Abstract
The Young Men’s Health Project (YMHP) has shown efficacy in reducing drug use and condomless anal sex (CAS) with casual partners among young gay, bisexual and other men who have sex with men (YGBMSM). The study examined whether relationship status at the time of intervention predicted response to YMHP by comparing baseline (pre-intervention) and follow-up (3-, 6-, 9, and 12-months post-intervention) data from the original trial. A group of 13 partnered YGBMSM who received YMHP was compared to a matched subsample of single YGBMSM. Among single men, drug use declined significantly at all follow-ups. Among partnered men, drug use was largely stable. While significant reductions were observed at 9 month assessment, 3, 6, and 12 month use did not differ significantly from baseline. Regardless of relationship status, CAS with casual partners declined significantly at 12-month follow-up. Results suggest the incorporation of components which address relationship factors, particularly those associated with drug use, may enhance benefits of YMHP for partnered YGBMSM.
Keywords: HIV prevention, drug use, gay and bisexual men, gay and bisexual couples
INTRODUCTION
Rates of HIV infection among gay, bisexual, and other men who have sex with men (GBMSM) rose 12% from an estimated 27,394 cases in 2009 to 30,689 cases in2012[1]. In 2015, GBMSM accounted for 67% of new HIV infections (approximately 26,636 of 40,040 reported cases) and rates were highest among younger GBMSM (YGBMSM). Men between 20 and 29 accounted for approximately 43.5% (or 11,491) of the 26,376 infections attributed to male sexual contact accounted in 2015[2]. Exacerbating their risk for HIV infection, rates of substance use are higher among GBMSM relative to their heterosexual counterparts[3–7]. YGBMSM in particular use drugs at higher rates than older GBMSM[8] and heterosexual men their same-age[3, 9].
The co-occurrence of elevated HIV risk and drug use among YGBMSM may arise in part because these two health-related outcomes are linked to one another. Numerous studies examining aggregate data have found that GBMSM who use drugs are more likely to engage in condomless anal sex (CAS)[10, 11]. The association between substance use and sexual risk behavior has also been documented among YGBMSM specifically[12, 13]. Studies of YGBMSM utilizing event level data to examine the occurrence of sex on specific days when drug use occurs have shown that the association between drug use and CAS was strong and significant[14, 15].
To date, the Young Men’s Health Project (YMHP) [14] is the only intervention to show significant reductions in drug use and CAS with casual partners among HIV-negative YGBMSM in an efficacy trial. A casual partner refers to any sexual partner outside of a primary romantic relationship. This would include any casual partner for those YGBMSM who identify their relationship status as “single” and any partner other than the identified main partner for those YGBMSM in relationships. Parsons et al. [14] conducted a randomized control trial (RCT) involving 143 HIV-negative, sexually active YGBMSM (ages 18 to 29) who reported recent (past 30 day) drug use. They found that YMHP reduced the odds of drug use, the overall odds of CAS with casual partners, and the odds of CAS with casual partners on days when drugs were used relative to an attention-matched education control condition.
YMHP is a brief – 4-session – intervention based upon the principles of Motivational Interviewing (MI)[14, 16]. Similar MI-based interventions have shown efficacy in targeting substance use and sexual health among youth, including YGBMSM[17–19]. MI is a client-centered approach to discussing a target issue; understanding that issue from a client’s perspective; and subsequently developing plans to achieve identified goals[16]. MI emphasizes the individual’s self-efficacy and autonomous capacity to make well-informed health decisions. It provides a framework for delivering information regarding the target behavior and specific strategies to cultivate motivation for change[16].
YMHP’s primary focus is on sexual HIV transmission risk involving casual partners. Since its development, a growing body of research on partnered YGBMSM has illustrated that drug use and HIV-related sexual risk taking with casual partners are linked to relationship functioning within main or primary partnerships. While there is variability in the literature with respect to how main or primary partnerships are defined, here we use these terms to denote a sexual partner with whom the respondent indicates having an established relationship (e.g., boyfriend, partner, spouse). The influence of partners on health-related behavior generally has been conceptualized within the framework of Couples Interdependence Theory (CIT)[20, 21]. Over the course of relationship development, partners in a relationship must reconcile divergent preferences in order to accomplish joint goals – those which require resources from both partners. This process of accommodation results in a transformation of motivation, wherein individuals begin to consider the consequences of their actions for their relationship in addition to their individual outcomes. This focus on couple-level consequences may lead partners to implement social control strategies to bring one another’s behavior in line with desired goals[21].
Research on CIT processes enacted within gay couples indicates that drug use and HIV-related sexual risk taking are among the behaviors most commonly targeted by partners’ social control efforts[20]. Gay couples frequently utilize sexual agreements – understandings about the boundaries and limitations on sex with partners outside the relationship – as a mechanism to manage HIV-related risk[22, 23]. Research on sexual agreements has typically distinguished between monogamous agreements (those in which sex with partners outside the relationship is not permitted) and non-monogamous agreements (those in which some kinds of sexual behavior with outside partners may occur)[22, 46, 49]. Some have distinguished between subtypes of non-monogamy in which sex with a casual partner may only occur when both main partners are present – termed “monogamish” – and those in which the partners in the primary relationship may have sex with outside partners independently [26].
