Abstract
Throughout infancy and early childhood, stable and secure relationships with caregivers are needed to promote optimal socioemotional (SE) and cognitive development.
The objective is to examine socio-demographic, maternal, and child indicators of SE problems in 2-year-olds living in an urban-suburban community in the southern United States.
Mother–infant pairs enrolled in a prospective pregnancy cohort study.
Shelby County (Memphis), Tennessee.
One thousand five hundred three women were recruited during their second trimester and followed with their children through the child's age of 2 years.
Child SE development was measured by the Brief Infant-Toddler Social Emotional Assessment at 2 years of age. Mothers reported their own behavioral and mental health, temperament, parenting stress, and potential for child abuse during gestation and/or when their child was 1 year of age. Examiners measured maternal IQ during data collection at the child's age of 1 year. Child communication, cognitive development, and risk for autism spectrum disorder were assessed at 1 and 2 years of age. Multivariable regression models were developed to predict mother-reported SE problems.
In bivariate analyses, multiple maternal behavioral and mental health indicators and child cognitive skills were associated with reported child SE problems at 2 years of age. Regression analyses, controlling for socio-demographic, maternal, and child variables, showed the following factors were independently associated with mother-reported child SE problems: maternal education of high school or less, lower maternal IQ, higher maternal cyclothymic temperament score, greater parenting stress, greater maternal psychological distress, lower child expressive communication score, and child risk for autism spectrum disorder. Socio-demographic variables accounted for the variance often attributed to race.
Since mothers in the study were medically low-risk, generalizing these findings to medically high-risk mothers is unwarranted. In addition, these SE outcomes in 2-year-old children do not reflect the trajectory of SE development throughout early childhood.
Attention to independent indicators of future SE problems in children may help identify individual children and families needing intervention and target public prevention/treatment programs in communities.
Keywords: child development, maternal behavioral health, neurocognitive development, socioemotional development
1. Introduction
Socioemotional (SE) development is the progressive ability to effectively explore, experience, interact with and learn from the social environment, regulate and communicate emotions, and develop and sustain relationships. From bioecological[1] and life course[2] perspectives, SE development is a neurodevelopmental process influenced by interacting biological, social, cultural, neighborhood, and other environmental factors beginning before conception, continuing during pregnancy, and developing throughout childhood. Well-developed SE capacities and early interventions that support their development[3–6] facilitate school readiness,[7] ongoing learning and academic success,[8] longer term employment and income, and improved physical health,[9] mental health,[5] and social outcomes.[6] Similarly, SE problems in early childhood are associated with a wide range of poorer life outcomes such as disruptions in family life,[10] poorer mental health,[11] early initiation of sexual behaviors,[12] poorer academic[13] and employment outcomes,[14] and criminal behaviors.[6]
From infancy through childhood, warm, nurturing, and secure relationships with parents or other caregivers are needed for optimal SE development. Interrelated factors interfering with or disrupting SE development include perinatal factors such as preterm birth,[15] maternal stressors and depression, maternal cognitive dysfunction associated with depression,[16] family poverty,[10,17] family violence,[18] and a wide variety of adverse childhood experiences.[19] The prevalence of SE problems in minority children is higher than among majority children in some studies[20]; however, poverty is a critical confounding variable also associated with SE problems.[21] Such disrupting factors create toxic stress[22] and increase biologic effects of adversity in the developing child. Underlying physiologic processes include dysregulation of the hypothalamic–pituitary–adrenal axis[23] and neurological changes, particularly in the hippocampus and limbic system.[24] Impaired hippocampal neurogenesis, abnormally reduced neurotropic factor levels, and monoaminergic system dysfunctions together seem to be associated with chronic stress exposure and major depression. Chronic stress and depressive symptoms are associated with structural brain changes (i.e., loss of dendritic spines and synapses, reduced dendritic arborization, and diminished glial cells of the hippocampus).[25]
This study was designed to examine socio-demographic; maternal behavioral health, mental health, and intelligence; and child developmental and behavioral characteristics associated with maternal-reported child SE problems in 2-year-old children living in an urban-suburban community in the southern United States. We previously reported characteristics associated with SE problems in 1-year olds and noted different patterns in black and white children. However, in both races maternal psychological distress and parenting stress were associated with SE problems at 1 year of age.[26]
We hypothesized that mother-reported socioemotional problems in 2-year olds are impacted by maternal socio-demographics, positively associated with maternal behavioral health and mental health problems, negatively associated with child neurocognitive development at 1 and 2 years of age, and negatively associated with child anthropometric measurements (birth to 1 year). We further postulated that the effect often attributed to race on child SE development is reduced when controlling for these factors.[27]
2. Methods
2.1. Participants
This study uses data from the Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) study, a prospective cohort study that enrolled 1503 healthy pregnant women during their second trimester of pregnancy. Women between 16 and 40 years old and who were living in Memphis/Shelby County, were able to read and write English, and had a singleton pregnancy were recruited from a university obstetric clinic or community obstetric practices. Women were excluded if they had chronic disease requiring medication (e.g., diabetes, hypertension, sickle cell disease), known complications of pregnancy (e.g., complete placenta previa, oligohydramnios), or had plans to deliver at a hospital not participating in the study. A 2-stage recruitment process occurred between December 2006 and July 2011.[28] Data collection was completed in 2015. Participants were contacted every 3 to 6 months via telephone, email of social media, and quarterly newsletters and holiday and birthday cards were mailed to participants as efforts to maximize retention of the cohort.
Mothers and their children available for follow-up by the CANDLE study team at child age of 1-year (range, 10–15 months) and 2-years (range, 21–27 months) are shown in Figure 1. Retention rates were 92.3% (3rd trimester), 99.5% (birth), 80.4% (1-year child visit), and 79.6% (2-year child visit). Of the 1455 live birth mother–child dyads scheduled for the 2-year CANDLE study visit, 1103 participated in data collection and defined the sample size for this analysis. For the purpose of this analysis, the 20 dyads not identifying as Black or White or with missing race data were excluded from this analysis. Data from 1083 (98%) mother–child dyads were available for analyses. Maternal data during gestation and maternal and child data at the 1-year and 2-year child visits were used in these analyses.
