Abstract
This paper reports an ethnobotanical study that focused on the traditional medicinal plants used by local communities to treat human diseases. Ethnobotanical study of medicinal plants was carried out from June 25 to September 5, 2015, in Berbere district of Oromia region, Ethiopia. The study focused on documentation of medicinal plants used to treat various human diseases in the study area. Ethnobotanical data were collected using semistructured interviews, group discussion, guided field walks, and observations with participants. Preference ranking, paired comparison, direct matrix ranking, and informant consensus factors (ICF) were used to analyze the importance of some plant species. A total of 70 medicinal plants, distributed in 56 genera and 46 families, were collected and identified. Plant family with the highest medicinal plants in the study area used for various diseases treatment was Euphorbiaceae (11.4%). The result of growth form analysis showed that shrubs constituted the highest proportion of medicinal plants (48.6%). Roots, 43 (44.8%), were the most frequently utilized plant parts for preparation of traditional herbal medicines. Crushing was a widely used mode of preparation of traditional remedies where oral administration (37.5%) was the dominant route. The highest informants consensus factor (ICF) values were linked to gonorrhea and syphilis disease (0.95); the lowest was linked with external parasites and wound (0.69). Local people in the study area possess traditional knowledge of medicinal plants to treat various human ailments; however, agricultural expansion and disinterest of young generation became the major threat to medicinal plants. It is, therefore, necessary to preserve this indigenous knowledge on traditional medicines by proper documentation, identification of plant species used, and herbal preparation. To save medicinal plants from further loss, involving local communities in cultivation of the most utilized medicinal plants is recommended.
1. Introduction
Plant resources have remained an integral part of human society throughout history. After fulfilling the primary needs like food and shelter, man has sought for a suitable remedy among plants for curing various diseases [1].
Traditional medicine is defined as indigenous medicine that is used to maintain health and to prevent, diagnose, and treat physical and mental illnesses differently from allopathic medicine based on theories, beliefs, and experiences [2]. Traditional medicine has been used for thousands of years with great contributions made by practitioners to human health, particularly as primary health care providers at the community level and has maintained its popularity worldwide [3]. According to Sofowora [4], about 60-85% of the population in every country of the developing world has to rely on traditional medicine. The practice of traditional medicine is widespread in China, India, Japan, Pakistan, Sri Lanka, Thailand, and Korea [5]. In China, traditional medicine accounts for around 40% of all health care delivered and is used to treat roughly 200 million patients annually [6].
In Ethiopia, plants have been used as a source of medicine from time immemorial to treat different ailments due to its long history, and traditional medicine has in fact become an integral part of culture [7]. These traditional medical practices and remedies are recorded in oral tradition and in early medico-religious manuscripts and traditional pharmacopoeias, which, according to the estimates of some historians, date back to the 15th century AD [8].
Ethiopia possesses about 6,000 species of vascular plants which could be due to its different topography and climatic conditions [9]. About 80% of human population and 90% of livestock rely on traditional medicine in this country [10]. Traditional medicine of Ethiopia is commonly used to treat various human and livestock ailments. Traditional healers known by different names in different parts of the country are the primary players in the curative aspect of traditional medicine practice [11]. Thus, this study was initiated to document the traditional medicinal plants knowledge accumulated by local communities of Berbere district.
2. Methods
2.1. Study Area
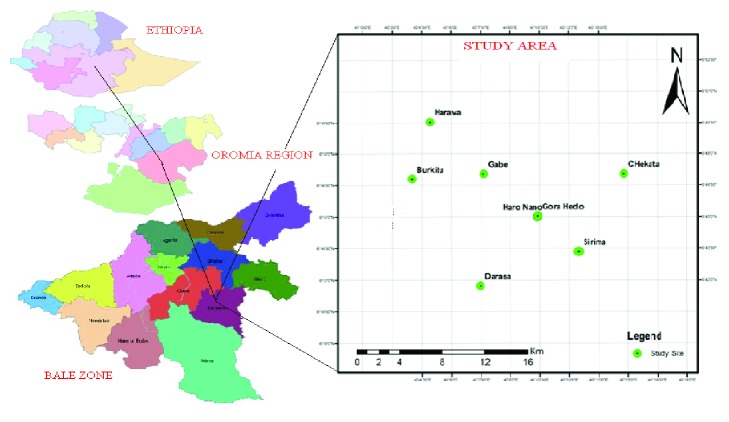
Berbere district is situated between 06°33′ N and 06°75′N and 039°95′ E and 040°29′E. It is located at about 526 km southeast of Addis Ababa, in Bale Zone of Oromia Regional State. This district has 17 kebeles which are characterized by undulating highlands in the north and lowlands in the south (Figure 1).
Figure 1.
Map showing study area.
2.2. Selection of Study Sites
A reconnaissance survey of the study area was conducted from June 25 to July 5, 2015. The study sites were selected depending on recommendation from elders, local authorities, and altitudinal range. Thus, the study was carried out in eight kebeles from two agro-climatic zones.
2.3. Selection of Participants
A total of 60 participants (41 men and 19 women) were selected randomly from the representative kebeles. Representative common participants and knowledgeable traditional medicine practitioners (key participants) of Berbere district were selected using random and purposive sampling approaches, respectively, following Martin [12]. Twenty key participants were selected purposively and systematically based on the recommendations of knowledgeable elders, local authorities, and development agents. The selection of key participants was also based on the quality of explanations that particular participants gave during an interview. Local healers automatically qualified as key participants being traditional experts who are guardians of indigenous knowledge on medicinal plants.
2.4. Ethnobotanical Data Collection
Ethnobotanical data were collected from July 6, 2015, to September 5, 2015. The standard data collection methods [12–14] have been followed to document indigenous knowledge of the local community on health, use, conservation, and threats of medicinal plants. The techniques employed for data collection were semistructured interviews, group discussion, guided field walks, and observations with participants. Semistructured interviews were undertaken based on checklist of questions prepared in English and translated to ‘Afaan Oromo', the language of local people. Information was carefully recorded during an interview with a participant. The interview was guided to cover the key topics on the checklist. The place and the time for interview were set based on the interest of the participants. Field observations were performed with the help of local guides on the morphological features and habitats of each medicinal plant species in the field. Brief group discussions were made with participants regarding the medicinal plants in the study area. The discussions were conducted on threats to medicinal plants, conservation of the medicinal plants, and transferability of knowledge in the community. Letter of consent was taken from Jimma University, prior to the data collections. Verbal consents were also obtained from the participants by performed group discussions about the objectives of the study prior to the interviews, and all data were collected through their oral consents.
2.5. Voucher Specimen Collection
The voucher specimens were collected onsite during guided field walk, numbered, pressed, dried, and deep frozen for identification. Identification of specimens was carried out both in the field and in the herbarium. Identification was also carried out using Flora of Ethiopia comparing with already identified specimens. Finally, the identified specimens were stored at the National Herbarium of the Addis Ababa University, Ethiopia.
2.6. Data Analysis
The collected ethnobotanical data were entered into Excel spreadsheet 2007 and summarized using descriptive statistical methods such as frequency, percentage, tables, and graphs. Preference ranking and paired comparison were computed following [13]. Preference ranking was conducted for five important medicinal plants used to treat stomachache. Ten randomly selected participants from total key participants were participated in this exercise to identify the best preferred medicinal plants for treatment of stomachache.