Research on the behavioral correlates of these agreements illustrates the inter-related nature of drug use and sexual behavior. The use of drugs has been linked to violations of sexual agreements among GBMSM[24]. Monogamous GBMSM are significantly less likely to report substance use than non-monogamous men[25, 26]. In addition, partners in monogamous couples report less between-partner variability in use that men in relationships where one or both partners may have sex with people outside of the relationship[25].
Interventions which reduce HIV-related risk among partnered YGBMSM are of critical importance to addressing the HIV epidemic in the US. Once HIV infection is introduced into one partner in a primary relationship, the likelihood of transmission between partners is very high. Epidemiological studies have estimated that 35–68% of new HIV infections are transmitted between partners in primary (rather than casual) relationships[27, 28]. This risk of infection is greater for young GBMSM (YGBMSM, those 18–29), where main partners are estimated to account for as many as 79% of new infections[27].
CIT theory suggests that primary partners have the potential to shape drug use and sexual health goals as well as the capacity to engage in strategies which may directly influence their partner’s behavior [20, 21]. This raises the possibility that being partnered may meaningfully contextualize YGBMSM’s experience of individual-delivered interventions such as YMHP. YMHP was not developed to address relationship factors, which may be relevant to drug use and sexual health for partnered YGBMSM. This raises the potential that YGBMSM who are in relationships may show a smaller intervention response compared to men who are single.
The purpose of the current study was to examine whether relationship status (being partnered) at the time of YMHP receipt predicted response to the intervention. Consistent with this goal, we utilized data from men who received YMHP as part of the original efficacy trial to test the hypothesis that partnered men would show smaller changes in target outcomes between baseline (pre-intervention) and follow up (post-intervention assessments conducted at 3-, 6-, 9-, and 12-months post baseline) relative to a comparison group of men who were single at the time of intervention receipt. Outcomes examined included drug use instances and CAS with casual partners.
METHODS
Participants and Procedures
This study utilized data from the original YMHP RCT[14]. Eligible participants in the trial were 18–29 years old, resided in the New York City (NYC) metropolitan area, and reported having a negative or unknown HIV status, at least 5 days of drug use (including: cocaine, methamphetamine, gamma hydroxybutyrate, ecstasy, ketamine or poppers) and at least one instance of CAS with a casual partner or an HIV-positive or unknown-status main partner in the 90 days prior to assessment. Additionally, men were excluded if they reported an HIV-positive main partner at baseline or if they reported no anal sex in the 30 days prior to baseline.
Recruitment was ongoing between September 2007 and August 2010. A multi-method campaign – encompassing both active and passive recruitment strategies executed online and in person – was utilized to enroll participants from across the NYC metropolitan area [29, 30]. Most of the YMHP sample, (71%) was recruited through active, in-person recruitment efforts involved recruiters screening potential participants using Palm Pilots at a variety of venues including bars, clubs, sex venues, streets in predominantly gay neighborhoods and LGBT community events. Passive recruitment activities yielded 12% of the sample. These included the distribution of tear-off flyers and project recruitment cards (at venues where active recruitment activities were also carried out) and advertisements placed in both LGBT specific and general publications. An additional 9% of participants were recruited through online-recruitment activities. These included active strategies (in which recruiters entered chat-rooms to distribute study information and links to an online screener) and passive strategies (in which banner advertisements were placed on LGBT websites). Finally, 8% of the sample was recruited through friend-referrals.
Potentially eligible participants identified through recruitment efforts were contacted by phone to complete a more detailed screener. Those who screened eligible were scheduled for a baseline appointment. A detailed review of informed consent was conducted as a first step in the baseline appointment. The appointment then involved the completion of a battery of self-report survey instruments administered through audio computer-assisted self-interview (ACASI) software and an interviewer-administered time-line follow-back (TLFB) interview covering substance use and sexual behavior for the past 30 days. Subsequently, participants were randomly assigned to complete either 4 sessions of MI following the YMHP protocol or 4 sessions of individually delivered education sessions. Participants returned for follow-up assessments at 3-, 6-, 9-, and 12-months post-baseline. Participants were compensated $40 for completion of the 2 hour baseline and $10 for each intervention session. Participants were compensated $45 for the 3-month follow up and compensation increased by $5 for each subsequent follow up. All procedures were approved by the Hunter College Institutional Review Board. The trial was registered with clinicaltrials.gov (NCT# 01118416).
Measures
Demographics
Participants reported their age, race/ethnicity, education level, and income. Relationship status was assessed using a single item which asked, “How do you define your current relationship status?” Participants could select from one of four responses, including: “I am legally married,” “I have a partner or a lover, “”I have a boyfriend or a girlfriend,” or “I am single.” Responses were collapsed to create a dichotomous variable indicate whether a participant indicated being in any kind of relationship (versus being single).
