Abstract
Rationale:
Evidence from cadaveric studies note that the sympathetic nerves from the second and third thoracic ganglia bypass the stellate ganglion in 20% of the population. We present a novel alternative technique for sympathetic blockade of upper extremity via thoracic epidural approach.
Patient concerns:
The patient-reported anxiety about “the placement of the needle in the front of the neck” and severe pain secondary to complex regional pain syndrome.
Diagnoses:
Complex regional pain syndrome type-1 with involvement of upper extremity.
Interventions:
A patient with upper extremity complex regional pain syndrome underwent sympathetic blockade of the upper extremity via thoracic epidural approach with advancement of a catheter through neural foramen and positioning the catheter tip in the upper thoracic paravertebral space.
Outcomes:
Clinical signs of successful sympathetic blockade of upper extremity were consistently observed after each block utilizing this alternative technique multiple times in a single patient.
Lessons:
Thoracic paravertebral block via thoracic epidural approach and catheter use may be an alternative technique for upper extremity sympathetic blockade. Potential advantages of this technique include complete sympathetic blockade of upper extremity for both diagnostic and therapeutic purposes, patient comfort with more effective local anesthetic administration for needle entry site, and potentially reduced risk of pneumothorax and inadvertent intravascular injection.
Keywords: complex regional pain syndrome, paravertebral block, stellate ganglion block, thoracic sympathetic block, upper extremity
1. Introduction
Sympathetic blocks are clinically used for both diagnosis and treatment of various pain syndromes and vascular disorders including complex regional pain syndrome (CRPS). Stellate ganglion block (SGB) is the most commonly used sympathetic block technique for upper extremity, neck and face. However, evidence from cadaveric studies note that the sympathetic nerves from second thoracic (T2) and third thoracic (T3) ganglia bypass the stellate ganglion in 20% of the population.[1,2] SGB may fail to provide complete sympathetic blockade of upper extremity in this patient population, thereby leading to false-negative clinical response when utilized for diagnostic and therapeutic purposes.[3] This concept is important when sympathetic blockade is planned for diagnostic purposes to differentiate neuropathic pain types as sympathetically mediated pain (SMP) or sympathetically independent pain (SIP). SMP has a greater chance of responding favorably to sympathetic blockade. Therefore, a prospective therapy plan of performing repeated sympathetic blocks may be considered. On the contrary, as the chance of responding favorably to sympathetic blocks is less likely in SIP, alternative therapies must be considered. Therefore, complete sympathetic block is important to differentiate SMP versus SIP.[4,5] Theoretically, blocking sympathetic fibers in the upper thoracic segments may provide a more complete sympathetic blockade.[3] Image-guided posterior thoracic paravertebral sympathetic block (TSB) has also been described in the literature,[3,6,7] and recommended as an alternative to SGB.[2] However, pneumothorax is an important risk associated with posterior TSB.[3] We report another alternative approach to upper thoracic segment sympathetic block via epidural approach and catheter use. Based on our search, this technique has not been described in the literature.
Data for the single patient presented in this case report were obtained from the retrospective chart review in a single academic hospital. Data obtained were between the dates May 22, 2017 and February 5, 2018. The patient was diagnosed with CRPS Type 1 based on Budapest criteria. Evaluation, follow-up and the sympathetic blocks of the patient were performed by the same physician who had been fellowship-trained in interventional pain medicine with 17 years of experience in this field. The authors have obtained written consent to publish this case report from the patients. Institutional Review Board approval was obtained for this case report.
2. Case report
A 46-year-old female with history of trauma to right shoulder and arm, diagnosed with CRPS type-1, presented with burning pain in her entire right upper extremity. A sympathetic blockade for diagnosis and treatment of SMP was planned. As the patient was concerned about “the placement of the needle in the front of the neck” and IV sedation option was not available, SGB was not considered. As the symptoms were only confined to upper extremity, posterior TSB was another option, however, after considering the potential risk of pneumothorax with posterior TSB technique in an ambulatory setting, we decided to perform an alternative technique of thoracic paravertebral block via epidural approach and catheter use.
