Abstract
Increasing the uptake of pre-exposure prophylaxis (PrEP) to prevent HIV acquisition among at-risk populations, such as young men who have sex with men (YMSM), is of vital importance to slowing the HIV epidemic. Stigma and negative injunctive norms, such as the so called “Truvada Whore” phenomenon, hamper this effort. We examined the prevalence and types of PrEP stigma and injunctive norm beliefs among YMSM and transgender women and associated individual and geospatial factors. A newly created measure of PrEP Stigma and Positive Attitudes was administered to 620 participants in an ongoing longitudinal cohort study. Results indicated lower stigma among White, compared to Black and Latino participants, and among participants not identifying as male. Prior knowledge about PrEP was associated with lower stigma and higher positive attitudes. PrEP stigma had significant geospatial clustering and hotspots were identified in neighborhoods with high HIV incidence and concentration of racial minorities, whereas coldspots were identified in areas with high HIV incidence and low LGBT stigma. These results provide important information about PrEP attitudes and how PrEP stigma differs between individuals and across communities.
Keywords: pre-exposure prophylaxis, geospatial, Homosexuality, male, HIV, stigma
INTRODUCTION
Since 2010, the number of new HIV infections in the United States has remained steady at around 40,000 cases per year.(1) In 2015, approximately two-thirds of new infections were attributed to male-to-male sexual contact, and 48.8% of those infections were in men under the age of 30.(1) Therefore, addressing the spread of HIV among men who have sex with men (MSM), particularly young MSM (YMSM), is of vital importance to slowing the HIV epidemic in the United States.
When taken as directed, pre-exposure prophylaxis (PrEP) is an effective method to prevent HIV acquisition. Randomized controlled trials such as iPrEx and open-label studies conducted primarily with MSM demonstrated that use of once-daily oral PrEP could reduce HIV incidence by up to 92% when adherence is high.(2–4) As a result of these studies, in 2012 the U.S. Food and Drug Administration (FDA) approved Truvada for use as PrEP among populations at high risk for HIV acquisition.(5) Consequently, the Centers for Disease Control and Prevention (CDC) released guidelines for healthcare providers on PrEP indications in 2014.(6)
Despite the promise of PrEP for preventing new HIV infections in YMSM in the U.S., there remain multiple barriers to its uptake. Foremost among these obstacles is PrEP awareness – in a three city study of nearly 700 YMSM who had never used PrEP, 16.9% had never heard of PrEP and 15.6% had heard of it, but did not know what it was.(7) However, this study also found that PrEP awareness significantly increased over time, indicating growing awareness among YMSM. Other studies among MSM have also demonstrated that lack of PrEP awareness is a substantial barrier to its use.(8, 9) Willingness to use PrEP among MSM has been shown to be relatively high (70–80%),(10–12) but in one study of YMSM, over one-third refused to use PrEP due to potential side effects.(13)
One understudied area of barriers to PrEP uptake and adherence is the role that PrEP stigma plays in the decisions about use among YMSM. Stigma is defined as an attribute that discredits an individual due to deviations from social norms for behaviors or identities.(14) Injunctive social norms—what a group commonly approves or disapproves of—are one of the strongest predictors of both risky and protective health behaviors.(15) Injunctive norms originated in the theories of reasoned action and planned behavior and are essentially synonymous with subjective or moral norms because behavior is governed by the moral values of the individual.(16) The influence of injunctive norms has been widely studied in the area of sexual behaviors.(17, 18) Importantly, research has shown differences between the influence of injunctive norms on risk and protective factors, with researcher’s inquiring far less on the latter. This has contributed to a general tendency in the literature to underestimate the effect of injunctive norms on protective behaviors and perhaps overestimate their relationship with risky behaviors.(19) Among MSM, for example, Peterson and Bakeman(20) found that perceived approval of condom use (an injunctive norm) mediated the relationship between the belief that HIV was less of a threat due to the availability of biomedical treatments and risky sexual behavior with casual partners. According to social cognitive theory, health behaviors are shaped by observing and communicating with others in one’s social networks and proximal environment (e.g., neighborhood).(21) Thus, when attempting to understand or change the behavior of individuals, the role of injunctive norms in the proximal community on the perceived acceptability of specific risk and protective behaviors should be considered. When individuals engage in risky or protective behaviors that the community deems unacceptable by virtue of injunctive norms, they are at risk for experiencing stigma and internalizing stigmatized views of the behavior.
In terms of injunctive norms related to PrEP, there has been the stigmatizing belief that PrEP is used by individuals who are unacceptably promiscuous and/or that PrEP causes increases in engagement in HIV risk behaviors—the so called “Truvada Whore” phenomenon.(22–24) Since the advent of PrEP, there has been widespread concern of risk compensation,(25) or increased frequency of condomless sex due to the protection conferred by PrEP,(24, 26–29) but evidence that PrEP use is associated with change in condom use is mixed. Several earlier studies of MSM and heterosexuals in Africa observed either no change or an increase in condom use among PrEP users in randomized trials.(30–33) However, more recent studies using clinic-based and longitudinal cohort designs have found strong evidence of risk compensation among MSM in the U.S.(34–36) In terms of PrEP stigmatizing beliefs, a recent study of Black and White MSM and transwomen found that 70% thought PrEP would cause risky sex, and 23% believed that only promiscuous people use PrEP.(37) Other studies of MSM have found similarly prevalent negative PrEP beliefs across all demographics, although PrEP stigma among Black MSM is more connected to medical mistrust and other forms of stigma (HIV, LGBT, etc.) than White MSM.(38–40) As a result, healthcare providers may be less likely to prescribe PrEP to their patients, and high risk individuals may be less likely to seek out PrEP, due both to perceived and experienced stigma.
Although the empirical literature on experiences with and consequences of PrEP stigma has yet to be well developed, likely there will be parallels with the large body of research on HIV stigma. There is an extensive body of research demonstrating clear ties between HIV-related stigma and both avoidance of healthcare seeking behaviors(41, 42) and poor ART adherence.(43, 44) Of great concern to people living with HIV has been the worry that people would see them taking their HIV medication, resulting in an unintentional disclosure of their HIV status.(44) Similarly, the fact that the medications used for PrEP are also used by HIV-positive patients may serve to initiate an unintended discussion with family and friends about serostatus and risk behaviors.
In light of the importance of the role that PrEP stigma may play in the lives and decisions about PrEP use among YMSM and young transgender women (YTW), our manuscript seeks to address the near absence of research on this topic. In this study, we sought to examine (1) whether YMSM/YTW in Chicago experience PrEP stigma; (2) which PrEP stigma constructs are most germane to this sample; and (3) individual (e.g., gender, race/ethnicity, sexual orientation) and geospatial factors (e.g., neighborhood LGBT stigma) that may be associated with PrEP stigma.