Sexual and Substance Use Behavior
The timeline follow-back (TLFB) semi-structured interview [31] was used to collect day-level information about the occurrence of anal sex, condom use during sexual events, and substance use in the preceding month. Using a calendar, interviewers asked participants to report any days on which substance use occurred. Participants were then asked to report any sexual activity (anal or oral intercourse), condom use (whether or not condoms were used), and partner type (main or casual) on each day of the preceding 1-month period. The current study examined two specific outcome variables: total drug use instances (the number of days a participant reported using cocaine, methamphetamine, GHB, Ketamine, or ecstasy) and the number of condomless anal (insertive or receptive) sex acts with casual partners. The drugs classes included in this outcome variable were selected to be consistent with previous analyses of YMHP outcome data [14]. The original trial focused on these substances because their use was relatively common and frequently reported to occur along with sexual activity among GBMSM at the time the YMHP trial was proposed. Poppers are excluded here to retain consistency with previous studies of the YMHP outcome data which excluded poppers use because it was so prevalent in the YMHP sample overall (87% reported poppers use at baseline). Sensitivity analyses in this analytic sample suggested that the inclusion of poppers had a negligible impact on the significance of overall effects.
YMHP Intervention condition
Participants who received the YMHP condition completed 4 sessions of MI following a structured protocol. Full detail on intervention implementation are available elsewhere[14]. In brief, the intervention had two target behaviors: drug use and HIV-related sexual risk taking. Session 1 focused on establishing rapport, exploring goals and values, and discussing one target behavior selected at the client’s discretion. Session 2 then consisted of a discussion of the target behavior not focused on in session 1. Session 3 emphasized the identification of goals specific to target behaviors and the exploration of steps which might be taken to achieve these goals. Session 4 included relapse prevention and termination.
Statistical Analyses
This article focuses on relationship status as a predictor of response to YMHP over time. In the original trial, 14 partnered YGBMSM received the YMHP intervention. In order to enhance the validity of inferences related to between-group differences between partnered and single men we utilized Case Controlled Matching function available in SPSS v24 to select a matched comparison group of single YGBMSM based upon race and ethnicity (White versus non-White), education (more versus less than a 4 year degree), baseline drug use, and baseline CAS. Matching was done without replacement. Tolerances were set at zero for race and ethnicity as well as education. Tolerances were set at 4 for drug use instances and CAS. Exact matches were identified for 2 participants while “fuzzy” matches were identified for an additional 11. There was one partnered YGBMSM for whom a match could not be identified. This participant was therefore dropped from analyses yielding an analytic sample comprised of 13 partnered YGBMSM and 13 comparison YGBMSM who were single.
Generalized estimating equation (GEE) models [32] were calculated to account for the nesting of observations within people across time. Separate models were calculated for each outcome. Given the count nature of all outcomes of interest, all models specified a negative binomial outcome distribution and utilized a logistic-link function. Each model incorporated the main effect of time as a 5 category predictor (baseline, 3-month, 6-month, 9-month, and 12-month follow-up) represented with 4 dummy codes. Models also included the main effect of being partnered at the time of intervention delivery (a dichotomous variable). The interaction between partnered status at intervention and time involved an additional four dummy codes. The significance of each main effect and the time by partnered status interaction was indicated by Wald χ2 tests for each overall effect. Where tests of overall effects were significant, the significance of regression coefficients associated with specific dummy codes was evaluated using t-tests associated with the respective parameter. Models incorporated dichotomous education as well as race and ethnicity (White versus not-White) variables utilized in the matching procedure. Post hoc sensitivity analyses examined whether results were influenced by the inclusion of relationship status at follow-up (a time-varying predictor) or age. Conclusions were robust to the inclusion of these covariates.
RESULTS
A detailed description of the YMHP recruitment and retention cascade has been published elsewhere[14]. Of the 1,282 individuals reached during recruitment efforts and assessed for eligibility, 175 completed all baseline assessment procedures and were randomized to an intervention condition. Of the 92 who were randomized to the YMHP condition, 19 were subsequently removed from the study after being deemed ineligible post-baseline. This resulted in a final sample of 73 individuals who completed at least one session of the YMHP condition. Within the YMHP condition, retention was high at 3-(83.6%), 6-(74%), 9-(75.3%), and 12-(80.8%) month follow up. Attrition analyses suggested that partnered and single men did not differ in the probability of retention at any follow-up time point within the condition.
Table 1 contains demographic data for the 26 participants included in these analyses. The sample was primarily comprised of men who identified as a racial or ethnic minority (69.2%). Most identified as gay (91.8%), had less than a college degree (84.6%) and earned less than $30,000 per year (84.6%). There were no differences in demographic variables or baseline drug use and sexual behavior between partnered YGBMSM and selected single comparison participants.
Table I.
