Abstract
Background
Despite increased ethnic diversity in more economically developed countries it’s unclear whether residential concentration of ethnic minority people (ethnic density) is detrimental or protective for mental health. This is the first systematic review and meta-analysis covering the international literature, assessing ethnic density associations with mental health outcomes.
Methods
We systematically searched Medline, PsychInfo, Sociological Abstracts, Web of Science from inception to March 31st, 2016. We obtained additional data from study authors. We conducted random effects meta-analysis taking into account clustering of estimates within datasets. Meta-regression assessed heterogeneity in studies due to ethnicity, country, generation and area-level deprivation. Our main exposure was ethnic density, defined as the residential concentration of own racial/ethnic minority group. Outcomes included depression, anxiety and the common mental disorders (CMD), suicide, suicidality, psychotic experiences and psychosis.
Results
We included 41 studies in the review, with meta-analysis of 12 studies. In the meta-analyses, we found a large reduction in relative odds of psychotic experiences (OR:0.82(95% CI:0.76-0.89) and suicidal ideation (OR:0.88(95% CI:0.79-0.98) for each 10 percentage-point increase in own ethnic density. For CMD, depression and anxiety, associations were indicative of protective effects of own ethnic density however results were not statistically significant. Findings from narrative review were consistent with those of the meta-analysis.
Conclusions
The findings support consistent protective ethnic density associations across countries and racial/ethnic minority populations as well as mental health outcomes. This may suggest the importance of the social environment in patterning detrimental mental health outcomes in marginalized and excluded population groups.
Keywords: Bolded references refer to estimates included in meta-analyses, Green-colored text indicates protective ethnic density effects, Red-colored text indicates detrimental ethnic density effects
Introduction
Mental health disorders account for 8.6 million years of life lost to premature mortality, and are the leading cause of years lived with disability worldwide (Whiteford et al., 2013), ranking second only to cardiovascular disease in their impact on disability in high income countries (Murray and Lopez, 1996). There is some heterogeneity in the incidence and prevalence of mental disorders across racial/ethnic populations, and longstanding controversies in the etiological origins of these differences. Whereas a body of research has focused on the intrinsic biologic variations among human subpopulations (Kaufman and Cooper, 2001), a parallel line of research has examined the social determinants of mental health and has indicated that social factors rooted in the experience of belonging to a racial/ethnic minority, marginalized group, has a significant effect on adverse mental health outcomes (Pickett and Wilkinson, 2008).
A burgeoning body of research suggests that for racial/ethnic minority populations, there might be benefits to living in neighborhoods with a greater concentration of other racial/ethnic minority residents, a so-called ethnic density effect (Bécares et al., 2012b, Shaw et al., 2012). Studies suggest that ethnic density - the residential concentration of racial/ethnic minorities in a neighborhood - protects racial/ethnic minorities from the stress of racial discrimination, low status stigma, and socioeconomic disadvantage, while encouraging stronger social support and community cohesion. Understanding the contribution of ethnic density effects for mental health is important because it highlights the role of the environment, including racialization and exclusion, in maintaining and perpetuating the increased risk of mental health disorders among racial/ethnic minority populations.
However, this body of work is contentious, as protective effects are offset by the detrimental effects of concentrated poverty and disinvestment in areas with larger concentrations of racial/ethnic minority people. Previous research has been unable to disentangle the competing effects for mental health of ethnic density and area deprivation, and there are challenges in attempting to draw conclusions from diverse, international settings with distinct historical patterns of settlement and diversity. A previous narrative review was not able to quantify the magnitude of differences for mental health by ethnic density (Shaw and Pickett, 2011), and sources of potential heterogeneity have hitherto remain unexplored, although understanding these may lead to important clues around underlying mechanisms for mental disorder. These issues are particularly salient given the current scale of global migration (United Nations, 2016) and policies around the forced dispersal of migrant populations to areas without previous histories of migrant settlement.
To address these controversies, we conducted a systematic review with meta-analysis and meta-regression of observational studies of mental disorders where ethnic density effects have been examined. The aim of the review and meta-analysis was to establish: 1) if ethnic density associations are evident, whether they are consistent across mental health outcomes including depression, anxiety and the common mental disorders, suicide, suicidality, psychotic experiences and psychosis; 2) the nature and magnitude of ethnic density effects on mental disorders across and within countries, racial/ethnic groups, generational status and by area-level deprivation.
Methods
Search Strategy
Search strategies were based on and updated from a narrative review of ethnic density and mental health (Shaw and Pickett, 2011) that searched the following databases: Medline, Psychinfo, Sociological Abstracts, and the Social Science Citation and Science citations from the Web of Science. We performed searches to March 2016. All reference lists for retrieved papers with potential studies for inclusion were hand-searched and first and/ or last authors of all papers were contacted for further additional and unpublished data.
Eligibility
We excluded ecological studies, and studies that did not focus on adult (aged 16+) populations. We included all cross-sectional survey, case-control, or cohort-design studies that used representative population data, in order to minimize biases from differences in help-seeking from using patient/service-level data. In order to further minimize ascertainment bias due to differences in health-seeking behavior we restricted to studies which used community samples. As schizophreniform/psychotic disorders are rare and not usually detected in community samples for these disorders we also included first contact studies which utilized leakage studies to identify all cases of schizophreniform disorders/psychosis, or alternatively studies which employed databases of whole populations with linkage. We also included studies of suicide which employed death certificate information, since there is no other way to ascertain this outcome from community survey-level data.
Main outcomes and measures
Ethnic density was measured as 10% increase in the residential concentration of own racial/ ethnic group, for the purposes of meta-analysis. Studies had to have a measure of ethnic density and had to specify the geographical area of measurement, which had to be at the level of neighborhoods. Studies could be in a journal or book, but we also included doctoral dissertations and unpublished estimates obtained from contacting authors. Outcomes were depression, anxiety, suicidality and suicide, psychotic experiences, and schizophreniform/ psychotic disorders. For some studies it was not possible to examine depression and anxiety separately, in these instances we opted to analyze the outcome of common mental disorders (anxiety or depression).
Search and Extraction
Searches were conducted by two of the authors (JD and LB). Retrieved studies were compared with inclusion/exclusion criteria. Uncertainties around whether to include studies were settled by discussions between the authors. For each of the studies which met criteria for inclusion, relevant fields including medical outcomes, were extracted and cross-checked between two of the investigators (JD and LB). Where possible, we extracted estimates for the association of own ethnic density and mental health outcome, adjusted for age, sex, individual-level and area-level deprivation. For studies where data on ethnic density measured as a ten percentage point increase in the residential concentration of own ethnic group was not available, study authors were contacted for additional estimates, and in some cases, for unpublished estimates. We considered multiple publications using the same dataset as one set of analyses. There were no restrictions on language of manuscript. We were aware of two other studies for which we were co-investigators, but we could not include the data due to the publications being embargoed at the time of analysis.
Assessment of Methodological Quality
A small pilot study was conducted to assess the reliability of a scale devised to assess the quality of retrieved studies (based on quality assessment scales of observational studies (Khan et al., 2001)). LB and JD independently assessed the quality of a random sample of 20 papers using this scale, blind to each other’s quality ratings (see Supplementary Table 1 for criteria in quality assessment tool). Kappa for inter-rater reliability of the scale was 67%. Efforts to avoid publication biases were taken by contacting all first authors and experts in the field for unpublished data. Funnel plots were derived to formally assess this (see Supplementary Figure 1). We registered the review protocol with PROSPERO (registration number: CRD42014012992).
Statistical Analysis
We conducted meta-analysis followed by meta-regression to examine the association between own ethnic density and the following mental health outcomes: depression, anxiety and the common mental disorders, suicide, suicidality, psychotic experiences and psychosis. We obtained raw data from some of the studies (Bécares, 2014, Bécares and Das-Munshi, 2013, Bécares et al., 2014, Bécares et al., 2012a, Bécares et al., 2009, Das-Munshi et al., 2012, Das-Munshi et al., 2010) which permitted us to obtain estimates adjusted for a priori confounders, including age and gender, and area-level deprivation, or if area-level deprivation was not available, adjusted only for age and gender. These were combined with estimates extracted from publications or provided by authors of publications, also adjusted for the same confounders. We then used meta-regression to assess the effect of moderators, which included: race/ethnicity, country of study, generational status. We assessed the moderating effect of area-level deprivation using datasets which had estimates adjusted for age and sex. Meta-regression models were run with fixed-effects for moderators, and random effects for study. Studies which used symptom scales for depression were converted into mean differences and their standard errors using the method outlined by Chinn (Chinn, 2000). In each of our models we derived an I2-like statistic for each level of random variability. To assess for bias introduced through small study effects we used funnel plots. Meta-analysis and meta-regression were conducted in R (Team, 2015), version 3.2.2, using the package metafor, version 1.9-8 (Viechtbauer, 2010). To supplement findings from the meta-analysis and meta-regression we also conducted narrative review synthesis to all papers, which relied on vote-counting of studies (Popay et al., 2006), based on statistical significance of results.