METHODS
Study Design & Recruitment
Data were collected as part of the RADAR study, an ongoing longitudinal cohort study of YMSM living in the Chicago metropolitan area.(45, 46) The primary objective of this cohort study is to apply a multilevel perspective to a syndemic of health issues associated with HIV among diverse YMSM.(47, 48) Diverse methods for participant recruitment were selected in order to achieve the accelerated longitudinal design.(49) First, a subset of participants from two cohort studies of YMSM, Project Q2 (n=67) and Crew 450 (n=163), who were first recruited in 2007 and 2010 respectively, were enrolled. In 2015, a third cohort of YMSM (n=467) was recruited. At the time of enrollment into their original respective cohorts, all participants were between 16 and 20 years of age, born male, spoke English, and had a sexual encounter with a man in the previous year or identified as gay, bisexual or transgender. Next, the RADAR cohort was expanded through an iterative process where serious romantic partners were recruited at each visit, thereby creating a dynamic dyadic network. All male assigned at birth serious romantic partners were eligible for enrollment into the cohort regardless of gender identity or sexual orientation. Romantic partners who were assigned female at birth or were older than 29 completed a study visit but were not enrolled in the cohort. Lastly, cohort members were allowed to refer a maximum of three YMSM peers for enrollment into the study as long as they were between 16 and 29 years of age.
The PrEP Stigma and Positive Attitudes measure was administered to study participants at baseline or follow-up visits between February 8th, 2016, and October 10th, 2016. Participants who self-reported taking PrEP in the previous six months or being HIV positive were not administered this measure and thus were excluded from subsequent analyses. A total of 620 participants have data regarding PrEP attitudes; however, since this measure was administered for approximately eight months in a longitudinal cohort study with biannual visits, some participants had data at two time points (n=98). In order to best reflect the most current YMSM community attitudes towards PrEP use, data from the second time point (where applicable) was used as part of the final analytic sample (n=620). No significant within-person change (p>.05) existed among the small sample of participants who had data at more than one time point.
Measures
Demographics
Participants provided demographic information such as age, race/ethnicity, birth sex, gender identity and sexual orientation at each visit. For purposes of this analysis, participants reporting a Hispanic/Latino ethnicity were coded as such, regardless of their racial identity.(50)
Perceived LGBT Stigma in Residential Neighborhood
To examine the level of perceived LGBT stigma within participants’ residential neighborhood, a five-item measure assessing social acceptance by neighbors as well as availability and satisfaction with local LGBT-identified gathering places was administered to participants. Neighborhood was defined as “the area surrounding where you live”. Study investigators developed items. The three items measuring social acceptance were “I feel comfortable with my neighbors knowing my sexual orientation.”, “In my neighborhood, I would feel comfortable being seen with LGBT individuals.” and “In my neighborhood, I feel comfortable holding my partner’s hand in public.” Participants responded on a four-point scale ranging from strongly disagree (1) to strongly agree (4), but responses were reverse coded prior to scoring so higher values represented greater perceived stigma. Measure scoring consisted of averaging the reverse coded three items assessing social acceptance. Measure reliability was found to be adequate (Cronbach’s alpha = 0.84).
PrEP Knowledge, Awareness, and Communication
To assess participants’ knowledge about PrEP, participants were asked to respond “True”, “False”, or “I Don’t Know” to the following question: “Taking pre-exposure prophylaxis (a pill, also known as PrEP or Truvada) regularly can reduce the risk of contracting HIV from an HIV-positive sex partner.” For purposes of these analyses “I Don’t Know” responses were coded as incorrect knowledge. Later, participants were asked to indicate their prior awareness of PrEP by responding to the question “Before today, have you ever heard of pre-exposure prophylaxis (PrEP)?”. Also, participants’ feelings about talking with a sex partner about using PrEP was assessed on a 5-point Likert scale using two questions: (1) “Talking to a partner about pre-exposure prophylaxis (a pill, also known as PrEP or Truvada) would be:” (1=very bad, 5=very good) and “How hard would it be for you to talk to a partner about using a medication that can help prevent HIV transmission (pre-exposure prophylaxis or PrEP)?” (1=very hard, 5=very easy).
PrEP Stigma and Positive Attitudes
Eleven items were developed by study investigators to assess participants’ injunctive norms(17) about whether it is a good or bad thing for others to take PrEP. Each item was measured on a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5). To assure a baseline level of awareness of PrEP, participants who indicated having no prior awareness of PrEP, based on the item described above, were provided with a description explaining the purpose, effectiveness, administration method and dosing schedule of PrEP. This description was based on publically available information provided by the CDC.(51) The structure of the scale was examined using factor analysis (described below).
HIV Risk Behaviors
The HIV-Risk Assessment for Sexual Partnerships (H-RASP) is a self-administered questionnaire designed to assess sexual behaviors and associated situational/contextual variables at the level of the sexual partnership in the previous six months.(52, 53) The sexual risk variables used in these analyses include: (1) sexually active (yes/no), (2) number of male condomless anal sex partners, (3) sexual partners categorized as male partners, male and female partners, female partners, or no sexual partners, (4) relationship type of most recent sex partner categorized as serious or non-serious, (5) perceived PrEP use by most recent sex partner (yes/no), and (6) perceived HIV status of most recent sex partner categorized as positive or negative/I don’t know.
Analyses
Exploratory factor analysis (EFA) using oblique rotation (geomin) was conducted to examine the factor structure of the PrEP attitudes measure. Model fit was assessed by the root mean square error of approximation (RMSEA), Comparative Fit Index (CFI), and the standardized root mean square residual (SRMR) using criteria recommended for categorical data: RMSEA <.06, CFI >.95, and SRMR <.08.(54) The EFA model utilized listwise deletion and a weighted least squares mean- and variance-adjusted estimator (WLSMV). Subsequent non-parametric analyses were conducted to test for demographic, PrEP awareness and sexual behavior differences in PrEP attitude scores. EFA was conducted using Mplus software while all other analyses were conducted using SAS software.
Geographical information system (GIS) analyses were performed to explore spatial patterns of participants’ attitudes towards PrEP use based on the hypothesis that injunctive norms cluster within proximal environments. Participants’ residential addresses at time of data collection were geocoded using a local composite geocoder. Community area boundaries were plotted using a shapefile obtained from the City of Chicago and 2014–15 HIV incidence data by community area were obtained from the Chicago Department of Public Health 2016 STI/HIV Surveillance Report.(55, 56) Only participants who were geocoded using the StreetAddress or AddressPoint locator and were within the city of Chicago’s geographical boundaries were included in analyses (n=411). Further analytic exclusions were performed based on the presence of outliers or geographically sparse data, defined as a distance of more than three standard deviations away from the nearest neighbor. Computed scores from the PrEP Stigma and Positive Attitudes measure for each participant were assessed with optimized hot spot analyses. Optimized hot spot analysis first aggregates the participant locations (points) before utilizing Getis-Ord GI* statistic, to identify the existence of spatial clusters.(57) GIS analyses were conducted using ArcGIS and ArcMap 10.5.
RESULTS
Demographic characteristics of the analytic sample (n=620) are displayed in Table 1.