Demographic characteristics
| Total | Unpartnered | Partnered | Fischer exact test | |
|---|---|---|---|---|
|
|
|
|||
| n (%) | n (%) | n (%) | ||
|
|
|
|
||
| n (%) | 26 (100.0) | 13 (100.0) | 13 (100.0) | |
| Race | 1.00 | |||
| White | 8 (30.8) | 4 (30.8) | 4 (30.8) | |
| Black | 9 (34.6) | 5 (38.5) | 4 (30.8) | |
| Latino | 7 (26.9) | 3 (23.1) | 4 (30.8) | |
| Other | 2 (7.7) | 1 (7.7) | 1 (7.7) | |
| Sexual Orientation | 0.59 | |||
| Gay | 67 (91.8) | 12 (92.3) | 10 (76.9) | |
| Bisexual | 6 (8.2) | 1 (7.7) | 3 (23.1) | |
| Education | 1.00 | |||
| < 4 year degree | 22 (84.6) | 11 (84.6) | 11 (84.6) | |
| 4 year degree or more | 4 (15.4) | 2 (15.4) | 2 (15.4) | |
| Income | 1.00 | |||
| Less than $30,000 | 22 (84.6) | 11 (84.6) | 11 (84.6) | |
| $30,000 or more | 2 (15.4) | 2 (15.4) | 2 (15.4) | |
|
| ||||
| M(SD) | M(SD) | M(SD) | test statistic | |
|
|
|
|
||
| Age | 24.4 (3.0) | 24.1 (3.2) | 24.5 (3.6) | t(24) = 0.18 |
| Drug use Instances | 3.73 (3.9) | 3.9 (3.7) | 3.5 (4.3) | Wald χ2(1) = 0.07 |
| CAI with a casual partner | 2.4 (2.1) | 2.5 (2.1) | 2.3 (2.2) | Wald χ2(1) = 0.04 |
Drug Use Instances
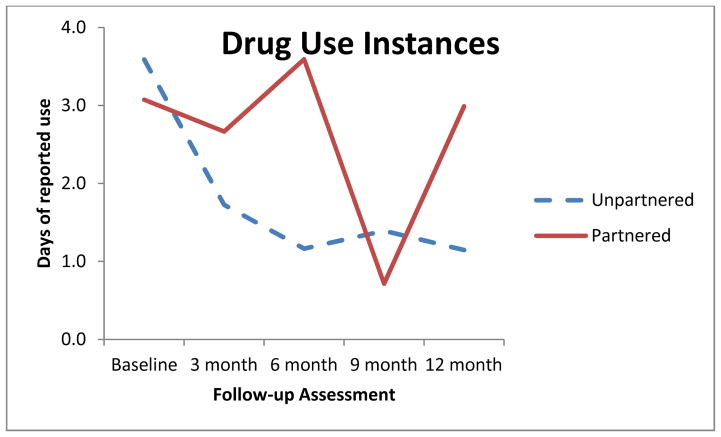
Results of the GEE model predicting drug use instances are displayed in Table 2. There was a significant main effect of time and also a significant relationship status by time interaction. Estimated marginal means are pictured in Figure 1. Examination of specific model parameters revealed that, among single men, the number of drug use instances was significantly lower at all follow up time points compared to baseline. A follow up model calculating the simple main effect of time among partnered men revealed that drug use instances differed from baseline only at the 9-month follow up time point (B = −1.46; 95% CI: −2.51, −0.41; p = .01). Results at 3-(B = −0.14; 95% CI: −0.86, 0.58; p = .70); 6-(B = 0.16; 95% CI: −0.88, 1.20; p = .76); and 12-(B = −0.03; 95% CI: −1.43, 1.37, p = .97) did not differ from baseline.
Table II.
GEE model results: Drug use instances.
| B | 95%CI | expB | overall effect | |
|---|---|---|---|---|
| Intercept | 1.25** | (0.63, 1.87) | 3.48 | Wald χ2 (1) = 10.02** |
| Race (ref = non-white) | 0.67** | (0.26, 1.08) | 1.95 | Wald χ2 (1) = 10.22** |
| Education (ref = < 4 yr degree) | −0.97** | (−1.46, −0.47) | 0.38 | Wald χ2 (1) = 14.70** |
| Partnered status (ref = single) | −0.16 | (−1.00, 0.69) | 0.56 | Wald χ2 (1) = 1.55 |
| Time (ref = baseline) | Wald χ2 (4) = 14.51** | |||
| 3 month | −0.73** | (−1.30, −0.17) | 0.48 | |
| 6 month | −1.13** | (−2.02, −0.23) | 0.33 | |
| 9 month | −0.95* | (−1.72, −0.18) | 0.39 | |
| 12 month | −1.14** | (−1.94, −0.35) | 0.32 | |
| Partnered X Time interaction | Wald χ2 (4) = 10.71** | |||
| 3 month | 0.59 | (−0.32, 2.72) | 1.80 | |
| 6 month | 1.28 | (−1.81, 0.78) | 3.60 | |
| 9 month | −0.51 | (−0.09, 2.65) | 0.60 | |
| 12 month | 1.11 | (−0.32, 1.50) | 3.05 |
p ≤ .05;
p ≤ .01
Figure 1.