In paired comparison, ten participants were selected and asked to choose the best item from every pair according to personal perception in treating wound. The total number of possible pairs [15] was obtained by applying the formula n (n-1)/2, where n is the number of medicinal plants being compared. A total rank of paired comparison was obtained by summing the number of times each item was chosen. An item with the highest frequency of choices had the highest score.
Direct matrix ranking is used to compare multipurpose uses of a given plant species based on information gathered from participants, number of multipurpose species were selected out of the total medicinal plants, and use diversities of these plants were listed for four randomly selected key participants to assign use values to each species.
Informants consensus factor (ICF) was calculated for each category to identify the agreements of the participants on reported cures for the group of ailments. The ICF was calculated as follows [15].
| (1) |
where ICF is informants consensus factor, nur is number of use citation in each category, and nt is number of species used.
3. Results and Discussion
3.1. Medicinal Plants of the Study Area
A total of 70 medicinal plant species belonging to 56 genera and 39 families were used by the local communities to treat 42 human ailments (Table 1). Euphorbiaceae was the leading family with eight species (11.4%). Of the ethnomedicinally important plant species that are used to treat human ailments recorded in eight kebeles of Berbere district, 12 (19%) were from homegardens and 58 (81%) species were from the wild. Various studies conducted in Ethiopia reported that most of medicinal plants are being harvested from noncultivated areas. For instance, the study conducted by [16] indicated that the highest number (90.43%) of medicinal plants was collected from wild in Mana Angetu District. Similarly, [17, 18] reported that about 54% and 49% of medicinal plants were harvested from wild in Tehuledere and Halaba districts, respectively. This observation is a good indication of the fact that the local people have not yet started cultivating most of the plant species they are using as remedies.
Table 1.
List of medicinal plants used for human Ailments (Ha: habit, S: shrub, C: climber, T: tree, E: epiphyte, and H: herb, A/O-Afaan Oromo).
| V. No | Family | Scientific name | Vernacular name (A/O) | Ha. | Ailments | Part used | Mode of preparation | Dosage | Route of administration |
|---|---|---|---|---|---|---|---|---|---|
| TT 34 | Acanthaceae | Barleria eranthemoides R. Br. ex C. B. Cl. | Shabi | H | Heart burn | Root | The roots crushed and mixed with water and then given | Length of finger | Oral |
|
| |||||||||
| TT 5 | Acanthaceae |
Justicia schimperiana T. Anderson |
Dhumugaa | S | Bat urine | Leaves | The leaves are crushed; drink the juice and the residue put on the head for 7 days | 5 leaves | Oral |
|
| |||||||||
| TT 17 | Aloaceae | Aloe sp. | Argiisa | S | Spleeno megally | Latex | The latex from leaf is taken with honey in the morning for 3 days | 2-4 bottle stopper | Oral |
|
| |||||||||
| TT 12 | Anacardaceae | Schinus molle L. | Qundbarbare | T | Bile | Seeds | The seed powdered and boiled with tea then 1 cup is given for 3 mornings | 3-5 seeds | Oral |
| Spleeno megally | Leaves | The leaves are crushed and the filter is given for 5 days | 5 leaflets | ||||||
|
| |||||||||
| TT 56 | Anacardiaceae |
Rhus natalensis (Bernh. ex Krauss) F. A. Barkley |
Dabobessaa | S | Boils | Root | The root is crushed and ties on the infected area | 1 local spoon | Dermal |
|
| |||||||||
| TT 39 | Apocynaceae | Carissa spinarum L. | Hagamsa | S | Wound | Root | Root bark is pounded & applied on wound for 3 days | Quarter of palm | Dermal |
| Evil eye | Root | The smoke of pounded roots is inhaled | A palm of pounded root | ||||||
|
| |||||||||
| TT 36 | Asteraceae | Laggera crispata (Vahl) F.N. Hepper & J.R.I. Wood | Rashadii | H | Dizziness | Leaves | The crushed leaf is tie on the head for 3 days | 5-8 leaves | Dermal |
|
| |||||||||
| TT 30 | Asteraceae | Xanthium strumarium L. | Katerokantro | H | Dandruff | Leaves | The powdered root is painted on the head | 5 leaves /treatment | Dermal |
|
| |||||||||
| TT 37 | Asteraceae | Vernonia amygdalina Del. | Dhebicha | S | Intestinal worm | Leaves | Drinking the decocted leaves with 1 cup of coffee for elders and half for children | 3 -7 leaves | Oral |
| Headache | Leaves | Crushed leaves are put on head for 3 days | 10 leaves | Dermal | |||||
|
| |||||||||
| TT 11 | Bignoniaceae | Stereospermum kunthianum Cham. | Wolgabis | T | Kidney | Bark | Drunk the juice from crushed bark & residue of the bark is steam bathed | 5 spoon of crushed bark | Oral |
|
| |||||||||
| TT 55 | Boraginaceae | Cordia africana Lam. | Waddeessa | T | Itching | Root | The roots are powdered then painted at bed time for 5 days | 1 hand palm | Dermal |
|
| |||||||||
| TT 16 | Boraginaceae | Cynoglossum lanceolatum Forrsk | Maxxannee | H | Fibril illness | Leaves | Juice of the leaf is taken. | Half to 1 stick | Oral |
| Boils | Leaves | Fresh leaf is ground and then tie on | 5 leaves | Dermal | |||||
|
| |||||||||
| TT 25 | Boraginaceae | Ehretia cymosa Thonn. | Ulaagaa | S | Bleeding | Leaves | The squeezed leaves put on the cut area | 1-5 leaves | Dermal |
| Fibril illness | Leaves | The fluids from the leaves are taken through nose | 2 leaves | Oral | |||||
|
| |||||||||
| TT 21 | Canellaceae | Warburgia ugandensis Sprague | Befit | T | Boils | Stem | Pounded stem is concocted with butter and put on the infected part | 1 sticken | Dermal |
| Cough | Stem | The smoke of vascular part is inhaled to relief from cough | 2-3 sticken | ||||||
|
| |||||||||
| TT 7 | Capparidaceae | Capparis sepiaria L. | Gursama | S | Stomachache | Bark | The bark is pounded and drink with hot water. | 3-5 spoon | Oral |
|
| |||||||||
| TT 59 | Capparidaceae | Capparis tomentosa Lam. | Lukkuu | S | Mental health problem | Root | The roots are powdered and then dry bathed for 3 days | 1 palm of powdered root | Dermal |
|
| |||||||||
| TT 18 | Caricaceae | Carica papaya L. | Papaayee | S | Diarrhea | Seed | Seeds ground and boiled with coffee and taken with honey | 15-20 seed | Oral |
| Ascariasis | |||||||||
|
| |||||||||
