Abstract
Background
The prognostic significance of galectin-1 (Gal-1) expression in cancerous patients has been assessed for several years while the results remain controversial. Thus, we performed the first comprehensive meta-analysis to evaluate the prognostic value of Gal-1 expression in cancerous patients.
Methods
We searched Pubmed, Embase and Web of Science to recruit studies on the prognostic impact of Gal-1 expression in cancerous patients. Eighteen studies containing 2674 patients were involved in this meta-analysis until March 30, 2018. Pooled hazard ratios (HRs) with 95% confidence interval (95% CI) were calculated to estimate the effect using random-effects model.
Results
The pooled results revealed that high Gal-1 expression in cancer tissue associated with a poor OS (HR = 1.79, 95% CI 1.54–2.08, P < 0.001). In the subgroup of tumor type, it’s observed that high Gal-1 expression was significant correlated with poor OS in digestive cancers without heterogeneity (HR = 1.94, 95% CI 1.64–2.30, P < 0.001; fixed-effects model; I2 = 20.1%, P = 0.276).
Conclusions
Our present meta-analysis indicates that high Gal-1 expression might be a predictive factor of poor prognosis in cancers, particularly in digestive cancers.
Keywords: Galectin-1, Cancer, Prognosis, Meta-analysis
Background
Cancer has been a globally severe health problem. As demonstrated by the data from NCHS, about 1,658,370 people were newly diagnosed with cancers and about 589,430 cancerous patients died in the year of 2015 [1]. Although the survival rate of cancer patients have been increasing in the last decades, the latest diagnostic approaches with better sensitivity and specificity are needed to accurately detecting and treating cancers [2]. Thus, finding better tumor biomarkers is really important to improve the sensitivity and specificity, increasing the efficiency of detecting and treating cancers.
The galectin (Gal) family is a family of endogenous lectins with high affinity for polysaccharides including β-galactosyl residues and a part of animal lectins in the lectin family. Nowadays, 15 members have been found out in the lectin family, which have highly carbohydrate recognition domain (CRD). Galectin-1 (Gal-1) is a secretion from cells and can bind and cross-link glycoconjugates on the cell surfaces, which includes various integrins and glycoproteins of the extracellular matrix (ECM) [3]. Besides, Gal-1 expression is regularly increased in tumor tissues since it can modulate cell adhesion, migration, survival and signaling [4]. At present, it has been clarified by some clinical studies that the expression of Gal-1 has close association with metastasis, recurrence and bad tumor prognosis, which includes cholangiocarcinoma [5], gastric cancer [6–8], gingival squamous cell carcinoma [9], hepatocellular cancer [10–12], renal cell cancer [13], head and neck squamous cell carcinomas [14], ovarian cancer [15, 16], non-small cell lung cancer [17, 18], classic Hodgkin lymphoma [19], laryngeal squamous cell carcinomas [20], glioblastoma [21, 22] and so on. Nevertheless, we still don’t clearly know the impact of Gal-1 on the consistency and magnitude of the prognosis. Therefore, we combined all those published evidences in a systematical manner so as to expose the relationship of Gal-1 and cancerous patients’ prognosis for different kinds of tumors. We attempted to find out whether Gal-1 could help the treatment and prognosis of cancerous patients.
Materials and methods
This meta-analysis was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [23].
Search strategy
The literature was done via PubMed, Embase and Web of Science databases. Keywords were “carcinoma OR cancer OR neoplasm OR tumor OR tumour” (in all fields) AND “prognostic OR prognosis OR outcome OR survival” (in all fields) AND “Galectin1 OR Galectin-1 OR Gal-1” (in all fields). The latest study was done on March 30, 2018. References of identified literature were also screened to further identify the related researches. Two authors independently searched the database. (Wu Rongzu and Wu Tingchun).
Criteria for inclusion and exclusion
The following criteria must be met for those literatures eligible for inclusion in this meta-analysis:
Gal-1’s expression in cancer tissue.
Investigating the association between the level of expression of Gal-1 and survival outcome, which includes overall survival (OS), cancer-specific survival (CSS), disease-free survival (DFS), relapse-free survival (RFS) or progression-free survival (PFS).
Offering enough data for the estimation of HR and 95% CI.
When several researches found out the same patient cohort, the whole or the latest cohort was included, with the exclusion of letters, editorials, expert opinions, reviews, case reports and non-human trials. Some researches without critical data for comprehensive analysis were also excluded. Besides, researches with sample sizes less than 40 were not included. The titles and abstracts of determined literatures were independently assessed by two viewers and the irrelevant literature was excluded. The enrolled articles were comprehensively evaluated and further screened by carefully viewing the whole text. Disagreement (if any) was resolved with negotiation.
Data extraction and quality assessment
Two researchers independently collected the required data from all available studies, including surname of the first author, the date of publication, origin of population, type of tumors, size of sample, mean or median age, gender of patients, stage of tumor, cut-off value, methods for tumor detection, results, and HR and 95% CI of the high Gal-1 expression group versus the low Gal-1 expression group for OS, CSS, DFS, and RFS, if applicable. For those studies without HRs, the survival information was extracted from the raw data (Kaplan–Meier curves) by applying the Engauge Digitizer 4.1, and the data about survival rate was calculated with Tierney’s method [24]. If both the results of univariate and multivariate analysis were reported in a study, only the latter was chosen since its accuracy increased when the confounding factors were considered.
