Abstract
Objectives
As well as debridement and irrigation, soft-tissue coverage, and osseous stabilization, systemic antibiotic prophylaxis is considered the benchmark in the management of open fractures and considerably reduces the risk of subsequent fracture-related infections (FRI). The direct application of antibiotics in the surgical field (local antibiotics) has been used for decades as additional prophylaxis in open fractures, although definitive evidence confirming a beneficial effect is scarce. The purpose of the present study was to review the clinical evidence regarding the effect of prophylactic application of local antibiotics in open limb fractures.
Methods
A comprehensive literature search was performed in PubMed, Web of Science, and Embase. Cohort studies investigating the effect of additional local antibiotic prophylaxis compared with systemic prophylaxis alone in the management of open fractures were included and the data were pooled in a meta-analysis.
Results
In total, eight studies which included 2738 patients were eligible for quantitative synthesis. The effect of antibiotic-loaded poly(methyl methacrylate) beads was investigated by six of these studies, and two studies evaluated the effect of local antibiotics applied without a carrier. Meta-analysis showed a significantly lower infection rate when local antibiotics were applied (4.6%; 91/1986) than in the control group receiving standard systemic prophylaxis alone (16.5%; 124/752) (p < 0.001) (odds ratio 0.30; 95% confidence interval 0.22 to 0.40).
Conclusion
This meta-analysis suggests a risk reduction in FRI of 11.9% if additional local antibiotics are given prophylactically for open limb fractures. However, due to limited quality, heterogeneity, and considerable risk of bias, the pooling of data from primary studies has to be interpreted with caution.
Cite this article: M. Morgenstern, A. Vallejo, M. A. McNally, T. F. Moriarty, J. Y. Ferguson, S. Nijs, WJ. Metsemakers. Bone Joint Res 2018;7:447–456. The effect of local antibiotic prophylaxis when treating open limb fractures: A systematic review and meta-analysis. DOI: 10.1302/2046-3758.77.BJR-2018-0043.R1
Keywords: Open fracture, Fracture-related infection, Local antibiotics, Meta-analysis
Article focus
Local antibiotics have been used for decades as prophylaxis in open fractures, but the evidence for its beneficial effect is scarce.
The purpose of the present study was to review the evidence regarding the effect of prophylactic application of local antibiotics in open limb fractures and to identify clinically available applications and carriers for local antibiotics.
Key messages
This meta-analysis suggests a considerable risk reduction if additional local antibiotics are applied in open limb fractures.
Primary studies investigating the prophylactic effect of absorbable carriers including implant coatings for local antibiotic delivery show promising results.
Strengths and limitations
Systematic review of currently available literature including eight comparative studies and ten case series.
Due to limited quality, heterogeneity, and considerable risk of bias, the pooling of data from primary studies has to be interpreted with caution.
Introduction
Open limb fractures are often associated with considerable bone damage, including periosteal stripping, extensive soft-tissue trauma, and severe contamination.1,2 This enables bacteria to breach the damaged skin barrier and to adhere to non-living surfaces, such as implants or dead bone fragments, and to establish a fracture-related infection (FRI).3 After attachment, the bacteria grow in biofilms that protect the pathogens from antibiotics and host immune defences. Biofilm formation is one of the major reasons that FRI is very challenging to treat.1,3,4 FRIs may occur in up to 30% of complex open fractures and are associated with a significant socioeconomic impact,5,6 and so a principal objective in the management of open fractures is to prevent infection.7
As well as debridement and irrigation, soft-tissue coverage, and osseous stabilization, systemic antibiotic prophylaxis is the benchmark in the management of open fractures and has been shown to considerably reduce the risk of subsequent FRI.8-10
However, the local vascular anatomy is often disrupted in complex open limb fractures, leading to reduced tissue concentrations of systemically administered antibiotics. Locally administered antibiotics may overcome this issue with the antibiotic delivered directly to the surgical site, with the resultant tissue concentrations being many times higher than those achieved after systemic antibiotic administration.11 In addition, high local antibiotic levels can be achieved even when local vasculature is compromised and the risk of toxic systemic levels is avoided.11,12 Locally administered antibiotics may also prevent bacteria from colonizing any implant or non-viable tissue surfaces and prevent biofilm formation.6
Although local antibiotics have been used prophylactically for many years in open limb fractures, the available evidence for its beneficial effect is limited.13-20
The purpose of the present study was to review the current literature for evidence regarding the effect of prophylactic application of local antibiotics in open limb fractures. The secondary aim was to identify clinically available applications and carriers for local antibiotics.
Materials and Methods
Reporting guidelines
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, the Meta-analyses of Observational Studies in Epidemiology guidelines, and the Cochrane Handbook for Systematic Reviews of Interventions were followed.21-23 The review was prepared and maintained using the software programme RevMan5 (Version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology was used to rate the quality of evidence.24
Data sources and search strategy
The search was performed with the help of a biomedical information specialist in the PubMed, Web of Science, and Embase databases, and was limited to studies published up to 1 August 2017. The main three search concepts were open fractures, antibiotic prophylaxis, and infection (supplementary material).
Eligibility and study selection
After all the publications had been identified, duplicates were removed and study selection was accomplished by two independent reviewers (MM and AV) in three phases. Disagreements were resolved through discussion with a third reviewer (WJM).