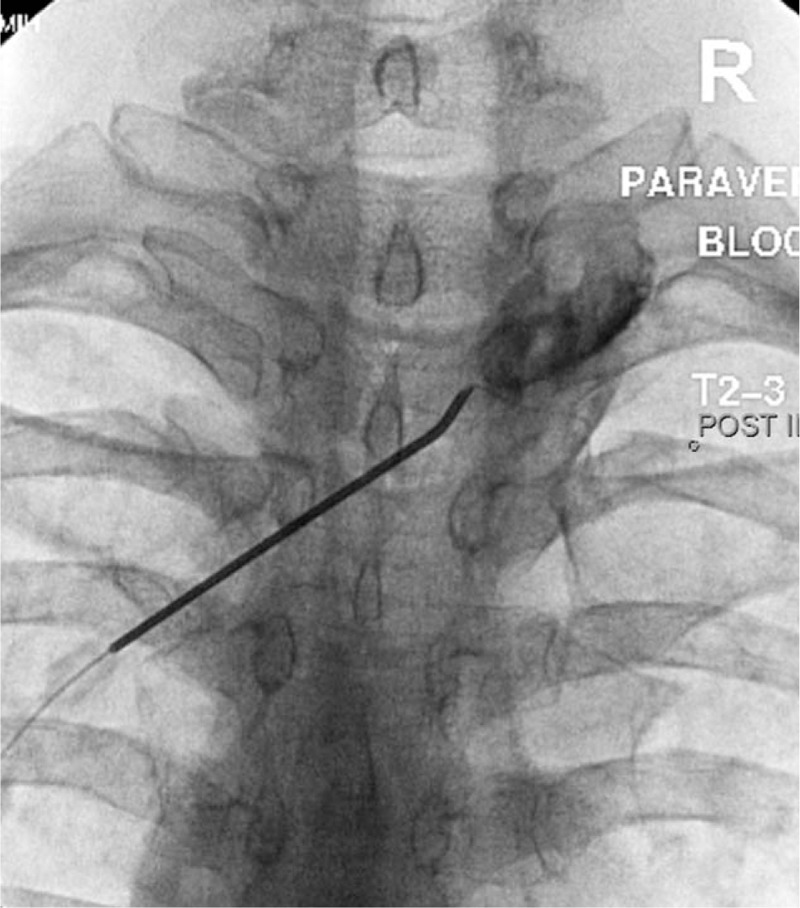
Following informed consent, 18-gauge 3.5 inch RX Coudé needle (Epimed, Farmers Branch, TX) with a curved and blunt tip was placed to the T2–T3 interlaminar epidural space from the contralateral approach with loss of resistance technique, and the needle tip directed toward the right T2–T3 neural foramen. Coudé needle with curved tip was preferred as it facilitates advancement of the catheter to the desired direction. After negative aspiration, a radiopaque epidural catheter with rounded, flexible, and spring-reinforced tip (Versa-Kath epidural catheter 21-gauge, 12 inch length, Epimed) was introduced into the epidural space via Coudé needle. The catheter was advanced into the right paravertebral space through right T2–T3 neural foramen under fluoroscopic guidance (Fig. 1). After negative aspiration for air and body fluids, 5 mL of Iohexol (180 mgI/mL) contrast was injected via catheter, verifying spread in the right paravertebral space, followed by 5 mL of bupivacaine 0.125% (Fig. 2). Signs of the right upper extremity sympathetic blockade were noted postprocedure, including at least 2°C increase in the right upper extremity skin temperature as compared to baseline after each procedure. The patient tolerated the procedures well although the patient reported mild and tolerable pain and tingling sensation in the distribution of T2 nerve during advancement of catheter through the T2–T3 neural foramen in 1 out of 6 procedures. There were no complications.
Figure 1.

Epidural needle entry and catheter exiting through the T2–T3 neural foramen (anteroposterior view).
Figure 2.
Contrast spread within the right paravertebral space (anteroposterior view).
As the patient responded favorably to the first block with approximately 50% reduction in symptoms, diagnosis of SMP was made, and the patient underwent further series of total 6 procedures utilizing the same technique with successful sympathetic blockade of upper limb after each procedure as well as clinical improvement of symptoms. The procedures were well tolerated except mild and tolerable paresthesia sensation in 1 procedure. No complications were encountered.