By referring to the Newcastle–Ottawa quality assessment scale (NOS), two reviewers evaluated each study’s quality systematically and independently [25]. A score of 0 was regarded as the poorest quality while 9 the highest quality. A study whose score was no less than six shall be considered as high quality.
Statistical analysis
The definition of high expression of Gal-1 was made based on the cut-off values given by the authors. The association between Gal-1 expression and cancerous patients’ prognosis was described applying the pooled HRs and their 95% CIs. The evaluation of heterogeneity was made by applying Cochran’s Q test and Higgins I-squared statistics. I2 > 50% and/or P < 0.1 suggested a obvious heterogeneity in terms of statistics, according to which a random effect model could be utilized. Alternatively, a model with fixed-effect was needed. If there was the heterogeneity, its source should be explored through the subgroup analysis. The sensitivity analysis was done by omission of each single study so as to evaluate the stability of results. The publication bias was assessed via the Begg and Egger funnel plot. In this meta-analysis, STATA software version 12.0 (Stata Corporation, College Station, TX, USA) was applied. A P-value < 0.05 could suggest statistical significance.
Results
Study characteristics
As for the strategy used for search, totally 253 references were retrieved at the beginning. When the titles, abstracts, types of publication and overall text were comprehensively screened, the relationship between Gal-1 expression and the outcomes of patients with various malignant tumors were studied in 33 articles. In addition, 15 articles were not included (Gal-1 was detected not in tumor tissue in 8 articles, some key data were lacked in 2 articles, the sample size of 1 articles was less than 40, Only DSS (not OS) was discussed in 3 articles while DFS (not OS) was discussed in 1 article. Eventually, 18 articles were added into the meta-analysis when the comprehensive assessment was done (Fig. 1). Totally 2674 patients from China, Japan, Hungary, Argentina, Belgium, Germany, Denmark and USA were diagnosed with different cancers, such as cholangiocarcinoma, gastric cancer, gingival squamous cell carcinoma, hepatocellular cancer, renal cell cancer, head and neck squamous cell carcinomas, ovarian cancer, non-small cell lung cancer, classic Hodgkin lymphoma, laryngeal squamous cell carcinomas, glioblastoma and so on. The design of all studies was done retrospectively and the year of publication was between 2005 and 2018. 12 studies targeted Asians while six Caucasians. Totally 18 studies reported OS, while CSS and DFS were assessed only in two studies. OS was selected as the major survival outcome for all of the available studies in our meta-analysis. 7 studies reported HRs with their 95% CIs. Through the graphical survival plots, the data was extracted in 11 studies. The cut-off values of Gal-1 differed in different studies. Table 1 demonstrates the significant features of these 18 available studies. Figure 2 is show how different tumor types are distributed amongst studies and patients.
Fig. 1.
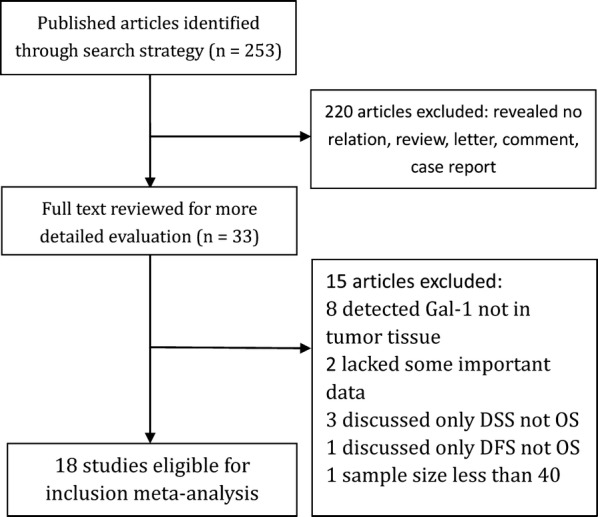
Study identification flowchart
Table 1.