Results
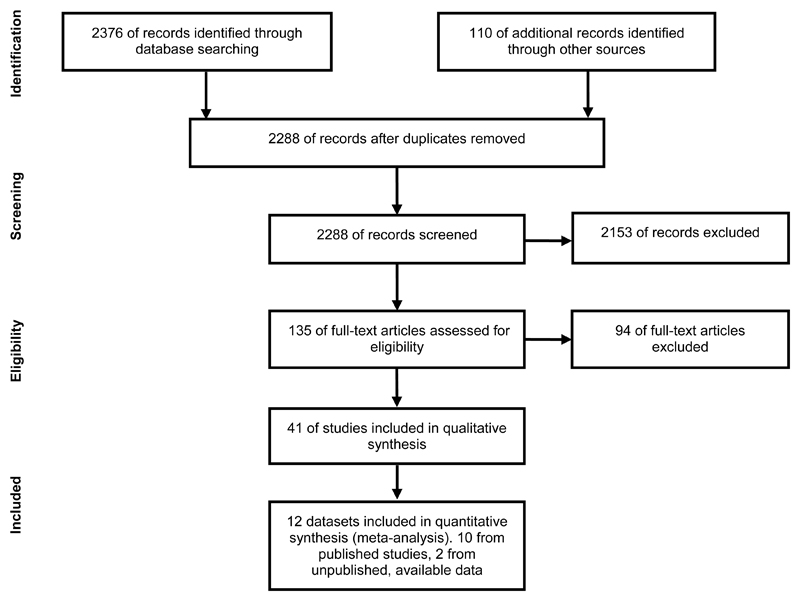
Our search retrieved 2288 articles, 135 were assessed for eligibility, and 41 studies were included in the synthesis. Of these we were only able to include 12 studies in meta-analysis because, despite our efforts, most authors either did not respond to our requests, were unable to provide data in suitable format for meta-analysis, or no longer had access to the data (Figure 1). In total, there were 29 studies assessing common mental disorders, depression and anxiety (Table 1), 12 studies assessing ethnic density associations for psychotic experiences and psychosis and 4 studies assessing suicidality and completed suicide. Table 1 is ordered according to outcome and quality of studies; asterisked studies in the table provided estimates for meta-analysis. All of the studies that were included in the meta-analysis were of a moderate to high quality rating. No studies were excluded based on quality. We also obtained two other datasets from the UK, publicly available under end user-license agreements, which had not been published as part of any study but which we included in meta-analysis and meta-regression. For the meta-analysis and meta-regressions we focus on datasets and not on studies, reflecting the fact that several studies may have used the same data sources, to avoid duplication. Visual assessment of funnel plots did not indicate publication biases (see Supplementary Figure 1).
Figure 1. PRISMA flow chart of studies.
Table 1. Studies investigating ethnic density effects with mental health outcomes. Studies ranked according to quality assessment by outcome.
| Reference | Dataset, country | Sample | Instrument | Area Unit | Ethnic density measure | Covariates | Method | Results [threshold/nonlinearity] | QA score |
|---|---|---|---|---|---|---|---|---|---|
| DEPRESSION | |||||||||
| *Arévalo et al, 2015(Arévalo et al., 2015) | Boston Puerto Rican Health Study (USA) | 1142 Puerto Ricans from initial sample of 1504 (76%) with complete baseline and follow up assessment. Aged 45-75. | Center for Epidemiologic Studies-Depression (CES-D). | census tract | Percentage Puerto Ricans | Gender, age, education, depressive symptoms at baseline (for follow up assessment), Neighbourhood poverty level, pre-migration urbanicity, reasons for migration, length of stay, acculturation, discrimination, recreational/ friend/ neighbour/ family/ church activities |
Multilevel multivariate linear regression | At 2 year follow up, after adjusting for all covariates and baseline CES-D, men living in high vs. low ethnic density neighbourhoods had lower CES-D scores but not women | 14 |
| Booth, 2014(Booth, 2014) | Chicago Community Adult Health Survey (CCAHS) 2001-2003 (USA) | 802 Latino people; 64% Mexican American, 17% Puerto Rican, 19% other Hispanic/Latino | Center for Epidemiologic Studies-Depression (CES-D) | 343 neighbourhood ‘clusters’ consisting of one or more contiguous census tracts, from 865 aggregated census tracts | Percentage of Hispanic people, continuous according to 2000 US census | Gender, age, education Neighbourhood-level disadvantage, generational status |
Multilevel regression models | Protective association of increasing own Hispanic density in crude models and models adjusting for individual and area-level covariates excluding generational status and acculturation. | 14 |
| Alegria et al., 2014(Alegria et al., 2014) | 2001-2003 Collaborative Psychiatric Epidemiology Surveys (CPES)- these included National Comorbidity Survey Replication (NCS-R), the National Survey of American Life (NSAL), the National Latino and Asian American Study (NLAAS) (USA) | 4180 Non-Latino white, 2554 Latino, 2095 Asian, 3570 African American and 1438 African Caribbean residents | World Health Organization World Mental Health Composite International Diagnostic Interview (WHO WMH-CIDI) | Census tracts | Percentage Latino and foreign-born population – interacted with race/ethnicity | Individual-race/ethnicity, age, gender, marital status, education, poverty status, work status, and nativity. Neighbourhood-Disadvantage, Latino/immigrant concentration, affluence, and residential instability |
Multi-level logistic regression models | In an interaction between individual-level ethnicity (Latino vs. non-Latino White), there wasn’t a statistically significant association between increased Latino/immigrant ethnic density and depressive disorders. | 14 |
| *Bécares et al., 2014(Bécares et al., 2014) | NSAL; (USA) | 3570 African Americans | Center for Epidemiologic Studies-Depression (CES-D). | Census tract | Percentage black residents | Age, gender, marital status, household income, education, employment Area deprivation score composed of 4 indicators |
Multi-level logistic regression models |
Increased black ethnic density up to 85% associated with decreased depressive symptoms. Increased black ethnic density from 85% onwards associated with increased depressive symptoms. |
14 |
| Mair et al., 2010(Mair et al., 2010) | Multi-Ethnic Study of Atherosclerosis (MESA); (USA) | 837 African American women, 669 African American men, 608 Hispanic women, 571 Hispanic men, 339 Chinese women, 321 Chinese men |
Center for Epidemiologic Studies-Depression (CES-D) | Census tract | Percent non-Hispanic African American, Hispanic, non-Hispanic white, and non-Hispanic Asian. | Age, income, marital status, education and nativity. Analyses stratified by gender. Neighbourhood social cohesion, safety, problems, aesthetic quality and socioeconomic factors. |
Multilevel regression models. |
Living in a neighbourhood with a higher ethnic density was associated with increased CES-D scores in African American men. When adjusted for area deprivation, Hispanic ethnic density was association with decreased CES-D scores among Hispanic men. No association between ethnic density and depression for the other racial/ethnic and gender categories. |
13 |
| Wight et al., 2009(Wight et al., 2009) | Study of Assets and Health Dynamics Among the Oldest Old (AHEAD); (USA) | 3442 older adults at Time 1 (17% African American, 6% Hispanic), 2632 at Time 2 (16% African American, 6% Hispanic), 1871 at Time 3 (16% African American, 6% Hispanic) |
8-item Center for Epidemiologic Studies-Depression (CES-D). | Census tracts | Proportion of African American residents; proportion of Hispanic residents. Numerator is proportion of residents who are over the age of 65 years. |
Educational attainment, household income, household wealth, gender, age, ethnicity, marital status, religion, assistance with activities of daily living (ADL), heart problems, stroke, a count of other major medical conditions, and cognitive function. Neighbourhood-level SES factor based on proportion of residents aged 25+ without a high school degree, households receiving public assistance income, residents living below the poverty level, and unemployed residents aged 16+. Affluence indicator based on proportion of households with incomes of $50,000 or more. |
Multilevel regression models. | There was a trend for a protective, but not statistically significant association between Hispanic ethnic density and a reduction in depressive symptoms from Time 1 to Time 2, and from Time 2 to Time 3. There were no statistically significant associations for African American ethnic density, although the direction of the effect was detrimental from Time 1 to Time 2, and protective from Time 2 to Time 3. |
13 |
| Shell et al., 2013(Shell et al., 2013) | Texas City Stress and Health Study; (USA) | 1238 U.S.-born and Mexican-born Hispanics of Mexican descent | Center for Epidemiologic Studies Depression Revised scale (CES-DR) | 48 neighbourhoods, with boundaries defined using street patterns, residential patterns | Percentage of Hispanic people in the neighbourhood based on US Census 2000 data, in 6 groups: ≥ 16% > 16% - ≤ 20% > 20 - ≤ 25% > 25 - ≤ 35% > 35 - ≤ 45% >45% |
Gender, age, education, income, marital status, language spoken, life events, physical health, social support, discrimination, stress Residential stability, median house value |
Multilevel regression models. |
Living in the highest category of Hispanic ethnic density is associated with a reduction in depressive symptoms in models that adjust for individual-level demographic covariates and area level covariates. This association loses statistical significance after adjusting for social support. |
12.5 |
| *Ostir el al., 2003(Ostir et al., 2003) | Hispanic established population for the epidemiologic study of the elderly (HEPSE); (USA) | 2710 Mexican Americans aged 65 years or older | Center for Epidemiologic Studies-Depression (CES-D). Subjects with a score of 16 or more were classified as having high depressive symptomatology | Census tracts | Percentage Mexican American | Age, gender, marital status, highest grade of schooling completed, per capita household income, nativity, chronic disease and activities of daily living (ADL) limitations. Neighbourhood socioeconomic status |