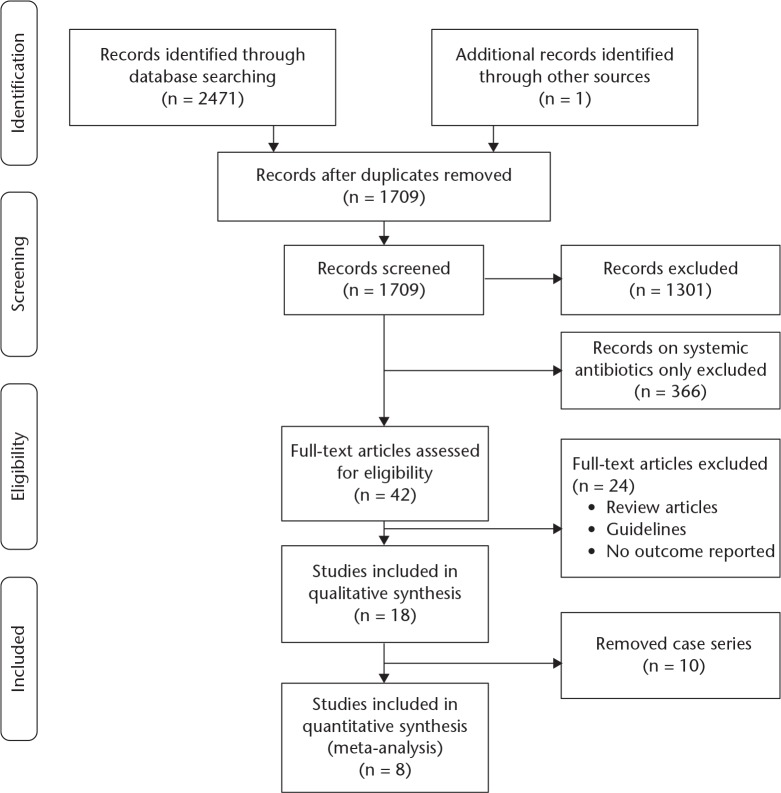
A PRISMA flow diagram provides an overview of the selection process and the number of papers retrieved and excluded, together with reasons, at various stages (Fig. 1).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram: eligibility assessment.
Studies were assessed for eligibility against the following criteria25: 1) population – patients with an open long-bone fracture; 2) intervention – supplementary locally delivered antibiotics at open fracture site; 3) comparator – prophylactic intravenous antibiotics only; 4) outcome – infection at former fracture site occurring in the follow-up period3 (due to the absence of a dedicated definition for FRI until recently,26-28 details on the definition of FRI were also recorded); and 5) study design. The following study designs were included: randomized controlled trials (RCTs) and prospective and retrospective observational designs investigating the effectiveness of supplemental local antibiotics versus systemic antibiotic prophylaxis alone in open limb fractures.
Studies restricted to the following populations or interventions were excluded: paediatric patients; local or systemic antibiotics in treatment of established infections; open fractures associated with previous ulcers or with HIV/AIDS; open fractures not involving long bones; open fractures in the context of military conflicts or associated with gunshots or explosions; experimental studies or animal studies; and studies written in any language other than English.
Data extraction
Extracted data from the eligible papers were entered into RevMan5 (Version 5.3) and are summarized in Table I and in the supplementary material. Comparative studies directly comparing locally delivered antibiotics with standard systemic prophylaxis were considered for quantitative synthesis in a meta-analysis. Observational case series evaluating the effect of local antibiotics, but lacking a control group, were summarized in a qualitative analysis and narrative review.
Table I.
Characteristics of eligible studies for quantitative analysis
| Study/characteristic | Details |
|---|---|
| 01_Henry et al13 (1990) | |
| Study title | The role of local antibiotic therapy in the management of compound fractures |
| Objective | Effect of tobramycin PMMA beads in open fracture wounds for temporary wound coverage |
| Setting | Single centre in the United States (Humana Hospital, University of Louisville) |
| Level of evidence | Low |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive |
| Follow-up interval | Control group: 20.9 mths (6 to 50); intervention group: 17.5 mths (6 to 51) |
| Inclusion criteria | Open limb fractures |
| Number of open fractures for analysis | 404 |
| Gustilo–Anderson | I: 127 (31%); II: 153 (39%); III: 124 (31%) |
| Report of relevant prognostic factors | Partially |
| Systemic antibiotics in both groups | Yes, penicillin, cefazolin, tobramycin |
| Intervention group: local antibiotics | Tobramycin PMMA beads |
| Matching of cohorts | Yes |
| Outcome parameter(s) | Wound infection and/or bone infection |
| Definition of infection? | Incomplete; infection = identification of pathogen in culture |
| 02_Ostermann et al14 (1993) | |
| Study title | The role of local antibiotic therapy in the management of compound fractures |
| Objective | Effect of tobramycin PMMA beads in open fracture wounds for temporary wound coverage |
| Setting | Single centre in the United States (University of Louisville) |
| Level of evidence | Low |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive |
| Follow-up interval | Not reported |
| Inclusion criteria | Open limb fractures |
| Number of open fractures for analysis | 704 |
| Gustilo–Anderson | I: 198 (28%); II: 259 (37%); III: 247 (35%) |
| Report of relevant prognostic factors | Partially |
| Systemic antibiotics in both groups | Yes, penicillin, cefazolin, tobramycin |
| Intervention group: local antibiotics | Tobramycin PMMA beads |
| Matching of cohorts | Similar case-matching reported: grade open fracture, age, gender, fracture location, follow-up interval; no matching in wound closure |
| Outcome parameter(s) | Wound infection and/or bone infection |
| Definition of infection? | Incomplete; infection = identification of pathogen in culture; bone infection = “deep bony infection occurring after 6 weeks” |
| 03_Ostermann et al15 (1995) | |
| Study title | Local antibiotic therapy for severe open fractures. A review of 1085 consecutive cases |
| Objective | Effect of tobramycin PMMA beads in open fracture wounds for temporary wound coverage |
| Setting | Single centre in the United States (University of Louisville) |
| Level of evidence | Low |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive |
| Follow-up interval | Not reported |
| Inclusion criteria | Open limb fractures |
| Number of open fractures for analysis | 1085 |
| Gustilo–Anderson | I: 279 (26%); II: 364 (34%); III: 442 (41%) |
| Report of relevant prognostic factors | Partially |
| Systemic antibiotics in both groups | Yes, penicillin, cefazolin, tobramycin |
| Intervention group: local antibiotics | Tobramycin PMMA beads |
| Matching of cohorts | Similar case-matching reported: grade open fracture, age, gender, fracture location, follow-up interval; no matching in wound closure |
| Outcome parameter(s) | Wound infection and/or bone infection |
| Definition of infection? | Not reported |
| 04_Keating et al16 (1996) | |
| Study title | Reamed nailing of open tibial fractures: does the antibiotic bead pouch reduce the deep infection rate? |
| Objective | Determine whether addition of the bead pouch to a standard protocol of wound management of open fractures was associated with a concomitant reduction in the rate of deep infection |
| Setting | Single centre in the United Kingdom |
| Level of evidence | Low |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive: first control (historical group), then intervention group |
| Follow-up interval | 23 mths (12 to 50) |
| Inclusion criteria | Grade II and III open tibial fractures |
| Number of open fractures for analysis | 78 |
| Gustilo–Anderson | II: 38 (49%); III: 40 (51%) |
| Report of relevant prognostic factors | Partially |
| Systemic antibiotics in both groups | For 72 hrs: cefazolin every 8 hrs; grade III fracture: additional gentamicin |
| Intervention group: local antibiotics | Tobramycin PMMA beads |
| Matching of cohorts | Similar case-matching reported: fracture comminution, age, gender, mean time to wound coverage |
| Outcome parameter(s) | Deep infection and/or nonunion |
| Definition of infection? | Incomplete: “presence of a purulent discharge, with bony involvement evident at the time of surgical debridement” |
| 05_Moehring et al17 (2000) | |
| Study title | Comparison of antibiotic beads and intravenous antibiotics in open fractures |