Main characteristics of all studies included in the meta-analysis
| Study | Country | Cancer | Case number | Median age (year, range) | M/F | Stage | Gal-1 (±) NO. | Cut-off | Multivariate analysis | HR and 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|
| Wu [5] | Japan | CCA | 78 | NA | 50/28 | TNM I–IV | (45/33) | IRS ≥ 3 | No | SC |
| Chen [6] | China | gastric | 214 | Mean 64.5 | 129/85 | TNM I–IV | (138/76) | IRS ≥ 2 | No | SC |
| Noda [9] | Japan | GSCC | 80 | Mean 63.8 | 39/41 | TNM I–IV | (22/58) | IHC > 50% | No | SC |
| Chong [8] | China | Gastric | 111 | NA | NA | TNM I–IV | (61/50) | IHC > 20% | No | SC |
| Zhang [10] | China | HCC | 209 | NA | 179/30 | TNM I–IV | (128/81) | IHC > 20% | No | SC |
| Huang [13] | Tainan | RCC | 45 | NA | 31/14 | TNM I–IV | (25/20) | H-score > median | No | SC |
| Le [14] | USA | HNSCC | 101 | Median 58 | 84/17 | TNM I–IV | (56/44) | IRS ≥ 3 | No | SC |
| Schulz [15] | Germany | Ovarian | 150 | Median 62 (31–88) | 0/150 | FIGO I–IV | (102/48) | IRS > 1 | No | SC |
| Chen [7] | China | Gastric | 108 | NA | 61/47 | TNM I–IV | (68/40) | IRS ≥ 2 | Yes | Report |
| You [11] | China | HCC | 162 | NA | 127/35 | TNM I–IV | (105/57) | IRS ≥ 2 | Yes | Report |
| Wu [12] | China | HCC | 386 | NA | 341/45 | TNM I–IV | (189/197) | NA | Yes | Report |
| Kamper [19] | Denmark | cHL | 143 | 35 | 78/80 | Ann Arbor I–IV | (35/108) | NA | No | Report |
| Ye [20] | China | LSCC | 187 | Mean 52.4 | 179/8 | TNM I–IV | (102/85) | NA | No | SC |
| Szoke [17] | Hungary | NSCLC | 94 | Mean 58.8 | 84/10 | TNM I–III | (40/54) | NA | No | SC |
| Carlini [18] | Argentina | NSCLC | 103 | Median 64 (45–85) | 69/34 | TNM I–III | (53/47) | IRS > 1 | No | SC |
| Van Woensel [21] | Belgium | GBM | 349 | NA | NA | NA | (174/175) | Median gene expression | No | Report |
| Chou [22] | China | GBM | 45 | NA | 27/18 | NA | (34/11) | IHC > 35% | No | Report |
| Chen [16] | China | EOC | 109 | NA | 0/109 | FIGO | (91/18) | IRS ≥ 3 | Yes | Report |
CCA cholangiocarcinoma, GSCC gingival squamous cell carcinoma, HCC hepatocellular carcinoma, RCC renal cell carcinoma, HNSCC head and neck squamous cell carcinomas, cHL classic Hodgkin lymphoma, LSCC laryngeal squamous cell carcinomas, NSCLC non-small cell lung cancer, GBM glioblastoma multiforme, EOC epithelial ovarian cancer, NA not available, SC survival curve, IRS immunoreactivity score, IHC immunohistochemistry
Fig. 2.
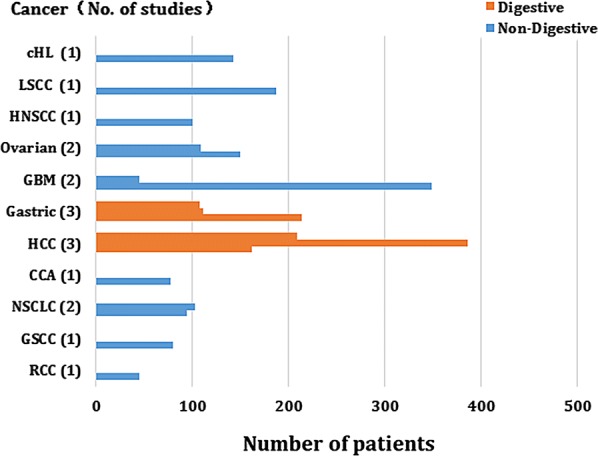
Tumor types are distributed amongst studies and patients. CCA cholangiocarcinoma, GSCC gingival squamous cell carcinoma, HCC hepatocellular carcinoma, RCC renal cell carcinoma, HNSCC head and neck squamous cell carcinomas, cHL classic Hodgkin lymphoma, LSCC laryngeal squamous cell carcinomas, NSCLC non-small cell lung cancer, GBM glioblastoma multiforme
Quality assessment
The quality of all those 18 available studies in our meta-analysis was evaluated based on the NOS. The selection bias was observed in each and every study, maybe because only a single type of cancer was included in each study. Therefore, any study in this meta-analysis failed to represent the whole range of cancers. The study quality was between 6 and 7, with a mean value of 6.6. A larger value suggested a better methodology. Thus, the subsequent analysis included all available studies.
Meta-analysis results
Table 2 demonstrates the main results of this meta-analysis. Since the studies which evaluated OS have significant statistical heterogeneity (I2 = 43.6%, P = 0.025), a model with random-effects was applied to get the HRs pooled. As shown by the statistical results, high expression of Gal-1 is obviously correlated with poor OS in various carcinomas, with the pooled HR of (HR = 1.79, 95% CI 1.54–2.08, P < 0.001) (Fig. 3).
Table 2.
The pooled associations between Gal-1 expression and the prognosis of cancerous patients (OS)
| Outcome subgroup | No. of studies | No. of patients | HR (95% CI) | P value | Model | Heterogeneity | |
|---|---|---|---|---|---|---|---|
| I2 (%) | P | ||||||
| All | 18 | 2674 | 1.79 (1.54–2.08) | < 0.001 | Random | 43.6 | 0.025 |
| Ethnicity | |||||||
| Asian | 12 | 1734 | 1.96 (1.60–2.42) | < 0.001 | Random | 50.5 | 0.023 |
| Caucasian | 6 | 940 | 1.42 (1.21–1.66) | < 0.001 | Fixed | 0.00 | 0.716 |
| Tumor type | |||||||
| Digestive system | 7 | 1268 | 1.94 (1.64–2.30) | < 0.001 | Fixed | 20.1 | 0.276 |
| NOT digestive system | 11 | 1406 | 1.61 (1.33–1.94) | < 0.001 | Random | 42.5 | 0.066 |
| Analysis type | |||||||
| Univariate | 18 | 2674 | 1.79 (1.54–2.09) | < 0.001 | Random | 50.0 | 0.008 |
| Multivariate | 4 | 765 | 1.93 (1.60–2.32) | < 0.001 | Fixed | 0.00 | 0.572 |
| HR obtained method | |||||||
| Reported in text | 7 | 1302 | 1.77 (1.42–2.20) | < 0.001 | Random | 49.2 | 0.066 |
| Data extrapolated | 11 | 1372 | 1.77 (1.42–2.20) | < 0.001 | Random | 47.6 | 0.039 |
Fig. 3.