Figure 1.
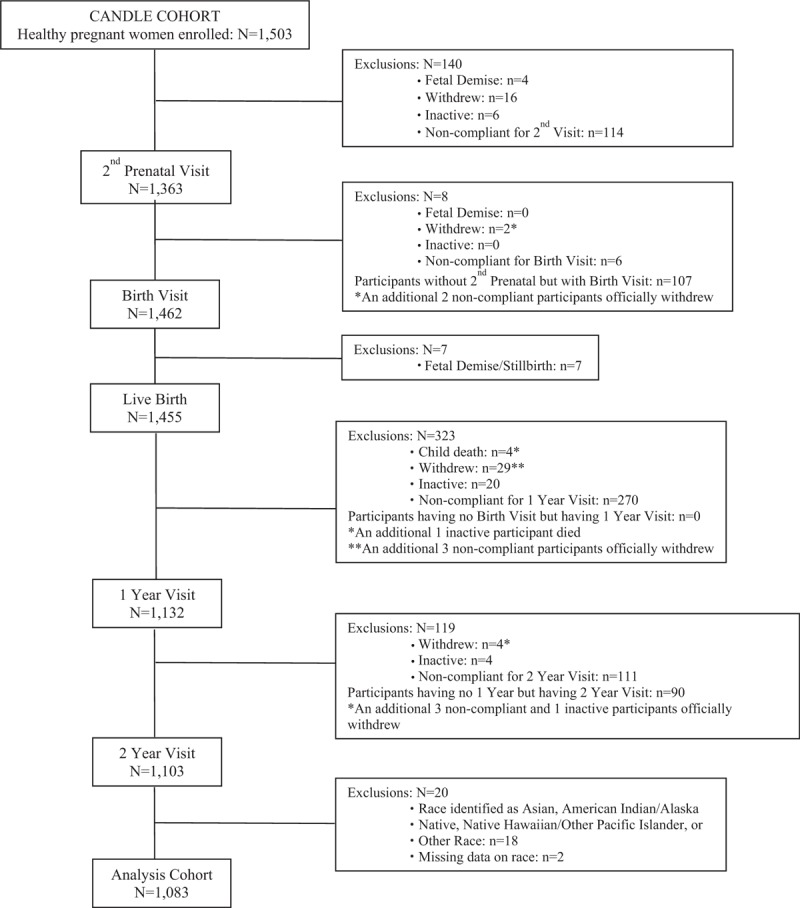
Flowchart of participants included in this research report.
Informed consent was obtained from the mother or the child's legally authorized representative. A gift card was offered as incentive for participation at each visit, that is, $50 at the second trimester visit, $50 at delivery, $100 at the 1-year visit, and $100 at the 2-year visit. The University of Tennessee Health Science Center Institutional Review Board approved the study.
2.2. Socio-demographic characteristics
At enrollment, mothers provided information on age, education, race, marital status, and source of health insurance using a self-administered questionnaire. Health insurance (Medicaid vs Other/None) was used as a proxy for family income, given possible questions about the accuracy of mothers’ reported estimates of income. Child sex and gestational age were collected from birth records. The CANDLE study was designed to recruit individuals that represented healthy pregnant women living in Memphis/Shelby County. The CANDLE study sample and Memphis/Shelby County population showed similar characteristics on age, education, marital status, race, and income. The percent of single mothers (42%) in our study population approximated that found in Memphis/Shelby County (44%).[26]
2.3. Maternal behavioral and mental health
2.3.1. Brief symptom inventory
The 53-item Brief Symptom Inventory (BSI)[29] is a reliable and valid measure of the nature and intensity of psychological symptoms and includes 3 global indices of distress and 9 primary symptom dimensions. The intensity of distress was measured on a 5-point Likert-type scale, from 0 (not at all) to 4 (extremely).[29,30] The BSI was completed by mothers during the 1-year study visit. The T-score for the BSI Global Severity Index, one of the 3 indices, was used in this analysis as an overall measure of severity of psychological symptoms. The Cronbach alpha in the CANDLE study cohort was 0.95.
2.3.2. Edinburgh postnatal depression scale
The self-report 10-item Edinburgh Postnatal Depression Scale (EPDS)[31] was used to assess maternal depression at the 1-year child visit. Items are scored on a 4-point Likert-type scale from 0 (no, not at all) to 3 (yes, most of the time). Continuous EPDS scores were analyzed. This validated and reliable (Cronbach alpha, 0.87–0.88) scale[31] had a Cronbach alpha of 0.84 in the CANDLE study cohort.
2.3.3. Temperament evaluation of Memphis, Pisa, Paris, and San Diego
The 84-item self-report Temperament Evaluation of Memphis, Pisa, Paris, and San Diego (TEMPS)[30] measured maternal temperament during gestation. The TEMPS is a reliable and valid measure of affective temperament characteristics. Four subscales identify personality styles: hyperthymic (intrusive, cheerful, exuberant, overly talkative), dysthymic (gloomy, pessimistic, incapable of fun, self-critical, self-derogatory, brooding, worried, feelings of inadequacy), cyclothymic (lethargy alternating with activity, marked unevenness in quantity and quality of productivity, mental confusion alternating with sharp/creative thinking), and irritable (angry, impulsive, snapping or cursing often, unpleasant). Mothers rated items “yes” if the item statement did apply to much of their lives or “no” if the statement did not apply to much of their lives. The responses (yes=1, no=0) were summed for each subscale, and total scores were analyzed by subscale. The number of items for the hyperthymic, dysthymic, cyclothymic, and irritable subscales were 21, 22, 20, and 21, respectively. Cronbach alpha for subscales ranged from 0.51 (dysthymic) to 0.80 (cyclothymic) in this cohort.