Table I.
Demographic characteristics of analytic sample (n=620)
| n | % | |
|---|---|---|
| Birth Sex | ||
| Male | 620 | 100.0 |
| Female | 0 | 0.0 |
| Gender Identity | ||
| Male | 577 | 93.1 |
| Transgender | 23 | 3.7 |
| Other | 20 | 3.2 |
| Age (M=21.1; SD=2.8) | ||
| 16–17 | 52 | 8.4 |
| 18–20 | 317 | 51.1 |
| 21–24 | 184 | 29.7 |
| 25+ | 67 | 10.8 |
| Race/Ethnicity | ||
| Black or African American | 182 | 29.4 |
| Hispanic/Latino | 206 | 33.2 |
| White | 162 | 26.1 |
| Other | 70 | 11.3 |
| Sexual Orientation | ||
| Gay | 414 | 66.8 |
| Bisexual | 136 | 21.9 |
| Queer | 32 | 5.2 |
| Other | 38 | 6.1 |
Measurement Psychometrics
Examination of item-item correlations using all 11 questions showed each to be significantly correlated (p<.05) except for three pairs with each pair including the item “I think condoms are a better choice than PrEP”. Further analysis also showed this item to have the lowest item-total correlation (r=0.15). Based on these findings and determination by study investigators that this item assessed HIV prevention preferences rather than PrEP stigma, it was excluded from subsequent analyses.
Factor structure for the remaining 10 items was assessed by EFA with a WLSMV estimator and oblique rotation (where applicable) for a one, two and three factor solution. Based on model fit statistics, eigenvalues greater than one (4.99 & 1.58) and interpretability of extracted factors, results suggested a two factor solution to be most appropriate (RMSEA=0.123, CFI=0.965, SRMR=0.040). Standardized factor loadings are shown in Table 2. The first factor consists of seven items pertaining to PrEP stigma while the second factor consists of three items pertaining to positive attitudes towards PrEP use. Cronbach’s alpha for each of these two factors are 0.85 and 0.69 respectively. Scale scores are calculated by taking the mean of all items per factor. The full wording of the measure is provided in Appendix A.
Table II.
PrEP attitudes item-level descriptives with EFA standardized factor loadings
| EFA | ||||
|---|---|---|---|---|
| Mean (SD) | IQR | Factor #1 | Factor #2 | |
| People should take PrEP | 4.03 (0.95) | 2.0 | 0.09 | 0.76 |
| People on PrEP sleep around | 2.60 (1.07) | 1.0 | 0.70 | 0.02 |
| People on PrEP are irresponsible | 2.05 (0.98) | 2.0 | 0.73 | −0.19 |
| Sex with someone on PrEP is risky | 2.42 (1.03) | 1.0 | 0.62 | −0.13 |
| PrEP users make smart decision to protect health | 4.21 (0.91) | 1.0 | −0.01 | 0.92 |
| Wouldn't trust someone who told me they're on PrEP | 2.26 (1.08) | 2.0 | 0.71 | −0.17 |
| People on PrEP can't control sex drive | 2.02 (0.96) | 2.0 | 0.77 | −0.22 |
| PrEP is used as excuse to have condomless sex | 2.66 (1.15) | 1.0 | 0.79 | 0.08 |
| PrEP users lie about taking it everyday | 2.63 (0.93) | 1.0 | 0.82 | 0.08 |
| People on PrEP are responsible | 3.59 (0.94) | 1.0 | −0.15 | 0.48 |
Note: RMSEA=.123; CFI=.965; SRMR=.040; IQR=interquartile range
Demographic Differences
Employing Kruskal-Wallis tests, statistically significant differences (p<.05) were found for the stigma scale score by racial/ethnic groups (χ2=35.2, p<.0001) and gender identity (χ2=10.8, p=.005), but not sexual orientation (χ2=6.9 p=.076). No such differences were found for the PrEP positive attitudes scale score. Using a Bonferroni correction to the alpha level, White participants had significantly lower stigma scores compared to Black and Latino participants. In addition, participants indicating another gender identity (e.g., gender non-conforming, gender queer) had significantly lower stigma scores compared to male and transgender identified participants. The aforementioned group differences are displayed in Table 3. Participants’ age was not found to be significantly correlated with the PrEP positive attitudes scale score (rs=− 0.07, p=.087) or the stigma scale score (rs=−.01, p=.825).
Table III.
Demographic differences in PrEP stigma and positive attitudes factors
| Stigma | Positive Attitudes | ||||
|---|---|---|---|---|---|
| n (%) | Median (IQR) | Kruskal-Wallis Test χ2 (p-value) | Median (IQR) | Kruskal-Wallis Test χ2 (p-value) | |
| Race/Ethnicity (n=620) a, b | |||||
| Black or African American | 182 (29.4) | 2.57 (1.0) | 35.2 (<.0001) | 4.00 (1.3) | 7.0 (.071) |
| Hispanic/Latino | 206 (33.2) | 2.57 (1.1) | 4.00 (1.0) | ||
| White | 162 (26.1) | 2.08 (1.0) | 4.00 (1.0) | ||
| Other | 70 (11.3) | 2.43 (1.1) | 4.00 (0.7) | ||
| Gender Identity (n=620) c, d | |||||
| Male | 577 (93.1) | 2.43 (1.1) | 10.8 (.005) | 4.00 (1.0) | 2.2 (.328) |
| Transgender | 23 (3.7) | 2.86 (1.0) | 4.00 (1.3) | ||
| Other | 20 (3.2) | 1.78 (1.1) | 4.17 (1.5) | ||
| Sexual Orientation (n=620) | |||||
| Gay | 414 (66.8) | 2.29 (1.1) | 6.9 (.076) | 4.00 (1.3) | 3.4 (.335) |
| Bisexual | 136 (21.9) | 2.43 (1.1) | 4.00 (1.3) | ||
| Queer | 32 (5.2) | 2.00 (1.1) | 4.00 (0.7) | ||
| Other | 38 (6.1) | 2.71 (1.1) | 3.67 (1.0) | ||
| Sexually Active in Past 6 Months (n=620) | |||||
| No | 107 (17.3) | 2.23 (1.1) | 0.4 (.553) | 4.00 (1.0) | 2.5 (.117) |
| Yes | 513 (82.7) | 2.43 (1.1) | 4.00 (1.3) | ||
| Sexual Partners in Past 6 Months (n=620) | |||||
| Male Partners | 451 (72.7) | 2.43 (1.1) | 1.1 (.769) | 4.00 (1.0) | 4.5 (.211) |
| Male and Female Partners | 45 (7.3) | 2.71 (1.1) | 4.00 (1.0) | ||
| Female Partners | 17 (2.7) | 2.43 (1.3) | 3.67 (1.3) | ||
| No Sexual Partners | 107 (17.3) | 2.29 (1.1) | 4.00 (1.0) | ||
| Prior PrEP Awareness (n=620) | |||||
| No | 139 (22.4) | 2.86 (1.0) | 26.5 (<.0001) | 3.67 (1.0) | 12.5 (<.001) |
| Yes | 481 (77.6) | 2.29 (1.1) | 4.00 (1.0) | ||
| PrEP Reduces HIV Transmission Risk (n=226) e | |||||
| True | 175 (77.4) | 3.00 (0.7) | 13.8 (<.001) | 3.67 (1.0) | 17.2 (<.0001) |
| False | 51 (22.6) | 2.29 (1.1) | 4.00 (1.0) | ||
| Most Recent Partner on PrEP (n=452) f, g | |||||
| No | 419 (92.7) | 2.43 (1.1) | 2.3 (.127) | 4.00 (1.0) | 0.3 (0.594) |
| Yes | 33 (7.3) | 2.57 (1.1) | 4.00 (0.7) | ||
| HIV Testing in Past 6 Months (n=620) | |||||
| No | 190 (30.7) | 2.43 (1.1) | 0.2 (.701) | 4.00 (1.0) | 0.1 (.754) |
| Yes | 428 (69.3) | 2.43 (1.1) | 4.00 (1.2) | ||
| Most Recent Partner Serious (n=546) f | |||||
| No | 290 (53.1) | 2.43 (1.1) | 0.0 (.970) | 4.00 (1.0) | 0.6 (.458) |
| Yes | 256 (46.0) | 2.43 (1.1) | 4.00 (0.8) | ||
| Most Recent Partner HIV+ (n=546) f | |||||
| No | 530 (97.1) | 2.43 (1.1) | 4.5 (.034) | 4.00 (1.0) | 3.7 (.053) |
| Yes | 16 (2.9) | 2.00 (1.1) | 4.33 (0.8) | ||
Significant difference between Black and White participants.