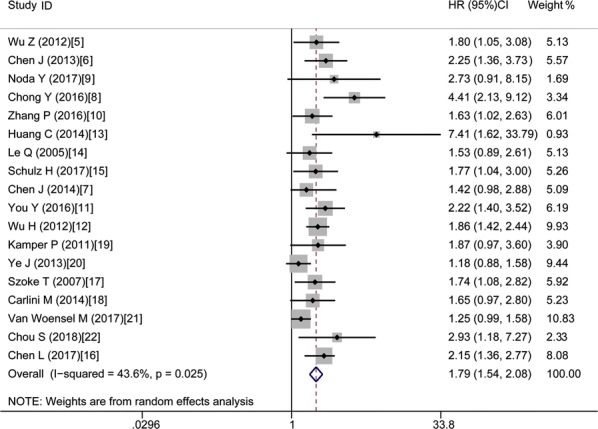
Forest plots of studies assessing HR of high Gal-1 expression in cancers
In order to study these studies’ heterogeneity, subgroup analysis was done on the basis of four important characteristics, i.e. type of tumor, ethnicity, type of analysis and methods used for obtaining HR. In the subgroup of tumor type, it’s observed that high Gal-1 expression was correlated with poor OS in digestive cancers without heterogeneity (HR = 1.94, 95% CI 1.64–2.30, P < 0.001; fixed-effects model; I2 = 20.1%, P = 0.276) (Fig. 4a) and in not digestive cancers with obvious heterogeneity (HR = 1.61, 95% CI 1.33–1.94, P < 0.001; random-effects model; I2 = 42.5%, P = 0.066) (Fig. 4b). In the subgroup of Caucasian, there is also without heterogeneity, with the pooled HR of (HR = 1.42, 95% CI 1.21–1.66, P < 0.001; fixed-effects model; I2 = 0.00%, P = 0.716) (Fig. 5b). However, in other subgroups, the correlation between high Gal-1 expression and poor OS have statistical significance but with obvious statistical heterogeneity, including Asians (HR = 1.96, 95% CI 1.60–2.42, P < 0.001; model with random-effects; I2 = 50.5%, P = 0.023) (Fig. 5a), data extrapolated (HR = 1.77, 95% CI 1.42–2.20, P < 0.001; random-effects model, I2 = 47.6%, P = 0.039), reported in text (HR = 1.77, 95% CI 1.42–2.20, P < 0.001; random-effects model; I2 = 49.2%, P = 0.066), univariate analysis (HR = 1.79, 95% CI 1.54–2.09, P < 0.001; random-effects model; I2 = 50.0%, P = 0.008), Only multivariate analysis with no heterogeneity (HR = 1.93, 95% CI 1.60–2.32, P < 0.001; fixed-effects model; I2 = 0.0%, P = 0.572) (Table 2).
Fig. 4.
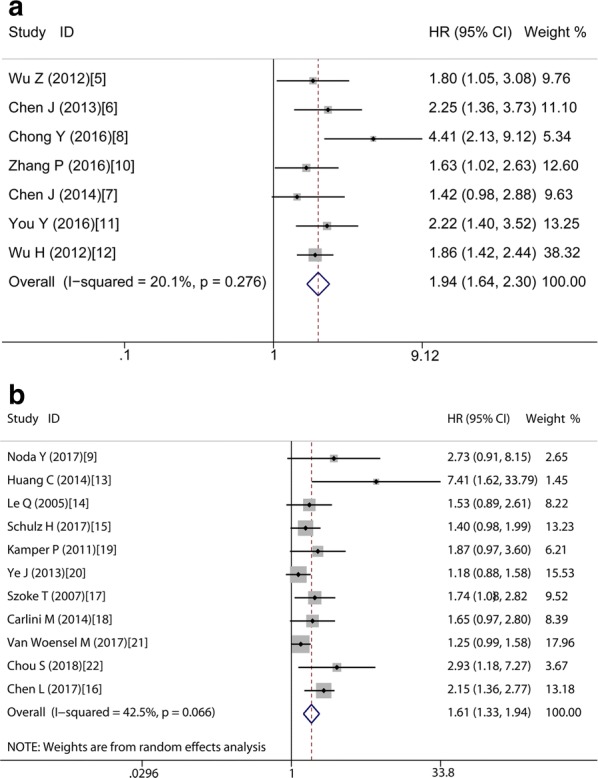
Forest plots of studies assessing HR of high Gal-1 expression in digestive cancers (a) and not digestive cancers (b)
Fig. 5.