Multilevel regression models. | There was a non-significant association between Mexican ethnic density and depression in models adjusted for age and sex only. After adjusting for individual-level covariates and for area deprivation, a 10% increase in percentage Mexican American was associated with reduced CES-D scores. |
12 |
| Wight et al., 2011(Wight et al., 2011) | Health and Retirement Study (HRS); (USA) | 4805 adults aged 52 to 63. 77% white, 13.18% African American, 7.37% Hispanic, 2.45% Other | Center for Epidemiologic Studies-Depression (CES-D) | Census tracts | Percentage of African American residents, and percentage of Hispanic residents | Education, household wealth, household income, religion, gender, age, ethnicity, marital status, activities of daily living, medical conditions. Socioeconomic disadvantage factor, neighbourhood affluence. |
Multilevel regression models. | No associations were found between ethnic density and depression. | 11.5 |
| English,et al., 2014(English et al., 2014) | Healthy Aging in Neighborhoods of Diversity across the Life Span study (HANDLS); (USA) | 2197 African American and 1523 white American adults aged 30-64 years | Center for Epidemiologic Studies-Depression (CES-D). | Census tract | Proportion African American and white American residents | Age, gender, poverty status (family income) | Structural Equation Modelling (SEM) | No association was found between African American ethnic density and depression, after adjusting for covariates | 11 |
| Kwag et al., 2011(Kwag et al., 2011) | Own data; (USA) | 567 Korean American adults aged 60+ | Geriatric Depression Scale-Short Form (GDS-SF) | Census block group | Proportion of racial/ ethnic minorities-comprising ‘Hispanic, non-Hispanic white, non-Hispanic black, Asian, native Hawaiian and Pacific islander, American Indian, Alaskan native and non-Hispanic multi-race’ | Age, gender, marital status, education, length of stay (US), chronic conditions, functional disability, health perceptions. Area-level proportion people living below poverty-line, proportion people>65 years, proportion ethnic minorities |
Multilevel multivariate linear regression | No association between proportion racial/ ethnic minorities and mean depression after adjusting for covariates | 11 |
| Yuan et al., 2008(Vogt Yuan, 2007) | 1995 Community, Crime, and Health Survey Illinois; (USA) | 2292 black and Hispanic respondents | Center for Epidemiologic Studies-Depression (CES-D). | Census tract | Percentage black and percentage Hispanic (logged) | Age, gender, education, household income, employment status, number of children, and marital status. Neighbourhood-level: % households below federal poverty threshold & %female headed households with children | Multilevel multiple linear regression models | Black Americans living in areas of higher own group density had lower mean depression in models adjusted for neighbourhood disadvantage | 11 |
| Aneshensel et al., 2007(Aneshensel et al., 2007) | AHEAD; (USA) | 3442 older adults (10% African American, 4% Hispanic) | 8-item Center for Epidemiologic Studies-Depression (CES-D). | Census tracts | Proportion of African American residents; proportion of Hispanic residents. | Gender, age, marital status, educational attainment, household wealth, household income, religion, assistance with activities of daily living, number of medical conditions, heart problems, stroke, cognition. Neighbourhood-level SES factor based on proportion of residents aged 25+ without a high school degree, households receiving public assistance income, residents living below the poverty level, and unemployed residents aged 16+. Affluence indicator based on proportion of households with incomes of $50,000 or more. |
Multilevel regression models. Tested census-tract variables for non-linear associations, especially threshold effects, but found no significant departures from linearity. |
No associations between ethnic density and depressive symptoms | 11 |
| Stafford et al., 2011(Stafford et al., 2011) | 2000–2001 Canadian Community Health Survey (CCHS); (Canada) | 108064 participants | Composite Diagnostic Interview Schedule Short Form for major depression | Health Region | Percentage immigrant population | Immigrant status, length of residence, visible minority status, gender, age, marital status, tenure, education | Multilevel regression models. | An increase in immigrant ethnic density was associated with lower likelihood of depression among immigrants and visible minority participants | 9 |
| ANXIETY | |||||||||
| Alegria et al., 2014(Alegria et al., 2014) | 2001-2003 CPES, NCS-R, NSAL, NLAAS; (USA) | 4180 Non-Latino white, 2554 Latino, 2095 Asian, 3570 African American and 1438 African Caribbean residents | World Health Organization World Mental Health Composite International Diagnostic Interview (WHO WMH-CIDI) | Census tracts | Percentage Latino and foreign-born population – interacted with race/ethnicity | Individual-race/ethnicity, age, gender, marital status, education, poverty status, work status, and nativity. Neighbourhood-Disadvantage, Latino/immigrant concentration, affluence, and residential instability |
Multi-level logistic regression models | In the interaction model of Latino vs non-Latino White, there was an adverse association between increased Latino/immigrant ethnic density and any-past year anxiety disorders, compared to non-Latino Whites. | 14 |
| Menezes et al., 2011(Menezes et al., 2011) | 2002 CCHS; (Canada) | 35708 individuals of which 21.8% immigrant and 78.2% non-immigrant | World Health Organization World Mental Health Composite International Diagnostic Interview (WHO WMH-CIDI) | Dissemination Area (DA) | Percentage immigrants | Age, gender, income, marital status, education. Mean income, % moving in the past 5 years, % rental & % below low income cut-off thresholds | Multilevel multivariate logistic regression models | Immigrants in the sample had reduced relative odds of mood and anxiety disorders with increasing immigrant density. | 12 |
| COMMON MENTAL DISORDERS | |||||||||
| *Das-Munshi et al., 2010(Das-Munshi et al., 2010) *Bécares and Das-Munshi, 2013(Bécares and Das-Munshi, 2013) |
Ethnic Minorities Psychiatric Illness Rates In the Community (EMPIRIC); (UK) | 837 white British, 733 Irish, 694 black Caribbean people, 650 Bangladeshi, 643 Indian and 724 Pakistani people | Clinical Interview Schedule-Revised (CIS-R) |
Middle super output level | Percentage people of same ethnic group | Age, gender, social class, education, marital status, area-level deprivation | Multilevel multivariate logistic regression |
Protective associations for common mental disorders in Irish and Bangladeshi people. No associations were found for other ethnic groups. |
15 |
| *Bécares 2014(Bécares, 2014) | NLAAS; (USA) | 577 Cubans, 495 Puerto Ricans, 868 Mexican Americans | 6-item Kessler Psychological Distress scale (K6) |
US County | Percentage Cuban residents, percentage Puerto Rican residents, percentage Mexican American residents, percentage Latin American immigrant residents, percentage Latino residents | Age, gender, household income, education, work status, marital status, language of interview, nativity. Area deprivation score composed of 3 indicators | Structural equation models accounting for clustering | Increased Cuban ethnic density was not associated with psychological distress for Cuban respondents. Increased Puerto Rican ethnic density was not associated with psychological distress for Puerto Rican respondents, but increased immigrant and Latino ethnic density were associated with decreased psychological distress for Puerto Rican respondents. These associations were stronger for the second generation. Increased Mexican American ethnic density was not associated with psychological distress among Mexican American participants. Among the first generation, an increase in own, immigrant and overall Latino ethnic density was associated with increased psychological distress. |
15 |
| Alegria et al., 2014(Alegria et al., 2014) | 2001-2003 CPES, NCS-R, NSAL, NLAAS; (USA) | 4180 Non-Latino white, 2554 Latino, 2095 Asian, 3570 African American and 1438 African Caribbean residents | World Health Organization World Mental Health Composite International Diagnostic Interview (WHO WMH-CIDI) | Census tracts | Percentage Latino and foreign-born population | Individual-race/ethnicity, age, gender, marital status, education, poverty status, work status, and nativity. Neighbourhood-Disadvantage, Latino/immigrant concentration, affluence, and residential instability |