Over-time change in drug use instances
CAS with Casual Partners
Table 3 contains results of the GEE model predicting CAS with casual partners. There was a significant main effect of time. The main effect for relationship status and the relationship status by time interaction were both non-significant. A parsimonious model which omitted the non-significant interaction effect revealed that, regardless of relationship status, YGBMSM reported significantly fewer instances of CAS with casual partners at the final follow-up point (B = −1.12; 95% CI: −1.93, −0.30; p = .01). The differences between 3-month, 6-month and 9-month follow-ups and baseline were non-significant (B = −0.46; 95% CI: −1.17, 0.26; p = .21; B = −0.46; 95% CI: −1.11, 0.20; p = .17; B = −0.28; 95% CI: −0.95, 0.40; p = .42), as was the main effect of relationship status (B = 0.39; 95% CI: −0.15, 0.93; p = .16).
Table III.
GEE model results: CAS with casual partners
| B | 95%CI | expB | overall effect | |
|---|---|---|---|---|
| Intercept | 0.88* | (0.38, 1.39) | 2.42 | Wald χ2 (1) = 2.41 |
| Race (ref = non-white) | 0.13 | (−0.38, 0.64) | 1.14 | Wald χ2 (1) = 0.26 |
| Education (ref = < 4 yr degree) | −0.22 | (−0.87, 0.42) | 0.80 | Wald χ2 (1) = 0.46 |
| Partnered status (ref = single) | −0.08 | (−0.72, 0.57) | 0.82 | Wald χ2 (1) = 2.28 |
| Time (ref = baseline) | Wald χ2 (4) = 12.85** | |||
| 3 month | −1.01** | (−1.79, −0.22) | 0.37 | |
| 6 month | −1.48** | (−2.61, −0.35) | 0.23 | |
| 9 month | −0.54 | (−1.59, 0.51) | 0.58 | |
| 12 month | −0.98* | (−1.98, −0.00) | 0.38 | |
| Partnered X Time Interaction | Wald χ2 (4) = 6.08 | |||
| 3 month | 1.04 | (−0.24, 2.31) | 2.82 | |
| 6 month | 1.52** | (0.16, 2.88) | 4.56 | |
| 9 month | 0.54 | (−0.78, 1.86) | 1.72 | |
| 12 month | −0.42 | (−2.11, −1.27) | 0.66 |
p ≤ .05;
p ≤ .01
DISCUSSION
Findings from the current study highlight the unique intervention needs of partnered YGBMSM. Consistent with hypotheses, YGBMSM who were single at intervention showed significant reductions in drug use instances. Similar reductions in drug use were not observed among those YGBMSM who were partnered when they received the YMHP intervention. Contrary to hypotheses, both partnered and single YGBMSM who received YMHP showed significant decreases in CAS with casual partners at the most distal post intervention follow-up.
The observation that YMHP showed uniform effects on CAS regardless of relationship status must be understood in the context of several factors. First, the intervention was designed to address HIV-related sexual risk taking specifically with casual partners[14]. The findings here support the assertion that the intervention’s content in this domain may be adequately broad and flexible to be relevant for participants regardless of relationship status. Second, study inclusion criteria excluded behaviorally monogamous couples[14]. Men in relationships characterized by open agreements report sexual behavior more similar to those of their single counterparts[26]. The study may therefore have included those partnered men who were most able to utilize content from a sexual health intervention designed to focus primarily on sex with casual partners.
The diminished response to intervention for partnered YGBMSM with respect to drug use may arise from a number of factors. Being partnered may influence health-related goals and behavior in a manner not fully encompassed by the existing YMHP intervention. While YMHP incorporates a discussion of broader goals and values, the intervention focuses primarily on the individual-level. It is possible that, in doing so, it fails to fully explore the ways in which the goals and values expressed by the individual receiving YMHP are influenced by his partner’s goals and values through the accommodation process[21]. This might lead to the development of intervention goals which are at odds with couple-level concerns. In addition, YMHP does not incorporate an explicit examination of how the actions of partners may reinforce or discourage engagement in the target behaviors (drug use and HIV-related sexual risk taking). The intervention may therefore miss aspects of behavioral motivation that are specifically relevant for partnered YGBMSM.
Communication is inherent in the concept of the accommodation process and the notion of negotiating joint goals[21]. YGBMSM score lower on measures of assertive communication relative to their heterosexual age-mates[33]. Given the interdependent nature of drug use and sexual health for partnered YGBMSM, it may be that executing individual-level change is facilitated by communication between primary partners. The existing YMHP framework does not include a communication skills building component. To the extent that partnered YGBMSM need communication skills in order to respond to relationship-factors associated with behavior change, this may in part explain diminished effects.
These findings point directly to ways in which the existing YMHP intervention might be tailored to enhance its effectiveness for partnered YGBMSM. First, the intervention could be altered to incorporate a discussion of drug use along with sexual goals which encompass joint goals and a couple-level perspective. This kind of strategy has been utilized effectively to address HIV prevention and sexual health in Couples HIV Testing and Counseling (CHTC) for gay couples[34, 35]. CHTC involves a facilitated conversation between relationship partners about their sexual agreement and HIV-prevention strategy. Second, the intervention could be altered to specifically explore the influence of partners on the target behavior and how partners may respond to behavior change. Couples approaches to drug use intervention typically view relationship functioning and drug use as reciprocally related[36–38]. YMHP might be enhanced by incorporating attention to this reciprocal association. Third, the intervention might incorporate a social skills training component. Existing cognitive behavioral interventions targeting social skills (including communication skills) have demonstrated effects in reducing emotional and behavioral disorders in youth[39, 40]. While they have not been applied in the context of drug use and sexual risk reduction, these interventions typically focus on developing social perception as well as problem-solving skills[41] in a manner which partnered YGBMSM might find particularly useful during interactions with their primary partners.