| TT 20 | Cuccurbitaceae | Cucurbita pepo L. | Dabaqulaa | H | Gastritis | Leaves | The leaf cooked with Brassica oleracea then eaten | 2-3 leaves | Oral |
|
| |||||||||
| TT 65 | Ebenaceae | Euclea racemosa L. | Mi'eesaa | S | Evil spirit& evil eye | Root | Drinking the Crushed & decocted root and inhaling the smoke | 1 tea spoon | Oral |
| Heartburn | Root | The root crushed and mixed with water and drink 1 cup of glass | 1 tea spoon | ||||||
|
| |||||||||
| TT 31 | Euphorbiaceae |
Bridelia scleroneura Mul.Arg. |
Abayi | T | Scabies | Seed | The seeds are crushed and applied on the affected area | 5-8 seed | Dermal |
|
| |||||||||
| TT 29 | Euphorbiaceae | Croton macrostachyus Hochst. ex Del. | Bakkanisa | T | Hemorrhoids | Bark | Bark is crushed and cooked with meat then soup is taken | 2 spoon | Oral |
| Gonorrhea | Root | The root is decocted, and the mixture is taken. | 3-6 spoon | ||||||
| Spleeno megally | Bark | Bark is crushed and mixed with water and then taken. | Quarter of palm | ||||||
|
| |||||||||
| TT 28 | Euphorbiaceae | Euphorbia sp. | Guurii | H | Eczema | Leaves | The crushed and dried leaves are mixed with citrus aurantifolia and applied on the infected area | 2-7 leaves | Dermal |
|
| |||||||||
| TT 19 | Euphorbiaceae | Euphorbia heterophylla L. | Annoo | H | Wound | Leaves | Leaves crushed and put on the wound for 3 days | 2 spoon | Dermal |
|
| |||||||||
| TT 40 | Euphorbiaceae | Euphorbia hirta Millsp. | Qoricha aroo | H | Scabies | Root | The fresh root is crushed and painted on the body with butter for 5 mornings | 1 stick of root | Dermal |
|
| |||||||||
| TT 45 | Euphorbiaceae | Jatropha curcas L. | Abatamuluk | S | Intestinal worm | Root | Root is crushed and drink with half cup of coffee | 1 tea spoon | Oral |
| Excess bile production | Seed | Powdered seed are eaten with honey | 2 spoons | ||||||
|
| |||||||||
| TT 4 | Euphorbiaceae |
Phyllanthus ovalifolius A. Radcliffe-Smith |
Gurbi adi | S | Scabies | Leaves | The leaves squeezed by hand and applied on the skin | 5-17 leaves | Dermal |
|
| |||||||||
| TT 69 | Euphorbiaceae | Ricinus communis L. | Qobboo | S | Intestinal worm | Root and seed | Roots and seeds are crushed and drink with 1 cup of water | 1-3 seeds and 2 sticken | Oral |
|
| |||||||||
| TT 9 | Euphorbiaceae | Tragia cordata Michx. | Lalesa | C | Urinary tract | Root | The dried roots crushed and boiled then drinks the decocted | Half to 1 full hand | Oral |
| External parasite | Root | Powdered roots are applied to the affected cattle | 5-9 local spoons | Dermal | |||||
|
| |||||||||
| TT 49 | Fabaceae | Acacia mellifera detinens (Burch.) Brenan | Bilaal | S | Earache | Leaves | The leaf squeezed then droplet latex is applied to the ear | 1 leaf | Auricular |
| Eye disease | Leaves | The leaves are squeezed then the fluid is used as eye droplet | 3-5 leaves | Opticular | |||||
|
| |||||||||
| TT 10 | Fabaceae | Acacia senegal (L.) Willd. | Saphansa | T | Amebiasis | Latex from stem | Latex from the stem pounded and taken with honey | 3 spoon | Oral |
| Fire Wound | Latex | The powdered latex is applied on the wound | 1-2 bean size solid latex | Dermal | |||||
|
| |||||||||
| TT 70 | Fabaceae |
Calpurnia aurea (Ait.) Benth. |
Ceeka | S | Snake bite | Leaves | The decocted leaves are taken with Honey | 20 leaflets | Oral |
| Amebiasis | Root | The dried roots are crushed and boiled with leaf of coffee then 1 cup is given early in the morning | Half palm of hand | ||||||
|
| |||||||||
| TT 57 | Fabaceae | Rhynchosia ferruginea A.Rich. | Udusalim baricha | S | Amebiasis | Root | The crushed roots are mixed with water and the mixture is taken | 1-2 bottle stopper | Oral |
|
| |||||||||
| TT 47 | Fabaceae | Rhynchosia malacotricha Harms | Jidda dhiiga adii | S | Evil eye | Root | Dry bath of crushed root during bed time | 1-3 spoon | Dermal |
|
| |||||||||
| TT 13 | Fabaceae | Tamarindus indica L. | Roka | T | Bile and intestinal worm | Fruit | The Fruit juice is taken with hot water in early morning before breakfast | Up to 10 fruits | Oral |
|
| |||||||||
| TT 1 | Iradiaceae | Gladiolus schweinfurthii (Baker) Goldblatt & M.P. de Vos | Mirge | H | Headache | Root | The pounded root is dry bathed for 1-3 days | 1 tea spoon | Dermal |
|
| |||||||||
| TT 60 | Lamiaceae |
Clerodendrum myricoides (Hochst.) R.Br. ex Vatke |
Tiro | S | Earache | Root | Powdering the root and put small amount in the ear for 1hr and then wash | Half tea spoon | Auricular |
| Headache | Root | The crushed root is put on the head with butter for 2 days | 1 palm | Dermal | |||||
|
| |||||||||
| TT 15 | Lamiaceae | Ocimum lamiifolium Hochst. ex Benth. | Urgo haree/ Damakase | S | Fibril illness | Leaves | The fluid from the squeezed leaves are taken | 1-3 leaves depending on the age | Oral |
|
| |||||||||
| TT 53 | Lamiaceae | Premna schimperi Engl. | Urgeessaa | S | Mastitis | Root | The powdered roots are mixed with butter then painted on the breast of cows | 5 hand palms | Dermal |
| Boils | Leaves | crushed & pounded leaves are tied on the infected body | 3 spoons | Dermal | |||||
|
| |||||||||
| TT 66 | Loranthaceae | Erianthemum dregei (Eckl. & Zeyh.) van Tiegh. | Mankero mi'esa | E | Hyper menorrhea | Leaves | The leaves are crushed, and the juice is taken after 3 days of blood flow | 5 leaves | Oral |
|
| |||||||||
| TT 51 | Malvaceae | Sida rhombifolia L. | Gurbi | S | Epitaks/nose bleeding | Leaves | Leaf is squeezed and the liquid taken through the nose during bleeding | 2 leaves | Nasal |
|
| |||||||||
| TT 38 | Menispermaceae | Stephania abyssinica (Dill. & A. Rich.) Walp. | Baltokkee | Cl | stomachache | Root | The root is chewed, and the juice is swallowed | forefinger size | Oral |
|
| |||||||||
| TT 9 | Moringaceae |
Moringa stenopetala (E. G. Baker) Cufod. |
Shiferawu | T | Asthma | Root | The smoke of pounded root is inhaled at bed time for 3 days | Half palm | Oral |
|
| |||||||||
| TT 62 | Olacaceae | Ximenia americana L. | Hudhaa | S | Stomachache and tonsillitis | Root | The roots are crushed, pounded and then 1 cup is taken for 3 days | 2 spoons | Oral |
| Wound | Fruit | The oil from the fruit kernel is applied to flesh wounds to prevent infections | 1 bottle stopper | Dermal | |||||
|
| |||||||||
| TT 42 | Oleaceae | Olea europaea subsp. cuspidata (Wall.G.Don)Cif. | Ejersa | T | Bone TB | Root | The extracted oil from the roots put on the affected site | Half of tea spoon | Dermal |