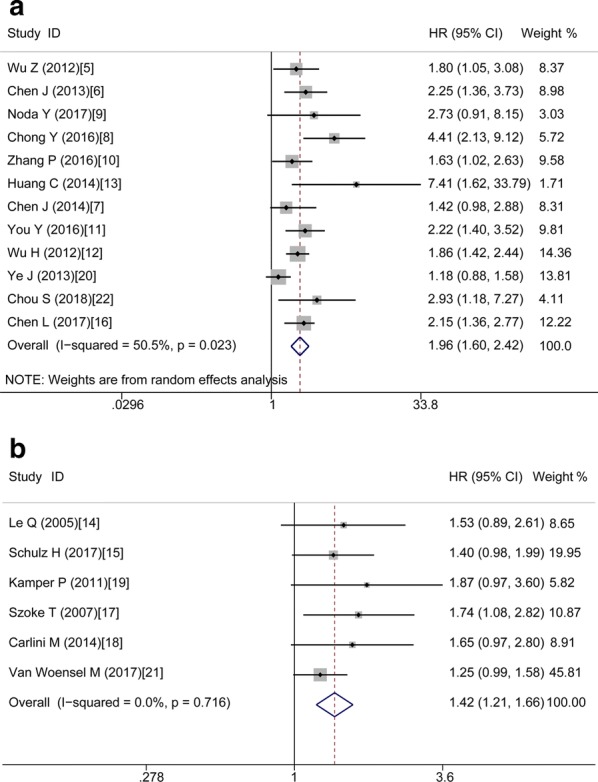
Forest plots of studies assessing HR of high Gal-1 expression in Asian (a) and Caucasian (b)
Sensitivity analysis
Sensitivity analysis was done through the sequential omission of single studies using a model with fixed-effects, and the result pattern was not obviously impacted by any single study (Fig. 6).
Fig. 6.
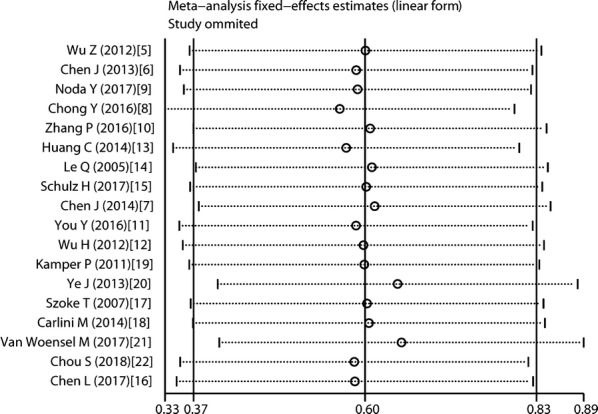
Sensitivity analysis for meta-analysis Gal-1
Publication bias
The assessment of the publication bias for OS was done through Begg’s funnel plot and Egger’s test. The shape of the funnel plot revealed some evidence of asymmetry (OS, P = 0.103 for the Begg’s test, P = 0.002 for the Egger’s test) (Fig. 7). After adjustment with the trim-and-fill method, the pooled association between Gal-1 expression and OS in tumor patients was also significant (fixed-effects model: HR = 1.49, 95% CI 1.36–1.64, P < 0.001; random model: HR = 1.53, 95% CI 1.30–1.80, P < 0.001), and with significant heterogeneity (P < 0.001). Thus, the results of this meta-analysis are reliable.
Fig. 7.
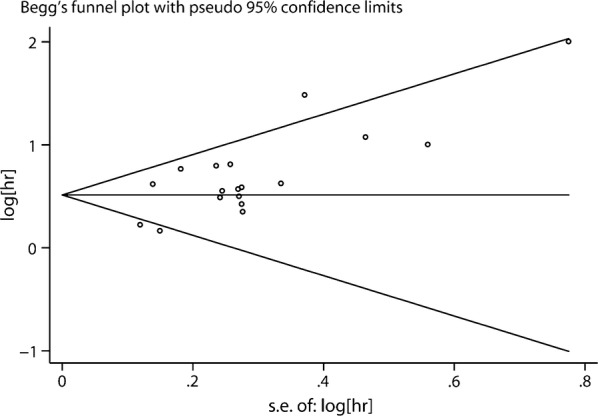
Funnel plots for the evaluation of potential publication bias
Discussion
Although the past decades have witnessed great achievements in preventing and treating cancers, lots of cancers can’t be treated or cured. Two of the major reasons are the lack of effective biomarkers required for early detection and the inefficient treatment of cancers diagnosed at the terminal stages. As shown by many researches, the expression of Gal-1 has statistically clinical significance, indicating Gal-1 might be a potential biomarker for the prognosis of cancers. Gal-1 is the prototype member of the Galectin superfamily, with the characteristics of high affinity binding to β-galactosides via a well-conserved carbohydrate recognition domain (CRD) [26]. Gal-1 can bind and cross-link glycoconjugates on the cell surfaces and regulate various biological processes, such as T cell homeostasis, resolution of inflammatory responses, host–pathogen interactions, selective deletion of specific thymocytes during T cell development, fetomaternal tolerance, and embryogenesis [3, 27–29]. Besides, it’s known that high levels of Gal-1 expressed broadly over primary tumor sections via immunohistochemistry [30–32]. In the tumor microenvironment, Gal-1’s upregulation benefits the tumor growth and reinforces the tumor progression by the modulation of cell motility [33], inducing apoptosis of activated T cells [34], mediation of cell adhesion [35], and participation in tumor angiogenesis [36]. Besides, intracellular Gal-1 links oncogenic H-Ras to promote its anchorage to plasma membrane and stimulate the extracellular signal-regulated kinase (ERK) signaling pathway for neoplastic transformation [37]. Indeed, in most of the clinical studies, it’s reported the raised level of Gal-1 is connected to the poor prognosis [7, 11, 13, 20, 22]. On the other hand, although the relationship between Gal-1 expression and tumorigenesis has been studied intensively, no comprehensive analysis is done for the available data. Therefore, the consistency and scope regarding Gal-1’s prognostic impact are unknown. As far as we know, except this one, there is no other meta-analysis focusing on the association between Gal-1 expression and cancerous patients’ survival rate.