| Objective | Efficacy of antibiotic-impregnated beads compared with conventional intravenous antibiotics in the treatment of open fractures |
| Setting | Single centre in the United States (University of California) |
| Level of evidence | Moderate |
| Study design | Randomized prospective study |
| Selection of participants | Consecutive enrolment not possible because patients declined to consent or inadvertently were omitted |
| Follow-up interval | 15 mths (12 to 27) |
| Inclusion criteria | Grade II and IIIA/B open long-bone fracture |
| Number of open fractures for analysis | 62 |
| Gustilo–Anderson | Not reported |
| Report of relevant prognostic factors | No |
| Systemic antibiotics in both groups | Cefazolin + aminoglycoside or anaerobic coverage or both added for Grade IIIA/B fractures |
| Intervention group: local antibiotics | Tobramycin PMMA beads; no further systemic antibiotics |
| Control group: additional antibiotics | Yes, intravenous cephalosporin and gentamicin until wound coverage |
| Matching of cohorts | Similar case-matching reported: fracture comminution, age, gender, time to wound coverage |
| Outcome parameter(s) | Infection |
| Definition of infection? | Incomplete: “Persistent drainage, that was positive on culture, from an open fracture site or wound that had broken down” |
| Further information | A third group of 13 fractures was not randomized and received both local and systemic antibiotics (due to limb saving or other reasons). This group was not taken into consideration for this meta-analysis. |
| 06_Ziran et al20 (2004) | |
| Study title | Intramedullary nailing in open tibial fractures: a comparison of two techniques |
| Objective | Comparison of reamed and unreamed tibial nailing in terms of union and infection rate; subgroup analysis: effect of antibiotic beads in IIIIB open tibial fractures |
| Setting | United States, not reported if single or multicentre trial |
| Level of evidence | Very low |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive |
| Follow-up interval | Not reported |
| Inclusion criteria | Grade IIIB open tibial fractures for subgroup analysis |
| Number of open fractures for analysis | 28 |
| Gustilo–Anderson | III: 28 (100%) |
| Report of relevant prognostic factors | No |
| Systemic antibiotics in both groups | Penicillin, cefazolin, and gentamicin |
| Intervention group: local antibiotics | Tobramycin PMMA beads |
| Matching of cohorts | Similar case-matching for all 51 fractures stated but no detailed information given |
| Outcome parameter(s) | Infection |
| Definition of infection? | None |
| Further information | In total, 51 open tibial fractures investigated: 22 reamed and 29 unreamed. In reamed IIIB open tibial fractures, PMMA beads were applied to wound. Just 28 IIIB open tibial fractures are considered in this systematic review. Level of evidence rated very low because prophylactic effect of local antibiotics in open fractures was investigated in just a small cohort. |
| 07_Singh et al18 (2015) | |
| Study title | Surgical site infection in high-energy periarticular tibial fractures with intra-wound vancomycin powder: a retrospective pilot study |
| Objective | Assess the efficacy of intraoperative vancomycin powder administration on preventing deep surgical site infection |
| Setting | Single centre in the United States (Vanderbilt Orthopaedic Institute) |
| Level of evidence | Very low |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive |
| Follow-up interval | Average not reported (minimum 6 mths) |
| Inclusion criteria | Articular tibial fractures, adult, staged fixation with > 5 days after injury |
| Number of open fractures for analysis | 26 |
| Gustilo–Anderson | Not reported |
| Report of relevant prognostic factors | Partially |
| Systemic antibiotics in both groups | Cefazolin every 8 hrs for 24 hrs |
| Intervention group: local antibiotics | 1 g vancomycin powder into surgical wound at time of definitive fixation |
| Matching of cohorts | Similar case-matching for age, gender, smoking, diabetes, fracture location (of all 93 cases) |
| Outcome parameter(s) | Deep surgical site infection |
| Definition of infection? | Surgical site infection not specified |
| Further information | In total, 93 tibial fractures analyzed. For this review, only the 26 open fractures were taken into account. Level of evidence rated very low because prophylactic effect of local antibiotics in open fractures was investigated in just a small cohort. |
| 08_Lawing et al19 (2015) | |
| Study title | Local injection of aminoglycosides for prophylaxis against infection in open fractures |
| Objective | Determine efficacy of local aminoglycosides (gentamicin and tobramycin), in conjunction with systemic antibiotics, to lower the prevalence of infection in patients with open fractures |
| Setting | Single centre in the United States (University of North Carolina) |
| Level of evidence | Moderate |
| Study design | Retrospective cohort study |
| Selection of participants | Consecutive |
| Follow-up interval | Control group: 12.5 mths; intervention group: 11.3 mths |
| Inclusion criteria | Open fractures |
| Number of open fractures for analysis | 351 |
| Gustilo–Anderson | I: 44 (12%); II: 139 (40%); III: 168 (48%) |
| Report of relevant prognostic factors | Yes (very detailed) |
| Systemic antibiotics in both groups | Cefazolin; in grade III fractures gentamicin added; in contaminated fractures penicillin added |
| Intervention group: local antibiotics | Local aminoglycoside injection after wound closure |
| Matching of cohorts | Similar case-matching for age, gender, polytrauma; multivariate analysis was performed to adjust for potential differences for confounding variables |
| Outcome parameter(s) | Infection |
| Definition of infection? | CDC definition of superficial and deep infection |
PMMA, poly(methyl methacrylate); CDC, Centers for Disease Control and Prevention
Assessment of the bias and confidence in the effect
In both RCTs and non-RCTs, the GRADE methodology was used independently by two reviewers to rate the quality of evidence in one of the four categories of evidence: high, moderate, low, and very low.24
Data synthesis and statistical analysis
The data from primary studies comparing the effect of local antibiotics against systemic antibiotics alone on the risk of a subsequent FRI was pooled in a meta-analysis. The pooled odds ratio (OR) for dichotomous outcome measures with the associated 95% confidence interval (CI) was calculated for infection using a fixed-effect model applying the Mantel-Haenszel method.21
The statistical heterogeneity was assessed using a chi-squared test. The I2 statistic was used to quantify the heterogeneity of included studies by quantifying the proportion of the variation in point estimates due to differences between the studies.21,29 Calculations were performed in RevMan5.