There are two formats which might be used to expand YMHP for use with partnered men. One option is to focus on dyadic interventions, such as behavioral couples therapy[42] and CHTC[34, 35], both of which have shown beneficial effects in samples of sexual minority individuals. Dyadic level interventions permit a direct exploration of the couples’ perspective, facilitate communication between partners, and allow partners to practice relationship skills in sessions. Despite these advantages, there is also compelling evidence that individually-delivered services may be necessary to meet the needs of diverse partnered YGBMSM[43, 44]. Dyadic intervention requires partner coordination. For some, this is a logistical barrier. For others, one partner may desire services while the other does not. In addition, there are substantive challenges to implementing services for couples. These include provider level skill-building and agency-level concerns about service provision and integration[45]. At the same time, researchers have expressed concerns that dyadic engagement may bias samples towards couples with higher relationship satisfaction[43, 44].
These findings must be understood in light of several limitations. First, the external validity of these findings is limited by sample size. The original YMHP trial was not intended to examine relationship status as a putative moderator. The overall number of partnered men in the trial was small (n = 33). Of these, 14 received the intervention and 13 were utilized in these analyses. These analyses are best understood as a preliminary look at the potential utility of tailoring YMHP to the needs of partnered men. Future studies, with more diverse and representative samples of partnered GBMSM are needed in order to fully explicate how men in relationships might experience the intervention. Second, consistent with the goals of the YMHP intervention (which focused on HIV-related sexual risk taking with casual partners), the existing study was not powered to examine risk within primary partnerships. Third, in the present study, post hoc analyses confirmed that the pattern of results was robust to the inclusion of a variable indicating whether a participant was partnered at each follow up point. Future studies should examine the impact of intervention on the emergence of drug use and sexual risk taking following the establishment or cessation of primary partnerships which begin post-intervention. Fourth, the study excluded YGBMSM who were monogamous prior to intervention receipt and relationship agreements were not assessed. Given the relevance of these agreements for both sexual behavior and drug use[25, 26, 46], future studies should examine these agreements as moderators of potential outcomes. Finally, the current study was executed prior to the emergence of pre-exposure prophylaxis. Studies of male couples suggest that more than half of partnered MSM are interested in PrEP for HIV prevention[47, 48] and personal interest in PrEP is a significant predictor of willingness to persuade one’s partner to use PrEP[49]. Future studies of YMHP should incorporate a focus on PrEP and specifically examine how partners’ interactions shape PrEP-related decision making.
Despite these limitations, these findings highlight the relevance of relationship status to intervention response. Men who were partnered when they received YMHP benefited significantly less from the intervention with respect to drug use. While YMHP remains the only available best-practice intervention endorsed by CDC to address drug use and HIV prevention among HIV negative YGBMSM, these findings point to the potential utility of tailoring the intervention for those YGBMSM in relationships. Given the relevance of relationship factors – including sexual agreements – to drug use in this population [25], it is plausible that incorporating intervention components which enhance relationship skills and address the role of romantic partners in shaping substance use behavior may yield greater reductions in drug use among partnered men who experience the YMHP intervention.
Acknowledgments
Collection of these data was supported by was supported by a grant from the National Institute on Drug Abuse (NIDA) (R01-DA020366, Jeffrey T. Parsons, Principal Investigator). Data analysis was supported by grants from the National Institute of Child and Human Development (NICHD) (U19 HD089875, Jeffrey T. Parsons and Sylvie Naar, Principal Investigators) and NIDA (R01 DA041262, Jeffrey T. Parsons, Principal Investigator). Dr. Starks’ effort on this paper was also supported by a grant from NIDA (R01 DA045613; PI Starks).
The authors gratefully acknowledge the contributions of the Young Men’s Health Project team—Sarit Golub, Corina Lelutiu-Weinberger, Anthony Bamonte, Chris Hietikko, Juline Koken, John Pachankis, Kevin Robin, Brooke Wells and the CHEST recruitment team, as well as Richard Jenkins for his support of the project.