2.3.4. Parenting stress index-short form
Maternal parenting stress was assessed at the 1-year visit using the 36-item Parenting Stress Index-Short Form (PSI-SF).[32] This is a reliable and valid self-report measure intended to identify parents at risk for dysfunctional parenting characteristics which do not promote typical development in children. The PSI-SF yields a Total Stress score as well as Parental Distress, Parent-Child Dysfunctional Interaction, and Difficult Child subscale scores. PSI-SF Total Stress scores were analyzed in this study. Each subscale consists of 12 items rated from 1 (strongly disagree) to 5 (strongly agree). Cronbach alpha for Total Stress in the CANDLE study cohort was 0.92.
2.3.5. Child abuse potential inventory
Maternal risk for physical child abuse was assessed at the 1-year child visit using the self-report Child Abuse Potential Inventory (CAPI). Mothers were asked to indicate if they agree or disagree with each item statement. Responses were summed and binary cut-off scores were calculated to indicate elevated risk. Categories of risk for abuse (CAPI score ≥166) or not at risk (CAPI score < 166) were used in the analysis. The CAPI is a reliable instrument with high levels of construct, content, and concurrent validity.[33] Cronbach's alpha for the CANDLE study cohort was 0.90.
3. Maternal intelligence
3.1. Wechsler abbreviated scale of intelligence
The Wechsler Abbreviated Scale of Intelligence (WASI)[34] is a valid and reliable measure of intelligence that was administered to mothers at the 1-year child visit. The Verbal intelligence quotient (IQ) comprises the Vocabulary and Similarities subtests, and the Performance IQ comprises Block Design and Matrix Reasoning. The WASI Full Scale IQ (FSIQ) score is a standard score derived from the sum of two Verbal subtest T-scores and two Performance subtest T-scores. FSIQ scores were used in the analysis.
3.2. Child anthropometrics
Gestational age was measured by ultrasound or mother's report of last menstrual period. At the 1-year child visit, sex-specific weight and length percentiles for age were used in analyses.
4. Child development and behavior
4.1. Bayley scales of infant and toddler development
Child cognitive and communication development at the 1-year child visit were measured using the Bayley Scales of Infant and Toddler Development, Third Edition Screening Test (Bayley-III Screener). Infant cognitive, receptive communication, and expressive communication scaled scores were classified as at risk (<2nd percentile), emerging (2nd to ≤25th percentile), or competent (>25th percentile).[35] Only 10 of the 1-year-olds were deemed at risk, so children with at risk and emerging scores were combined.
Bayley-III Screener items were selected from the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III)[36] such that Bayley-III items with the highest differentiation between typically performing and low performing children were included in the Bayley-III Screener. The Bayley-III Screener validity was supported by classification rates of the Bayley-III Screener with the Bayley-III scaled scores.[35] Child cognitive and communication development at the 2-year child visit were measured using the Bayley-III. Scaled scores obtained from the cognitive, receptive communication, and expressive communication subtest raw scores were used in the analyses.
4.2. Modified checklist for autism in toddlers
The Modified Checklist for Autism in Toddlers (M-CHAT),[37,38] rated by the mother without the secondary interview, was used to indicate risk for autism spectrum disorder at the 2-year child visit. This 23-item yes/no parent report checklist is a reliable and valid measure that has been found to accurately detect children at risk for autism and pervasive developmental disorder.[38] M-CHAT categories of “Fail” (M-CHAT total score ≥ 3 or critical items ≥2) or “Pass” were used in the analyses. The M-CHAT also includes items associated with SE delays.
4.3. Brief infant-toddler social and emotional assessment
The Brief Infant-Toddler Social and Emotional Assessment (BITSEA) is a reliable and valid measure of socioemotional and behavioral problems and socioemotional competences. The 42-item BITSEA is scored as 0 (not true/rarely), 1 (somewhat true/sometimes), and 2 (very true/always). Total BITSEA problem scores ≤25th percentile for age indicated a possible SE problem. This means that the child's total problem score is higher than the score obtained by 75% of children of the same age and sex in the normative sample.[39] Mothers completed the BITSEA at the 2-year child visit, rating their children's behaviors for the last month.
4.4. Statistical analyses
Socio-demographic, maternal, and child characteristics were summarized using descriptive statistics. Unadjusted odds ratio (OR) estimates and 95% confidence intervals (CI) were computed using simple logistic regression to assess bivariate associations between each variable and possible SE problem (yes, no) at the 2-year child visit. Multivariable logistic regression was conducted to build a final model to identify socio-demographic, socioeconomic, and maternal and child factors associated with reported SE problems at the 2-year visit. Any variable associated with possible SE problem at 2 years of age with P < .10 from the bivariate analyses was included in the initial regression model. Afterward, a final model was developed using an iterative process, specifically the stepwise model selection procedure, and only variables with P < .05 were retained. The exception was race, which was forced into the model at each step of the iterative process, to examine its contribution while controlling for other factors. Adjusted odds ratio estimates and 95% CI are reported for the final model. All analyses modeled the probability of the child developing SE problems at 2 years of age. SAS version 9.3 (SAS Institute Inc) was used to perform all analyses.
5. Results
Maternal and child characteristics are shown in Table 1. Of the 1083 mother–infant dyads examined, 850 (78.5%) mothers did not rank their 2-year-olds in the possible SE problem range on the BITSEA while 230 (21.2%) reported a possible problem. Three dyads (0.3%) had missing outcome data.
Table 1.
Maternal and child characteristics.