Results
Following screening and confirmation of eligibility, 18 articles were available for analysis. Further review of these studies revealed the absence of a control group in ten case series, leaving eight studies eligible for quantitative analysis (Fig. 1). One of these records was identified through other sources, namely in the systematic review of Craig et al.6,20
Overview of selected studies for quantitative analysis
Table I provides an overview of the primary studies included for quantitative analysis (supplementary material): one RCT17 and seven retrospective case-control studies,13-16,18-20 with a total of 2738 analyzed open fractures.
FRI was the primary outcome of interest in all of the included studies. However, there was considerable variation in the definition of FRI, if in fact it was defined at all (Table I).
The mean follow-up period was reported in only four studies and ranged from 11 to 23 months.13,16,17,19
The majority of the studies (six studies) investigated the prophylactic effect of tobramycin-loaded poly(methyl methacrylate) (PMMA) beads placed in the open fracture wound.13-17,20 The remaining two studies investigated the effect of local antibiotics that were applied without a carrier in the fracture wound: vancomycin powder18 and aqueous aminoglycosides.19
Quality assessment of included studies for quantitative analysis
The quality of the evidence ranged from very low to moderate (Table I). The quality of the single RCT included was rated moderate due to a risk of bias because of the lack of reporting of prognostic factors, non-consecutive enrolment, and missing robust measures for infection.17 In contrast, in their cohort study, Lawing et al19 used an established definition for infection, reported detailed relevant prognostic factors, and performed a multivariate analysis to adjust potential differences for confounding variables. The GRADE approach was performed in accordance with the published criteria.24
All included observational studies used a consecutive enrolment, suggesting that the reported study population is likely to be representative. Most of the studies reported some relevant prognostic factors and case-matching,13-16,18,19 whereas only one study covered several important confounding variables and used them for a multivariate analysis.19
Seven studies have a substantial risk of bias, mainly due to the lack of a robust definition of the primary outcome parameter infection. None of the studies reported a sample size calculation.
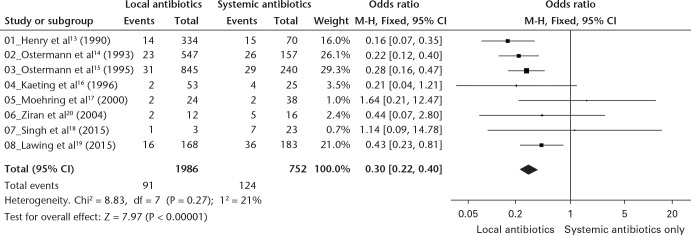
The I2 statistic for the included studies was 21%, suggesting that there was low statistical heterogeneity (Fig. 2).30 However, there was considerable clinical heterogeneity among the included studies, which was due to differing patient populations (e.g. Gustilo–Anderson grade and fracture localizations), interventions, outcome measures, follow-up intervals, and study designs (Table I).
Fig. 2.
Forest plot presenting fracture-related infection with additional local antibiotics versus systemic antibiotic prophylaxis alone in open limb fractures. Blue squares represent the odds ratio (OR), whereas values < 1.0 indicate that the addition of local antibiotics is associated with decreased risk of infection. The vertical line (OR = 1) indicates no effect of local antibiotics. A value of > 1.0 indicates an increased risk of infection if additional local antibiotics were given. Horizontal lines represent the 95% confidence intervals (CIs), whereas lines that do not cross 1.0 indicate significant difference. The diamond is demonstrating the meta-analysis: horizontal tips equal the CI, vertical tips equal the pooled OR (Mantel–Haenszel (M–H)).
Merging all considerations in the GRADE process, the body of evidence of all studies was rated low. Since the two very low-ranked studies are of small sample size and are contributing only 2.0% of all fractures (54 out of 2738 fractures) to the meta-analysis, the overall body of evidence was rated low rather than very low.
Synthesis of study results
The effect of additional local antibiotics versus systemic antibiotic prophylaxis on subsequent infection was analyzed for every individual study and across all studies in a meta-analysis, and results are summarized in Table II and Figure 2. The overall infection rate of all 2738 reported fractures was 7.9% (n = 215).
Table II.