Footnotes
COMPLIANCE WITH ETHICAL STANDARDS
The authors have no conflicts of interest to disclose. All procedures were approved by the Institutional Review Board of Hunter College, City University of New York. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
References
- 1.Centers for Disease Control and Prevention. [Accessed February 2017];HIV Surveillance Report. 2013 25 https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2013-vol-25.pdf. Published February 2015. [Google Scholar]
- 2.Centers for Disease Control and Prevention. [Accessed February 2017];HIV Surveillance Report. 2015 27 https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. Published November 2016. [Google Scholar]
- 3.Austin EW, Bozick R. Sexual orientation, partnership formation, and substance use in the transition to adulthood. Journal of Youth and Adolescence. 2011;41:167–178. doi: 10.1007/s10964-011-9653-7. [DOI] [PubMed] [Google Scholar]
- 4.Corliss HL, Rosario M, Wypij D, Wylie SA, Frazier AL, Austin SB. Sexual orientation and drug use in a longitudinal cohort study of US adolescents. Addictive behaviors. 2010;35(5):517–521. doi: 10.1016/j.addbeh.2009.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lanfear C, Akins S, Mosher C. Examining the relationship of substance use and sexual orientation. Deviant Behavior. 2013;34(7):586–597. [Google Scholar]
- 6.Parsons JT, Grov C, Kelly BC. Club drug use and dependence among young adults recruited through time-space sampling. Public Health Reports. 2009;124(2):246–254. doi: 10.1177/003335490912400212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCabe SE, Boyd C, Hughes TL, d’Arcy H. Sexual identity and substance use among undergraduate students. Substance Abuse. 2003;24(2):77–91. doi: 10.1080/08897070309511536. [DOI] [PubMed] [Google Scholar]
- 8.Salomon EA, Mimiaga MJ, Husnik MJ, et al. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: Implications for Age-Specific Interventions. AIDS Behavior. 2009;13(4):811–821. doi: 10.1007/s10461-008-9439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshal MP, Friedman MS, Stall R, Thompson AL. Individual trajectories of substance use in lesbian, gay and bisexual youth and heterosexual youth. Addiction. 2009;104(6):974–981. doi: 10.1111/j.1360-0443.2009.02531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonar EE, Cunningham RM, Chermack ST, Blow FC, Barry KL, Booth BM, Walton MA. Prescription drug misuse and sexual risk behaviors among young men who have sex with men (YMSM) in Philadelphia. AIDS and Behavior. 2014;19(5):847–856. doi: 10.1007/s10461-014-0898-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgenstern J, Bux DA, Jr, Parsons J, Hagman BT, Wainberg M, Irwin T. Randomized trail to reduce club drug use and HIV risk behaviors among men who have sex with men. Journal of Consulting and Clinical Psychology. 2009;77(4):645–656. doi: 10.1037/a0015588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newcomb ME. Moderating effect of age on the association between alcohol use and sexual risk in MSM: evidence for elevated risk among younger MSM. AIDS and Behavior. 2013;17(5):1746–1754. doi: 10.1007/s10461-013-0470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newcomb ME, Mustanski B. Developmental change in the relationship between alcohol and drug use before sex and sexual risk behavior in young men who have sex with men. AIDS and Behavior. 2014;18(10):1981–1990. doi: 10.1007/s10461-014-0766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA. A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. Journal of Consulting and Clinical Psychology. 2014;82(1):9–18. doi: 10.1037/a0035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA. Predictors of day-level sexual risk for young gay and bisexual men. AIDS and Behavior. 2013;17(4):1465–1477. doi: 10.1007/s10461-012-0206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller WR, Rollnick S. Motivational Interviewing. 3. New York: Guilford Press; 2013. [Google Scholar]
- 17.D’Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Naar-King S, Parsons JT, Murphy D, Kolmodin K, Harris DR. A multisite randomized trial of a motivational intervention targeting multiple risks in youth living with HIV: Initial effects on motivation, self-efficacy, and depression. Journal of Adolescent Health. 2010;46(5):422–428. doi: 10.1016/j.jadohealth.2009.11.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Lam P, Murphy D. Healthy Choices: Motivational enhancement therapy for health risk behaviros in HIV-positive youth. AIDS Education & Prevention. 2006;18(1):1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- 20.Lewis MA, Gladstone E, Schmal S, Darbes LA. Health-related social control and relationship interdependence among gay couples. Health Education Research. 2006;21(4):488–500. doi: 10.1093/her/cyh075. [DOI] [PubMed] [Google Scholar]
- 21.Rusbult CE, Van Lange PA. Interdependence, interaction, and relationships. Annual Review of Psychology. 2003;54:351–375. doi: 10.1146/annurev.psych.54.101601.145059. [DOI] [PubMed] [Google Scholar]
- 22.Hoff CC, Beougher SC. Sexual agreements among gay male couples. Archives of Sexual Behavior. 2010;39:774–787. doi: 10.1007/s10508-008-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoff CC, Beougher SC, Chakravarty D, Darbes LA, Neilands TB. Relationship characteristics and motivations behind agreements among gay male couples: Differences by agreement type and couple serostatus. AIDS Care. 2010;22(7):827–835. doi: 10.1080/09540120903443384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell JW, Boyd C, McCabe S, Stephenson R. A cause for concern: Male couples’ sexual agreements and their use of substances with sex. AIDS and Behavior. 2014;18(7):1401–1411. doi: 10.1007/s10461-014-0736-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parsons JT, Starks TJ. Drug use and sexual arrangements among gay couples: frequency, interdependence and associations with sexual risk. Archives of Sexual Behavior. 2014;43(1):89–98. doi: 10.1007/s10508-013-0237-3. [DOI] [PubMed] [Google Scholar]