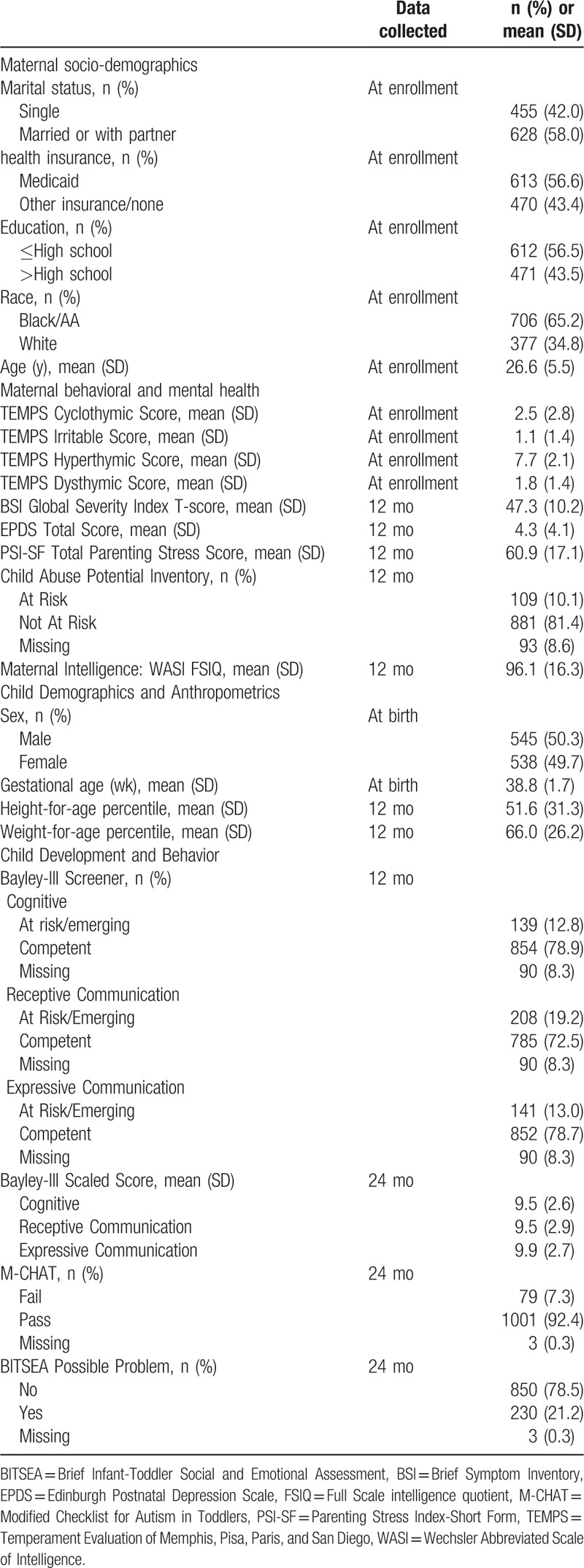
Table 2 displays unadjusted associations between mother-reported SE problems in 2-year olds and maternal variables at enrollment and the 1-year child visit and child variables at birth, the 1-year child visit, and the 2-year child visit. Associations are shown as odds ratios. For continuous variables, the OR represents an increase in SE problem risk for 1 standard deviation (SD) increase in risk represented by each variable. For categorical variables, the OR represents SE problem risk of the specified category compared to the reference level. In these unadjusted analyses, maternal characteristics during gestation that were significantly associated with possible SE problems in 2-year-old children included marital status, Medicaid insurance, high school education or less, Black/African American race, and younger age (all P < .001). Mothers reporting possible child SE problems had higher cyclothymic (P < .001), dysthymic (P = .006), and irritable (P < .001) scores on the TEMPS. Mothers with higher hyperthymic scores were less likely to report SE problems in their child (P = .005). Possible SE problems at 2 years of age were associated with greater maternal psychological distress on the BSI, higher EPDS depression score, greater parenting stress, lower maternal IQ, and identified risk for child abuse on the CAPI (all P < .001) at 1 year of age.
Table 2.
Associations between maternal and child characteristics for possible SE problems at 2 years of age.
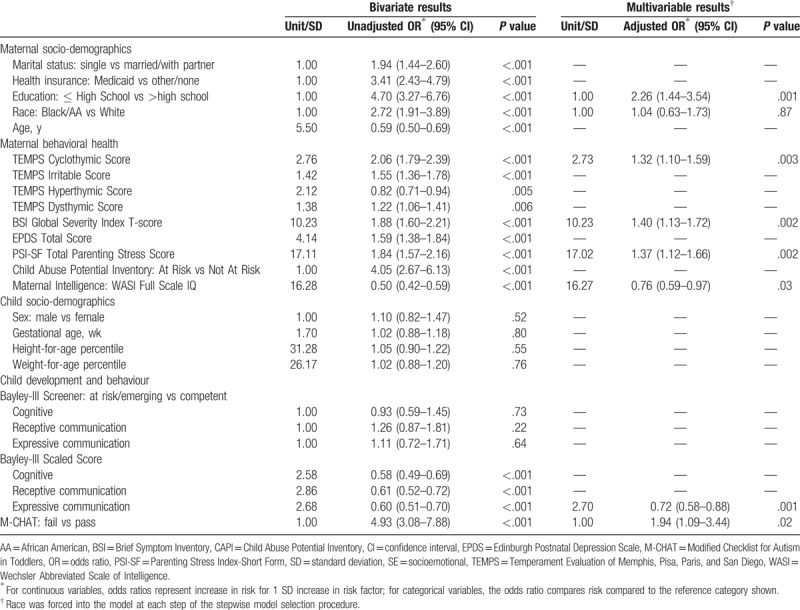
Child variables at birth (sex, gestational age) and at 1 year of age (Bayley-III Screener status for cognitive, receptive communication, expressive communication; and weight and length for age) were not significantly associated with reported SE problems at 2 years of age. However, at 2 years of age, child variables began to show associations with reported possible SE problems. Children with possible SE problems were more likely to fail the M-CHAT and have lower Bayley-III cognitive, receptive communication, and expressive communication scaled scores (all P < .001).