Quantitative analysis of primary studies: number of fractures, number of infections, and infection rate in all reported open fractures, in the intervention group, and in the control group; 13 patients who were not randomized and received local antibiotics are not included in this analysis
| Study (year) | All open fractures |
Intervention group (additional local antibiotics) |
Control group (systemic antibiotics only) |
p–value* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fractures, n | Infections, n | Infection rate, % | Fractures, n | Infections, n | Infection rate, % | Fractures, n | Infections, n | Infection rate, % | ||
| 01_Henry et al13 (1990) | 404 | 29 | 7.2 | 334 | 14 | 4.2 | 70 | 15 | 21.4 | < 0.001 |
| 02_Ostermann et al14 (1993) | 704 | 49 | 7.0 | 547 | 23 | 4.2 | 157 | 26 | 16.6 | < 0.001 |
| 03_Ostermann et al15 (1995) | 1085 | 60 | 5.5 | 845 | 31 | 3.7 | 240 | 29 | 12.1 | < 0.001 |
| 04_Keating et al16 (1996) | 78 | 6 | 7.7 | 53 | 2 | 3.8 | 25 | 4 | 16.0 | 0.079 |
| 05_Moehring et al17 (2000) | 62 | 4 | 6.5 | 24 | 2 | 8.3 | 38 | 2 | 5.3 | 0.637 |
| 06_Ziran et al20 (2004) | 28 | 7 | 25.0 | 12 | 2 | 16.7 | 16 | 5 | 31.3 | 0.662 |
| 07_Singh et al18 (2015) | 26 | 8 | 30.8 | 3 | 1 | 33.3 | 23 | 7 | 30.4 | 1 |
| 08_Lawing et al19 (2015) | 351 | 52 | 14.8 | 168 | 16 | 9.5 | 183 | 36 | 19.7 | 0.010 |
| Overall | 2738 | 215 | 7.9 | 1986 | 91 | 4.6 | 752 | 124 | 16.5 | < 0.001 |
Fisher’s exact test
Results from the meta-analysis suggest a large reduction in infection risk with the use of additional local antibiotics (OR = 0.30; 95% CI 0.22 to 0.40). Open fractures that received local antibiotic prophylaxis subsequently had an infection rate of 4.6%, whereas open fractures treated with standard systemic prophylaxis alone had an infection rate of 16.5% (p < 0.001).
Local antibiotics were associated with a lower infection rate compared with the control group in all three Gustilo–Anderson grades (Table III).
Table III.
Infection rates divided by Gustilo–Anderson (GA) grade between systemic and local antibiotics
| GA grade | All open fractures* |
Intervention group (additional local antibiotics) |
Control group (systemic antibiotics only) |
OR (95% CI) | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fractures, n | Infections, n | Infection rate, % | Fractures, n | Infections, n | Infection rate, % | Fractures, n | Infections, n | Infection rate, % | |||
| I | 604 | 9 | 1.5 | 471 | 3 | 0.6 | 133 | 6 | 4.5 | 0.14 (0.03 to 0.55) | 0.005 |
| II | 814 | 39 | 4.8 | 643 | 20 | 3.1 | 171 | 19 | 11.1 | 0.26 (0.13 to 0.49) | < 0.001 |
| III† | 1085 | 103 | 12.4 | 677 | 49 | 7.2 | 204 | 54 | 26.5 | 0.22 (0.14 to 0.33) | < 0.001 |
| All | 2299 | 151 | 6.8 | 1791 | 72 | 4.0 | 508 | 79 | 15.6 | 0.22 (0.16 to 0.31) | < 0.001 |
Results from qualitative analysis
A qualitative analysis was performed in the ten studies that were excluded from the meta-analysis for a lack of control group (supplementary material).30-39 Five of these studies investigated the effect of PMMA containing tobramycin31,32,39 or the combination of tobramycin and vancomycin, and reported an infection rate from 0% to 20.0%.33,35 Chaudhary et al37 assessed the efficacy of gentamicin-impregnated collagen fleeces in the treatment of open fractures and found an infection rate of 16.1%. Cai et al36 observed no infection in 26 open long-bone fractures treated with local vancomycin-loaded calcium-sulphate pellets. Three series reported no deep infection after treating; in total, 22 open tibial fractures with a polylactic acid/gentamicin-coated tibial nail.30,34,38
Discussion
This systematic review identified one RCT and seven cohort studies investigating the prophylactic effect of local antibiotics on the risk of developing a FRI following open fracture. The pooled meta-analysis, enrolling a total of 2738 open limb fractures, suggested a large beneficial effect of locally applied antimicrobials, when compared with systemic prophylaxis only. This effect was present in all three main Gustilo–Anderson grades.
However, these results should be interpreted with caution due to the low rating of the recommendation when evaluated using the GRADE approach and, therefore, the uncertain impact of heterogeneity and bias on the pooled data results.40
The clinical heterogeneity is mainly due to different patient populations, fracture localizations, study designs, interventions, follow-up intervals, and definitions of infection.
Only one study in this review used an established definition for infection, namely the Centers for Disease Control and Prevention guidelines for surgical site infections (SSI). However, this definition was not exclusively designed for FRIs and has considerable limitations when applied to patients with fractures.19,27,41,42 Incomplete and imprecise definitions of infection were provided in four studies,13,14,16,17 with three studies providing no description of their primary outcome.15,18,20 An international consensus group meeting has recently proposed a standardized definition of FRI in response to a systematic review, which found that only 2% of fracture management trials provided a recognized definition of infection.26,27
Another important factor of clinical heterogeneity is that five primary studies used different anatomical locations13-15,17,19 and only three studies focused solely on tibial fractures.16,18,20 Rates of FRI vary significantly between different anatomical locations,43 and grouping open fractures of upper and lower extremity together in one analysis introduces a degree of bias. A subgroup analysis of one anatomical location would be desirable, but with a low number of cases it is difficult to produce a meaningful conclusion.
The large-scale studies of Henry et al13 and Ostermann et al14,15 found a beneficial effect of locally applied tobramycin PMMA beads. This finding was supported by Keating et al,16 who reported a trend towards reduced risk of FRI with the addition of local tobramycin-loaded PMMA beads (Table II and Fig. 2).