Significant difference between Latino and White participants.
Significant difference between male and other gender identities.
Significant difference between transgender and other gender identities.
Sample size reduced since item was only administered at baseline visit.
Sample size reduced since item was only administered to sexually active participants.
Sample size reduced since item was not asked on all versions of survey and only asked about HIV-negative partners.
Sexual Behavior Differences
Sexually active participants did not show statistically significant differences in stigma scale score (χ2=0.4, p=.553) or positive attitudes scale score (χ2=2.5, p=.117) compared to their non-sexually active peers. Similarly, participants’ gender of sexual partners (e.g., male partners, male and female partners), receipt of an HIV test in prior six months and relationship type (serious vs. non-serious) did not show statistically significant differences for either PrEP stigma or positive attitudes scale scores (see Table 3 for further detail). In addition, number of condomless anal sex partners in the past 6 months was not significantly correlated with either the stigma (rs=.03, p=.483) or positive attitudes (rs=.02, p=.706) scale scores. However, participants whose most recent sex partner was HIV-positive reported significantly lower PrEP stigma scale scores compared to those whose partner was HIV-negative (χ2=4.5, p=.034).
PrEP Awareness
Significant differences exist between participants who had previously heard of PrEP and those who had not for both the stigma (χ2=26.5, p<.0001) and positive attitudes factors (χ2=12.5, p<.001). Similar effects were found for participants who knew that regular PrEP use could reduce the risk of HIV transmission compared to those who did not for both the stigma (χ2=13.8, p<.001) and positive attitudes factors (χ2=17.2, p<.0001). In both instances, participants who already had knowledge about PrEP reported lower stigma and higher positive attitudes. Furthermore, participants who were more in favor of talking with a partner about PrEP use and who indicated those conversations as being less difficult had higher scores on the PrEP positive attitudes scale, rs=0.30 (p<.0001) and rs=0.30 (p<.0001), respectively, and lower PrEP stigma scale scores, rs=−0.24 (p<.001) and rs=−0.15 (p<.05), respectively. PrEP use by most recent sexual partner did not show any statistically significant differences in either scale.
Exploratory Spatial Analyses
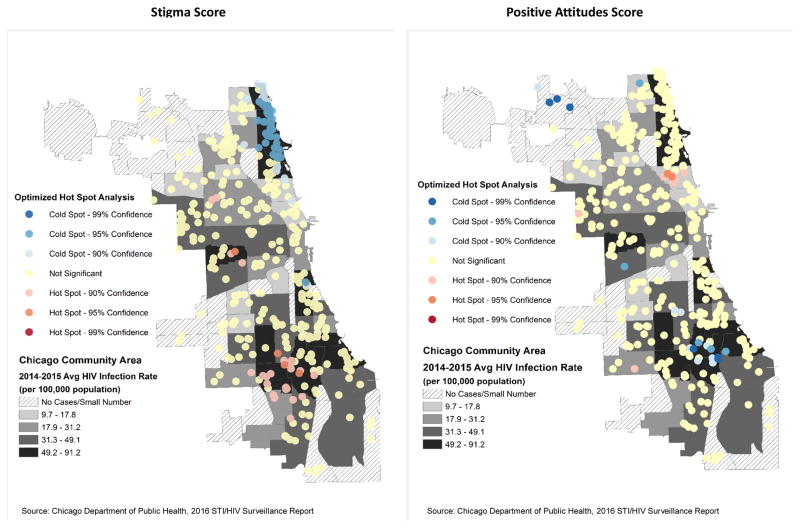
Examining the geographical representation of PrEP stigma and positive attitudes scores (n=411), using optimized hot spot analysis, resulted in the detection of statistically significant clusters (p<.10 or 90% CI) consisting of 100 and 19 participants respectively. Clustering of low PrEP stigma scores (cold spots) were found among some northern communities of Chicago while clustering of high stigma scores (hot spots) were found among some western and southern communities. Though not as prominent, similar geographical patterns emerged with clustering of high positive attitudes scores (hot spots) found among some northern communities while low positive attitudes scores (cold spots) were concentrated more in some southern and northwestern communities (see Figure 1).
Figure 1.
GIS optimized hot spot analysis for PrEP stigma and positive attitudes scores regardless of participants’ prior awareness of PrEP (n=411)
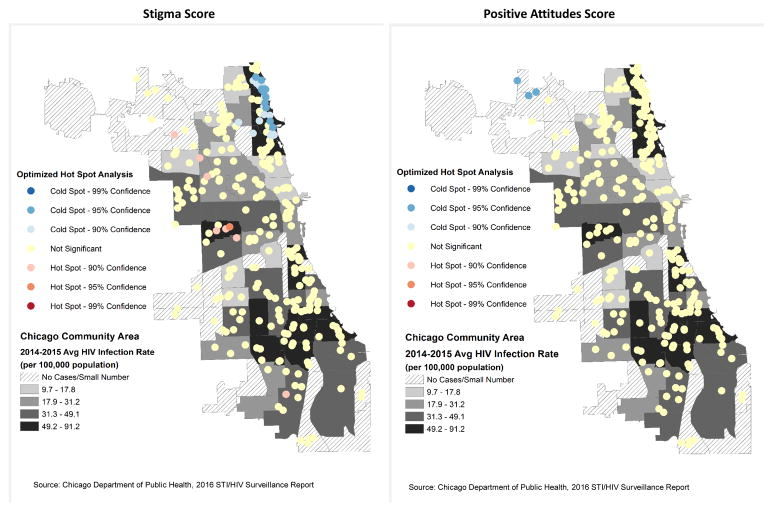
Restricting the previous analyses to only participants who had previously heard of PrEP (n=313) resulted in the detection of statistically significant clusters (p<.10 or 90% CI) consisting of 48 and 3 participants for the PrEP stigma and positive attitudes scales respectively. In this follow-up analysis, clustering of low stigma scores (cold spots) continued to be concentrated among the northern communities while higher stigma scores (hot spots) diminished considerably from the southern communities. However, for the positive attitudes scores, significant high values (hot spots) among those northern communities and low values (cold spots) among southern communities no longer exist. The only statistically significant values appear among northwestern communities (see Figure 2).
