMed] [Google Scholar]
- [31].Gellis Z. Assessment of brief CES-D measure for depression in homebound medically III older adults. J Gerontol Soc Work 2010;53:289–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Perkins DF, Hartless G. An ecological risk-factor examination of suicide ideation and behavior of adolescents. J Adolesc Res 2002;17:3–26. [Google Scholar]
- [33].Cole DA, Maxwell SE. Testing mediational models with longitudinal data: question and tips in the use of structural equation modeling. J Abnorm Psychol 2003;112:558–77. [DOI] [PubMed] [Google Scholar]
- [34].Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equat Model 1999;6:1–55. [Google Scholar]
- [35].McDonald RP, Ho MHR. Principle and practice in reporting structural equation analyses. Psychol Methods 2002;7:64–82. [DOI] [PubMed] [Google Scholar]
- [36].Mallinckrodt B, Abraham WT, Wei M, et al. Advances in testing the statistical significance of mediation effects. J Counsel Psychol 2006;53:372–8. [Google Scholar]
- [37].Zvolensky MJ, Jardin C, Garey L, et al. Acculturative stress and experiential avoidance: relations to depression, suicide, and anxiety symptoms among minority college students. Cogn Behav Ther 2016;45:501–17. [DOI] [PubMed] [Google Scholar]
- [38].Conwell Y, Thompson C. Suicidal behavior in elders. Psychiatr Clin North Am 2008;31:333–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Juurlink DN, Herrmann N, Szalai JP, et al. Medical illness and the risk of suicide in the elderly. Arch Intern Med 2004;164:1179–84. [DOI] [PubMed] [Google Scholar]
- [40].Simmons L, Braun B, Charnigo R, et al. Depression and poverty among rural women: a relationship of social causation or social selection. J Rural Health 2009;24:292–8. [DOI] [PubMed] [Google Scholar]
- [41].Brown RL, Richman JA, Rospenda KM. Economic stressors and psychological distress; exploring age cohort variation in the wake of the great recession. Stress Health 2017;33:267–77. [DOI] [PubMed] [Google Scholar]
- [42].Schmidt L, Danziger S. Filling holes in the safety net? Material hardship and subjective wellbeing among disabled benefit applicants and recipients after the 1996 welfare reform. Soc Sci Res 2012;41:1581–97. [DOI] [PubMed] [Google Scholar]
- [43].Kaslow NJ, Sherry A, Bethea K, et al. Social risk and protective factors for suicide attempts in low income African American men and women. Suicide Life Threat Behav 2005;35:400–12. [DOI] [PubMed] [Google Scholar]
- [44].Maris RW. Social and familial risk factors in suicidal behavior. Psychiatr Clin North Am 1997;20:519–50. [DOI] [PubMed] [Google Scholar]
- [45].Velez CE, Krause ED, McKinnon A, et al. Social support seeking and early adolescent depression and anxiety symptoms: the moderating role of rumination. J Early Adolesc 2016;36:1118–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Tebbe EA, Moradi B. Suicide risk in trans populations: an application of Minority Stress Theory. J Couns Psychol 2016;63:520–33. [DOI] [PubMed] [Google Scholar]
- [47].American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- [48].Snarr JD, Heyman RE, Slep AMS. Recent suicidal ideation and suicide attempts in a large-scale survey of the U.S. Air Force: prevalences and demographic risk factors. Suicide Life Threat Behav 2010;40:544–52. [DOI] [PubMed] [Google Scholar]
- [49].Carrà G, Bartoli F, Crocamo C, et al. Attempted suicide in people with co-occurring bipolar and substance use disorders: systematic review and meta-analysis. J Affect Disord 2014;167:125–35. [DOI] [PubMed] [Google Scholar]