Multi-level logistic regression models | Latinos residing in neighbourhoods with higher Latino/immigrant ethnic density had increased risk of any past year common mental disorder, compared to non-Latino whites. | 14 |
| *Bécares et al., 2013(Bécares et al., 2013) | New Zealand Health Survey (NZHS); (New Zealand) | 3160 Maori people | Doctor-diagnosed common mental disorders and 10-item Kessler Psychological Distress scale (K10) |
Census Area Units | Percentage Maori residents | Age, gender, education, household income and work status, area-level deprivation | Multilevel multivariate logistic and linear regression |
Increasing ethnic density was associated with a reduction in reporting doctor-diagnosed common mental disorders Ethnic density not associated with non-specific psychological distress (K10) |
13 |
| Choi et al., 2016(Choi et al., 2016) | 2004–2007 Medical Expenditure Panel Survey linked to county-level data from the Area Health Resources Files; (USA) | 29011 individuals categorised into U.S.-born individuals (n = 24225); earlier immigrants (≥15 years in the U.S.; n = 3866); and recent immigrants (<15 years in the U.S.; n = 920) |
6-item Kessler Scale (K-6) and the Patient Health Questionnaire (PHQ-2) |
County | Percentage of foreign-born individuals in the county (continuous variable) |
Age, gender, education, income, race/ethnicity, marital status, limiting illnesses. % foreign born in county; % uninsured in county; % unemployed in county; population density per square mile; % in poverty in county; % families with female head in county |
Multilevel linear regression with interactions between immigrant status and the percentage of foreign-born individuals in the county |
Increased foreign-born density associated with worse mental health among earlier immigrants when mental health was measured with the K6. When mental health was measured with the PHQ-2, increased foreign-born density was associated with worse mental health for recent and earlier immigrants. |
12 |
| *Schrier et al., 2014(Schrier et al., 2014) | G4 Monitor 2008; (Netherlands) | 1206 Surinamese-Dutch, 978 Turkish-Dutch and 784 Moroccan-Dutch citizens |
10-item Kessler Psychological Distress scale (K10) |
356 neighbourhoods. Mean population size of 5,853 inhabitants, ranging from 30 to 26,960. | Percentage native Dutch, Percentage Surinamese-Dutch, Percentage Turkish-Dutch Percentage Moroccan-Dutch |
Length of stay in the Netherlands, marital status, highest educational qualification, financial situation. Percentage of households in with an income under the national minimum poverty threshold, average house value in the neighbourhood | Multilevel regression models | Ethnic density was not associated with non-specific psychological distress in any of the three ethnic minority groups. | 12 |
| *Jarrin et al., 2013(Jarrin et al., 2013) | Own data; (Spain) | 568 Ecuadorians living in Spain, aged 18 to 55 | General Health Questionnaire (GHQ-28), dichotomised at 5+ | 17 city neighbourhoods and 16 municipalities (largely rural) within 4 regions in Spain (Alicante, Almeria, Madrid, Murcia) | Proportion of people with Ecuadorian nationality among all subjects recorded in the municipal council registry within the 33 areas. Ethnic density ranged from 0.9 to 19.5 % with a median of 4.7 % and a mean of 6.1 %. Categorised as: Low >5.9% High 6%+ | Gender, age, civil status, number of children, education, social support, social network diversity, emotional support, financial strain, income, employment, time since migration, discrimination. Proportion of people with less than primary education | Multilevel regression models. | In unadjusted models, residence in areas of high ethnic density was associated with increased odds of common mental disorders. No association between ethnic density and common mental disorders in fully adjusted models. |
11 |
| Syed & Juan, 2012(Syed and Juan, 2012) | NLAAS; (USA) | Vietnamese Americans (n=478), Chinese Americans (n=566), Filipino Americans (n=493) | 10-item Kessler Psychological Distress scale (K10) |
US county | Percentage Vietnamese, percentage Chinese, percentage Filipino, percentage any Asian American, percentage non-White. | Age, gender, nativity, English fluency, schooling, racial discrimination, social cohesion | Multilevel regression models | Vietnamese, Chinese and Filipino ethnic densities were not associated with psychological distress. | 11 |
| Leu et al., 2011(Leu et al., 2011) | NLAAS; (USA) | 1583 respondents including Vietnamese, Chinese, Filipino and ‘other Asian’ people | World Health Organization World Mental Health Composite International Diagnostic Interview (WHO WMH-CIDI); 12 month prevalence common mental disorders |
Census tract | Number of Asians divided by total population in census tract | Education, household income, subjective social status, employment, family size, marital status, age, ethnicity, citizenship, language, time in US, ethnic identification | Multivariate logistic regression |
Protective association for common mental disorders of Asian ethnic density in men only. | 11 |
| Propper et al., 2005(Propper et al., 2005) | 10 waves of the British Household Panel Survey (BHPS) (1991–2000); (UK) | 8184 individuals | General Health Questionnaire (GHQ-12) | Bespoke neighbourhoods, composed of approximately the nearest 500 – 800 people to the respondent’s home address | Percent Indian, percent black, percent Pakistani or Bangladeshi | Age, gender,ethnicity, and education, household income, number of adults, number of children, tenure, employment status of the head of household. Composite index of area characteristics | Multilevel regression models. Ethnic density analyses examined with interaction between individual and area-level ethnicity. | There was a significant interaction for ethnicity of area and ethnicity of the individual. Non-white participants in more ethnically mixed areas experience less negative mental ill health trajectories than whites. | 10.5 |
| *Halpern & Nazroo, 2000 (Halpern and Nazroo, 2000) | Fourth National Survey of ethnic minorities (FNS); (UK) | 2867 white British, 1205 black Caribbean, 1273 Indian, 728 African Asian, 1185 Pakistani, 591 Bangladeshi, 214 Chinese people | Clinical Interview Schedule-Revised (CIS-R) |
Ward | Percentage people of same ethnic group | Age, gender, hardship, language, age at migration | Multivariate linear regression (re-analysed using robust standard errors for meta-analysis) |
Ethnic minorities had a lower mean score on CIS-R in areas of higher ethnic density Indian and Caribbean people had lower mean scores on CIS-R in areas of higher ethnic density |
10 |
| *Feng et al., 2013(Feng et al., 2013) | 45 and up study; (Australia) | 226487 adults from 19 ethnic groups | 10-item Kessler Psychological Distress scale (K10) | Census collection districts | Percentage of people of same ethnic group | Age and gender | Multilevel multivariate logistic regression | Protective associations for common mental disorders with increasing ethnic density for Australians not born in Australia, English born in the UK, Scottish born in Australia, Irish born in Australia and Chinese born in Australia. | 9 |
| Ecob & Williams, 1991(Ecob and Williams, 1991) | Self-collected data in Glasgow from 1986 to 1987; (UK) | 173 Asians aged 30 – 40 years old | General Health Questionnaire (GHQ-12), dichotomised at 4+ | Postcode sectors | Proportion of Asian born. Three categories, high (>6%), medium (3 <6%), and low (<3%) | Age, gender, religion, household size, car ownership, house needing repair, number of household durables | Single-level regressions | Protective effect of ethnic density found for mental health (GHQ) and feeling sad or low. | 7 |
| PSYCHOSIS AND SCHIZOPHRENIA | |||||||||
| Mezuk et al 2015 | Swedish population based registries; (Sweden) | 1442931 adults age 15 to 60 years followed from 2005-2010. | Incident cases of non-affective and affective psychosis identified from psychiatric in-patient and out-patient registries | Small Area Market Statistics (SAMs) from Sweden used to determine ethnic enclaves | Proportion Iraqi people ‘enclave’ versus ‘non-enclave’ areas. | Age, gender, family income, education attainment, generation status | Multi-level logistic regression models | Iraqi people living in Iraqi enclaves did not have an increased risk of psychosis | 16 |