Figure 2.
GIS optimized hot spot analysis for PrEP stigma and positive attitudes scores for participants who had previously heard of PrEP (n=313)
Levels of perceived neighborhood LGBT stigma vary across the city of Chicago, so to further build on the exploratory GIS analyses we examined aspatial correlations with PrEP stigma. Increased perceived LGBT stigma within residential neighborhoods was found to be positively correlated with the PrEP stigma scale score (rs=.30, p<.0001) and negatively correlated with the positive attitudes scale score (rs=−0.21, p=.003).
DISCUSSION
The present study is one of the first to investigate stigma associated with PrEP among YMSM, a population that experiences a heavy burden of the domestic HIV epidemic.(58) Analyses of our newly created measure of PrEP attitudes identified two subscales measuring PrEP stigma and positive attitudes about PrEP. Analyses revealed demographic and geographic differences in PrEP stigma and positive attitudes about PrEP. Black participants scored significantly higher on PrEP stigma compared to other racial groups. Overlaying our GIS optimized hotspot analysis on HIV rates reported by the Chicago Department of Public Health suggest that the geographic areas that were found to have the most PrEP stigma are also those that have a higher incidence of HIV and a higher concentration of racial minorities (minority data not shown).(56) In order to address the rising burden of HIV among racial minority MSM in Chicago, more work needs to be done to reduce PrEP stigma in these communities, which likely will necessitate reducing structural barriers to HIV prevention and care, including improved access to LGBT-affirming healthcare.
Importantly, our analyses indicate that stigma was lower and positive attitudes were higher among those with prior awareness of PrEP, so a clear first stop toward reducing stigma is to simply increase awareness. Targeting awareness campaigns to key communities may help to reduce community differences in stigma. Some work along these lines is already underway in Chicago in–2016, a citywide social marketing campaign (PrEP4Love) targeted at increasing PrEP uptake and adherence, particularly among racial minority populations, was launched. As PrEP4Love ran concurrently with our study, it is likely that the level of PrEP awareness reported by participants exceeds that of YMSM in other urban and suburban areas where no social marketing campaigns were occurring. However, the fact that PrEP stigma remains, especially within areas and populations targeted by the PrEP4Love campaign, indicates that additional focused effort is necessary to reduce barriers other than knowledge and awareness.
There has been very little research to date on PrEP stigma and injunctive norms, but various stereotypes and beliefs about individuals who take PrEP have proliferated throughout the LGBT community (i.e., “Truvada Whore” stererotype(22)). Of note, research has not conclusively demonstrated that PrEP use is associated with increased engagement in condomless sex and other sexual risk behaviors.(24, 33, 59, 60) Nevertheless, stigmatized beliefs about promiscuity and risk compensation among PrEP users exists. This stigma associated with PrEP may serve as a barrier to PrEP uptake amongst some individuals who are at high risk for HIV infection, either because they themselves ascribe to these stereotypes and do not want to be perceived in a negative light, or because their medical providers are reluctant to prescribe PrEP due to fears of increased sexual risk behavior. Social cognitive theory provides a useful lens for interpreting the role of injunctive norms and stigma on PrEP uptake. Perceptions of how common or uncommon the prevalence of a behavior is, whether among individual users or prescribers, influence actual uptake of health behaviors. Individuals are known to place the greatest value on the observed behaviors of proximal peers, which include social and sexual networks and patient populations, but also on biased perceptions shaped by extreme examples of the normative behavior. Thus, systems level approaches to increase the uptake of PrEP could have a dual focus on improving perceptions of prevalence of PrEP usage and correcting biased views. One intervention that has been found to improve stigmatized health behaviors is called personalized normative feedback(61), which juxtaposes individuals’ own reported normative perceptions (e.g., degree of PrEP users’ promiscuity with risky sex partners) and personal behaviors (own prevalence risky sex behaviors) against their peers’ true normative values (actual number of risky sex partners among peers). Similarly, HIV prevention interventions that focus on increasing motivations for safer sex behaviors have been shown to impact perceived norms about condom use and similar approaches could be applied to PrEP.(62–64) As our findings on the racial and geographical differences in PrEP stigma reveal, further tailoring of the intervention is indicated for these two important contextual factors.
More longitudinal research is needed to track changes in PrEP stigma over time, as well as to understand how stigma may predict a lower likelihood of PrEP uptake by an individual or others in their network who are exposed to those attitudes. Importantly, the majority of participants in the present analyses endorsed positive attitudes about PrEP (70.8% had an average of “agree” or “strongly agree” across all positive attitude items) and scored low on the PrEP stigma scale (58.1% had an average of “disagree strongly” or “disagree” across all stigma items). While this is indeed encouraging, there were individual differences in the endorsement of PrEP stigma and more research is needed to reduce these negative attitudes and stereotypes in order to optimize PrEP uptake.
The racial differences we observed in endorsement of PrEP stigma are concerning in light of the fact that Black YMSM experience a disproportionately high rate of new HIV infections(65, 66) and these participants also scored significantly higher on PrEP stigma. While it is important to reduce barriers to PrEP uptake for all YMSM, it is also critically important that we target efficacious prevention methods to those that are most burdened by new HIV infections. Black YMSM have not been shown to differ from other racial groups in their use of condoms leading many to hypothesize that structural and network factors (e.g., higher within-race sexual partnering resulting from geographic isolation and/or race-based stigma) are responsible for increased HIV incidence in this population.(66–68) Additional prevention strategies are necessary for curbing HIV incidence in this population, and uptake of PrEP within the sexual networks of Black YMSM may help to do so. To achieve this goal, strategies for PrEP implementation must be cognizant of racial differences in structural barriers as well as stigma, otherwise they risk widening rather than shrinking existing disparities.