Conversely, the only RCT in this meta-analysis did not find any beneficial effect in preventing FRI with the use of tobramycin-loaded PMMA beads. Moehring et al17 reported an increased risk of FRI with the use of antibiotic-loaded PMMA depots (8.3% vs 5.3%). However, this study is associated with a considerable risk of bias due to patient prognostic factors not being reported, inadequate case-matching with regard to Gustilo–Anderson grade, and the absence of a clearly defined primary outcome (Table I). The somewhat greater infection rate in the intervention group may be explained by the smaller group size and by the fact that this cohort received just a single-dose systemic antimicrobial prophylaxis, whereas in the control group, systemic antibiotics were continued until wound coverage.17 Although antibiotic beads alone can provide high antimicrobial levels at the fracture site, their effects may be limited beyond the fracture site.
Ziran et al20 also investigated the effect of tobramycin-loaded PMMA beads and reported a twofold risk reduction in infection rate (31.3% vs 16.7%). However, due to the small sample size, the study is associated with a considerable risk of bias and the results should be interpreted with caution.
PMMA has been in use since the 1970s and is the most widely studied carrier in this review. Due to its beneficial effect, antibiotic-impregnated PMMA beads should not be neglected in the acute management of open fractures and offer a treatment option for cases that need a planned second-look operation. PMMA is non-biodegradable and, therefore, requires surgical removal, which limits its application after definitive wound closure. In addition, following the initial high level of antibiotic released from PMMA, there is a prolonged low-level antibiotic release that may be below the minimum inhibitory concentration for potential pathogenic organisms, resulting in a selection pressure that favours the emergence of resistant strains, as well as potentially inciting a foreign body reaction.11
There were two studies included in this review that investigated the effect of local antibiotics without a carrier.18,19 The main advantage of this technique is that the antimicrobial can be applied at wound closure and does not require surgical removal. A previous meta-analysis with a limited quality of evidence showed a significant protective effect of topical vancomycin powder in reducing SSI rate in spinal surgery.44 Owen et al45 reported in a recently published cohort study a significant reduction of postoperative infection if vancomycin or tobramycin powder were applied in pelvic/acetabular fracture surgery. In open articular tibial fractures, Singh et al18 found no beneficial effect of topical vancomycin, although this study is associated with a considerable risk of bias due to a small sample size and inadequate reporting of soft-tissue involvement and length of follow-up.
O’Toole et al46 recognized the missing evidence of topical vancomycin in limb fractures and recently published a study outline of a planned multicentre RCT investigating its effect on FRI. The advantages of topical vancomycin are: widespread availability; low cost; efficacy against most common pathogens; and limited concerns regarding inhibition of bone healing or osteogenic cytotoxicity.46 Nonetheless, there are concerns that in the age of widespread antimicrobial resistance, vancomycin should be reserved for therapeutic, rather than prophylactic, purposes.19 Lawing et al19 recognized this and investigated the effect of locally injected aqueous aminoglycosides in open fractures in a methodologically well-designed observational trial. They found a significantly reduced infection rate (9.5%) compared with the control group (19.7%). There was no obvious evidence that local aminoglycosides were inhibiting bone healing since they were not associated with a higher nonunion rate (p = 0.881).19
The main disadvantage of locally administered antibiotics without a carrier is that there is no controlled delivery of antibiotics directly into target tissues and no sustained release over time.11 Biodegradable carriers overcome this issue and do not have the limitations of PMMA. New absorbable biocomposites, such as a gentamicin-loaded calcium-sulphate/hydroxyapatite, have been shown to be highly effective in the treatment of chronic osteomyelitis.47 Malizos et al48 demonstrated in a recently published multicentre RCT that a fast-resorbable antibiotic-loaded hydrogel significantly reduced infection rates after internal fixation of closed fractures. However, evidence of the effectiveness of degradable carriers in open fractures is limited. Our literature search identified only five case series analyzing the effect of biodegradable antibiotic carriers in open fractures. Even though these studies are associated with a considerable risk of bias, the results are promising. No infections were reported in 26 open fractures treated with vancomycin-loaded calcium-sulphate pellets,36 nor in 22 open tibial fractures stabilized with a gentamicin-coated tibial nail.30,34,38
Our current systematic review provides an update on local antibiotic prophylaxis in open long-bone fractures, including various new absorbable carriers.11,48,49 The beneficial effect of local antibiotics in open limb fractures was proven by pooling data exclusively from cohort studies that were directly comparing the effect of additional local antibiotics with that of standard systemic antibiotic prophylaxis. The main limitation of this review and meta-analysis is the low quality of evidence available in the literature. Further controlled trials of sufficient statistical power and bias limiting methodologies are required to corroborate the findings of this meta-analysis. Of critical importance is the reporting of trials in accordance with agreed minimum data sets, and the use of a standardized definition of FRI.
Another limitation of this systematic review may be that Henry et al13 and Ostermann et al14,15 might have used a cumulative cohort since the same group of authors, from the same centre, using a similar technique, described their results in three different studies. However, since they did not mention having used the same cohort of patients, all three studies were included in this meta-analysis. Assuming a cumulative cohort was used, and excluding their first two studies (Henry et al13 and Ostermann et al14) from our meta-analysis, the recalculation of pooled data would show similar results with a significant risk reduction if local antibiotics were given prophylactically (4.9%) compared with the control group receiving standard systemic prophylaxis alone (15.8%) (p < 0.001).
In conclusion, this meta-analysis found a risk reduction (11.9%) of FRI associated with the application of local antibiotics in open limb fractures. However, due to limited quality, heterogeneity, and considerable risk of bias, the pooling of data from primary studies has to be interpreted with caution.
Acknowledgments
The authors wish to thank Thomas Vandendriessche, PhD, biomedical information specialist (KU Leuven Libraries - 2Bergen – Learning Centre Désiré Collen, Belgium), for his help in conducting the systematic literature search.
Footnotes
Author Contributions: M. Morgenstern: Principal investigator, Study design, Literature search, Selection process of primary studies, Statistical analysis, Writing the manuscript.