| Kirkbride, Morgan et al., 2007(Kirkbride et al., 2007) | Aetiology and Ethnicity in Schizophrenia and Other Psychoses study (AESOP); (UK) | 218 cases aged 16-64 identified during 565 000 person-years of follow-up over a 2-year period (1997–1999). | Schedules for Clinical Assessment in Neuropsychiatry (SCAN) and a modified Personal and Psychiatric History Schedule. Non-affective psychoses (F20–29), Schizophrenia (F20), Other non-affective psychoses (F21–29) | Census statistical wards (CAS wards) | Proportion of ethnic minorities in ward | Age, gender Population density, ethnic fragmentation, Index of Multiple Deprivation |
Multilevel Poisson regression with random effects | Trend for negative association between overall ethnic minority density and risk of schizophrenia for ethnic minority individuals. Association not statistically significant. | 12 |
| Kirkbride, Boydell et al., 2008(Kirkbride et al., 2008) | AESOP and postal survey conducted January and March 2004, and January and March 2006; (UK) | 4231 survey participants living in South London (8.2% Black Caribbean and 7% Black African) | Ethnic minorities living in neighbourhoods with the lowest proportion of ethnic minorities had higher risk of schizophrenia than white people. This increased risk was not statistically significant in areas of medium and high ethnic density. | ||||||
| Menezes et al, 2011(Menezes et al., 2011) | CCHS 2002; (Canada) | 35708 individuals of which 21.8% immigrant and 78.2% non-immigrant | WMH-CIDI; respondents given screening questions on whether they had a life time diagnosis of schizophrenia or any other psychosis | Dissemination Area (DA) | Percentage immigrants | Age, gender, income, marital status, education. Mean income, % moving in the past 5 years, % rental & % below low income cut-off thresholds | Multilevel multivariate logistic regression models | Very weak evidence supportive of immigrants in the sample having a reduced relative odds of reporting life-time schizophrenia or psychosis diagnosis with increasing immigrant density. | 12 |
| Kirkbride et al, 2014 (Kirkbride et al., 2014) | East London First Episode Study (ELFEP); (UK) | 484 people with First episode psychosis, aged 18-65; 68 white British, 38 non-British white, 55 black Caribbean, 49 black African, 53 Bangladeshi people | SCAN: Non-affective psychoses (schizophrenia, schizophreniform disorder, and schizoaffective disorder) & affective psychoses | ‘statistical wards’ based on information from LSOA | SD increase in own group density | Age at first contact, social class, gender, ethnicity | Bayesian hierarchical modelling of standardised incidence ratios | Reduced risk of psychosis in black African people with increasing own group density | 10.5 |
| Veling et al., 2008(Wim Veling et al., 2008) | Prospective first-contact incidence study of psychotic disorders in the Hague over 7-year period (from April 1, 1997 to April 1 1999 and October 1, 2000 to October 1, 2005); (Netherlands) | 463 subjects of Moroccan, Surinamese, Turkish, and native Dutch origin | Comprehensive Assessment of Symptoms and History | Neighbourhoods classified according to postal codes (n=44). Maximum of 38,000 inhabitants per neighbourhood. | Percentage immigrant group | Age, gender, marital status, area-level deprivation (average income, housing quality, proportion long-term unemployed, mean educational level) | Multilevel poisson regression |
Compared with native Dutch, immigrants had a higher incidence rate of schizophrenia in low ethnic density neighbourhoods, but not in high ethnic density neighbourhoods. Interactions between ethnic density and ethnicity showed a significant ethnic density effect for Moroccans only, so that elevated incidence rates of psychotic disorders was higher among Moroccan people living in low ethnic density neighborhoods. |
10 |
| PSYCHOTIC EXPERIENCES | |||||||||
| *Das-Munshi et al, 2012(Das-Munshi et al., 2012) *Bécares and Das-Munshi, 2013(Bécares and Das-Munshi, 2013) |
EMPIRIC; (UK) | 837 white British, 733 Irish, 694 black Caribbean people, 650 Bangladeshi, 643 Indian and 724 Pakistani people | Psychosis Screening Questionnaire (PSQ) | Middle super output level | Percentage people of same ethnic group | Age, gender, social class, education, marital status, area-level deprivation | Multilevel multivariate logistic regression |
Strong evidence of increased OR of psychotic experiences with decreasing ethnic density for Indian people. Weaker evidence of increased OR psychotic experiences with decreasing ethnic density for Irish and Bangladeshi people. No association for black Caribbean and Pakistani people. |
15 |
| *Bécares et al., 2009(Bécares et al., 2009) | FNS; (UK) | 2867 white British, 1205 black Caribbean, 1273 Indian, 728 African Asian, 1185 Pakistani, 591 Bangladeshi, 214 Chinese people | Psychosis Screening Questionnaire (PSQ) | Electoral ward | Percentage people of same ethnic group | Age, gender, socioeconomic position. A Classification of Residential Neighbourhoods (ACORN) measure of area deprivation | Regression models with robust standard errors |
Protective association between ethnic density and psychotic symptomatology for Indian and Bangladeshi respondents. Detrimental association for Pakistani respondents. |
14 |
| *Halpern et al, 2000(Halpern and Nazroo, 2000) | FNS; (UK) | 2867 white British, 1205 black Caribbean, 1273 Indian, 728 African Asian, 1185 Pakistani, 591 Bangladeshi, 214 Chinese people | Psychosis Screening Questionnaire (PSQ) | Electoral ward | Percentage people of same ethnic group | Age, gender, hardship, language, age at migration | Multivariate linear regression |
Ethnic minorities had a lower mean score on PSQ in areas of higher ethnic density Indian, Caribbean and Bangladeshi people had lower mean PSQ scores in areas of higher ethnic density |
10 |
| SUICIDE | |||||||||
| Termorshuizen et al., 2015(Termorshuizen et al., 2015) | Population registry linked to the causes of death registry of Statistics Netherlands, 2000-2011; (Netherlands) | 20240668 person years of observation (59% Dutch, 13% Other western, 5% Turkish, 5.5% Moroccan, 9.7% Surinamese/Antillean, 7.4% Other non-Western) | ICD-10 X60-84, ICD-10 Y10-34 | 384 neighbourhoods in Amsterdam, Rotterdam, Den Haag, and Utrecht | Percentage of observation time in 2000-2011 related to a specific ethnic group | Age, gender, mean neighbourhood income | Multilevel Poisson regression | Increasing minority density was associated with a decreased rate ratio (RR) of suicide among immigrants (both Western and non-Western), when compared to Dutch people. | 8 |
| Neeleman and Wessely, 1999(Neeleman and Wessely, 1999) | Coroners' records of suicides in Lewisham, Lambeth, Southwark, Greenwich between 1 January 1991 and 31 December 1993; (UK) | 902,008 cases | Deaths considered as suicides if suicide verdicts given, suicide notes found, methods unambiguously indicated suicide and/or communications of suicidal intent had been recorded | 109 electoral wards of the London boroughs of Lewisham, Lambeth, Southwark and Greenwich | Proportions of all ethnic minority groups combined in ward; proportion Afro-Caribbean residents in ward; proportion Asians in ward | Age, gender, local Jarman underprivileged area (UPA) scores excluding ethnicity | Random effects Poisson regression | Increased ethnic density was associated with lower suicide rates among ethnic minority groups | 7 |
| SUICIDAL IDEATION | |||||||||
| *Bécares and Das-Munshi, 2013(Bécares and Das-Munshi, 2013) | EMPIRIC; (UK) | 837 white British, 733 Irish, 694 black Caribbean people, 650 Bangladeshi, 643 Indian and 724 Pakistani people | Suicidal ideation | Middle super output level | Percentage people of same ethnic group | Age, gender, social class, education, marital status, generation, area-level deprivation | Multilevel multivariate logistic regression |
Protective associations for suicidal ideation in Bangladeshi and Irish people. No associations between ethnic density and suicidal ideation for the other ethnic minority groups. |
15 |
| *Bécares et al., 2012(Bécares et al., 2012a) | NSAL, (USA) and EMPIRIC, (UK) | 1568 black Caribbean American and 661 black English people. Aged 18 to 74 |
Suicidal ideation | Census tracts, middle super output level | Percentage born in the Caribbean Percentage black Percentage black Caribbean Percentage black African + black Caribbean + black Other |
Age, gender, household income, educational qualifications, employment, nativity, marital status, racism and discrimination, area-level deprivation | Multilevel multivariate logistic regression | No associations between any of the two ethnic density measures and suicidal ideation for black Caribbean American people. No associations between any of the two ethnic density measures and suicidal ideation for black Caribbean English people. |
13 15 |