This study demonstrates the relationship between high expression of Gal-1 in cancer tissue and a poor OS in cancerous patients with obvious statistical heterogeneity (HR = 1.79, 95% CI 1.54–2.08, P < 0.001; I2 = 43.6%, P = 0.025). Nevertheless, in the analysis of subgroup, the elevated galectin-1 expression was considered as a bad prognostic marker in cancerous patients for OS, regardless of the kind of tumor, ethnicity, the kind of analysis and the method of obtaining HR. In particular, no obvious statistical heterogeneity is observed in digestive cancers, Caucasian and multivariate analysis (I2 < 50%, P > 0.1). Thus, we believe that the heterogeneity of this meta-analysis mainly due to the difference in tumor type, patient, and type of analysis. In addition, all cut-off values are reported in the study, which may also lead to heterogeneity due to the absence of uniform standards. In summary, Gal-1 might function as a poor prognostic biomarker for cancerous patients, in particular, those of digestive origin and Caucasian.
This study is limited on several aspects. First, because of the missing of a unified cut-off value in Gal-1 expression, various cut-off values are utilized. This possibly exerts influences on the validity of Gal-1 as a predictive marker in the prognosis of cancer. Second, some HRs were computed according to the data gained from the survival curves, which unavoidably contributes to minor statistical errors. Finally, significant heterogeneity was shown, possibly because of the differences in patient origin, date of publication, kind of tumor, tumor stage, method used in the experiment, follow-up time, cut-off values and others. Since the current analysis has some limitations, more excellently-designed large-sized researches including more kinds of tumor should be done in the future.
Conclusions
This meta-analysis combined all researches, and attempted to study the relationship between the high expression of Gal-1 and the survival rate of cancerous patients. High Gal-1 expression can be used as a poor prognostic marker for tumors. This conclusion should be regarded carefully since the current analysis has some limitations. Given the sparse data, additional studies regarding Gal-1 are warranted.
Authors’ contributions
WR collected and analyzed the data, wrote the paper; TW analyzed the data; KW conceived and designed this study, analyzed the data; and all authors reviewed the paper. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank the researchers and study participants for their contributions.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Consent for publication
Consent for publication was obtained from the participants.
Ethics approval and consent to participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (the Institutional Ethics Committee of the Third Affiliated Hospital of Soochow University) and with the Helsinki Declaration of 1964 and later versions.
Funding
This work was supported by the Youth Medical Talent Project of Jiangsu Province (QNRC2016292), China Postdoctoral Science Foundation (Grant No. 63, 2018M632371) and the Natural Science Foundation of Jiangsu Province (Grant Nos. BK20141161 and BK20150251). We thank AJE for its linguistic assistance during the preparation of this manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- HR
hazard ratio
- 95% CI
95% confidence interval
- CCA
cholangiocarcinoma
- GSCC
gingival squamous cell carcinoma
- HCC
hepatocellular carcinoma
- RCC
renal cell carcinoma
- HNSCC
head and neck squamous cell carcinomas
- cHL
classic Hodgkin lymphoma
- LSCC
laryngeal squamous cell carcinomas
- NSCLC
non-small cell lung cancer
- GBM
glioblastoma multiforme
- EOC
epithelial ovarian cancer
- NA
not available
- SC
survival curve
- IRS
immunoreactivity score
- IHC
immunohistochemistry
- OS
overall survival
- CSS
cancer-specific survival
- DFS
disease-free survival
- RFS
relapse-free survival
- PFS
progression-free survival
- DSS
disease-specific survival
Contributor Information
Rongzu Wu, Email: rongzu0902@163.com.
Tingchun Wu, Email: m13912315268@163.com.
Kai Wang, Email: 384503852@qq.com.
Shicheng Luo, Email: 1768222120@qq.com.
Zhen Chen, Email: 1250239983@qq.com.
Min Fan, Email: fm765@126.com.
Dong Xue, Email: xuedongdx@163.com.
Hao Lu, Email: 1195904753@qq.com.
Qianfeng Zhuang, Email: zhuangqianfeng19@163.com.