Our exploratory spatial analyses revealed geographic differences within the city of Chicago in the endorsement of PrEP stigma. More specifically, the two clusters of high PrEP stigma scores were centered in communities on the south and west side of the city; examination of these communities on maps from the Chicago Department of Public Health revealed these community areas are characterized by high HIV incidence and high concentrations of racial minorities relative to other community areas in Chicago.(56) Interestingly, these analyses found a particularly low concentration of PrEP stigma in a community area on the north side of the city. This community area is also characterized by a relatively high HIV incidence, but a lower concentration of racial minorities. Furthermore, this north side neighborhood has high visibility of LGBT people, community centers and businesses. This increased visibility of LGBT people and organizations means that individuals in this community area are more likely to see advertisements about PrEP, have healthcare providers that are more knowledgeable about PrEP (and LGBT health more broadly), and encounter other individuals who are on PrEP. Our analyses showing a significant correlation between perceived neighborhood LGBT stigma and PrEP stigma support this hypothesis. Consistent with prior research linking homophobia with HIV risk,(69) our findings suggest that addressing anti-LGBT bias and discrimination may support PrEP implementation. Future research is needed on how to reduce PrEP stigma in geographic areas that have lower concentrations of LGBT people and businesses. Increasing PrEP awareness campaigns citywide, particularly campaigns that depict individuals of varied backgrounds, may help to increase awareness and reduce stigma. However, there are clearly structural forces in place in certain communities on the south and west side of Chicago that are contributing to stigma. Increasing medical provider knowledge about PrEP in these areas, and encouraging providers to recommend PrEP for all individuals who meet CDC guidelines for its use may help expand the reach of PrEP. However, given that the majority of individuals who meet CDC guidelines for PrEP use are MSM, improving access to LGBT-affirming care will be a necessary step in reducing stigma and increasing PrEP uptake.
Finally, our analyses indicate that awareness of and knowledge about PrEP play a central role in both reducing stigma and increasing positive attitudes. Not only did previous awareness of PrEP and knowledge that PrEP lowers HIV risk reduce PrEP stigma and increase positive attitudes about PrEP, but restricting our exploratory spatial analyses to just those individuals who had previously heard of PrEP reduced geographic differences in PrEP attitudes. This lends further support to the idea that increasing visibility of PrEP campaigns and improving provider awareness of and knowledge about PrEP may help to reduce PrEP stigma in key community areas in the city of Chicago. While these data do not allow us to determine what is at the root of this shift toward reduced stigma and increased positive attitudes once one becomes aware of PrEP, increasingly widespread advertising campaigns and shifting community norms are likely candidates. Furthermore, individuals who endorsed more self-efficacy in talking to their partners about PrEP had lower PrEP stigma and more positive attitudes about PrEP, which indicates that YMSM may need to be taught skills necessary to have effective conversations with their partners about HIV risk reduction.
These findings should be interpreted in the context of several limitations. First, these analyses were cross-sectional in nature, and therefore we are not able to make any conclusions about the causes of the observed differences in PrEP attitudes. PrEP stigma and positive attitudes were measured among individuals who had not used PrEP in the prior 6 months, and it is possible some individuals had used PrEP earlier and had discontinued, which could affect their subsequent attitudes. Future longitudinal research with this cohort of YMSM will examine changes over time in PrEP stigma and positive attitudes, the causes of these changes, and the impact of PrEP attitudes on individual and neighborhood PrEP uptake. Second, our measure defined and explained PrEP only to individuals who had not heard of it before, which leaves the possibility that some individuals had heard of it but believed incorrect information. In future administrations of this scale we recommend everyone be provided the same factual information. Third, our exploratory spatial analyses were limited in that certain community areas had relatively low numbers of study participants residing within their boundaries. As such, we may not have observed some areas of the city of Chicago that are characterized by differing levels of PrEP attitudes. Fourth, knowledge of PrEP was assessed with a single item, which has lower reliability than a multi-item scale. Finally, these data come from a large cohort of racially-diverse YMSM living in Chicago and surrounding areas. These findings may not generalize to other areas of the U.S. that have more or less exposure to PrEP messaging, higher or lower concentrations of LGBT individuals, and different distributions of racial groups across community areas. This newly-developed measure of PrEP attitudes, including PrEP stigma and positive attitudes, should be evaluated in multiple contexts in order to assess generalizability of these findings.
These limitations notwithstanding, these analyses provide important information about PrEP attitudes and how PrEP stigma differs between individuals and across communities. Overall, we observed generally positive attitudes about PrEP, but we also observed important racial and geographic differences in the endorsement of PrEP stigma. If we do not work to reduce PrEP stigma through increased PrEP awareness and knowledge, these negative attitudes may serve as a critical barrier to PrEP uptake amongst those YMSM at high risk for HIV infection. Indeed, reducing PrEP stigma may be a key component to the widespread effectiveness of PrEP at curbing the domestic HIV epidemic.
Acknowledgments
We would like to thank participants of RADAR. RADAR is funded by the National Institute on Drug Abuse of the National Institutes of Health under award number U01 01DA036939. Third Coast Center for AIDS Research is supported by the National Institutes of Health under award number P30 AI117943. The content of this article is solely the responsibility of the authors and does not necessarily reflect the view of the National Institutes of Health.
Appendix A: Measure of PrEP Stigma and Positive Attitudes
Before today, have you ever heard of pre-exposure prophylaxis (PrEP)?
No (go to prompt A)
Yes (go to prompt B)
Prompt A
Pre-exposure prophylaxis (PrEP) is a way for people who do not have HIV, but who are at substantiated risk of getting it to prevent HIV infection by taking a pill every day. When someone is exposed to HIV through sex or injection drug use, the pill can work to keep the virus from establishing a permanent infection. When taken consistently, PrEP has been shown to reduce the risk of HIV infection in people who are at high risk by up to 92%. PrEP is much less effective if it is not taken consistently. People have different opinions about PrEP. Now that you have learned about PrEP, please indicate how much you agree with the following statement.
Prompt B
People have different opinions about PrEP. Please indicate how much you agree with the following statements.