Key: Bolded references refer to estimates included in meta-analyses; Green-colored text indicates protective ethnic density effects; Red-colored text indicates detrimental ethnic density effects.
In general, qualitative assessment of included studies (Table 1) provide support for a protective association between increased own ethnic density and reduced risk of depression, anxiety and the common mental disorders, suicide, suicidality, psychotic experiences and psychosis; for all outcomes over half of studies supported protective associations. This was particularly evident for psychotic experiences (3/4 studies) and suicide (2/2 studies). Negative associations were identified only in US studies. Out of 30 international studies that assessed the association between ethnic density and common mental disorders, depression, and anxiety, 6 reported a detrimental effect in African American and Latino populations; all of these studies were from the US. One of these studies examined the non-linearity of ethnic density and depression in African American people and found that the detrimental association of own ethnic density and depression was only observed at the highest level of ethnic density (85% or greater); at levels below this the association was protective (Bécares et al., 2014).
One UK-based study (out of 4) reported detrimental associations between Pakistani ethnic density and psychotic experiences. There were no studies of psychosis and suicidality in the narrative review that reported detrimental associations with ethnic density (Table 1).
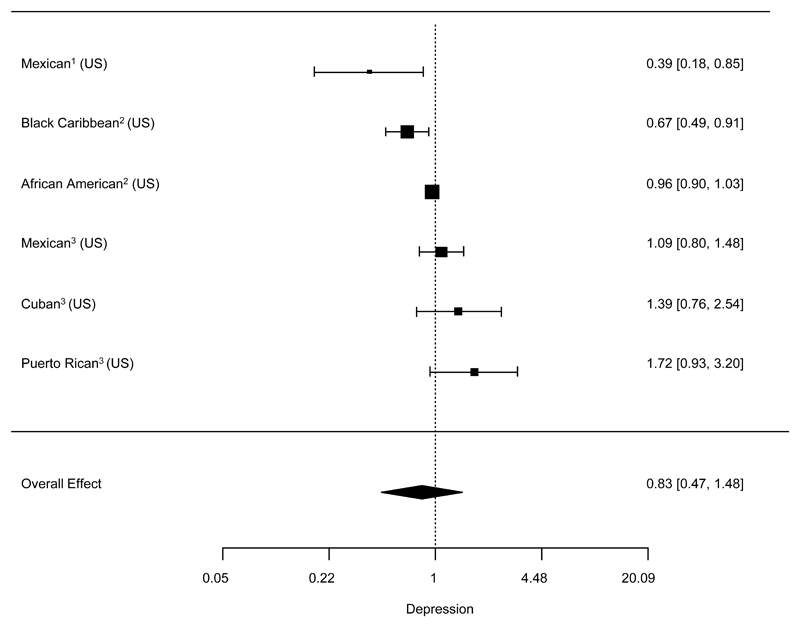
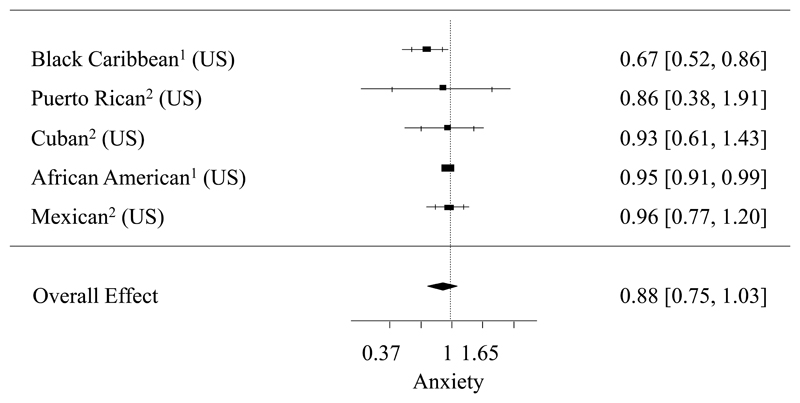
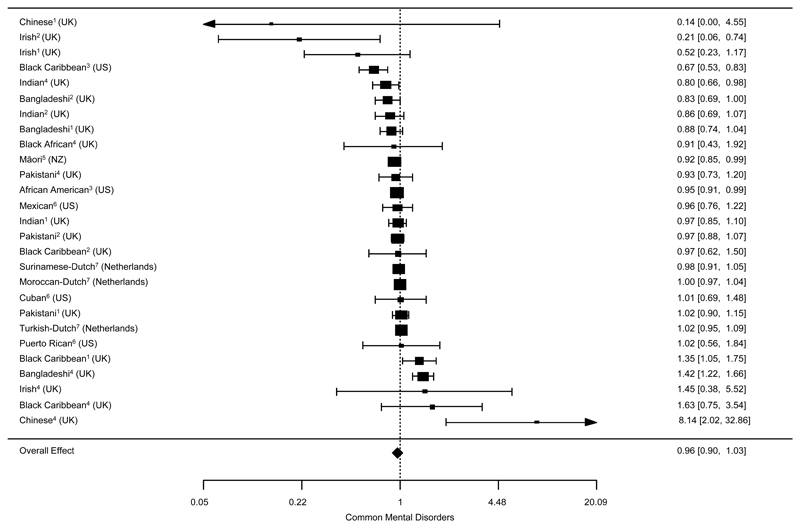
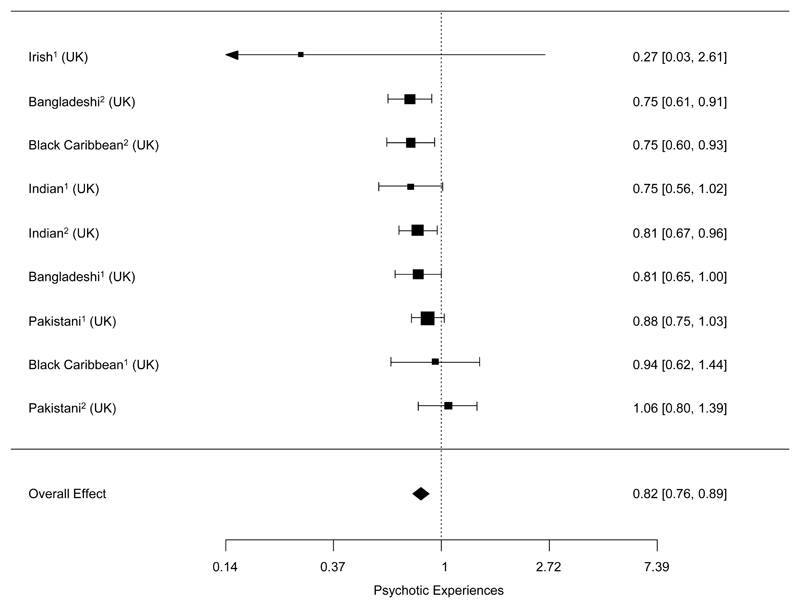
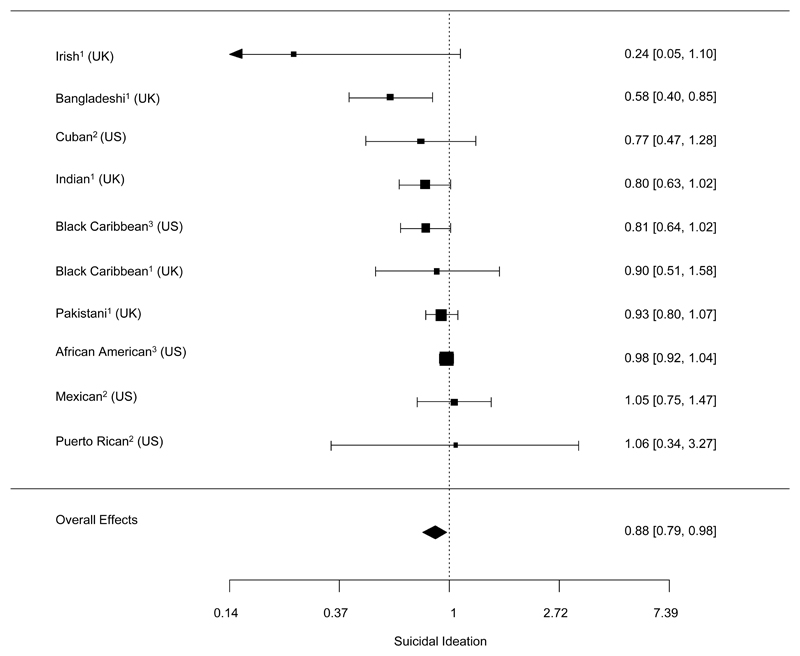
In the meta-analysis, we found that for common mental disorders, depression and anxiety, associations were indicative of protective effects of own ethnic density, however 95% confidence intervals just spanned the null (Figures 2, 3 and 4). We also observed a large reduction in relative odds of psychotic experiences (OR 0.82(95% CI: 0.76, 0.89)) and suicidal ideation (OR: 0.88(95% CI: 0.79, 0.98)) for each 10 percentage point increase in own ethnic density (Figures 5-6).
Figure 2. Forest plot of the association between 10% increase in own ethnic density and depression.
1: Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE); 2: National Survey of American Life (NSAL); 3: National Latino and Asian American Study (NLAAS); I2: estimates between datasets 76.9%, estimates within datasets 13.2%
Figure 3. Forest plot of the association between 10% increase in own ethnic density and anxiety.
1: National Survey of American Life (NSAL); 2: National Latino and Asian American Study (NLAAS)
Figure 4. Forest plot of the association between 10% increase in own ethnic density and common mental disorders.
1: Health Survey for England (HSE) 1999; 2: Ethnic Minority Psychiatric Illness Rates in the Community (EMPIRIC); 3: National Survey of American Life (NSAL); 4: HSE 2004; 5: New Zealand Health Survey (NZHS); 6: National Latino and Asian American Study (NLAAS); 7: G4 Monitor 2008; I2: estimates between datasets 0%, estimates within datasets 82.2%
Figure 5. Forest plot of the association between 10% increase in own ethnic density and psychotic experiences.
1: Ethnic Minority Psychiatric Illness Rates in the Community (EMPIRIC); 2: Fourth National Survey of Ethnic Minorities (FNS); I2: estimates between datasets 8.4%
Figure 6. Forest plot of the association between 10% increase in own ethnic density and suicidal ideation.
1: Ethnic Minority Psychiatric Illness Rates in the Community (EMPIRIC); 2: National Latino and Asian American Study (NLAAS); 3: National Survey of American Life (NSAL); I2: estimates between datasets 54.5%
We assessed the role of race/ethnicity, country, generational status and area-level deprivation as moderators in the association between own ethnic density and each of the mental health outcomes. Assessment for a priori moderators indicated that these did not account for any observed heterogeneity across estimates.
From the studies reviewed, several mechanisms emerged as providing possible explanations behind ethnic density effects. Racism and social support were the most commonly examined mechanisms. Studies across different national settings suggested that reports of experienced racial discrimination were lower in areas of higher own ethnic density, and reports of social support were higher(Arévalo et al., 2015, Bécares, 2014, Bécares et al., 2013, Bécares and Das-Munshi, 2013, Bécares et al., 2012a, Bécares et al., 2009, Das-Munshi et al., 2012, Das-Munshi et al., 2010, Shell et al., 2013). Studies provided support for the role of perceived racism and social support in either moderating(Bécares et al., 2009, Shell et al., 2013, Syed and Juan, 2012), or mediating(Bécares, 2014, Bécares et al., 2009, Das-Munshi et al., 2012, English et al., 2014, Shell et al., 2013) the association between own ethnic density and mental health outcome. Other less explored mechanisms included social cohesion(Bécares, 2014, Syed and Juan, 2012), acculturation (Arévalo et al., 2015) and stress (Das-Munshi et al., 2012, Shell et al., 2013).
In many of the studies area-level deprivation was adjusted for as a confounder. Only a few studies permitted the comparison of models adjusted for/ not adjusted for area-level deprivation (Bécares et al., 2013, Bécares et al., 2014, Mezuk et al., 2015, Schrier et al., 2014). Where it was possible to assess adjustment for area-level deprivation, protective ethnic density associations became stronger or more apparent, and detrimental ethnic density associations reversed direction into a positive association (Bécares et al., 2013, Bécares et al., 2014, Mezuk et al., 2015, Schrier et al., 2014). Formal assessment of area-level deprivation as a moderator in the meta-analysis did not provide any conclusive results.
Discussion
Our meta-analysis and review finds evidence indicating protective ethnic density effects across suicidal ideation and psychotic experiences. For common mental disorders, depression and anxiety, associations were indicative of protective effects but were of a smaller magnitude. For psychosis, although we were unable to perform meta-analysis on any of the studies, the narrative review indicated protective density effects across three studies (Kirkbride et al., 2008, Kirkbride et al., 2014, Wim Veling et al., 2008), with no evidence of detrimental associations across the other studies. The results of the meta-analysis for depression and anxiety were all from the US, and so should be considered in light of this limitation. Nonetheless, findings relating to all the mental health outcomes were broadly consistent with the narrative review, which tended to suggest positive associations, except for some negative findings reported in US studies.
Because the ethnic density variable was scaled as per 10% increase, these estimates appear to be small effects, however given the range of actual own ethnic density (eg. Bangladeshi people in the UK ranging up to 73% own ethnic density, Māori people in New Zealand up to 86% and Black Caribbean people in the US up to 53%) (Bécares et al., 2013, Bécares et al., 2012a, Bécares et al., 2009) in absolute terms, this means that for people from minority groups living in higher ranges of own ethnic density this could translate into larger protective effects for mental health. Conversely for people from minority groups living in areas of the lowest own ethnic density these associations potentially represent larger detrimental effects. Results from the meta-analysis did not find any evidence of detrimental effects of ethnic density on any mental health outcomes.
The mechanisms underlying ethnic density effects are not yet fully understood although the evidence suggests that in areas of higher own ethnic density experiences of racial discrimination are fewer, and the association between racism and adverse mental health outcomes are weaker. Studies show that in these areas levels of social support are higher. Our assessment of moderation by race/ethnicity, country, generational status, and area-level deprivation did not find any support in moderation by these variables. This may suggest that ethnic density associations are not particular to one racial/ethnic group or national context but rather may be a consequence of being a marginalized racial/ethnic minority. We were only able to empirically assess heterogeneity across 12 studies which may limit conclusions. Other factors such as social cohesion, stigma in reporting mental health problems in areas of high ethnic density, stress and acculturation may play a role, however further research is needed.