Xianlin Xu, Email: xuxianlincz@163.com.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Paul D, Kumar A, Gajbhiye A, Santra MK, Srikanth R. Mass spectrometry-based proteomics in molecular diagnostics: discovery of cancer biomarkers using tissue culture. Biomed Res Int. 2013;2013:783131. doi: 10.1155/2013/783131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Camby I, Le Mercier M, Lefranc F, Kiss R. Galectin-1: a small protein with major functions. Glycobiology. 2006;16(11):137R–157R. doi: 10.1093/glycob/cwl025. [DOI] [PubMed] [Google Scholar]
- 4.Elola MT, Wolfenstein-Todel C, Troncoso MF, Vasta GR, Rabinovich GA. Galectins: matricellular glycan-binding proteins linking cell adhesion, migration, and survival. Cell Mol Life Sci CMLS. 2007;64(13):1679–1700. doi: 10.1007/s00018-007-7044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, Boonmars T, Nagano I, Boonjaraspinyo S, Pinlaor S, Pairojkul C, Chamgramol Y, Takahashi Y. Alteration of galectin-1 during tumorigenesis of Opisthorchis viverrini infection-induced cholangiocarcinoma and its correlation with clinicopathology. Tumour Biol. 2012;33(4):1169–1178. doi: 10.1007/s13277-012-0360-0. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Zhou SJ, Zhang Y, Zhang GQ, Zha TZ, Feng YZ, Zhang K. Clinicopathological and prognostic significance of galectin-1 and vascular endothelial growth factor expression in gastric cancer. World J Gastroenterol. 2013;19(13):2073–2079. doi: 10.3748/wjg.v19.i13.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen J, Tang D, Wang S, Li QG, Zhang JR, Li P, Lu Q, Niu G, Gao J, Ye NY, et al. High expressions of galectin-1 and VEGF are associated with poor prognosis in gastric cancer patients. Tumour Biol. 2014;35(3):2513–2519. doi: 10.1007/s13277-013-1332-8. [DOI] [PubMed] [Google Scholar]
- 8.Chong Y, Tang D, Xiong Q, Jiang X, Xu C, Huang Y, Wang J, Zhou H, Shi Y, Wu X, et al. Galectin-1 from cancer-associated fibroblasts induces epithelial-mesenchymal transition through beta1 integrin-mediated upregulation of Gli1 in gastric cancer. J Exp Clin Cancer Res. 2016;35(1):175. doi: 10.1186/s13046-016-0449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noda Y, Kishino M, Sato S, Hirose K, Sakai M, Fukuda Y, Murakami S, Toyosawa S. Galectin-1 expression is associated with tumour immunity and prognosis in gingival squamous cell carcinoma. J Clin Pathol. 2017;70(2):126–133. doi: 10.1136/jclinpath-2016-203754. [DOI] [PubMed] [Google Scholar]
- 10.Zhang PF, Li KS, Shen YH, Gao PT, Dong ZR, Cai JB, Zhang C, Huang XY, Tian MX, Hu ZQ, et al. Galectin-1 induces hepatocellular carcinoma EMT and sorafenib resistance by activating FAK/PI3K/AKT signaling. Cell Death Dis. 2016;7:e2201. doi: 10.1038/cddis.2015.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.You Y, Tan JX, Dai HS, Chen HW, Xu XJ, Yang AG, Zhang YJ, Bai LH, Bie P. MiRNA-22 inhibits oncogene galectin-1 in hepatocellular carcinoma. Oncotarget. 2016;7(35):57099–57116. doi: 10.18632/oncotarget.10981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu H, Chen P, Liao R, Li YW, Yi Y, Wang JX, Sun TW, Zhou J, Shi YH, Yang XR, et al. Overexpression of galectin-1 is associated with poor prognosis in human hepatocellular carcinoma following resection. J Gastroenterol Hepatol. 2012;27(8):1312–1319. doi: 10.1111/j.1440-1746.2012.07130.x. [DOI] [PubMed] [Google Scholar]
- 13.Huang CS, Tang SJ, Chung LY, Yu CP, Ho JY, Cha TL, Hsieh CC, Wang HH, Sun GH, Sun KH. Galectin-1 upregulates CXCR4 to promote tumor progression and poor outcome in kidney cancer. J Am Soc Nephrol. 2014;25(7):1486–1495. doi: 10.1681/ASN.2013070773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le QT, Shi G, Cao H, Nelson DW, Wang Y, Chen EY, Zhao S, Kong C, Richardson D, O’Byrne KJ, et al. Galectin-1: a link between tumor hypoxia and tumor immune privilege. J Clin Oncol. 2005;23(35):8932–8941. doi: 10.1200/JCO.2005.02.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulz H, Schmoeckel E, Kuhn C, Hofmann S, Mayr D, Mahner S, Jeschke U. Galectins-1, -3, and -7 are prognostic markers for survival of ovarian cancer patients. Int J Mol Sci. 2017;18(6):1230. doi: 10.3390/ijms18061230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen L, Yao Y, Sun L, Tang J. Galectin-1 promotes tumor progression via NF-kappaB signaling pathway in epithelial ovarian cancer. J Cancer. 2017;8(18):3733–3741. doi: 10.7150/jca.20814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szoke T, Kayser K, Trojan I, Kayser G, Furak J, Tiszlavicz L, Baumhakel JD, Gabius HJ. The role of microvascularization and growth/adhesion-regulatory lectins in the prognosis of non-small cell lung cancer in stage II. Eur J Cardiothorac Surg. 2007;31(5):783–787. doi: 10.1016/j.ejcts.2007.01.072. [DOI] [PubMed] [Google Scholar]