3. Discussion
The stellate ganglion provides sympathetic innervation to the upper extremity, neck and cranium. There are 2 types of nerves involved in the transmission of sympathetic outflow from the spinal cord: preganglionic and postganglionic. Preganglionic sympathetic nerves arise from the T1 and T2 thoracic spinal levels, and exit the ventral roots to join the sympathetic chain. After synapsing in the inferior (stellate), middle, or superior cervical ganglia, postganglionic sympathetic nerves supply innervation to the neck and cranium. The preganglionic sympathetic nerves to the upper extremity primarily originate from T2 through T8. After exiting through ventral spinal roots, they join to the sympathetic chain, and synapse with their postganglionic components primarily in the T2 ganglion. They may also join to the sympathetic chain in the T1 ganglion, inferior cervical (stellate), and occasionally middle cervical ganglia.[2] Block of the stellate ganglion should successfully block the sympathetic component to the head and neck because all preganglionic nerves either synapse here or pass through on their way to more cephalad ganglia. Majority of the postganglionic sympathetic nerves destined for the upper extremity leave the stellate ganglion as gray communicating rami to join anterior divisions of C5 through T1, ultimately forming the brachial plexus.[3] Evidence from cadaveric studies note the sympathetic nerves from the T2 and T3 levels bypass the stellate ganglion in 20% of the population via alternate pathways known as Kuntz's nerves.[1–3] Kuntz's nerves bypass the stellate ganglion, and directly join the brachial plexus to innervate distal structures of the upper extremity. These fibers may be responsible for reports in the literature indicating inadequate sympathetic block of the upper extremity despite adequate sympathetic block of head and neck,[5] as well as for the common clinical observation that patients receiving SGB may clinically respond inconsistently to repeated blocks performed for therapeutic purposes, despite similar and noticeable Horner syndrome after each block.[3] Moreover, studies also failed to show consistency in terms of reliable and complete upper extremity sympathetic blockade after anterior SGB performed either at C6 or C7 levels.[3,5,8]
A block performed at the anterior lower cervical levels is falsely defined as SGB as the stellate ganglion is anatomically located more distally at the lower edge of the head of the first rib.[5] Studies showed that the solution injected at the cervical levels usually does not reach to stellate ganglion for anatomical reasons, and this is usually the principal reason for failure of SGB.[5,8,9] In addition to Kuntz nerves described above, there are several other alternate pathways for sympathetic fibers shown in anatomical studies that might contribute to failure of sympathetic blockade of the upper extremity after SGB.[5] Some of the sympathetic fibers may distribute along the carotid, subclavian, and vertebral arteries instead of joining brachial plexus, or directly join the peripheral nerves after synapsing outside the sympathetic chain in the intermediate ganglia located in spinal nerves, or possibly bypass the sympathetic chain in the sinuvertebral nerve of Luschka.[5]
Current available techniques for sympathetic block of upper extremity include anterior SGB and posterior TSB.[3,6,7] There are some restrictions of currently available techniques. As mentioned, SGB may fail to produce complete sympathetic blockade due to bypass of some sympathetic fibers.[1,2,3] Besides, local anesthesia of the anterior neck is difficult due to presence of thyroid gland and the abundant vascularity with direct communication to central nervous system; thus creating patient comfort, cooperation, and safety issues.[2,3] In general, when SGB is ineffective, posterior TSB may be recommended as an alternative.[2] However, there is increased risk of pneumothorax with TSB.[3] Pneumothorax creates significant safety and management issues as majority of these blocks are performed in the ambulatory setting. In this case report, we present an alternative epidural approach via an epidural catheter under fluoroscopic guidance. Potential advantages include more complete sympathetic blockade of upper extremity that is important for both diagnostic and therapeutic purposes, patient comfort with more effective local anesthetic administration at the needle entry site, potentially reduced risk of pneumothorax as compared to posterior TSB, and potentially reduced risk of cerebrovascular events as compared to SGB. One disadvantage may be that the somatic block of thoracic segments is almost unavoidable with this technique. However, this nonselectivity may spare the upper extremity, as the majority of sensory and motor innervation of the upper extremity is from the cervical spinal levels, and not from upper thoracic levels. If the type, concentration, and volume of the local anesthetic are carefully selected, a paravertebral block done at the T2–T3 level should create sympathetic blockade, while not significantly influencing sensorimotor innervation to the upper extremity or face. In this case, we preferred a local anesthetic agent with more selectivity to sympathetic nerves at low concentrations such as bupivacaine 0.125% and a low volume (maximum 5 mL) of injectate to avoid spread to cervical levels. Another limitation is the possibility of more significant cardiovascular side effects such as bradycardia and hypotension, due to blockage of the cardiac accelerator fibers in the upper thoracic segments. Therefore, we recommend intravenous access and IV hydration preprocedure, as well as availability of emergency medications for treatment cardiovascular side effects. Also, well-known risks associated with epidural injections may be a higher with this technique such as dural puncture and headache. However, when the risks of various alternative procedures are considered, management for dural puncture headache may be preferred over pneumothorax and intracranial events, specifically in an ambulatory setting.