I think people should take PrEP. (PA)
People who are on PrEP sleep around. (PS)
People who are on PrEP are irresponsible. (PS)
Having sex with someone on PrEP is risky. (PS)
People who are on PrEP are making a smart decision to protect their health. (PA)
I would not trust someone who told me they were on PrEP. (PS)
People who are on PrEP can’t control their sex drive. (PS)
People who are on PrEP use it as an excuse to have sex without a condom. (PS)
Many people on PrEP lie about whether or not they take it every day. (PS)
People who are on PrEP are responsible. (PA)
Response Options: 1=Strongly disagree, 2=Disagree, 3=Neither agree nor disagree, 4=Agree, 5=Strongly agree
*PS = PrEP stigma subscale, PA = Positive attitudes subscale
Author Recommendations
For future use of this measure, the authors recommend displaying Prompt A to all respondents regardless of their level of PrEP awareness at time of data collection and scoring the measure by calculating the mean value for each subscale.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: All authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the Northwestern University Institutional Review Board and with the 1964 Helsinki declaration and its later amendments. Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.CDC. HIV Surveillance Report, 2015. 2016 [Available from: http://www.cdc.gov/hiv/library/reports/surveillance/
- 2.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen SE, Vittinghoff E, Bacon O, Doblecki-Lewis S, Postle BS, Feaster DJ, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP demonstration project. J Acquir Immune Defic Syndr. 2015;68(4):439–48. doi: 10.1097/QAI.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2015 doi: 10.1016/S0140-6736(15)00056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Food and Drug Administration. FDA approves first drug for reducing the risk of sexually acquired HIV infection. U.S. Department of Health and Human Services; 2012. [Google Scholar]
- 6.CDC; Services DoHaH, editor. Preexposure prophylaxis for the prevention of HIV infection in the United States - 2014: A clinical practice guideline. 2014. [Google Scholar]
- 7.Strauss BB, Greene GJ, Phillips G, 2nd, Bhatia R, Madkins K, Parsons JT, et al. Exploring Patterns of Awareness and Use of HIV Pre-Exposure Prophylaxis Among Young Men Who Have Sex with Men. AIDS Behav. 2017;21(5):1288–98. doi: 10.1007/s10461-016-1480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krakower DS, Mimiaga MJ, Rosenberger JG, Novak DS, Mitty JA, White JM, et al. Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an Internet social networking site. PLoS One. 2012;7(3):e33119. doi: 10.1371/journal.pone.0033119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal Awareness and Stalled Uptake of Pre-Exposure Prophylaxis (PrEP) Among at Risk, HIV-Negative, Black Men Who Have Sex with Men. AIDS Patient Care STDs. 2015;29(8):423–9. doi: 10.1089/apc.2014.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP Uptake Among Racially/Ethnically Diverse Young Men Who Have Sex With Men: The P18 Study. AIDS Educ Prev. 2015;27(2):112–25. doi: 10.1521/aeap.2015.27.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr. 2009;50(1):77–83. doi: 10.1097/QAI.0b013e31818d5a27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brooks RA, Landovitz RJ, Kaplan RL, Lieber E, Lee SJ, Barkley TW. Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: A mixed methods study. AIDS Patient Care STDs. 2012;26(2):87–94. doi: 10.1089/apc.2011.0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men. Curr HIV Res. 2013;11(7):520–7. doi: 10.2174/1570162x12666140129100411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goffman E. Stigma; notes on the management of spoiled identity. Englewood Cliffs, N.J: Prentice-Hall; 1963. p. 147. [Google Scholar]
- 15.Neighbors C, Lee CM, Lewis MA, Fossos N, Larimer ME. Are social norms the best predictor of outcomes among heavy-drinking college students? Journal of studies on alcohol and drugs. 2007;68(4):556–65. doi: 10.15288/jsad.2007.68.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ajzen I. Understanding attitudes and predicting social behavior. Englewood Cliffs, N.J: Prentice-Hall; 1980. p. x.p. 278. [Google Scholar]
- 17.Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(Pt 4):471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 18.Van de Bongardt D, Reitz E, Sandfort T, Dekovic M. A meta-analysis of the relations between three types of peer norms and adolescent sexual behavior. Social Psychology Review. 2015;19(3):203–34. doi: 10.1177/1088868314544223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manning M. The effects of subjective norms on behaviour in the theory of planned behaviour: a meta-analysis. Br J Soc Psychol. 2009;48(Pt 4):649–705. doi: 10.1348/014466608X393136. [DOI] [PubMed] [Google Scholar]
- 20.Peterson JL, Bakeman R. Impact of beliefs about HIV treatment and peer condom normas on risky sexual behavior among gay and bisexual men. J Community Psychol. 2006;34:37–46. [Google Scholar]
- 21.Bandura A. Social foundations of thought and action: A social cognitive theory. Engelwood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 22.Duran D. Truvada Whores? HuffPost Gay Voices. 2012 [Available from: http://www.huffingtonpost.com/david-duran/truvada-whores_b_2113588.html.
- 23.Spieldenner A. PrEP Whores and HIV Prevention: The Queer Communication of HIV Pre-Exposure Prophylaxis (PrEP) Journal of Homosexuality. 2016;63(12):1685–97. doi: 10.1080/00918369.2016.1158012. [DOI] [PubMed] [Google Scholar]
- 24.Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: A call to destigmatize "Truvada Whores". Am J Public Health. 2015;105(10):1960–4. doi: 10.2105/AJPH.2015.302816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eaton LA, Kalichman S. Risk compensation in HIV prevention: implications for vaccines, microbicides, and other biomedical HIV prevention technologies. Curr HIV/AIDS Rep. 2007;4(4):165–72. doi: 10.1007/s11904-007-0024-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blumenthal J, Jain S, Krakower D, Sun X, Young J, Mayer K, et al. Knowledge is power! Increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19(5):802–10. doi: 10.1007/s10461-015-0996-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–40. doi: 10.1007/s10461-013-0675-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers' perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18(9):1712–21. doi: 10.1007/s10461-014-0839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Puro V, Palummieri A, De Carli G, Piselli P, Ippolito G. Attitude towards antiretroviral Pre-Exposure Prophylaxis (PrEP) prescription among HIV specialists. BMC Infect Dis. 2013;13:217. doi: 10.1186/1471-2334-13-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marcus JL, Glidden DV, Mayer KH, Liu AY, Buchbinder SP, Amico KR, et al. No evidence of sexual risk compensation in the iPrEx trial of daily oral HIV preexposure prophylaxis. PLoS One. 2013;8(12) doi: 10.1371/journal.pone.0081997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guest G, Shattuck D, Johnson L, Akumatey B, Clarke EE, Chen PL, et al. Changes in sexual risk behavior among participants in a PrEP HIV prevention trial. Sex Transm Dis. 2008;35(12):1002–8. [PubMed] [Google Scholar]
- 33.Liu AY, Vittinghoff E, Chillag K, Mayer K, Thompson M, Grohskopf L, et al. Sexual risk behavior among HIV-uninfected men who have sex with men participating in a Tenofovir preexposure prophylaxis randomized trial in the United States. J Acquir Immune Defic Syndr. 2013;64(1):87–94. doi: 10.1097/QAI.0b013e31828f097a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lal L, Audsley J, Murphy D, Fairley CK, Stoove M, Roth N, et al. Medication adherence, condom use and sexually transmitted infections in Australian PrEP users: interim results from the Victorian PrEP Demonstration Project. AIDS. 2017 doi: 10.1097/QAD.0000000000001519. [DOI] [PubMed] [Google Scholar]