- 18.Carlini MJ, Roitman P, Nunez M, Pallotta MG, Boggio G, Smith D, Salatino M, Joffe ED, Rabinovich GA, Puricelli LI. Clinical relevance of galectin-1 expression in non-small cell lung cancer patients. Lung cancer. 2014;84(1):73–78. doi: 10.1016/j.lungcan.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 19.Kamper P, Ludvigsen M, Bendix K, Hamilton-Dutoit S, Rabinovich GA, Moller MB, Nyengaard JR, Honore B, d’Amore F. Proteomic analysis identifies galectin-1 as a predictive biomarker for relapsed/refractory disease in classical Hodgkin lymphoma. Blood. 2011;117(24):6638–6649. doi: 10.1182/blood-2010-12-327346. [DOI] [PubMed] [Google Scholar]
- 20.Ye J, Liu H, Hu Y, Wan G, Li J, Wang Z, Li P, Zhang G, Li Y. The clinical implication of tumoral Gal-1 expression in laryngeal squamous cell carcinomas. Clin Transl Oncol. 2013;15(8):608–618. doi: 10.1007/s12094-012-0975-z. [DOI] [PubMed] [Google Scholar]
- 21.Van Woensel M, Mathivet T, Wauthoz N, Rosiere R, Garg AD, Agostinis P, Mathieu V, Kiss R, Lefranc F, Boon L, et al. Sensitization of glioblastoma tumor micro-environment to chemo- and immunotherapy by galectin-1 intranasal knock-down strategy. Sci Rep. 2017;7(1):1217. doi: 10.1038/s41598-017-01279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chou SY, Yen SL, Huang CC, Huang EY. Galectin-1 is a poor prognostic factor in patients with glioblastoma multiforme after radiotherapy. BMC Cancer. 2018;18(1):105. doi: 10.1186/s12885-018-4025-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 26.Barondes SH, Castronovo V, Cooper DN, Cummings RD, Drickamer K, Feizi T, Gitt MA, Hirabayashi J, Hughes C, Kasai K, et al. Galectins: a family of animal beta-galactoside-binding lectins. Cell. 1994;76(4):597–598. doi: 10.1016/0092-8674(94)90498-7. [DOI] [PubMed] [Google Scholar]
- 27.Blois SM, Ilarregui JM, Tometten M, Garcia M, Orsal AS, Cordo-Russo R, Toscano MA, Bianco GA, Kobelt P, Handjiski B, et al. A pivotal role for galectin-1 in fetomaternal tolerance. Nat Med. 2007;13(12):1450–1457. doi: 10.1038/nm1680. [DOI] [PubMed] [Google Scholar]
- 28.Rabinovich GA, Ramhorst RE, Rubinstein N, Corigliano A, Daroqui MC, Kier-Joffe EB, Fainboim L. Induction of allogenic T-cell hyporesponsiveness by galectin-1-mediated apoptotic and non-apoptotic mechanisms. Cell Death Differ. 2002;9(6):661–670. doi: 10.1038/sj.cdd.4401009. [DOI] [PubMed] [Google Scholar]
- 29.Zuniga E, Gruppi A, Hirabayashi J, Kasai KI, Rabinovich GA. Regulated expression and effect of galectin-1 on Trypanosoma cruzi-infected macrophages: modulation of microbicidal activity and survival. Infect Immun. 2001;69(11):6804–6812. doi: 10.1128/IAI.69.11.6804-6812.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiang WF, Liu SY, Fang LY, Lin CN, Wu MH, Chen YC, Chen YL, Jin YT. Overexpression of galectin-1 at the tumor invasion front is associated with poor prognosis in early-stage oral squamous cell carcinoma. Oral Oncol. 2008;44(4):325–334. doi: 10.1016/j.oraloncology.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Kim HJ, Jeon HK, Cho YJ, Park YA, Choi JJ, Do IG, Song SY, Lee YY, Choi CH, Kim TJ, et al. High galectin-1 expression correlates with poor prognosis and is involved in epithelial ovarian cancer proliferation and invasion. Eur J Cancer. 2012;48(12):1914–1921. doi: 10.1016/j.ejca.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Saussez S, Cucu DR, Decaestecker C, Chevalier D, Kaltner H, Andre S, Wacreniez A, Toubeau G, Camby I, Gabius HJ, et al. Galectin 7 (p53-induced gene 1): a new prognostic predictor of recurrence and survival in stage IV hypopharyngeal cancer. Ann Surg Oncol. 2006;13(7):999–1009. doi: 10.1245/ASO.2006.08.033. [DOI] [PubMed] [Google Scholar]
- 33.Camby I, Belot N, Lefranc F, Sadeghi N, de Launoit Y, Kaltner H, Musette S, Darro F, Danguy A, Salmon I, et al. Galectin-1 modulates human glioblastoma cell migration into the brain through modifications to the actin cytoskeleton and levels of expression of small GTPases. J Neuropathol Exp Neurol. 2002;61(7):585–596. doi: 10.1093/jnen/61.7.585. [DOI] [PubMed] [Google Scholar]
- 34.Kovacs-Solyom F, Blasko A, Fajka-Boja R, Katona RL, Vegh L, Novak J, Szebeni GJ, Krenacs L, Uher F, Tubak V, et al. Mechanism of tumor cell-induced T-cell apoptosis mediated by galectin-1. Immunol Lett. 2010;127(2):108–118. doi: 10.1016/j.imlet.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 35.Horiguchi N, Arimoto K, Mizutani A, Endo-Ichikawa Y, Nakada H, Taketani S. Galectin-1 induces cell adhesion to the extracellular matrix and apoptosis of non-adherent human colon cancer Colo201 cells. J Biochem. 2003;134(6):869–874. doi: 10.1093/jb/mvg213. [DOI] [PubMed] [Google Scholar]
- 36.Thijssen VL, Postel R, Brandwijk RJ, Dings RP, Nesmelova I, Satijn S, Verhofstad N, Nakabeppu Y, Baum LG, Bakkers J, et al. Galectin-1 is essential in tumor angiogenesis and is a target for antiangiogenesis therapy. Proc Natl Acad Sci USA. 2006;103(43):15975–15980. doi: 10.1073/pnas.0603883103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paz A, Haklai R, Elad-Sfadia G, Ballan E, Kloog Y. Galectin-1 binds oncogenic H-Ras to mediate Ras membrane anchorage and cell transformation. Oncogene. 2001;20(51):7486–7493. doi: 10.1038/sj.onc.1204950. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.