A multivariable logistic regression model predicting likelihood of child SE problems at 2 years of age was developed as described earlier. Results for the final model are shown in Table 2. The following variables were independently associated with SE problems in 2-year-olds: maternal education ≤ high school (P < .001), maternal cyclothymic score during gestation (p = .003), maternal psychological distress as measured by the BSI (p = .002), maternal parenting stress (p = .002) at 1 year of age, WASI FSIQ (p = .024), child expressive communication scaled score (p = .001), and M-CHAT status (p = .023) at 2 years of age. Maternal race, statistically significant in the bivariate analysis, was not significantly associated with reported possible child SE problems at 2 years of age when controlling for other socio-demographic, maternal, and child variables.
6. Discussion
In this representative sample of a southern urban-suburban community, mothers’ report of SE problems in their 2-year-old children was common (21.2%). Not surprisingly, this prevalence is comparable to the BITSEA standardization sample which set the cutoff designation for SE problems based on a problem score of less than or equal to the 25th percentile.[39] The National Center for Child Health and Human Development Study of Early Child Health and Youth Development, using the Child Behavior Checklist/2–3,[40] showed mothers of 24-month-old children reported internalizing behavior problems in 11% and externalizing behaviors in 16% of a large sample.[41] Our study did not distinguish between internalizing and externalizing behavior problems, but comparable overall problem prevalence is suggested. Maternal temperament measured during gestation, socio-demographic variables, psychological distress, and parenting stress at 1 year were associated with reported SE problems in 2-year-old children. Two-year-olds with better expressive communication were less likely to have mother-reported SE problems. The findings did not support associations between communication and cognitive development at 1 year with SE problems at 2 years. Two-year-olds who failed the M-CHAT were more likely to have reported SE problems.
Maternal mental health factors associated with child SE problems are well recognized. Maternal depression and anxiety are commonly associated with child SE problems[42] and may mediate the relationship between poverty and other environmental factors on child outcomes. In unadjusted analyses, measures of maternal depression, global psychological distress, and parenting stress when the child was 1 year of age were all associated with child SE problems at 2 years of age. Additionally, maternal child abuse potential at 1 year was associated with SE problem in 2-year-olds. In the final model, global psychological distress and parenting stress remained as the dominant mental health predictors. Although child abuse potential was not significantly associated with SE problems in the final model, the unadjusted association with SE problems highlights the potential increased risk for maltreatment and indicates that maternal report of SE problems should trigger efforts not only to address the apparent SE problems but also to assess maternal–child relationship and offer support as indicated.
The cyclothymic score, which was assessed during gestation, was associated with reported SE problems at 2 years of age in the final model. The same association of higher maternal cyclothymic score with report of child SE problems was seen in this cohort at age 1 year.[26] Maternal temperament measured during gestation is thought to be a behavioral disposition that is stable over time, irrespective of age and gender.[43] In a study of parents with bipolar disorder and their children, an association between unstructured, disorganized parenting in middle childhood, and altered hypothalamic-pituitary-adrenal functioning in their adolescent children has been shown.[44] While few mothers in our study reached “clinical levels” or reported bipolar disorder diagnoses, the varying mood reflected in higher cyclothymic scores may interfere with mothers’ abilities to provide structured, developmentally-appropriate and consistently responsive caregiving, thereby disrupting SE development.
While maternal depression may disrupt SE development, maternal emotional and cognitive dysfunction and impairment may also disrupt SE development. Cognitive dysfunction during depression is complex and multilevel[16] and varies depending on the depressive disorder.[45] Further examination of maternal mental health (i.e., global psychological distress, parenting stress), intelligence, and cyclothymic temperament as predictors of child SE problems is needed.
It is notable that our measured child developmental variables were not associated with maternal report of child SE problems until 2 years of age. This is consistent with previously reported analyses in this cohort of factors associated with SE problems at 1 year of age which identified similar maternal socio-demographic, mental health, and temperament associations but no associated child factors.[26] Expressive and receptive communication and cognitive skills develop rapidly during the second year of life. The greater array of skills to measure at 2 years of age likely contributes to the emergence of differences at this age, differences not present at 1 year, or at least not measureable with the Bayley-III Screener. At 2 years of age, in unadjusted models, lower cognitive and expressive and receptive communication scores were associated with SE problems. In the final model, lower child expressive communication at 2 years of age remained highly associated with SE problem status. It is logical to suspect that 2-year-olds with more limited expressive communication skills are more likely to use nonverbal behaviors to communicate, behaviors that may be interpreted as problematic. Mothers from lower socioeconomic circumstances in this cohort, those with lower education and/or on Medicaid, reported more SE problems. This is also noted in the UK Millennium Cohort Study[46] and supports a family stress model where lower socioeconomic environment adversely impacts parental mental health which, in turn, influences parenting practices and subsequent child outcomes. This may be compounded by the association of lower socioeconomic status with lower child communication skills in other research.[47] It is not surprising that children failing the M-CHAT[38] were more likely to have reported SE problems. The M-CHAT screens for specific SE behaviors that are also captured by the BITSEA. Although child internalizing and externalizing behavior may have been associated with maternal report of child SE problems, variables measuring these behaviors were not included in this study. This limitation needs to be addressed in future work.