| Wound | |||||||||
|
| |||||||||
| TT 43 | Plumbaginaceae | Plumbago zeylanica L. | Dhigaji | H | Gonorrhea | Root | The crushed root is cooked with meat and then eaten | 2 sticken | Oral |
| Hemorrhoids | Root | The pounded roots are mixed with honey and then put in the anus | Half palm | Dermal | |||||
| Toothache | Root | Small amount of crushed root put on the infected teeth | 1 sticken | ||||||
|
| |||||||||
| TT 14 | Polygalaceae | Polygala erioptera DC. | Harmal adii | H | Heart disease | Root | Pounding the root and chewing then drinking | 1-3 sticken | Oral |
|
| |||||||||
| TT 58 | Ranunculaceae | Clematis simensis Fresen. | Sariti/ fitii | Cl | Wound | Leaves | The crushed leaves are mixed with citrus lemon and then put on the wound | 2 leaves | Dermal |
| Stomachache | Root | The root pounded then taken with coffee for 3 days | The size of Fore finger | Oral | |||||
|
| |||||||||
| TT 41 | Rosaceae |
Prunus africana (Hook.f.) Kalkman |
Muka guracha | T | Wound | Bark | Crushed bark applies on the wounded area | Quarter palm | Dermal |
|
| |||||||||
| TT 35 | Rubiaceae | Coffea arabica L. | Buna | S | Scabies | Seed | The roosted seeds are powdered and applied on the infected area | 5-7 seeds | Dermal |
|
| |||||||||
| TT 23 | Rutaceae | Citrus aurantium L. | Harboo | S | Dermatophyte | Fruit | Fruit juice is used as cream ointment on head | 3 fruits | Dermal |
|
| |||||||||
| TT 64 | Rutaceae | Citrus sinensis (L.) Engl. | Burtukana | S | Stomach infection | Fruit | The juice is mixed with the fruits of Psidium guajava and taken early | 1-3 fruits | Oral |
| Wound | Bark | The dried bark is crushed and mixed with butter then creamed on the wound after washing the infected part | Half palm | Dermal | |||||
|
| |||||||||
| TT 54 | Rutaceae | Ruta chalepensis L. | Chelatama | S | Stomachache | Leaves | The leaves are chewed and the juice swallowed | 5 -10 leaf | Oral |
| Cough | Fruit | The fruits are boiled with tea and taken in the morning and night for 2 days | Up to 6 fruits | ||||||
|
| |||||||||
| TT 24 | Sapindaceae |
Dodonaea angustifolia (L. fil.) J.G.West |
Itachaa | S | Toothache | Root | Brushing the teeth | 1 stricken | Oral |
| Wound | Root | Squeezed root is smeared on the wound | Half spoon | Dermal | |||||
|
| |||||||||
| TT 48 | Sapotaceae | Mimusops kummel Bruce ex A. DC. | Qolati | T | Lung cancer | Root | The roots are grounded, and small quantity taken with water | 1 tea spoon | Oral |
| Fruit | The dried fruits are pounded and dissolved in water and given | 3 fruits | |||||||
|
| |||||||||
| TT 33 | Solanaceae | Datura stramonium L. | Manjii | H | Depression | Seed | The seed is grounded and smoked or mixed with butter and put on head | 15 seeds | Dermal |
|
| |||||||||
| TT 44 | Solanaceae | Nicotiana tabacum L. | Tamboo | H | Snake bite | Leaf | The leaf is chewed and the juice swallowed | 1 leaf | Oral |
|
| |||||||||
| TT 52 | Solanaceae |
Solanecio angulatus (Vahl) C.Jeffery |
Jiniras | H | Evil eye | Root | The powdered root is dry bathed at night for 3 days | 1 spoon | Oral |
|
| |||||||||
| TT 67 | Solanaceae | Solanum americanum Mill. | Mujulo | H | Intestinal worm | Leaves | The dried leaf is crushed | 7 leaves | Oral |
|
| |||||||||
| TT 68 | Solanceae | Solanum incanum L. | Hiddii | S | Emergency | Root | Chewing the root | Size of 1 sticken | Oral |
| Nose bleeding | Leaf | Juice of leaf is applied to nose | 1 leaf | Nasal | |||||
| Pain during menstruation | Root | Dried roots are chewed and juice intake to stomach | Half sticken | Oral | |||||
| Amebiasis | Root | Pounded roots are concocted with water and then taken | 2 sticken | Oral | |||||
|
| |||||||||
| TT 63 | Solanaceae |
Withania somnifera (L.) Dun. |
Unzo/ Gizawa | H | Evil eye | Root | Drinking the decocted roots and the residue is dry bathed | Half palm | Oral |
|
| |||||||||
| TT 32 | Tiliaceae | Grewia sp. | Gurbi dima | S | External parasite | Leaves | The leaves are squeezed and rubbed on the body | 5-15 leaves | Dermal |
|
| |||||||||
| TT 46 | Tiliaceae | Grewia villosa Willd. | Jidda dhiga dima | S | Headache | Root | Pounding the roots and dry bath during bed time | 1 and half palm | Oral |
|
| |||||||||
| TT 2 | Trymalaceae | Gnidia stenophylla Gilg. | Katarichaa | H | Intestinal worm | Root | The dried roots are crushed and mixed with water then taken for 2 days | 1 tea spoon | Oral |
| Amebiasis | Root | The powdered roots are taken with coffee in morning | 1-2 spoon | ||||||
| Liver disease | Root | The decoction of root is taken with goat milk | 1 tea spoon | ||||||
|
| |||||||||
| TT 61 | Ulmaceae | Celtis africana Burm. fil. | Mataqoma | T | Boils | Leaves | The leaves squeezed and tie on the swelled part | 5 leaves | Dermal |
|
| |||||||||
| TT 7 | Verbenaceae | Lippia adoensis Hochst. ex Walp. | Kusayee | S | Fibril illness | Leaves | The leaves squeezed and the filter is given through the nose and drink | 2 leaves | Oral |
|
| |||||||||
| TT 50 | Vitaceae |
Cayratia ibuensis (Hook.f.) Suess. |
Udusalim rumiyi | S | Liver disease | Root | The roots crushed and pounded then boiled and drink 2-3 cup of coffee in the morning | 5-7 of tea spoon | Oral |
|
| |||||||||
| TT 27 | Vitaceae | Cissus rotundifolia (Forssk.) Vahl | Burke | C | Swelling | Root | The crushed roots are tie on the swelled part | 1-5 full hand | Dermal |
| Wound | Root | Roots are pounded, mixed with water, rubbed and applied as ointment on wound | 2 hand palms | ||||||
|
| |||||||||
| TT 22 | Vitaceae | Cyphostemma sp. | Laaluu | C | Wound | Root | Root is pounded, mixed with water, rubbed and applied as ointment on wound | 2 bottle stopper | Dermal |
|
| |||||||||
| TT 26 | Zingiberaceae |
Zingiber officinale Roscoe |
Zinjibilaa | H | Cough, common cold & tonsillitis | Root | The roots crushed and boiled with tea and then taken | 2-5 medium root | Oral |
3.2. Growth Form of Medicinal Plants
The growth form analysis of medicinal plants revealed that shrubs constitute the highest proportion being represented by 34 species (48.6%), herbs represented by 17 species (24.3%), trees represented by 13 species (18.6%), and climbers represented by 5 species (7.1%), while there was one species (1.4%) of epiphyte (Figure 2).
Figure 2.
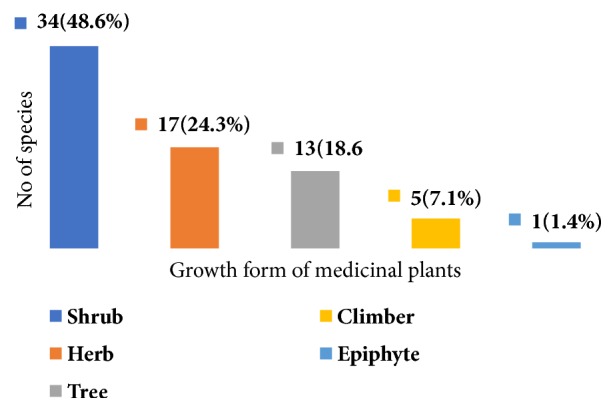
The habits (growth forms) of medicinal plants used to treat human ailments in the study area.
