Abstract
Palpitations are a frequent symptom in the general population, and if cardiac arrhythmias are the most frequent etiology, their diagnosis may be uncertain. We sought to see whether a specialized management of palpitations is associated with a high diagnostic accuracy in patients presenting with palpitations.
Consecutive patients addressed for isolated palpitations in our outpatient cardiac unit were prospectively included in this observational cohort study. The initial management was standardized: 12-lead electrocardiogram (ECG) as early as possible, ECG monitoring, potentially followed by an individualized management.
On 688 consecutive patients prospectively included, cardiac arrhythmia as the cause of palpitations was found in 81% of cases (77% of atrial arrhythmias, 15% of junctional tachycardia, and 8% of ventricular arrhythmias). A total of 96% of diagnoses were made during initial management. Prehospital ECG (92%) and ECG at admission (67%) had the best positivity rates.
A specialized management of patients presenting with lone palpitations allows the diagnostic of a cardiac arrhythmia in >80% of cases. Earliness of an ECG recording remains the key element in the diagnostic approach of these patients.
Keywords: arrhythmia, care, ECG, management, palpitations, unit
1. Introduction
Palpitations, that is, awareness of a rapid or irregular heartbeat, often described as an unpleasant sensation of pulsation or movement in the chest and/or adjacent areas, are most often caused by cardiac arrhythmias.[1] They are a frequent symptom in the general population, leading to a large amount of consultations in primary care settings.[2] Diagnosis may be difficult and uncertain, with a cardiac etiology found in 34% to 43%.[3,4] This may be partly explained by the absence of systematic diagnostic approach faced with this much frequent situation.
We sought to see whether a specialized management of palpitations improves diagnostic accuracy in patients presenting with acute palpitations.
2. Methods
2.1. Population
All consecutive patients addressed for acute isolated palpitations in the cardiac emergency department of the University Hospital of Tours from January 2014 to December 2016 (3 years) were prospectively included. Patients addressed from other departments or hospital centers (secondary or tertiary management) were excluded, as well as patients with a history of permanent atrial fibrillation. Patients with any other symptom than palpitations were also excluded. The ethics committee for human research of the University Hospital Center of Tours (France) approved the study protocol. All patients signed informed consent form.
2.2. Palpitations unit
The emergency call center was invited to address the patients complaining with palpitations rapidly towards our outpatient cardiac emergency unit. The initial management was standardized:
A 12-lead ECG was systematically carried out as early as possible: during prehospital management if possible or available; within 5 minutes of arrival in the outpatient unit.
ECG monitoring <6 hours was continuously performed in patients without an initial diagnosis.
Patients without a final diagnosis were discharged within 6 hours (thus rated as an outpatient consultation), and an individualized management was eventually proposed, including a 24-hour ECG Holter recording or an electrophysiological study, depending on clinical history and symptoms description.
2.3. Follow-up
Patients were prospectively followed in outpatient clinic until a final diagnosis was reached (endpoint): electrocardiographic documentation of a cardiac arrhythmia with concomitant complaint.
Follow-up ended on July 31, 2017.
2.4. Statistical analyses
Analyses were performed using JMP 9.0 software (SAS Institute, Cary, NC). Patient characteristics were expressed as percentages and averages ± standard deviation (95% confidence interval). Characteristics between subgroups were compared using the Chi2 test for qualitative variables and a Student test for quantitative variables. Accuracy of different tests was calculated using sensitivity, specificity, and positive and negative predictive values (PPV and NPV). A P-value <.05 was considered significant.