Strengths and limitations
This is the first systematic review with meta-analysis and detailed meta-regression to explore ethnic density effects on several mental health outcomes. Our inclusion criteria enables allows us to be certain that the findings are not a function of help-seeking differences. This is important as it is known that there are potential differences by race/ethnicity in health-seeking behaviors and more complex pathways into care for mental disorders (Bhui et al., 2003). Our inclusion of “leakage” studies for rare conditions such as psychosis in this review meant that we also included people with serious mental illness who would be missed in general population surveys. The use of meta-analysis with meta-regression allowed us to explore potential sources of heterogeneity which have previously been unexplored. The breadth of the systematic reviews meant that we were able to include estimates across national settings and diverse populations, which took into account characteristics such as generational status, area-level deprivation, and individual-level covariates such as age, gender and socioeconomic position. The review also includes previously unpublished data, which will have reduced publication biases and increased the validity of findings. This was confirmed by formal statistical assessment of publication biases. One of the limitations is that due to data availability we were only able to meta-analyze 12 studies and most of this data came from observational, cross-sectional studies, which did not allow us to ascertain the direction of causality or temporality of associations and also limited conclusions with respect to sources of heterogeneity. We aimed to address this through the narrative review which demonstrates difference across and within countries. Our review encompasses a number of countries, and although we did not restrict studies by location, generalizability of our findings is restricted to those countries included. In addition, we restricted inclusion criteria to studies of ethnic density that focused on adults, but for some of these mental health conditions, the risk for disorders may emerge earlier in the life course. Future research should consider the development of mental health disorders and the exposure to socio-environmental stressors earlier in the life course.
We were not able to assess the existence of threshold effects in the meta-analysis, but two studies in the literature document a non-linear association between ethnic density and mental health. Both studies noted this in African American populations in the US, for whom levels of own ethnic density are higher (Bécares et al., 2014, Mair et al., 2010). In one of the two studies the investigators noted that detrimental associations of own ethnic density with depression were only observed at a higher threshold of 85% or greater own ethnic density; at levels below this the association was protective (Bécares et al., 2014). These findings highlight that in the US extreme levels of own ethnic density as found among African American populations are not always beneficial for mental health, as these areas are characterized by long-standing dis-investment and concentrated poverty (Williams and Collins, 2001). It is this concentration of poverty, and not of ethnic minority people, which drives the harmful associations for mental health. Although we were unable to assess this further due to a lack of data, this could be relevant to other international contexts.
There are longstanding concerns that pre-existing mental health problems may cause people to “drift” into less affluent neighborhoods (Halpern and Nazroo, 2000). High levels of ethnic density correlate with high-levels of deprivation (Bécares et al., 2013, Bécares et al., 2014, Bécares et al., 2012a, Bécares et al., 2009, Bécares et al., 2012b), and these two phenomena operate in opposite directions – whereas area deprivation is associated with worse health (Pickett and Pearl, 2001), our meta-analysis and narrative review show that ethnic density has protective associations for the mental health of racial/ethnic minority people. If the drift hypothesis was true, one would anticipate that racial/ethnic minority people living in areas of high deprivation, and high ethnic density, would have higher rates of mental disorders, but in fact the opposite is true. Once area deprivation is adjusted for, living in areas of high ethnic density is protective for mental health. It is also possible that people with mental disorders move away from family and friends. However, in the context of ethnic density, it is unlikely that this move would happen towards an area of reduced ethnic density, as these areas tend to be more affluent. This would mean that individuals with mental disorders would have the social and economic resources to be able to move into a less dense, and more affluent area, which is unlikely as the evidence suggests that individuals with mental disorders tend to have lower socioeconomic resources (Lorant et al., 2003).
Implications
A previous narrative review found consistent associations for ethnic density and psychosis, and was only to make tentative conclusions about the association between ethnic density and other mental disorders (Shaw et al., 2012). Despite the methodological challenges of the present study, which included limited availability and heterogeneity of data, differential adjustment for confounders, and the differing contexts of racial/ethnic groups across different national settings, the findings of the current study are able to indicate, for the first time, protective ethnic density associations across countries and racial/ethnic minority populations, as well as across mental health outcomes. This is indicative of the importance of the social environment in patterning detrimental mental health outcomes in marginalized and excluded population groups, in particular the role of social exclusion (Selten and Cantor-Graae, 2005), racism and racial discrimination (Bécares et al., 2009) and minority stigma (Pickett and Wilkinson, 2008) for health.
Attempts to engineer patterns of racial/ethnic minority and migrant settlement have led to public policy initiatives to address the tendency for new migrants to concentrate in diverse cities by actively seeking to disperse people more widely, across a range of international settings, including the US, Canada, Australia and Europe and the UK, among others. These dispersal programmes place immigrants in areas with limited previous history of accommodating new migrants and lower ethnic density (Robinson and Reeve, 2006, Stewart and Shaffer, 2015). Although our study was not designed to examine this, results of our review and meta-analysis alert us to the possible unintended mental health consequences of these policies for new migrants, and provide evidence for positive outcomes emerging from the residential concentration of racial/ethnic minority populations, as long as the deprivation and concentrated poverty in these areas are adequately addressed.
Supplementary Material
Acknowledgements
We are grateful to all authors who responded to our inquiries. In particular we are grateful to the following authors for providing additional data: James Kirkbride, Sandra Arévalo, Devon English, Jamie Booth, Inma Jarrin, Thomas Jucik, Fabian Temorshuizen, Ozcan Erdem, and Kristine Molina. We are grateful to Craig Morgan for advice on leakage studies for psychosis. We are grateful to Richard Shaw for sharing search strategies from an earlier review. We are grateful to the British Library for use of their reading rooms and other facilities.
Financial Support:
LB was funded by the ESRC (grant number ES/K001582/1) and a Hallsworth Research Fellowship. JD is funded by the Health Foundation/Academy of Medical Sciences.
Footnotes
Conflict of Interest
None
References
- Alegria M, Molina KM, Chen CN. Neighborhood characteristics and differential risk for depressive and anxiety disorders across racial/ethnic groups in the United States. Depression & Anxiety. 2014;31:27–37. doi: 10.1002/da.22197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel CS, Wight RG, Miller-Martinez D, Botticello AL, Karlamangla AS, Seeman TE. Urban neighborhoods and depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2007;62:S52–S59. doi: 10.1093/geronb/62.1.s52. [DOI] [PubMed] [Google Scholar]
- Arévalo SP, Tucker KL, Falcón LM. Beyond cultural factors to understand immigrant mental health: Neighborhood ethnic density and the moderating role of pre-migration and post-migration factors. Social Science & Medicine. 2015;138:91–100. doi: 10.1016/j.socscimed.2015.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L. Ethnic density effects on psychological distress among Latino ethnic groups: An examination of hypothesized pathways. Health & Place. 2014;30:177–186. doi: 10.1016/j.healthplace.2014.09.010. [DOI] [PubMed] [Google Scholar]
- Bécares L, Cormack D, Harris R. Ethnic density and area deprivation: neighbourhood effects on Maori health and racial discrimination in Aotearoa/New Zealand. Social Science & Medicine. 2013;88:76–82. doi: 10.1016/j.socscimed.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Das-Munshi J. Ethnic density, health care seeking behaviour and expected discrimination from health services among ethnic minority people in England. Health & Place. 2013;22:48–55. doi: 10.1016/j.healthplace.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Bécares L, Nazroo J, Jackson J. Ethnic density and depressive symptoms among African Americans: Threshold and differential effects across social and demographic subgroups. American Journal of Public Health. 2014;104:2334–2341. doi: 10.2105/AJPH.2014.302047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Nazroo J, Jackson J, Heuvelman H. Ethnic density effects on health and experienced racism among Caribbean people in the US and England: a cross-national comparison. Social Science & Medicine. 2012a;75:2107–2115. doi: 10.1016/j.socscimed.2012.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health & Place. 2009;15:670–678. doi: 10.1016/j.healthplace.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Bécares L, Shaw R, Nazroo J, Stafford M, Albor C, Atkin K, Kiernan K, Wilkinson R, Pickett K. Ethnic density effects on physical morbidity, mortality, and health behaviors: a systematic review of the literature. American Journal of Public Health. 2012b;102:e33–66. doi: 10.2105/AJPH.2012.300832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhui K, Stansfeld SA, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK. British Journal of Psychiatry. 2003;182:105–116. doi: 10.1192/bjp.182.2.105. [DOI] [PubMed] [Google Scholar]