This finding shows that the most represented life forms of medicinal plants in the study area were shrubs followed by herbs. Similar findings were also reported in the earlier works in Ethiopia. For instance, [19] identified 46.8% shrubs and 24.1% herbs from Cheffa semi-wetland; [17] documented 46% shrubs and 25% herbs from Boosat subdistrict; [20] collected 37% of shrubs from Sekoru district, Jimma Zone. The more recent studies conducted by [21, 22] also reported the dominance of shrubs for preparation of traditional medicines. However, other findings [18, 23–25] indicated that herbs were the most frequently used plant categories.
3.3. Plant Parts Used to Treat Human Diseases
People of the study area harvest different plant parts for the preparation of traditional remedies (e.g., leaves, roots, seeds, barks, and fruit). In the study area, 43 species (44.8%) were harvested for their roots (Figure 3). This is because it is believed that roots contain more concentration of the active ingredients.
Figure 3.
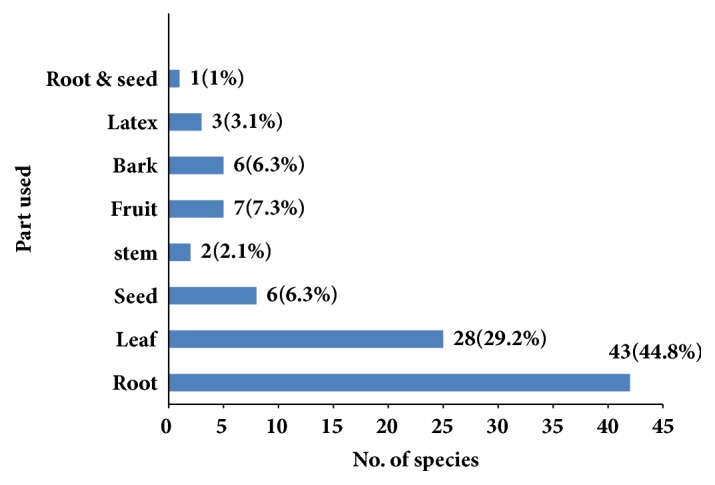
Plant parts used in human traditional medicine.
The finding of the roots as the contributor of higher number of plant species used for medicinal purpose than other plants parts is in line with similar study conducted by [17], in which roots (31.4%) were reported as the most widely used plant part followed by leaves 24.4%. The study conducted by [20] showed that roots 42% as a major plant parts used and [26] also documented root 35.8% as a major plant parts used in the treatment of human ailments. In this regard, [27] have indicated that plant harvest involving roots, rhizomes, bulb, bark, and stem has a serious effect on the survival of the mother plant in its habitat. However, the findings of [18, 21, 28–30] indicated that traditional medicinal preparations mainly involve the use of leaves. As leaves of medicinal plant species were also reported to be harvested for most remedy preparations next to roots, collection of leaves could be promoted as a more sustainable method since in most cases at least many leaves are left over on the parent plant [24].
3.4. Method of Preparation, Dosage, and Administration
In the collection of data concerning the preparation of medicine, participants reported various skills associated with herbal preparation. The results showed that the most remedies were prepared from a single plant or plant parts (73%) and preparation from combined plant species was 27%. Similarly, various research findings reported the use of single plant species or parts for traditional remedy preparation [22, 23, 31]. The potency of using a mixture of different plant or plant parts increased compared to using a single plant to cure a disease is evident.
The majority of the remedies (78.6%) in the study area were prepared from fresh parts of medicinal plants followed by dried form (15.7%) and (5.7%) prepared either from dry or fresh plant parts. The study conducted by [32] indicated that 86% of preparations were in fresh form and [33] reported that most of (64%) medicinal plants were used in fresh form and 36% in dried from. The dependency of local people on fresh materials is mostly due to the effectiveness of fresh medicinal plants in treatment as the contents are not lost before use compared to the dried forms.
The local communities employ various methods of preparation of traditional medicines for different types of diseases. The preparations vary based on the type and actual site of disease treated. The principal methods of remedy preparation were reported to be through crushing, which accounted for 30 preparations (38.5%) followed by pounding which accounted for 14 preparations (18.8%), powdering accounted for 10 preparations (14.6%), squeezing accounted for 7 preparations (10.4%), decoction accounted for 4 preparations (8.3%), crushing and pounding together accounted for three preparations (5.2%), and 4.2% of traditional medicines were prepared using concoction (Figure 4). Crushing as the most common mode of preparation is in agreement with the findings of [20, 34] who noted that the principal method of remedy preparation was through crushing. However, [27] in a similar study on people of Wonago District reported that powdering was a dominant method of preparation of remedy.
Figure 4.
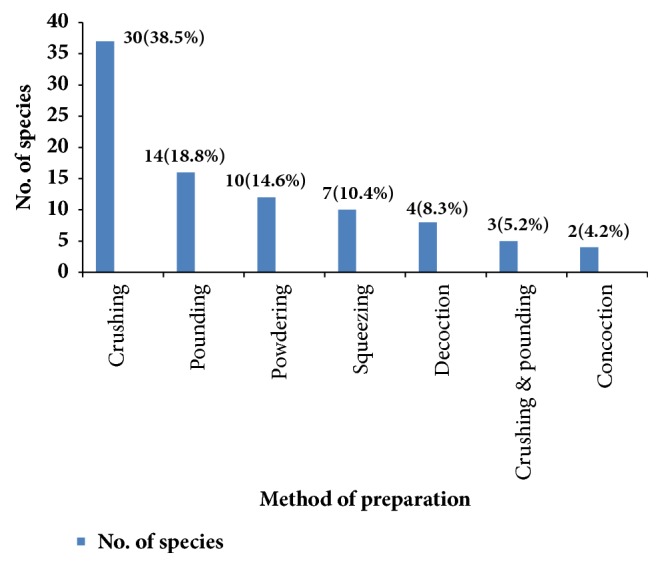
Mode of preparation of human medicinal plants in the study area.
Medicinal plants were applied through different routes of administration (Table 1). In the study area, the substantial proportions of prescriptions were administered orally (37.5%), followed by external application (13.5%), creaming (10.4%), and dry bath (8.3%). This result is in line with the findings of [29, 32, 35]. Internal ailments were commonly treated by making the patient drink herbal preparations; tooth infection was treated by crushing and applies on the remedial plant part on the tooth surface; skin infections such as ringworm were treated by creaming herbal preparations on an infected skin.
Concerning the dosage, local people of the study area used various units of measurement such as finger length (e.g., for root, bark, and stem), pinch (e.g., for powdered), and numbers (e.g., for leaves, seeds, fruits, and flowers) and locally made spoons from plants were used to estimate and fix the amount or dosage of medicine. For human disease treatment, the smallest number is one and the highest is 7 for the case of leaves. In the case of palm measurement units, the lowest is half palm and the highest is 3 palms depending on the age of the patients. The lack of precise dosage is one of the drawbacks of traditional medicinal plants [33, 36]. Tip part of the index figure is commonly used as a measurement of dose [37]. The result of [19] from Tehuledere district, South Wollo, showed that about 31% preparations were taken with known dosages mostly quantified by spoon, cup of tea, palm, and other equipment. The majority plant remedies (69%), however, are taken with no fixed dosage.