3. Results
3.1. Population
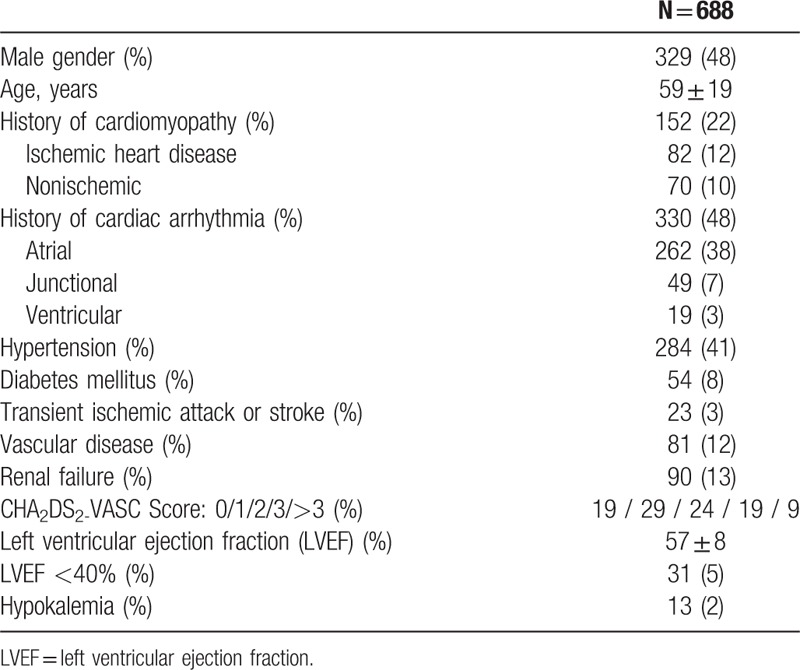
A total of 688 consecutive outpatient consultations for palpitations were included, representing 8.3% of all consultations in our cardiac emergency unit. Characteristics are reported in Table 1. Patients were followed during a mean of 147 ± 315 days.
Table 1.
Characteristics of the population at baseline.
3.2. Diagnoses
A total of 78% of patients were diagnosed within the first day. Among diagnosed patients, 18% of diagnoses were made during prehospital management and 78% in the outpatient unit, that is, 96% within 6 hours.
After discharge, 154 patients (22.4%) remained without a diagnosis. Only 3.2% of these patients were diagnosed within 1st month, 8.4% within 1st year, and 3.2% after 1 year (Fig. 1).
Figure 1.
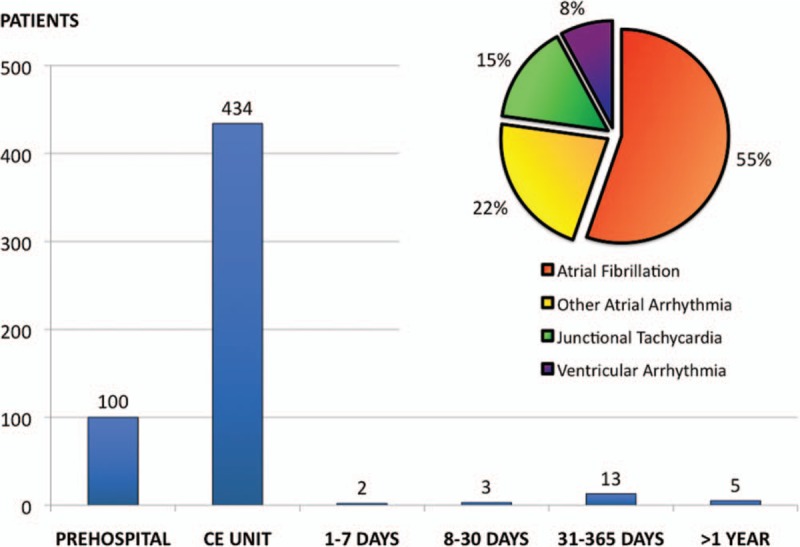
Final diagnosis (N = 557, 81%) and time to diagnosis during prehospital management, in the specialized cardiac outpatient unit, and after discharge during follow-up.
Fifteen patients without a diagnosis at discharge (9.7%) were readmitted for palpitations after a mean follow-up of 199 ± 243 days (range 6–720, median 70). A diagnosis was obtained in 80% of cases, all in the cardiac emergency unit, representing 52% of all diagnoses made after the initial admission.