In the unadjusted analysis, Black/African American race was a strong predictor of reported SE problems (unadjusted OR 2.72, 95% CI 1.91–3.89; P < .001). However, black mothers in this cohort were more likely to be on Medicaid, younger, a single parent and have lower educational attainment. Race was not statistically significant after adjusting for education, maternal behavioral and mental health, and child development variables in the final model. This finding highlights the complex role of race as an independent variable. Social and psychological dimensions of race are equally if not more important than biological dimensions and may be the main drivers of interest in important health outcomes, such as early child SE development.[27] Understanding the interactions of race and other socio-demographic variables as they relate to child development is necessary if we are to develop and implement prevention and intervention strategies to improve child SE development in diverse communities.[48] This study benefits from a large sample of socio-demographically diverse mother–child pairs. An exceptionally wide range of independent maternal and child variables were objectively measured. The demography of the sample very closely matches the demography of Memphis/Shelby County and is similar to other urban-suburban communities in the southern United States. Although the current study's higher percentage of single mothers limits the extrapolation to the general US population, this percentage may be equivalent to other urban populations. The CANDLE retention rate is good for a comprehensive, longitudinal assessment of a community population and is comparable to that of the Early Childhood Longitudinal Study-Birth Cohort.[49] SE problems were based on parental report using the BITSEA. While the BITSEA validation sample included children from minority and majority backgrounds,[39] these backgrounds may differ from parents and children in Memphis/Shelby County, Tennessee.
The enrolled mothers were medically low-risk. Therefore, generalizing these findings to medically high-risk mothers is unwarranted. This was a cross-sectional analysis of SE outcomes in 2-year-old children and cannot reflect the trajectory of SE development throughout early childhood. As the cohort ages, longitudinal analyses will assess factors predicting a trajectory of SE development through the preschool years. Finally, unmeasured variables are likely to be additional factors associated with child SE problems. These include experienced racism, family violence, neighborhood distress, and other environmental and genetic factors. Future research in this and other cohorts should examine the role of these variables, alone and in combination, in determining SE outcomes in very young children.
Within the bioecological and life course frameworks, our findings are consistent with models of poverty and related socio-demographic stressors that compromise the ability of parents to provide for optimal child SE development.[50] This compromise may be partially mediated by resulting parental psychological distress that interferes with parenting and thereby shapes neurodevelopmental underpinnings of SE development.[17,46]
Preventive and therapeutic approaches addressing parenting have been successful and offer promise at a system level. Nurse home visiting interventions to reduce parenting stress through parenting education and parent support have been shown to reduce child behavior problems in 2- to 3-year-olds.[51] Early childhood services, including quality child care and preschool services, are effective in fostering SE development.[3] Primary care settings provide opportunities for interventions designed to promote positive parenting and thereby improve child SE development.[52] A recent meta-analysis of primary care-based interventions demonstrates “modest, but significant” positive changes in parenting.[53] The Academic Pediatric Association Task Force on Poverty offers a roadmap for systematic redesign of primary care settings to support children and their families in poverty.[54] Expected benefits from such systems change should include enhanced child SE development among other important child health outcomes. This study examined select biological and social factors that are associated with SE development in young children. These factors represent aspects of mothers, their young children, and the prenatal and early childhood processes that contribute to SE development in a metropolitan community. Attention to the strongest maternal and child predictors of child SE development can alert professionals working with expectant and young families to identify individual children and families needing support, guide professionals to consider evidence-based interventions, and target public prevention/treatment programs in communities to improve child SE development.
Acknowledgments
The authors gratefully acknowledge the participants in this study, particularly mothers who agreed to participate and their children; the cognitive examiners from the University of Tennessee Health Science Center (UTHSC) Boling Center for Developmental Disabilities: Sacha Bliss, Lauren Gardner, Cynthia Klubnik, Kerrie Murphy, Jessica Myszak, Nichol Pritchard, Preeti Rao, Colby Reed, Colby Taylor, and Christina Warner-Metzger; individuals from UTHSC who participated in the design and conduct of the study: Pamela Connor, Marion Hare, Anand Kulkarni, and Phyllis Richey; CANDLE study staff who engaged in data collection, processing, and editing; Lauren Sims Taylor, CANDLE Clinic Coordinator; Mingjuan Wang, CANDLE Data Analyst; Maureen Sorrells, CANDLE Project Manager; Grant Somes who designed the study and obtained funding; and Curtis Roby, Scientific Editor.
Author contributions
Conceptualization: Frederick B. Palmer, J. Carolyn Graff, Tamekia L. Jones, Laura E. Murphy, Bruce L. Keisling, Toni M. Whitaker, Frances A. Tylavsky.
Data curation: Tamekia L. Jones, Lei Wang.
Formal analysis: J. Carolyn Graff, Tamekia L. Jones, Lei Wang.
Funding acquisition: Frederick B. Palmer, Frances A. Tylavsky.
Investigation: Laura E. Murphy, Bruce L. Keisling.
Methodology: Frederick B. Palmer, J. Carolyn Graff, Tamekia L. Jones, Laura E. Murphy, Frances A. Tylavsky.
Project administration: Frances A. Tylavsky.
Supervision: J. Carolyn Graff, Frances A. Tylavsky.
Validation: J. Carolyn Graff, Lei Wang, Frances A. Tylavsky.
Visualization: J. Carolyn Graff, Tamekia L. Jones, Lei Wang.
Writing – original draft: Frederick B. Palmer, J. Carolyn Graff, Tamekia L. Jones, Laura E. Murphy, Bruce L. Keisling, Toni M. Whitaker, Frances A. Tylavsky.
Writing – review & editing: Frederick B. Palmer, J. Carolyn Graff, Tamekia L. Jones, Laura E. Murphy, Bruce L. Keisling, Toni M. Whitaker, Lei Wang, Frances A. Tylavsky.