According to respondents, preparations were prescribed to patients differently for different age groups, sex, and other conditions. The dosage prescription for children was mostly lower than for adults. The amounts of remedy and prescription rates were generally dependent on the degree and duration of the ailment. Treatment durations varied between 1 and 7 days. This result is in line with the result of [29] in which treatment durations varied between 1 and 7 days.
Recovery from the disease, disappearance of the symptoms of the diseases, fading out of the disease sign, and judgment of the healer to stop the treatment were some of the criteria used in determining duration in the administration of the dosage. Most of the remedies were reported to have no serious adverse effects except vomiting and temporary inflammations. This could be attributed to the low toxicity of the remedy preparations of the medicinal plant species used by the traditional healers in the study area. A similar study by [36] indicated that some herbal preparations are considered harmless.
3.5. Knowledge on Medicinal Plants
Ethnomedicinal knowledge is concentrated in the elderly and relative members of the community and difficult in its transfer from the elders to the young generation. Most of the respondents (79%) preferred to transfer their indigenous knowledge to their family verbally and the remaining participants (21%) through showing the medicinal plants in the fields. Indigenous knowledge transfer to the young generation is considered poor which may cause erosion of the practice. The study revealed that medicinal plant knowledge transfer to the young generation is affected by modernization. This might be related to the diminishing of interest of the young generation on indigenous knowledge. Similar result was reported by [20] where young people showed disinterest on traditional medicinal plants.
3.6. Ranking of Medicinal Plants
Preference ranking of 5 medicinal plants that were reported as effective for treating stomachache was conducted after selecting ten key participants. Stomachache is the mostly occurring disease treated by more medicinal plants. The participants were asked to compare the given medicinal plants based on their efficacy. The results showed that Stephania abyssinica scored the highest mark and ranked first indicating that it was the most effective in treating stomachache and followed by Solanum incanum (Table 2).
Table 2.
Preference ranking of medicinal plants used for treating stomachache.
| Medicinal plants used | Respondents (A-J) | Total | Rank | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |||
| Solanum incanum | 5 | 4 | 5 | 5 | 4 | 5 | 4 | 4 | 5 | 5 | 46 | 2 |
| Stephania abyssinica | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 50 | 1 |
| Carissa spinarum | 4 | 3 | 4 | 5 | 4 | 3 | 2 | 3 | 5 | 4 | 37 | 4 |
| Calpurnia aurea | 5 | 5 | 3 | 3 | 5 | 4 | 5 | 5 | 4 | 3 | 42 | 3 |
| Croton macrostachyus | 4 | 3 | 2 | 3 | 5 | 4 | 3 | 4 | 3 | 5 | 36 | 5 |
For medicinal plants that were identified by the participants to be used in treating wounds, a paired comparison was made among six of them using ten participants to know their rank. Wound is frequently occurring external health problem in the study area. The results that were obtained from all the participants were summed up and compared plants were abbreviated in the table. Accordingly, Olea europaea subsp. cuspidata selected five times and stood first indicating that it is the most effective in treating wound followed by Prunus africana, Euphorbia heterophylla, Acacia senegal, Cyphostemma sp., and Clematis simensis (Table 3). The frequency of wound to be treated by more medicinal plants was also reported by [38] in other parts of Bale region. Nine medicinal plants were documented for wound treatment.
Table 3.
Paired comparison of medicinal plants used to treat wound (As: Acacia senegal, C. sp: Cyphostemma sp., Eh: Euphorbia heterophylla, Oe: Olea europaea subsp Cuspidata, and Pa: Prunus africana).
| Plant species | Acacia Senegal | Clematis simensis | Cyphostemma sp. | Euphorbia heterophylla | Olea europaea subsp Cuspidata | Prunus africana |
|---|---|---|---|---|---|---|
| Acacia Senegal | ||||||
| Clematis simensis | As | |||||
| Cyphostemma sp. | As | Csp | ||||
| Euphorbia heterophylla | Eh | Eh | Eh | |||
| Olea europaea subsp Cuspidata | Oe | Oe | Oe | Oe | ||
| Prunus africana | Pa | Pa | Pa | Pa | Oe | |
| Frequency | 2 | 0 | 1 | 3 | 5 | 4 |
| Rank | 4 | 6 | 5 | 3 | 1 | 2 |
In the study area, a number of medicinal plants were found to be multipurpose species being utilized for a variety of uses. Direct matrix ranking showed that of the total medicinal plants Croton macrostachyus is the most multipurpose use medicinal plant followed by Warburgia ugandensis (Table 5). The finding of [39] also reported Croton macrostachyus as the highest multipurpose use in Farta district South Gonder Zone of Amhara Regional State.
Table 5.
Direct matrix ranking of six plant species by four participants based on six use criteria.
| Use categories | Medicinal plants | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Warburgia ugandensis | Olea europaea subsp cuspidata | Acacia senegal | Prunus africana | Carissa spinarum | Croton macrostachyus | |||||||||||||||||||
| Participants (1-4) | Participants | Participants | Participants | Participants | Participants | |||||||||||||||||||
| 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | |
| Charcoal | 4 | 3 | 4 | 3 | 1 | 2 | 0 | 2 | 3 | 4 | 2 | 1 | 4 | 3 | 2 | 1 | 1 | 2 | 2 | 1 | 5 | 4 | 5 | 4 |
| Construction | 5 | 5 | 5 | 5 | 5 | 4 | 2 | 4 | 1 | 2 | 2 | 2 | 4 | 4 | 2 | 1 | 3 | 2 | 3 | 3 | 4 | 3 | 3 | 3 |
| Fence | 3 | 2 | 1 | 2 | 2 | 3 | 1 | 3 | 5 | 5 | 4 | 5 | 3 | 3 | 2 | 2 | 5 | 4 | 5 | 5 | 5 | 4 | 5 | 4 |
| Fire wood | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 4 | 5 | 5 | 5 | 5 | 4 | 4 | 4 | 5 | 5 | 5 | 5 | 5 | 4 | 5 |
| Furniture | 1 | 2 | 3 | 2 | 3 | 4 | 3 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 2 | 2 | 3 | 2 |
| Medicinal | 5 | 4 | 5 | 5 | 5 | 5 | 5 | 4 | 4 | 4 | 5 | 4 | 4 | 5 | 4 | 4 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Indi. Total | 23 | 21 | 25 | 22 | 21 | 23 | 16 | 20 | 20 | 21 | 20 | 18 | 22 | 21 | 15 | 12 | 19 | 19 | 20 | 20 | 26 | 23 | 25 | 23 |
| Grand total | 91 | 80 | 79 | 70 | 78 | 97 | ||||||||||||||||||
| Rank | 2 | 3 | 4 | 6 | 5 | 1 | ||||||||||||||||||
3.7. Informant Consensus Factor (ICF)
The diseases of the study area have been grouped into various categories based on the site of occurrence of the disease, condition of the disease, and treatment resemblance of the disease to the local people. The informant consensus factors have been calculated for each category (Table 4). The highest ICF (0.95) value was obtained for diseases related to gonorrhea and syphilis and the least one (0.69) was associated with boils, dandruff, eczema, haemorrhoids, scabies, Tinea versicolor, and wound.
Table 4.