At the end of the follow-up period, a final diagnosis had been made in 557 cases (81.0%): 308 atrial fibrillation (44.8%), 104 atrial tachycardia or atrial flutter (15.1%), 83 junctional tachycardia (12.1%), 29 premature ventricular contractions (4.2%), 18 premature atrial contractions (2.6%), and 15 monomorphic ventricular tachycardia (2.2%) (Fig. 1). Time to diagnosis was 9.5 ± 67 days (range 0–963, median 1, and interquartile range 1–1).
The 131 patients left remained without a diagnosis after a mean follow-up of 728 ± 285 days.
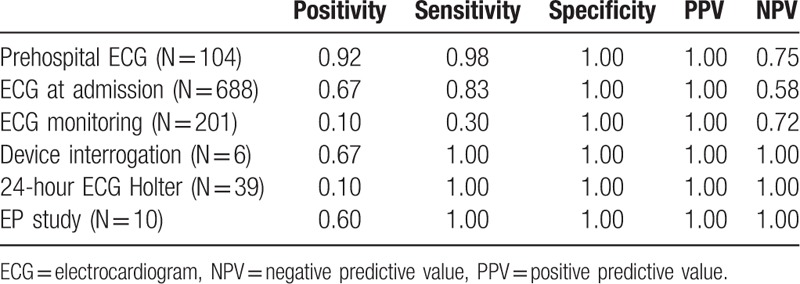
Diagnostic accuracy of complementary tests is represented in Table 2.
Table 2.
Diagnostic accuracy of different complementary tests.
3.3. Prehospital ECG
Prehospital ECG was performed in 104 patients (15.1%) with a positive diagnostic in 96: atrial fibrillation in 52 patients, atrial tachycardia or flutter in 11, junctional tachycardia in 29, premature ventricular contractions in 1, and monomorphic ventricular tachycardia in 3. Among the 82 patients who did not receive any antiarrhythmic therapy during prehospital management, rates of spontaneous self-termination before admission in emergency cardiac unit were 91% for atrial arrhythmia, 56% for junctional tachycardia and 0% for sustained monomorphic ventricular tachycardia.
3.4. ECG at admission
All patients underwent a 12-lead ECG ≤5 minutes after admission in outpatient unit, with a diagnostic positivity of 67%: atrial fibrillation in 265 patients, atrial tachycardia or flutter in 95, junctional tachycardia in 52, premature atrial contractions in 12, premature ventricular contractions in 23, and monomorphic ventricular tachycardia in 14. Among the 584 patients without prehospital ECG, diagnostic positivity was 73%. When prehospital and admission ECG were pooled, first ECG diagnostic positivity was 76%.
3.5. ECG monitoring
A total of 212 patients (45%) were monitored until discharge (<6 hours), with a diagnostic positivity of 10%: atrial fibrillation in 8 patients, atrial tachycardia or flutter in 2, premature atrial contractions in 6, and premature ventricular contractions in 5. Among the 165 patients without a diagnosis on ECG who underwent ECG monitoring, diagnostic positivity was 13%.
3.6. Device interrogation
An implanted device was interrogated in 10 patients (1.5%, 5 with a defibrillator, 4 with a pacemaker, and 1 with a loop recorder), with a diagnostic accuracy of 67%: atrial fibrillation in 4 patients, premature ventricular contractions in 1, and monomorphic ventricular tachycardia in 1.
3.7. Post-discharge investigations
A 24-hour ECG Holter was performed in 39 patients presenting with daily symptoms, with a 10% rate of positive diagnostics: atrial fibrillation in 4 patients.
An electrophysiological study was performed in 10 patients presenting with typical symptoms of junctional re-entrant tachycardia, with a diagnostic positivity of 60%: junctional tachycardia in 6 patients.