- Booth JM. The protective effect of community organization on distress in disadvantaged neighborhoods: Considering the Latino experience in Chcago. Arizona State University; 2014. [Google Scholar]
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Choi S, Kim G, Lee S. Effects of Nativity, Length of Residence, and County-Level Foreign-Born Density on Mental Health Among Older Adults in the U.S. Psychiatr Q. 2016;87:675–688. doi: 10.1007/s11126-016-9418-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das-Munshi J, Bécares L, Boydell JE, Dewey ME, Morgan C, Stansfeld SA, Prince MJ. Ethnic density as a buffer for psychotic experiences: findings from a national survey (EMPIRIC) British Journal of Psychiatry. 2012;201:282–290. doi: 10.1192/bjp.bp.111.102376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das-Munshi J, Bécares L, Dewey ME, Stansfeld SA, Prince MJ. Understanding the effect of ethnic density on mental health: multi-level investigation of survey data from England. BMJ. 2010;341:c5367. doi: 10.1136/bmj.c5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecob R, Williams R. Sampling Asian minorities to assess health and welfare. Journal of Epidemiology and Community Health. 1991;45:93–101. doi: 10.1136/jech.45.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Lambert SF, Evans MK, Zonderman AB. Neighborhood Racial Composition, Racial Discrimination, and Depressive Symptoms in African Americans. American journal of community psychology. 2014;54:219–228. doi: 10.1007/s10464-014-9666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X, Astell-Burt T, Kolt GS. Do social interactions explain ethnic differences in psychological distress and the protective effect of local ethnic density? A cross-sectional study of 226 487 adults in Australia. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-002713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. International Journal of Social Psychiatry. 2000;46:34–46. doi: 10.1177/002076400004600105. [DOI] [PubMed] [Google Scholar]
- Jarrin I, Garcia-Fulgueiras A, Ibanez-Rojo V, Alvarez D, Garcia-Pina R, Fernandez-Liria A, Garcia-Ortuzar V, Diaz D, Angeles Rodriguez-Arenas M, Mazarrasa L, Zunzunegui MV, et al. Absence of protective ethnic density effect on Ecuadorian migrants' mental health in a recent migration setting: a multilevel analysis. Social Psychiatry and Psychiatric Epidemiology. 2013;48:95–103. doi: 10.1007/s00127-012-0523-8. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Cooper R. Considerations for use of racial/ethnic classification in etiologic research. American Journal of Epidemiology. 2001;154:291–298. doi: 10.1093/aje/154.4.291. [DOI] [PubMed] [Google Scholar]
- Khan KS, Riet Gt, Popay J, Nixon J, Kleijnen J. STAGE II: Conducting the review; PHASE 5: Study quality assessment. In: Khan KS, Riet Gt, Glanville H, Sowden AJ, Kleijnen J, editors. CRD Report Number 4. NHS Centres for Reviews and Dissemination (CRD); York, UK: 2001. [Google Scholar]
- Kirkbride JB, Boydell J, Ploubidis GB, Morgan C, Dazzan P, McKenzie K, Murray RM, Jones PB. Testing the association between the incidence of schizophrenia and social capital in an urban area. Psychol Med. 2008;38:1083–1094. doi: 10.1017/S0033291707002085. [DOI] [PubMed] [Google Scholar]
- Kirkbride JB, Jones PB, Ullrich S, Coid JW. Social deprivation, inequality, and the neighborhood-level incidence of psychotic syndromes in East London. Schizophrenia Bulletin. 2014;40:169–180. doi: 10.1093/schbul/sbs151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Morgan C, Fearon P, Dazzan P, Murray RM, Jones PB. Neighbourhood-level effects on psychoses: re-examining the role of context. Psychological Medicine. 2007;37:1413–1425. doi: 10.1017/S0033291707000499. [DOI] [PubMed] [Google Scholar]
- Kwag KH, Jang Y, Rhew SH, Chiriboga DA. Neighborhood effects on physical and mental health: A study of Korean American older adults. Asian American Journal of Psychology. 2011;2:91–100. doi: 10.1037/a0023656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leu J, Walton E, Takeuchi D. Contextualizing acculturation: gender, family, and community reception influences on Asian immigrant mental health. American Journal of Community Psychology. 2011;48:168–180. doi: 10.1007/s10464-010-9360-7. [DOI] [PubMed] [Google Scholar]
- Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic Inequalities in Depression: A Meta-Analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Mair C, Roux AVD, Osypuk TL, Rapp SR, Seeman T, Watson KE. Is neighborhood racial/ethnic composition associated with depressive symptoms? The multi-ethnic study of atherosclerosis. Social Science & Medicine. 2010;71:541–550. doi: 10.1016/j.socscimed.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menezes NM, Georgiades K, Boyle MH. The influence of immigrant status and concentration on psychiatric disorder in Canada: a multi-level analysis. Psychological Medicine. 2011;41:2221–2231. doi: 10.1017/S0033291711000213. [DOI] [PubMed] [Google Scholar]
- Mezuk B, Li X, Cederin K, Concha J, Kendler KS, Sundquist J, Sundquist K. Ethnic enclaves and risk of psychiatric disorders among first- and second-generation immigrants in Sweden. Social Psychiatry and Psychiatric Epidemiology. 2015;50:1713–1722. doi: 10.1007/s00127-015-1107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray C, Lopez A. The Global Burden of Disease. Harvard University Press; Cambridge, MA: 1996. [Google Scholar]
- Neeleman JAN, Wessely S. Ethnic minority suicide: a small area geographical study in south London. Psychological Medicine. 1999;29:429–436. doi: 10.1017/s003329179800806x. [DOI] [PubMed] [Google Scholar]
- Ostir G, Eschbach K, Markides K, Goodwin J. Neighbourhood composition and depressive symptoms among older Mexican Americans. Journal of Epidemiology and Community Health. 2003;57:987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K, Pearl M. Multilevel analyses of neighbourhood socieoconomic context and health outcomes: a critical review. Journal of Epidemiology & Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K, Wilkinson R. People like us: ethnic group density effects on health. Ethnicity & Health. 2008;13:321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. Lancaster University; 2006. [Google Scholar]
- Propper C, Jones K, Bolster A, Burgess S, Johnston R, Sarker R. Local neighbourhood and mental health: Evidence from the UK. Social Science & Medicine. 2005;61:2065–2083. doi: 10.1016/j.socscimed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Robinson D, Reeve K. Neighbourhood experiences of new immigration. Reflections from the evidence base. Joseph Rowntree Foundation; York: 2006. [Google Scholar]
- Schrier AC, Peen J, de Wit MAS, van Ameijden EJC, Erdem Ö, Verhoeff AP, Dekker JJM, Beekman ATF. Ethnic density is not associated with psychological distress in Turkish-Dutch, Moroccan-Dutch and Surinamese-Dutch ethnic minorities in the Netherlands. Social Psychiatry and Psychiatric Epidemiology. 2014;49:1557–1567. doi: 10.1007/s00127-014-0852-x. [DOI] [PubMed] [Google Scholar]
- Selten JP, Cantor-Graae E. Social defeat: risk factor for schizophrenia? British Journal of Psychiatry. 2005;187:101–102. doi: 10.1192/bjp.187.2.101. [DOI] [PubMed] [Google Scholar]
- Shaw RJ, Atkin K, Bécares L, Albor CB, Stafford M, Kiernan KE, Nazroo JY, Wilkinson RG, Pickett KE. Impact of ethnic density on adult mental disorders: narrative review. British Journal of Psychiatry. 2012;201:11–19. doi: 10.1192/bjp.bp.110.083675. [DOI] [PubMed] [Google Scholar]
- Shaw RJ, Pickett KE. The association between ethnic density and poor self-rated health among US Black and Hispanic people. Ethnicity & Health. 2011;16:225–44. doi: 10.1080/13557858.2011.561428. [DOI] [PubMed] [Google Scholar]
- Shell AM, Peek MK, Eschbach K. Neighborhood Hispanic composition and depressive symptoms among Mexican-descent residents of Texas City, Texas. Social Science & Medicine. 2013;99:56–63. doi: 10.1016/j.socscimed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford M, Newbold BK, Ross NA. Psychological distress among immigrants and visible minorities in Canada: A contextual analysis. International Journal of Social Psychiatry. 2011;57:428–441. doi: 10.1177/0020764010365407. [DOI] [PubMed] [Google Scholar]
- Stewart E, Shaffer M. Moving on? Dispersal Policy, Onward Migration and Integration of Refugees in the UK. University of Strathclyde; Glasgow: 2015. [Google Scholar]
- Syed M, Juan MJD. Discrimination and psychological distress: Examining the moderating role of social context in a nationally representative sample of Asian American adults. Asian American Journal of Psychology. 2012;3:104–120. [Google Scholar]
- Team, R. C. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2015. [Google Scholar]
- Termorshuizen F, Braam AW, van Ameijden EJC. Neighborhood ethnic density and suicide risk among different migrant groups in the four big cities in the Netherlands. Social Psychiatry and Psychiatric Epidemiology. 2015;50:951–962. doi: 10.1007/s00127-014-0993-y. [DOI] [PubMed] [Google Scholar]
- United Nations, D. o. E. a. S. A., Population Division. International Migration Report 2015 (ST/ESA/SER.A/384) United Nations; 2016. [Google Scholar]
- Viechtbauer W. Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software. 2010;36:1–48. [Google Scholar]
- Vogt Yuan AS. Racial Composition of Neighborhood and Emotional Well-Being. Sociological Spectrum. 2007;28:105–129. [Google Scholar]
- Whiteford H, Degenhardt L, Rehm J, Baxter A, Ferrari A, Erskine H, Charlson F, Norman R, Flaxman A, Johns N, Burstein R, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Wight RG, Cummings JR, Karlamangla AS, Aneshensel CS. Urban Neighborhood Context and Change in Depressive Symptoms in Late Life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64B:247–251. doi: 10.1093/geronb/gbn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight RG, Ko MJ, Aneshensel CS. Urban neighborhoods and depressive symptoms in late middle age. Research on Aging. 2011;33:28–50. doi: 10.1177/0164027510383048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veling Wim, Susser Ezra, M.D., Dr.Ph., Susser Ezra, M. D., Dr.Ph., van Os Jim, M.D., Ph.D., van Os Jim, M. D., Ph.D., Mackenbach Johan P, M.D., Ph.D., Mackenbach Johan P, M. D., Ph.D., Selten Jean-Paul, M.D., Ph.D., Selten Jean-Paul, M. D., Ph.D., Hoek Hans W, M.D., Ph.D., Hoek Hans W., M. D., Ph.D. Ethnic Density of Neighborhoods and Incidence of Psychotic Disorders Among Immigrants. American Journal of Psychiatry. 2008;165:66–73. doi: 10.1176/appi.ajp.2007.07030423. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.