Informant consensus factor by categories of diseases in the study area.
| Disease categories | No. of species | Use citation | ICF |
|---|---|---|---|
| Asthma, cough, earache, epitaks, headache, Tonsillitis and Toothache | 6 | 19 | 0.72 |
| Epilepsis, evil spirit, evil eye, doziness | 13 | 47 | 0.74 |
| Bat urine, bile problem, splenomegaly, flunk pain and urinary retention | 17 | 55 | 0.70 |
| Gonorrhea and syphilis | 3 | 39 | 0.95 |
| Amoebiasis, appetite loss, diarrhea, gastritis, intestinal worm, stomachache and vomiting | 8 | 37 | 0.80 |
| Emergency and fibril illness | 5 | 15 | 0.71 |
| Rabies and Snake bite | 2 | 11 | 0.9 |
| Boils, dandruff, eczema, hemorrhoids, scabies, taenia resicolors and wound | 11 | 33 | 0.69 |
3.8. Threat and Conservation of Medicinal Plants of Study Area
Medicinal plants are at increasing risk from destruction of their habitats (agricultural expansion, fire, construction, overgrazing, and urbanization) and over harvesting of known medicinal species [40]. According to [41] about 15,000 medicinal plant species may be threatened with extinction world widely due to habitat loss and over harvesting and it is estimated that the earth is losing one potential major drug every two years. In the study area, the people also rely on medicinal plants for various purposes such as charcoal, medicine, firewood, construction, and food. The major threat to medicinal plants in the study area was agricultural expansion which accounted for 55%, charcoal production (15%), and fire wood accounted for 18%. The result of [42] indicated that intense deforestation became the major threat to medicinal plants in Zay people. According to [20] deforestation (40%) and agricultural expansion (12.5%) were the major threat to medicinal plants of Sekoru district of Jimma zone. Overgrazing reported to be the major threat to medicinal plants in Gozamin Woreda of East Gojjam [43].
This indicates that due consideration should be given for conservation of these plants since they are being widely exploited for purposes other than their medicinal value. Availability of medicinal plants has been affected by a dramatic decrease in the area of native vegetation due to agricultural expansion, deforestation, fire, overgrazing, and charcoal and firewood [40, 42].
The influences of human on the natural habitat of medicinal plants are the problems for the conservation of medicinal plants and associated knowledge. The effort to conserve medicinal plants in the district was observed to be very poor. Some participants have started to conserve medicinal plants by cultivating at home gardens, though the effort was minimal. About 13.8% of the medicinal plants collected were reported as found cultivated at home gardens and these include plants like Carica papaya, Coffea arabica, and Jatropha curcas. The result of [32] indicated that only 5.7% of medicinal plants were cultivated in home garden showing minimal effort of medicinal plant conservation in Mena Angetu district.
Suggestion given by [44] stated that natural resources could be utilized best in sustainable way if management practices are complete. In fact, such valuable activities require appropriate action, and changes by the full range of societies and stakeholders involved in the conservation, production, and management as well as use of medicinal plants. Since an action on conservation and sustainable use of medicinal plants need involvement of various sectors and greater public support, it needs a continuous task of creating public awareness [45]. The review made by Megersa et al. [46] suggested that identifying serious threats to medicinal plants and how local people manage medicinal plants will help to understand the best conservation strategies.
4. Conclusions
A study on medicinal plant utilization in area revealed that the communities commonly use medicinal plants for maintaining their primary healthcare. The study resulted in documenting 70 medicinal plants species where Euphorbiaceae is the leading family with the highest proportion of medicinal plants. Most of (58) medicinal plants in the study area were harvested from wild. Shrubs were found to be the dominant growth form of medicinal plants used for preparation traditional remedies and followed by herbs. Roots were found to be the most frequently used plant parts for the preparation of traditional remedies. Traditional medicine preparation mostly involves a single plant and the method of preparation was mainly crushing followed by pounding. Depletion of indigenous knowledge among the people of the study area was serious due to disinterest of young generation to gain the knowledge. Oral based knowledge transfer, unavailability of the species, and influence of modern education were considered as the main factors. The main threat on medicinal plants in the study area arises from agricultural expansion. Utilization of root plant parts for traditional medicine preparation could also be considered as a threat. Although Berbere district was found to be rich in medicinal plant diversity, the effort to conserve the plants and associated indigenous knowledge was observed to be very poor. Thus, conservation of medicinal plants by local communities and responsible bodies is vital to avoid further loss. Moreover, phytochemical and pharmacological investigation is recommended with due consideration to frequently used medicinal plants.
Acknowledgments
The authors would like to acknowledge Jimma University for financial support. All members of National Herbarium of Addis Ababa University also deserve appreciation for their help rendered during the identification of plants. They are also grateful to the local people of Berbere district for their hospitality and kind response to the enquiries on information about the medicinal plants.
Data Availability
The data used in this study is available from the corresponding author upon request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.WHO. Traditional Medicine: Growing Needs and Potentials. 2002. [Google Scholar]
- 2.WHO. Traditional medicine. 2012, http://www.who.int/mediacentre/factsheets/fs134/en.
- 3.WHO. Traditional medicine. 2008, http://www.who.int/mediacentre/factsheets/fs34/en.
- 4.Sofowora A. Medicinal Plants and Traditional Medicine in Africa. New York, NY, USA: John Wiley & Sons; 1982. [DOI] [PubMed] [Google Scholar]
- 5.Park H. L., Lee H. S., Shin B. C., et al. Traditional medicine in China, Korea, and Japan: a brief introduction and comparison. Evidence-Based Complementary and Alternative Medicine. 2012;2012:9. doi: 10.1155/2012/429103.429103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. Consultation meeting on traditional medicine and modern medicine: harmonizing the two approaches. (WP)TM/ICP/TM/001/RB/98-RS/99/GE/32(CHN)), 1999.