3.8. History of cardiac arrhythmia
A total of 358 patients (52%) had no previous history of cardiac arrhythmia. Previous history of atrial, junctional and ventricular arrhythmia were present in 262 (38%), 49 (7%), and 19 (3%) patients, respectively. Patients with a history of cardiac arrhythmia reached a final diagnosis in 92% of cases versus 71% for patients without any history of arrhythmia (P < .0001). Time to diagnosis was similar between groups: 21% before admission and 77% in cardiac emergency unit for patients without any history of arrhythmia, 15% and 79%, respectively, for the other patients (P = .11).
In patients with a history of cardiac arrhythmia, the final diagnostic was a recurrence of a previously diagnosed arrhythmia in 277 patients (84%) and a different diagnosis in 28 patients (8%). Patients with a history of atrial arrhythmia were diagnosed with recurrent atrial arrhythmia in 89% of cases, ventricular arrhythmia in 2% and junctional tachycardia in 2%. Patients with a history of junctional tachycardia were diagnosed with atrial arrhythmia in 27% of cases, ventricular arrhythmia in 2% and recurrent junctional tachycardia in 55%. Patients with a history of ventricular arrhythmia were diagnosed with atrial arrhythmia in 16% of cases, recurrent ventricular arrhythmia in 68%, never with junctional tachycardia.
4. Discussion
This large cohort study showed that: a specialized management of patients presenting with palpitations leads to a final diagnosis in >80% of cases; palpitations are related to atrial arrhythmias in >60% of cases; in patients with a history of cardiac arrhythmia, palpitations are related to a recurrence in most (but not all) cases; a first ECG performed as early as possible, ideally during prehospital management, is the cornerstone of the diagnostic approach to palpitations.
4.1. An early ECG recording
The only large prospective study previously published on this subject recruited 190 consecutive patients.[3] Cardiac arrhythmias were found in only 43% of cases, and psychiatric causes in 31%. In the Weber study, patients were younger (46 years old versus 59 in our study), with less comorbidities (29% hypertension, 13% heart failure), and 28% were admitted through medical clinic, which all may explain less cardiac arrhythmia in their cohort. As in our study, atrial arrhythmias represented the vast majority of diagnosed arrhythmia, which emphasizes the necessity of reaching a final diagnosis in these patients who may be at higher risk of stroke in the absence of an anticoagulation therapy.
Patients with a history of a previously documented cardiac arrhythmia were included, as it may still remain challenging to discern whether it is a true recurrence or another cause of palpitations. We show that in almost 10% of cases a different cardiac arrhythmia is found to be responsible of the symptoms. Indeed, the link between atrial fibrillation and junctional re-entrant tachycardia, either atrioventricular nodal re-entry or through an accessory pathway, is well demonstrated.[5,6] Even in patients with previously documented arrhythmia, palpitations should be systematically explored to deliver an appropriate treatment.
The superiority of a specialized management may be mainly due to the faster realization of a 12-lead ECG, <5 minutes after admission in 100% of cases. Prehospital management with an even earlier ECG showed additional benefits, especially in patients with paroxysmal atrial fibrillation or junctional tachycardia, as these arrhythmias tend to rapidly self-terminate, even without antiarrhythmic drug.[7,8] Generalization of a medical prehospital management in all patients presenting palpitations appear too costly, even if it may reduce drastically the amount of expensive complementary tests prescribed in patients with palpitations, especially 24-hour ECG Holter recordings. It may also decrease the duration of stay in the outpatient unit and the associated costs. The ideal solution is the rapid development and spread in our numeric era of connected objects (such as smartphones, smart watches, etc.), with built-in ECG-capable applications, which should increase further more the diagnostic accuracy in patients with palpitations, without the need of prehospital specialized management.[9] In case of palpitations, patients should be invited to record an ECG tracing as fast as possible, whatever method is used. ECG Holter should remain rare, and electrophysiological study be limited to cases with a strong clinical suspicion of paroxysmal junctional tachycardia, in which a definitive therapeutic ablation procedure can be performed through the same procedure. In some difficult cases, implantation of loop recorder may be proposed.[10]
4.2. Limitations
Admission of patients in a specialized cardiac unit may have induced a bias of selection with recruitment of more severe patients more likely to have cardiac arrhythmias. Near 50% of patients already had a previously diagnosed cardiac arrhythmia. Patients without a final diagnosis were patients without a documented cardiac arrhythmia. These patients may still have undocumented cardiac arrhythmia or palpitations for another cause, psychiatric for instance. Finally, clinical examination detailed standardized data were not collected, and may have helped to reach a final diagnosis on top of ECG recording.[11]
5. Conclusions
Rapid specialized management of patients presenting with lone palpitations allows the diagnostic of a cardiac arrhythmia in >80% of cases. Earliness of ECG recording remains the key element in the diagnostic approach.