A. Vallejo: Co-first author, Assisting study design, Literature search, Selection process of primary studies, Statistical analysis, Writing the manuscript.
M. A. McNally: Assisting in carrying out the study, Reviewing the manuscript.
T. F. Moriarty: Assisting study design, Assisting in carrying out the study, Reviewing the manuscript.
J. Y. Ferguson: Assisting in carrying out the study, Reviewing the manuscript.
S. Nijs: Supervising study, Reviewing the manuscript.
WJ. Metsemakers: Study design, Literature search, Selection process of primary studies, Writing the manuscript.
Conflict of Interest Statement: None declared
Follow us @BoneJointRes
Supplementary material
The search strategy, a detailed data form of primary studies eligible for quantitative analysis, and a table showing the characteristics of eligible studies for qualitative analysis.
Funding Statement
None declared
References
References
- 1. Cook GE, Markel DC, Ren W, et al. Infection in Orthopaedics. J Orthop Trauma 2015;29(Suppl 12):S19-S23. [DOI] [PubMed] [Google Scholar]
- 2. Papakostidis C, Kanakaris NK, Pretel J, et al. Prevalence of complications of open tibial shaft fractures stratified as per the Gustilo-Anderson classification. Injury 2011;42:1408-1415. [DOI] [PubMed] [Google Scholar]
- 3. Metsemakers WJ, Kuehl R, Moriarty TF, et al. Infection after fracture fixation: current surgical and microbiological concepts. Injury 2018;49:511-522. [DOI] [PubMed] [Google Scholar]
- 4. Morgenstern M, Post V, Erichsen C, et al. Biofilm formation increases treatment failure in Staphylococcus epidermidis device-related osteomyelitis of the lower extremity in human patients. J Orthop Res 2016;34:1905-1913. [DOI] [PubMed] [Google Scholar]
- 5. Metsemakers WJ, Smeets B, Nijs S, Hoekstra H. Infection after fracture fixation of the tibia: analysis of healthcare utilization and related costs. Injury 2017;48:1204-1210. [DOI] [PubMed] [Google Scholar]
- 6. Craig J, Fuchs T, Jenks M, et al. Systematic review and meta-analysis of the additional benefit of local prophylactic antibiotic therapy for infection rates in open tibia fractures treated with intramedullary nailing. Int Orthop 2014;38:1025-1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zalavras CG. Prevention of infection in open fractures. Infect Dis Clin North Am 2017;31:339-352. [DOI] [PubMed] [Google Scholar]
- 8. Gosselin RA, Roberts I, Gillespie WJ. Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst Rev 2004;1:CD003764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chang Y, Kennedy SA, Bhandari M, et al. Effects of antibiotic prophylaxis in patients with open fracture of the extremities: a systematic review of randomized controlled trials. JBJS Rev 2015;3:3. [DOI] [PubMed] [Google Scholar]
- 10. Bryson DJ, Morris DL, Shivji FS, et al. Antibiotic prophylaxis in orthopaedic surgery: difficult decisions in an era of evolving antibiotic resistance. Bone Joint J 2016;98-B:1014-1019. [DOI] [PubMed] [Google Scholar]
- 11. ter Boo GJA, Grijpma DW, Moriarty TF, Richards RG, Eglin D. Antimicrobial delivery systems for local infection prophylaxis in orthopedic- and trauma surgery. Biomaterials 2015;52:113-125. [DOI] [PubMed] [Google Scholar]
- 12. Carver DC, Kuehn SB, Weinlein JC. Role of systemic and local antibiotics in the treatment of open fractures. Orthop Clin North Am 2017;48:137-153. [DOI] [PubMed] [Google Scholar]
- 13. Henry SL, Ostermann PA, Seligson D. The prophylactic use of antibiotic impregnated beads in open fractures. J Trauma 1990;30:1231-1238. [DOI] [PubMed] [Google Scholar]
- 14. Ostermann PA, Henry SL, Seligson D. The role of local antibiotic therapy in the management of compound fractures. Clin Orthop Relat Res 1993;295:102-111. [PubMed] [Google Scholar]
- 15. Ostermann PA, Seligson D, Henry SL. Local antibiotic therapy for severe open fractures. A review of 1085 consecutive cases. J Bone Joint Surg [Br] 1995;77-B:93-97. [PubMed] [Google Scholar]
- 16. Keating JF, Blachut PA, O'Brien PJ, Meek RN, Broekhuyse H. Reamed nailing of open tibial fractures: does the antibiotic bead pouch reduce the deep infection rate? J Orthop Trauma 1996;10:298-303. [DOI] [PubMed] [Google Scholar]
- 17. Moehring HD, Gravel C, Chapman MW, Olson SA. Comparison of antibiotic beads and intravenous antibiotics in open fractures. Clin Orthop Relat Res 2000;372:254-261. [DOI] [PubMed] [Google Scholar]
- 18. Singh K, Bauer JM, LaChaud GY, Bible JE, Mir HR. Surgical site infection in high-energy peri-articular tibia fractures with intra-wound vancomycin powder: a retrospective pilot study. J Orthop Traumatol 2015;16:287-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lawing CR, Lin FC, Dahners LE. Local injection of aminoglycosides for prophylaxis against infection in open fractures. J Bone Joint Surg [Am] 2015;97:1844-1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ziran BH, Darowish M, Klatt BA, Agudelo JF, Smith WR. Intramedullary nailing in open tibia fractures: a comparison of two techniques. Int Orthop 2004;28:235-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, New Jersey: Wiley-Blackwell, 2008. [Google Scholar]
- 22. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-2012. [DOI] [PubMed] [Google Scholar]
- 23. Bhandari M, Guyatt GH, Montori V, Devereaux PJ, Swiontkowski MF. User's guide to the orthopaedic literature: how to use a systematic literature review. J Bone Joint Surg [Am] 2002;84-A:1672-1682. [PubMed] [Google Scholar]