- 7.Pankhurst R. An historical examination of traditional Ethiopian medicine and surgery. Ethiopian Medical Journal. 1965;3:157–172. [Google Scholar]
- 8.WHO. Legal Status of Traditional Medicine and Complementary/Alternative Medicine: A Worldwide Review. Geneva, Switzerland: WHO; 2001. [Google Scholar]
- 9.IBC. Addis Ababa, Ethiopia: IBC; 2012. Ethiopian third national report. http://www.fao.org/pgrfa-gpa-archive/eth/Reports/Third_Report.pdf. [Google Scholar]
- 10.PGRC. Country report to the FAO international technical conference on plant genetic resources. 1996
- 11.Kassaye K. D., Amberbir A., Getachew B., Mussema Y. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiopian Journal of Health Development. 2006;20(2):127–134. doi: 10.4314/ejhd.v20i2.10023. [DOI] [Google Scholar]
- 12.Martin G. J. Ethnobotany: A Method Manual. A “People and Plants” Conservation Manual. London, UK: Champman and Hall; 1995. [Google Scholar]
- 13.Alexiades M. Collecting ethnobotanical data. An introduction to basic concepts and techniques. In: Alexiades M., Sheldon J. W., editors. Selected Guideline for Ethnobotanical Research: A Field Manual. New York, NY, USA: Botanical Garden; 1996. pp. 58–94. [Google Scholar]
- 14.Cotton C. M. Ethnobotany, Principles and Applications. Chichister, UK: John Wiley & Sons; 1996. [Google Scholar]
- 15.Heinrich M., Ankli A., Frei B., Weimann C., Sticher O. Medicinal plants in Mexico: healers' consensus and cultural importance. Social Science & Medicine. 1998;47(11):1859–1871. doi: 10.1016/S0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 16.Lulekal E., Kelbessa E., Bekele T., Yineger H. An ethnobotanical study of medicinal plants in Mana Angetu District, southeastern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2008;4, article 10 doi: 10.1186/1746-4269-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunde D., Asfaw Z., Kelbessa E. Use of traditional medicinal plants by people of ‘Boosat’ Sub district, central eastern Ethiopia. Ethiopian Journal of Health Sciences. 2006;16(2):141–155. [Google Scholar]
- 18.Regassa R., Bekele T., Megersa M. Ethnobotanical study of traditional medicinal plants used to treat human ailments by Halaba people, southern Ethiopia. Journal of Medicinal Plants Studies. 2017;5(4):36–47. [Google Scholar]
- 19.Adefa M., Abraha B. Ethnobotanical survey of traditional medicinal plants in Tehuledere district, South Wollo, Ethiopia. Journal of Medicinal Plants Studies. 2011;5:6233–6242. [Google Scholar]
- 20.Yineger H., Yewhalaw D. Traditional medicinal plant knowledge and use by local healers in Sekoru District, Jimma Zone, Southwestern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2007;3, article 24 doi: 10.1186/1746-4269-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alemayehu G., Asfaw Z., Kelbessa E. Ethnobotanical study of medicinal plants used by local communities of Minjar-Shenkora district, North Shewa zone of Amhara region, Ethiopia. Journal of Medicinal Plants Studies. 2015;3(6):1–11. [Google Scholar]
- 22.Eshete M. A., Kelbessa E., Dalle G. Ethnobotanical study of medicinal plants in Guji Agro-pastoralists, Bule Hora district of Borana zone, Oromia region, Ethiopia. Journal of Medicinal Plants Studies. 2016;4(2):170–184. [Google Scholar]
- 23.Megersa M., Asfaw Z., Kelbessa E., Beyene A., Woldeab B. An ethnobotanical study of medicinal plants in Wayu Tuka District, East Welega Zone of Oromia Regional State, West Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;9, article 68 doi: 10.1186/1746-4269-9-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lulekal E., Asfaw Z., Kelbessa E., Van Damme P. Ethnomedicinal study of plants used for human ailments in Ankober District, North Shewa Zone, Amhara Region, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;9, article 63 doi: 10.1186/1746-4269-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luizza M. W., Young H., Kuroiwa C., et al. Local knowledge of plants and their uses among women in the Bale Mountains, Ethiopia. Ethnobotany Research and Applications. 2013;11:315–339. [Google Scholar]
- 26.Teklehaymanot T., Giday M. Ethnobotanical study of medicinal plants used by people in Zegie Peninsula, Northwestern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2007;3, article 12 doi: 10.1186/1746-4269-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mesfin F., Demissew S., Teklehaymanot T. An ethnobotanical study of medicinal plants in Wonago Woreda, SNNPR, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2009;5, article 28 doi: 10.1186/1746-4269-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abera B. Medicinal plants used in traditional medicine in Jimma Zone, Oromia Regional State southwest Ethiopia. Ethiopian Journal Health Sciences. 2003;13:85–94. [Google Scholar]
- 29.Bekalo T. H., Woodmatas S. D., Woldemariam Z. A. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta Special Woreda, southern nations, nationalities and peoples regional state, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2009;5, article 26 doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kitata G., Abdeta D., Amante M. Ethnoknowledge of plants used in veterinary practices in Midakegn district, west showa of Oromia region, Ethiopia. Journal of Medicinal Plants Studies. 2017;5(5):282–288. [Google Scholar]
- 31.Chekole G. Ethnobotanical study of medicinal plants used against human ailments in Gubalafto District, Northern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2017;13(1, article 55) doi: 10.1186/s13002-017-0182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdurhman N. Ethnobotanical study of medicinal plants used by local people in Ofla Wereda, Southern Zone of Tigray Regional State, Ethiopia [M.S thesis] Addis Ababa University; 2010. [Google Scholar]
- 33.Getahun A. Some Common Medicinal and Poisonous Plants Used in Ethiopian Folk Medicine. Addis Ababa, Ethiopia: Addis Ababa University; 1976. [Google Scholar]
- 34.Demie G., Negash M., Awas T. Ethnobotanical study of medicinal plants used by indigenous people in and around Dirre Sheikh Hussein heritage site of South-eastern Ethiopia. Journal of Ethnopharmacology. 2018;220:87–93. doi: 10.1016/j.jep.2018.03.033. [DOI] [PubMed] [Google Scholar]
- 35.Yineger H., Kelbessa E., Bekele T., Lulekal E. Plants used in traditional management of human ailments at Bale Mountains National Park, Southeastern Ethiopia. Journal of Medicinal Plants Research. 2008;2(6):132–153. [Google Scholar]
- 36.Yirga G. Ethnobotanical study of medicinal plants in and around Alamata, Southern Tigray, Northern Ethiopia. Current Research Journal of Biological Sciences. 2010;2:338–344. [Google Scholar]
- 37.Birhanu Z., Endale A., Shewamene Z. An ethnomedicinal investigation of plants used by traditional healers of Gondar town, North-Western Ethiopia. Journal of Medicinal Plants Studies. 2015;3(2):36–43. [Google Scholar]
- 38.Bussmann R. W., Swartzinsky P., Worede A., Evangelista P. Plant use in Odo-Bulu and Demaro, Bale region, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2011;7, article 28 doi: 10.1186/1746-4269-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ragunathan M., Abay S. M. The study of spiritual remedies in orthodox rural churches and traditional medicinal practice in Gondar Zuria district, Northwestern Ethiopia. Pharmacology Journal. 2009;1(3):178–183. [Google Scholar]
- 40.Cunningham A. B. Wild plant use and resource management. In: Bennun L. A., Aman R. A., Crafter S. A., editors. The Center for Biodiversity. Nairobi, Kenya: National Museums of Kenya; 1992. pp. 109–126. [Google Scholar]
- 41.Roberson E. Center for Biological Diversity; 2008. Medicinal plants at risk. A native plant conservation campaign report. http://www.scribd.com/doc/75492242/Medicinal-Plants-at—Risk. [Google Scholar]
- 42.Giday M., Asfaw Z., Elmqvist T., Woldu Z. An ethnobotanical study of medicinal plants used by the Zay people in Ethiopia. Journal of Ethnopharmacology. 2003;85(1):43–52. doi: 10.1016/s0378-8741(02)00359-8. [DOI] [PubMed] [Google Scholar]
- 43.Amsalu N., Bezie Y., Fentahun M., Alemayehu A., Amsalu G. Use and conservation of medicinal plants by indigenous people of Gozamin Wereda, East Gojjam Zone of Amhara region, Ethiopia: an ethnobotanical approach. Evidence-Based Complementary and Alternative Medicine. 2018;2018:23. doi: 10.1155/2018/2973513.2973513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yineger H., Yewhalaw D., Teketay D. Ethnomedicinal plant knowledge and practice of the Oromo ethnic group in southwestern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2008;4, article 11 doi: 10.1186/1746-4269-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schippmann U., Leaman D., Cunningham A. B. Impact of Cultivation and Gathering of Medicinal Plants on Biodiversity: Global Trends and Issues. Rome, Italy: FAO; 2002. [Google Scholar]
- 46.Woldeab B., Regassa R., Alemu T., Megersa M. Medicinal plants used for treatment of diarrhoeal related diseases in Ethiopia. Evidence-Based Complementary and Alternative Medicine. 2018;2018:20. doi: 10.1155/2018/4630371.4630371 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study is available from the corresponding author upon request.