Author contributions
NC analyzed the data and drafted the manuscript; AF designed the trial and collected the data; CA, AB, BP, LF, DB, and DA contributed substantially to data collection and manuscript revision.
Conceptualization: Nicolas Clementy, Dominique Babuty.
Data curation: Ambroise Fourquet.
Investigation: Ambroise Fourquet.
Methodology: Nicolas Clementy.
Supervision: Nicolas Clementy, Dominique Babuty, Denis Angoulvant.
Writing – original draft: Nicolas Clementy.
Writing – review & editing: Clémentine Andre, Arnaud Bisson, Bertrand Pierre, Laurent Fauchier.
Footnotes
Abbreviations: ECG = electrocardiogram, NPV = negative predictive value, PPV = positive predictive value.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors have no conflicts of interest to disclose.
References
- [1].Brugada P, Gursoy S, Brugada J, et al. Investigation of palpitations. Lancet 1993;341:1254–8. [DOI] [PubMed] [Google Scholar]
- [2].Kroenke K, Arrington ME, Mangelsdroff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med 1990;150:1685–9. [DOI] [PubMed] [Google Scholar]
- [3].Probst MA, Mower WR, Kanzaria HK, et al. Analysis of emergency department visits for palpitations (from the National Hospital Ambulatory Medical Care Survey). Am J Cardiol 2014;113:1685–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Weber BE, Kapoor WH. Evaluations and outcomes of patients with palpitations. Am J Med 1996;100:138–48. [DOI] [PubMed] [Google Scholar]
- [5].Brugada J, Mont L, Matas M, et al. Atrial fibrillation induced by atrioventricular nodal reentrant tachycardia. Am J Cardiol 1997;79:681–2. [DOI] [PubMed] [Google Scholar]
- [6].Wellens HJ, Durrer D. Wolff–Parkinson–White syndrome and atrial fibrillation. Relation between refractory period of accessory pathway and ventricular rate during atrial fibrillation. Am J Cardiol 1974;34:777–82. [DOI] [PubMed] [Google Scholar]
- [7].Zimetbaum P, Josephson ME. Evaluation of patients with palpitations. N Engl J Med 1998;338:1369–73. [DOI] [PubMed] [Google Scholar]
- [8].Raviele A, Giada F, Bergfeldt L, et al. Management of patients with palpitations: a position paper from the European Heart Rhythm Association. Europace 2011;13:920–34. [DOI] [PubMed] [Google Scholar]
- [9].Halcox JPJ, Wareham K, Cardew A, et al. Assessment of remote heart rhythm sampling using the aliveCor heart monitor to screen for atrial fibrillation: The REHEARSE-AF Study. Circulation 2017;136:1784–94. [DOI] [PubMed] [Google Scholar]
- [10].Giada F, Gulizia M, Francese M, et al. Recurrent unexplained palpitations (RUP) study comparison of implantable loop recorder versus conventional diagnostic strategy. J Am Coll Cardiol 2007;49:1951–6. [DOI] [PubMed] [Google Scholar]
- [11].Asensio-Lafuente E. Paroxysmal tachycardias: how to address the clinical presentation of a patient with palpitations/tachycardia. E-J Cardiol Pract 2015;13:24. [Google Scholar]