- 26.Parsons JT, Starks TJ, DuBois S, Grov C, Golub SA. Alternatives to monogamy among gay male couples in a community survey: implications for mental health and sexual risk. Archives of Sexual Behavior. 2013;42(2):303–312. doi: 10.1007/s10508-011-9885-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–62. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 28.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS ONE. 2012;7(11) doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parsons JT, Vial AC, Starks TJ, Golub SA. Recruiting drug-using men who have sex with men in behavioral intervention trials: A comparison of internet-based and field-based strategies. AIDS and Behavior. 2013;17(2):688–699. doi: 10.1007/s10461-012-0231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vial AC, Starks TJ, Parsons JT. Finding and recruiting the highest risk HIV-negative men who have sex with men. AIDS Education & Prevention. 2014;26(1):56–67. doi: 10.1521/aeap.2014.26.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sobell LC, Sobell MB. Timeline followback user’s guide. Toronto: Alcohol Research Foundation; 1996. [Google Scholar]
- 32.Hardin JW, Hilbe JM. Generalized estimating equations. 2. Boca Raton, FL: Taylor & Francis Group, LLC; 2013. [Google Scholar]
- 33.Rew L, Whittaker TA, Taylor-Seehafer MA, Smith LR. Sexual health risks and protective resources in gay, lesbian, bisexual, and heterosexual homeless youth. Journal of Specialists in Pediatric Nursing. 2005;10(1):11–19. doi: 10.1111/j.1088-145x.2005.00003.x. [DOI] [PubMed] [Google Scholar]
- 34.Sullivan PS, White D, Rosenberg ES, et al. Safety and acceptability of couples HIV testing and counseling for US men who have sex with men: a randomized prevention study. Journal of the International Association of Physicians in AIDS Care. 2014;13(2):135–144. doi: 10.1177/2325957413500534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stephenson R, Rentsch C, Sullivan PS. High levels of acceptability of couples-based HIV testing among MSM in South Africa. AIDS Care. 2012;24(4):529–535. doi: 10.1080/09540121.2011.617413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Epstein EE, McCrady BW. Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clinical Psychology Review. 1998;18(6):689–711. doi: 10.1016/s0272-7358(98)00025-7. [DOI] [PubMed] [Google Scholar]
- 37.Sher TG. Cognitive behavioral couples therapy. Encyclopedia of Clinical Neuropsychology. 2011:618–619. [Google Scholar]
- 38.Powers MB, Vedel E, Emmelkamp PMG. Behavioral couples therapy for alcohol and drug use disorders: a meta-analysis. Clinical Psychology Review. 2008;28(6):952–962. doi: 10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Cook CR, Gresham FM, Kern L, Barreras RB, Thornton S, Crews SD. Social skills training for secondary students with emotional and/or behavioral disorders: A review and analysis of the meta-analytic literature. Journal of Emotional and Behavioral Disorders. 2008;16(3):131–144. [Google Scholar]
- 40.Maag JW. Social skills training for students with emotional and behavioral disorders: A review of reviews. Behavioral Disorders. 2006;32(1):5–17. [Google Scholar]
- 41.Spence SH. Social skills training with children and young people: Theory, evidence and practice. Child and Adolescent Mental Health. 2003;8:84–96. doi: 10.1111/1475-3588.00051. [DOI] [PubMed] [Google Scholar]
- 42.Fals-Stewart W, O’Farrell TJ, Lam WKK. Behavioral couples therapy for gay and lesbian couples with alcohol use disorders. Journal of Substance Abuse Treatment. 2009;37(4):379–387. doi: 10.1016/j.jsat.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Starks TJ, Millar B, Parsons JT. Correlates of individual versus joint participation in online survey research with same-sex male couples. AIDS and Behavior. 2015;19:963–969. doi: 10.1007/s10461-014-0962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yucel D, Gassanov M. Exploring actor and partner correlates of sexual satisfaction among married couples. Social Science Research. 2010;39(5):725–738. [Google Scholar]
- 45.Stephenson R, Grabbe KL, Sidibe T, McWilliams A, Sullivan PS. Technical assistance needs for successful implementation of couples HIV testing and counseling (CHTC) intervention for male couples at US HIV testing sites. AIDS and Behavior. 2016;20:841–847. doi: 10.1007/s10461-015-1150-7. [DOI] [PubMed] [Google Scholar]
- 46.Mitchell JW, Harvey SM, Champeau D, Seal DW. Relationship factors associated with HIV risk among a sample of gay male couples. AIDS and Behavior. 2012;16(2):404–411. doi: 10.1007/s10461-011-9976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mitchell JW, Stephenson R. HIV-Negative partnered men’s willingness to use pre-exposure prophylaxis and associated factors among an internet sample of U.S. HIV-Negative and HIV-Discordant Male Couples. LGBT Health. 2015;2(1):35–40. doi: 10.1089/lgbt.2014.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gamarel KE, Golub SA. Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Ann Behav Med. 2015;49(2):177–186. doi: 10.1007/s12160-014-9646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.John SA, Starks TJ, Rendina HJ, Grov C, Parsons JT. Should I convince my partner to go on Pre-Exposure Prophylaxis? The role of personal and relationship factors on PrEP-related social control among gay and bisexual men. doi: 10.1007/s10461-017-1835-1. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]