- 35.Oldenburg CE, Nunn AS, Montgomery M, Almonte A, Mena L, Patel RR, et al. Behavioral Changes Following Uptake of HIV Pre-exposure Prophylaxis Among Men Who Have Sex with Men in a Clinical Setting. AIDS Behav. 2017 doi: 10.1007/s10461-017-1701-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Newcomb ME, Moran K, Feinstein BA, Forscher E, Mustanski B. Pre-Exposure Prophylaxis (PrEP) Use and Condomless Anal Sex: Evidence of Risk Compensation in a Cohort of Young Men Who Have Sex with Men. J Acquir Immune Defic Syndr. 2017 doi: 10.1097/QAI.0000000000001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eaton LA, Kalichman SC, Price D, Finneran S, Allen A, Maksut J. Stigma and Conspiracy Beliefs Related to Pre-exposure Prophylaxis (PrEP) and Interest in Using PrEP Among Black and White Men and Transgender Women Who Have Sex with Men. AIDS Behav. 2017;21(5):1236–46. doi: 10.1007/s10461-017-1690-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Golub SA, Gamarel KE, Surace A. Demographic Differences in PrEP-Related Stereotypes: Implications for Implementation. AIDS Behav. 2015 doi: 10.1007/s10461-015-1129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care. 2017;29(11):1351–8. doi: 10.1080/09540121.2017.1300633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lelutiu-Weinberger C, Golub SA. Enhancing PrEP Access for Black and Latino Men Who Have Sex With Men. J Acquir Immune Defic Syndr. 2016;73(5):547–55. doi: 10.1097/QAI.0000000000001140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schuster MA, Collins R, Cunningham WE, Morton SC, Zierler S, Wong M, et al. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. 2005;20(9):807–13. doi: 10.1111/j.1525-1497.2005.05049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–8. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;10(5):473–82. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Golin C, Isasi F, Bontempi JB, Eng E. Secret pills: HIV-positive patients' experiences taking antiretroviral therapy in North Carolina. AIDS Educ Prev. 2002;14(4):318–29. doi: 10.1521/aeap.14.5.318.23870. [DOI] [PubMed] [Google Scholar]
- 45.Mustanski B, Swann G, Newcomb ME, Prachand N. Effects of parental monitoring and knowledge on substance use and HIV risk behaviors among young men who have sex with men: Results from three studies. AIDS Behav. 2017;21(7):2046–58. doi: 10.1007/s10461-017-1761-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Janulis P, Feinstein BA, Phillips G, 2nd, Newcomb ME, Birkett M, Mustanski B. Sexual Partner Typologies and the Association Between Drug Use and Sexual Risk Behavior Among Young Men Who Have Sex With Men. Arch Sex Behav. 2017 doi: 10.1007/s10508-016-0909-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge B, Sheeran P, et al. A network-individual-resource model for HIV prevention. AIDS Behav. 2010;14(Suppl 2):204–21. doi: 10.1007/s10461-010-9803-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Duncan SC, Duncan TE, Hops H. Analysis of longitudinal data within accelerated longitudinal designs. Psychol Methods. 1996;1(3):236–48. [Google Scholar]
- 50.CDC. Diagnoses of HIV Infection among Adolescents and Young Adults in the United States and 6 Dependent Areas 2010–2014. 2015 [Available from: http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-21-3.pdf.
- 51.CDC. Pre-exposure prophylaxis (PrEP) Atlanta, GA: Centers for Disease Control and Prevention; 2016. [Available from: https://www.cdc.gov/hiv/risk/prep/ [Google Scholar]
- 52.Mustanski B, Starks T, Newcomb ME. Methods for the design and analysis of relationship and partner effects on sexual health. Arch Sex Behav. 2014;43(1):21–33. doi: 10.1007/s10508-013-0215-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Swann G, Newcomb ME, Mustanski B. Validation of the HIV Risk Assessment of Sexual Partnerships (H-RASP): Comparison to a 2-Month Prospective Diary Study. Arch Sex Behav. 2017 doi: 10.1007/s10508-017-1033-2. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. Journal of Educational Research. 2006;99(6):323–37. [Google Scholar]
- 55.City of Chicago. Chicago data portal. 2017 [Available from: https://data.cityofchicago.org/Facilities-Geographic-Boundaries/Boundaries-Community-Areas-current-/cauq-8yn6.
- 56.Chicago Department of Public Health. HIV/STI Surveillance Report 2016. Chicago, IL: 2016. [Google Scholar]
- 57.Ord JKGA. Local spatial autocorrelation statistics: Distributional issues and an application. Geographical Analysis. 1995;24(4) [Google Scholar]
- 58.Mustanski B, Newcomb M, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48(2–3):218–53. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hosek SG, Siberry G, Bell M, Lally M, Kapogiannis B, Green K, et al. The acceptability and feasibility of an HIV preexposure prophylaxis (PrEP) trial with young men who have sex with men. J Acquir Immune Defic Syndr. 2013;62(4):447–56. doi: 10.1097/QAI.0b013e3182801081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lewis MA, Patrick ME, Litt DM, Atkins DC, Kim T, Blayney JA, et al. Randomized controlled trial of a web-delivered personalized normative feedback intervention to reduce alcohol-related risky sexual behavior among college students. J Consult Clin Psychol. 2014;82(3):429–40. doi: 10.1037/a0035550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shelley G, Williams W, Uhl G, Hoyte T, Eke A, Wright C, et al. An Evaluation of Mpowerment on Individual-Level HIV Risk Behavior, Testing, and Psychosocial Factors Among Young MSM of Color: The Monitoring and Evaluation of MP (MEM) Project. AIDS Educ Prev. 2017;29(1):24–37. doi: 10.1521/aeap.2017.29.1.24. [DOI] [PubMed] [Google Scholar]
- 63.Hosek SG, Lemos D, Hotton AL, Fernandez MI, Telander K, Footer D, et al. An HIV intervention tailored for black young men who have sex with men in the House Ball Community. AIDS Care. 2015;27(3):355–62. doi: 10.1080/09540121.2014.963016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bull S, Pratte K, Whitesell N, Rietmeijer C, McFarlane M. Effects of an Internet-Based Intervention for HIV Prevention: The Youthnet Trials. AIDS Behav. 2008 doi: 10.1007/s10461-008-9487-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Garofalo R, Hotton AL, Kuhns LM, Gratzer B, Mustanski B. Incidence of HIV infection and sexually transmitted infections and related risk factors among very young men who have sex with men. J Acquir Immune Defic Syndr. 2016;72(1):79–86. doi: 10.1097/QAI.0000000000000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM, Group NS. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS. 2013;27(2):269–78. doi: 10.1097/QAD.0b013e32835ad489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The role of geographic and network factors in racial disparities in HIV among young men who have sex with men: an egocentric network study. AIDS Behav. 2015;19(6):1037–47. doi: 10.1007/s10461-014-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sifakis F, Hylton JB, Flynn C, Solomon L, Mackellar DA, Valleroy LA, et al. Racial disparities in HIV incidence among young men who have sex with men:The baltimore young men's survey. J Acquir Immune Defic Syndr. 2007;46(3):343–8. doi: 10.1097/QAI.0b013e31815724cc. [DOI] [PubMed] [Google Scholar]
- 69.Jeffries WL, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS Behav. 2013;17(4):1442–53. doi: 10.1007/s10461-012-0189-y. [DOI] [PubMed] [Google Scholar]