Footnotes
Abbreviations: Bayley-III = Bayley Scales of Infant and Toddler Development, Third Edition, Bayley-III Screener = Bayley Scales of Infant and Toddler Development, Third Edition Screening Test, BITSEA = Brief Infant-Toddler Social and Emotional Assessment, BSI = Brief Symptom Inventory, CANDLE = Conditions Affecting Neurocognitive Development and Learning in Early Childhood, CAPI = Child Abuse Potential Inventory, CI = confidence interval, EPDS = Edinburgh Postnatal Depression Scale, FSIQ = full scale intelligence quotient, IQ = intelligence quotient, M-CHAT = Modified Checklist for Autism in Toddlers, OR = odds ratio, PSI-SF = Parenting Stress Index-Short Form, SD = standard deviation, SE = socioemotional, TEMPS = Temperament Evaluation of Memphis, Pisa, Paris, and San Diego, WASI = Wechsler Abbreviated Scale of Intelligence.
This project was supported by a grant from The Urban Child Institute to the University of Tennessee Health Science Center, Department of Preventive Medicine. Drs FBP, JCG, LEM, TMW, and BLK were also supported in part by grant MC-00038-25 from the Health Resources and Services Administration's Maternal and Child Health Bureau and grant 90DD003-05 from the Administration on Intellectual and Developmental Disabilities. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, approval of, or decision to submit the manuscript.
The authors have no conflicts of interest to disclose.
References
- [1].Bronfenbrenner U, Morris PA. The bioecological model of human development. In: Lerner RM, ed. Handbook of Child Psychology. Vol 1. Hoboken, NJ: John Wiley & Sons, Inc.; 2007:793–828. [Google Scholar]
- [2].Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J 2003;7:13–30. [DOI] [PubMed] [Google Scholar]
- [3].Vogel CA, Yange X, Moiduddin EM, et al. Early Head Start children in grade 5: Long-term follow-up of the Early Head Start research and evaluation study sample. In: Office of Planning R, and Evaluation, Administration for Children and Families, ed. Washington, DC: Department of Health and Human Services; 2010. [Google Scholar]
- [4].Schweinhart LJ, Montie J, Xiang Z, et al. Lifetime Effects: The HighScope Perry Preschool Study Through Age 40. HighScope Press: Ypsilanti, MI; 2005. [Google Scholar]
- [5].Kitzman HJ, Olds DL, Cole RE, et al. Enduring effects of prenatal and infancy home visiting by nurses on children: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med 2010;164:412–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Reynolds AJ, Temple JA, Ou SR, et al. Effects of a school-based, early childhood intervention on adult health and well-being: a 19-year follow-up of low-income families. Arch Pediatr Adolesc Med 2007;161:730–9. [DOI] [PubMed] [Google Scholar]
- [7].Raver CC, Jones SM, Li-Grining C, et al. CSRP's impact on low-income preschoolers’ preacademic skills: self-regulation as a mediating mechanism. Child Dev 2011;82:362–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Briggs-Gowan MJ, Carter AS. Social-emotional screening status in early childhood predicts elementary school outcomes. Pediatrics 2008;121:957–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Campbell F, Conti G, Heckman JJ, et al. Early childhood investments substantially boost adult health. Science 2014;343:1478–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Briggs-Gowan MJ, Carter AS, Moye Skuban E, et al. Prevalence of social-emotional and behavioral problems in a community sample of 1- and 2-year-old children. J Am Acad Child Adolesc Psychiatry 2001;40:811–9. [DOI] [PubMed] [Google Scholar]
- [11].Essex MJ, Kraemer HC, Armstrong JM, et al. Exploring risk factors for the emergence of children's mental health problems. Arch Gen Psychiatry 2006;63:1246–56. [DOI] [PubMed] [Google Scholar]
- [12].McLeod JD, Knight S. The association of socioemotional problems with early sexual initiation. Perspect Sex Reprod Health 2010;42:93–101. [DOI] [PubMed] [Google Scholar]
- [13].Li-Grining CP, Votruba-Drzal E, Maldonado-Carreno C, et al. Children's early approaches to learning and academic trajectories through fifth grade. Dev Psychol 2010;46:1062–77. [DOI] [PubMed] [Google Scholar]
- [14].Goodman A, Joyce R, Smith JP, et al. The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci U S A 2011;108:6032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hornman J, de Winter AF, Kerstjens JM, et al. Emotional and behavioral problems of preterm and full-term children at school-entry. Pediatrics 2016;137:e20152255. [DOI] [PubMed] [Google Scholar]
- [16].Gonda X, Pompili M, Serafini G, et al. The role of cognitive dysfunction in the symptoms and remission from depression. Ann Gen Psychiatry 2015;14:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Johnson SB, Riis JL, Noble KG. State of the art review: poverty and the developing brain. Pediatrics 2016;137:e20153075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Davies PT, Sturge-Apple ML, Cicchetti D, et al. Children's patterns of emotional reactivity to conflict as explanatory mechanisms in links between interpartner aggression and child physiological functioning. J Child Psychol Psychiatry 2009;50:1384–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14:245–58. [DOI] [PubMed] [Google Scholar]
- [20].Gilliam W. Prekindergartners Left Behind: Expulsion Rates in State Prekindergarten Systems. New Haven, CT: Yale University Child Study Center; 2005. [Google Scholar]
- [21].Pascoe JM, Wood DL, Duffee JH, et al. Committee on Psychosocial Aspects of Child and Family Health CoCP. Mediators and adverse effects of child poverty in the United States. Pediatrics 2016;137:e20160340. [DOI] [PubMed] [Google Scholar]
- [22].Shonkoff JP, Garner AS. Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012;129:e232–46. [DOI] [PubMed] [Google Scholar]
- [23].Suor JH, Sturge-Apple ML, Davies PT, et al. Tracing differential pathways of risk: associations among family adversity, cortisol, and cognitive functioning in childhood. Child Dev 2015;86:1142–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hurt H, Betancourt LM. Effect of socioeconomic status disparity on child language and neural outcome: how early is early? Pediatr Res 2016;79:148–58. [DOI] [PubMed] [Google Scholar]