- 24. Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401-406. [DOI] [PubMed] [Google Scholar]
- 25. Whitehouse MR, McDaid C, Kelly MB, Moran CG, Costa ML. The effect of timing of antibiotic delivery on infection rates related to open limb fractures: a systematic review. Emerg Med J 2017;34:613-620. [DOI] [PubMed] [Google Scholar]
- 26. Metsemakers WJ, Kortram K, Morgenstern M, et al. Definition of infection after fracture fixation: A systematic review of randomized controlled trials to evaluate current practice. Injury 2018;49:497-504. [DOI] [PubMed] [Google Scholar]
- 27. Metsemakers WJ, Morgenstern M, McNally MA, et al. Fracture-related infection: A consensus on definition from an international expert group. Injury 2018;49:505-510. [DOI] [PubMed] [Google Scholar]
- 28. Metsemakers WJ, Moriarty TF, Morgenstern M, et al. Letter to the Editor: New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 2016;474:2726-2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence-inconsistency. J Clin Epidemiol 2011;64:1294-1302. [DOI] [PubMed] [Google Scholar]
- 30. Fuchs T, Stange R, Schmidmaier G, Raschke MJ. The use of gentamicin-coated nails in the tibia: preliminary results of a prospective study. Arch Orthop Trauma Surg 2011;131:1419-1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Henry SL, Ostermann PA, Seligson D. The antibiotic bead pouch technique. The management of severe compound fractures. Clin Orthop Relat Res 1993;295:54-62. [PubMed] [Google Scholar]
- 32. Wright BA, Roberts CS, Seligson D, Malkani AL, McCabe SJ. Cost of antibiotic beads is justified: a study of open fracture wounds and chronic osteomyelitis. J Long Term Eff Med Implants 2007;17:181-185. [DOI] [PubMed] [Google Scholar]
- 33. Gardner MJ, Mehta S, Barei DP, Nork SE. Treatment protocol for open AO/OTA type C3 pilon fractures with segmental bone loss. J Orthop Trauma 2008;22:451-457. [DOI] [PubMed] [Google Scholar]
- 34. Raschke M, Vordemvenne T, Fuchs T. Limb salvage or amputation? The use of a gentamicin coated nail in a severe, grade IIIc tibia fracture. Eur J Trauma Emerg Surg 2010;36:605-608. [DOI] [PubMed] [Google Scholar]
- 35. Hutson JJ, Jr, Dayicioglu D, Oeltjen JC, Panthaki ZJ, Armstrong MB. The treatment of gustilo grade IIIB tibia fractures with application of antibiotic spacer, flap, and sequential distraction osteogenesis. Ann Plast Surg 2010;64:541-552. [DOI] [PubMed] [Google Scholar]
- 36. Cai X, Han K, Cong X, et al. The use of calcium sulfate impregnated with vancomycin in the treatment of open fractures of long bones: a preliminary study. Orthopedics 2010;33:33. [DOI] [PubMed] [Google Scholar]
- 37. Chaudhary S, Sen RK, Saini UC, et al. Use of gentamicin-loaded collagen sponge in internal fixation of open fractures. Chin J Traumatol 2011;14:209-214. [PubMed] [Google Scholar]
- 38. Metsemakers WJ, Reul M, Nijs S. The use of gentamicin-coated nails in complex open tibia fracture and revision cases: A retrospective analysis of a single centre case series and review of the literature. Injury 2015;46:2433-2437. [DOI] [PubMed] [Google Scholar]
- 39. Eckman JB, Jr, Henry SL, Mangino PD, Seligson D. Wound and serum levels of tobramycin with the prophylactic use of tobramycin-impregnated polymethylmethacrylate beads in compound fractures. Clin Orthop Relat Res 1988;237:213-215. [PubMed] [Google Scholar]
- 40. Bhandari M, Joensson A. Meta-Analysis. In: Bhandari M, Joensson A. eds. Clinical Research for Surgeons. New York: Thieme, 2009. [Google Scholar]
- 41. CDC. Surgical Site Infection (SSI) Event. Centers for Disease Control and Prevention, National Healthcare Safety Network (NHSN), 2017, https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf (date last accessed 07 June 2018).
- 42. Morgenstern M, Moriarty TF, Kuehl R, et al. International survey among orthopaedic trauma surgeons: lack of a definition of fracture-related infection. Injury 2018;49:491-496. [DOI] [PubMed] [Google Scholar]
- 43. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res 1989;243:36-40. [PubMed] [Google Scholar]
- 44. Chiang HY, Herwaldt LA, Blevins AE, Cho E, Schweizer ML. Effectiveness of local vancomycin powder to decrease surgical site infections: a meta-analysis. Spine J 2014;14:397-407. [DOI] [PubMed] [Google Scholar]
- 45. Owen MT, Keener EM, Hyde ZB, et al. Intraoperative topical antibiotics for infection prophylaxis in pelvic and acetabular surgery. J Orthop Trauma 2017;31:589-594. [DOI] [PubMed] [Google Scholar]
- 46. O'Toole RV, Joshi M, Carlini AR, et al. Local antibiotic therapy to reduce infection after operative treatment of fractures at high risk of infection: a multicenter, randomized, controlled trial (VANCO Study). J Orthop Trauma 2017;31(Suppl 1):S18-S24. [DOI] [PubMed] [Google Scholar]
- 47. McNally MA, Ferguson JY, Lau AC, et al. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite: a prospective series of 100 cases. Bone Joint J 2016;98-B:1289-1296. [DOI] [PubMed] [Google Scholar]
- 48. Malizos K, Blauth M, Danita A, et al. Fast-resorbable antibiotic-loaded hydrogel coating to reduce post-surgical infection after internal osteosynthesis: a multicenter randomized controlled trial. J Orthop Traumatol 2017;18:159-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Penn-Barwell JG, Murray CK, Wenke JC. Local antibiotic delivery by a bioabsorbable gel is superior to PMMA bead depot in reducing infection in an open fracture model. J Orthop Trauma 2014;28:370-375. [DOI] [PubMed] [Google Scholar]