We present an alternative technique for sympathetic blockade of upper extremity via thoracic epidural approach with advancement of a catheter through neural foramen and positioning the catheter tip in the upper thoracic paravertebral space. Potential advantages of this technique include complete sympathetic blockade of upper extremity for both diagnostic and therapeutic purposes, patient comfort with more effective local anesthetic administration at the needle entry site, and potentially reduced risk of more severe complications as compared to other alternative techniques. Further studies are needed to clarify whether this alternative technique reliably produces sympathetic blockade of upper extremity with more favorable procedural risks.
Author contributions
Semih Gungor: Performance of the procedure, preparation of manuscript, final approval. Jasmit Brar: Preparation of manuscript, final approval.
Conceptualization: Semih Gungor, Jasmit Brar.
Data curation: Semih Gungor.
Investigation: Semih Gungor, Jasmit Brar.
Methodology: Semih Gungor.
Project administration: Semih Gungor.
Resources: Semih Gungor, Jasmit Brar.
Software: Semih Gungor, Jasmit Brar.
Supervision: Semih Gungor.
Visualization: Semih Gungor, Jasmit Brar.
Writing – original draft: Semih Gungor, Jasmit Brar.
Writing – review and editing: Semih Gungor, Jasmit Brar.
Footnotes
Abbreviations: CRPS = complex regional pain syndrome, SGB = stellate ganglion block, SIP = sympathetically independent pain, SMP = sympathetically mediated pain, TSB = thoracic paravertebral sympathetic block.
Hospital for Special Surgery Institution Review Board approval is obtained for this case presentation.
Written informed consent was obtained from the participant for publication of this article and any accompanying tables/images. A copy of the written consent is available for review by the Editor of this journal.
This manuscript was presented in part as an abstract in the ASRA 16th Annual Pain Medicine Meeting, November 16 to 18, 2017, at Disney's Yacht and Beach Club Resort in Lake Buena Vista, FL.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kuntz A. Distribution of the sympathetic rami to the brachial plexus: its relation to sympathectomy affecting the upper extremity. Arch Surg 1927;15:871–7. [Google Scholar]
- [2].Day M. Sympathetic blocks: the evidence. Pain Pract 2008;8:98–109. [DOI] [PubMed] [Google Scholar]
- [3].Rauck RL. Stellate ganglion block. Tech Reg Anesth Pain Manag 2001;5:88–93. [Google Scholar]
- [4].Gungor S, Rana B, Fields K, et al. Changes in the skin conductance monitor as an end point for sympathetic nerve blocks. Pain Med 2017;18:2187–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hogan QH, Abram SE. Neural blockade for diagnosis and prognosis: a review. Anesthesiology 1997;86:216–41. [DOI] [PubMed] [Google Scholar]
- [6].Rocha RO, Teixeira MJ, Yeng LT, et al. Thoracic sympathetic block for the treatment of complex regional pain syndrome I: a double-blind randomized controlled study. Pain 2014;155:2274–81. [DOI] [PubMed] [Google Scholar]
- [7].Yoo HS, Nahm FS, Lee PB, et al. Early thoracic sympathetic block improves the treatment effect for upper extremity neuropathic pain. Anesth Analg 2011;113:605–9. [DOI] [PubMed] [Google Scholar]
- [8].Malmqvist EÅ, Bengtsson M, Sörensen J. Efficacy of stellate ganglion block: a clinical study with bupivacaine. Reg Anesth Pain Med 1992;17:340–7. [PubMed] [Google Scholar]
- [9].Hogan QH, Abram SE, Erickson SJ, et al. The spread of solutions during stellate ganglion block. Reg Anesth Pain Med 1992;17:78–83. [PubMed] [Google Scholar]