- [25].Serafini G, Hayley S, Pompili M, et al. Hippocampal neurogenesis, neurotrophic factors and depression: possible therapeutic targets? CNS Neurol Disord Drug Targets 2014;13:1708–21. [DOI] [PubMed] [Google Scholar]
- [26].Palmer FB, Anand KJ, Graff JC, et al. Early adversity, socioemotional development, and stress in urban 1-year-old children. J Pediatr 2013;163:1733–9. [DOI] [PubMed] [Google Scholar]
- [27].Research CoP. Race/ethnicity, gender, socioeconomic status-research exploring their effects on child health: a subject review. Pediatrics 2000;105:1349–51. [DOI] [PubMed] [Google Scholar]
- [28].Sontag-Padilla LM, Burns RM, Shih RA, et al. The Urban Child Institute CANDLE Study: Methodological Overview and Baseline Sample Description. Santa Monica, CA: RAND Corporation; 2015. [Google Scholar]
- [29].Derogatis LR. BSI Brief Symptom Inventory: Administration, Scoring, and Procedure Manual. 4th ed. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- [30].Akiskal HS, Akiskal KK, Haykal RF, et al. TEMPS-A: progress towards validation of a self-rated clinical version of the temperament evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J Affect Disord 2005;85:3–16. [DOI] [PubMed] [Google Scholar]
- [31].Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782–6. [DOI] [PubMed] [Google Scholar]
- [32].Abidin RR. Parenting Stress Index: Short Form (3rd ed.): Professional Manual. 3rd ed. Lutz, FL: Psychological Assessment Resources, Inc.; 1995. [Google Scholar]
- [33].Milner JS. Child Abuse Potential Inventory. 2nd ed. Lutz, FL: Professional Assessment Resources, Inc.; 1986. [Google Scholar]
- [34].Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) Manual. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- [35].Bayley N. Bayley Scales of Infant and Toddler Development Screening Test Manual. 3rd ed. San Antonio, TX: Pearson; 2006. [Google Scholar]
- [36].Bayley N. Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III). San Antonio, TX: Pearson Education, Inc; 2005. [Google Scholar]
- [37].Robins DL, Dumont-Mathieu T M. Early screening for autism spectrum disorders: update on the modified checklist for autism in toddlers and other measures. J Dev Behav Pediatr 2006;27(2 suppl):S111–9. [DOI] [PubMed] [Google Scholar]
- [38].Robins DL, Fein D, Barton ML, et al. The modified checklist for autism in toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord 2001;31:131–44. [DOI] [PubMed] [Google Scholar]
- [39].Briggs-Gowan MJ, Carter AS. BITSEA: Brief Infant-Toddler Social and Emotional Assessment. San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- [40].Achenbach TM. Manual for the Child Behavior Checklist/2-3 and 1992 Profile. Burlington, VT: Department of Child Psychiatry, University of Vermont; 1992. [Google Scholar]
- [41].Bub KL, McCartney K, Willett JB. Behavior problem trajectories and first-grade cognitive ability and achievement skills: a latent growth curve analysis. J Educ Psychol 2007;99:653–70. [Google Scholar]
- [42].Feldman R, Granat A, Pariente C, et al. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. J Am Acad Child Adolesc Psychiatry 2009;48:919–27. [DOI] [PubMed] [Google Scholar]
- [43].Kawamura Y, Akiyama T, Shimada T, et al. Six-year stability of affective temperaments as measured by TEMPS-A. Psychopathology 2010;43:240–7. [DOI] [PubMed] [Google Scholar]
- [44].Ellenbogen MA, Hodgins S. Structure provided by parents in middle childhood predicts cortisol reactivity in adolescence among the offspring of parents with bipolar disorder and controls. Psychoneuroendocrinology 2009;34:773–85. [DOI] [PubMed] [Google Scholar]
- [45].Airaksinen E, Larsson M, Lundberg I, et al. Cognitive functions in depressive disorders: evidence from a population-based study. Psychol Med 2004;34:83–91. [DOI] [PubMed] [Google Scholar]
- [46].Kiernan KE, Huerta MC. Economic deprivation, maternal depression, parenting and children's cognitive and emotional development in early childhood. Br J Sociol 2008;59:783–806. [DOI] [PubMed] [Google Scholar]
- [47].Hart B, Risley TR. Meaningful Differences in the Everyday Experience of Young American children. Baltimore, MD: Paul H Brookes; 1995. [Google Scholar]
- [48].Cheng TL, Goodman E, Research TCOP. Race, ethnicity, and socioeconomic status in research on child health. Pediatrics 2015;135:e225–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Najarian M, Snow K, Lennon J, Kinsey S. Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), Preschool-Kindergarten 2007 Psychometric Report (NCES 2010-009). National Center for Education Statistics, Institute of Education Statistics, Institute of Education Sciences, U.S. Department of Education. Washington, DC, 2010. [Google Scholar]
- [50].McLoyd VC. The impact of economic hardship on black families and children: psychological distress, parenting, and socioeconomic development. Child Dev 1990;61:311–46. [DOI] [PubMed] [Google Scholar]
- [51].Olds DL, Holmberg JR, Donelan-McCall N, et al. Effects of home visits by paraprofessionals and by nurses on children: follow-up of a randomized trial at ages 6 and 9 years. JAMA Pediatr 2014;168:114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Weisleder A, Cates CB, Dreyer BP, et al. Promotion of positive parenting and prevention of socioemotional disparities. Pediatrics 2016;137:e20153239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Shah R, Kennedy S, Clark MD, et al. Primary care-based interventions to promote positive parenting behaviors: a meta-analysis. Pediatrics 2016;137:e20153393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Poverty ATFoC. A strategic road-map: Committed to bringing the voice of pediatricians to the most important problem facing children in the US today. In: Academic Pediatric Association; American Academy of Pediatrics; 2013. [Google Scholar]


