Abstract
Birt-Hogg-Dube (BHD) syndrome is an unusual disorder characterized by the triad of cutaneous lesions, renal tumors and lung cysts. In cases with BHD syndrome, the frequency of recurrent pneumothorax is increased due to presence of multiple lung cysts. It is important to evaluate the BHD syndrome in differential diagnosis of recurrent pneumothorax especially with multiple lung cysts predominating in the lung base. In these patients, the presence of accompanying kidney and other tumors should be investigated. Herein, we report a case of BHD syndrome presenting with recurrent pneumothorax.
Keywords: Birt-Hogg-Dube syndrome, cystic lung disease, pneumothorax, pituitary adenoma
INTRODUCTION
Spontaneous pneumothorax can be classified as primary or secondary depending on the presence or absence of an underlying lung disease, such as cystic lung diseases. Birt-Hogg-Dube (BHD) syndrome is an autosomal dominant disorder characterized by the development of cutaneous lesions, renal tumors and lung cysts. In cases with BHD syndrome, the frequency of recurrent pneumothorax is increased due to presence of multiple lung cysts [1]. Herein, we report a case of a 34-year-old woman with BHD syndrome who admitted to the emergency department with complaints of dyspnea and chest pain due to pneumothorax. We present imaging findings and associated conditions in BHD syndrome.
CASE PRESENTATION
A 34-year-old female patient was admitted to the emergency department with sudden onset of breathlessness and left-sided chest pain. The patient had complaints for 6 hours. The patient was a non-smoker. She had a history of spontaneous pneumothorax five years ago and a diagnosis of prolactin secreting pituitary adenoma for three years. Her family history revealed that the patient’s mother had a history of pneumothorax, and her aunt had cystic lung disease. Physical examination revealed breath sounds were reduced over the left side. Papular skin lesions involving the nose, face and chest wall were detected. She was afebrile and her blood pressure was normal. Chest x-ray showed suspicious focal pneumothorax on the left side. Computed tomography (CT) of the chest was obtained. Chest CT confirmed a loculated pneumothorax on the left side. Bilateral multiple lung cysts various in size and shape, predominantly located in the basal regions were evident (Figure 1). A chest tube was inserted into the left side and the pneumothorax improved immediately. The patient was diagnosed as BHD syndrome because of the presence of lung cysts and skin lesions, and her history suggestive of BHD syndrome. Contrast-enhanced CT of the abdomen was performed to investigate the presence of renal lesions. Abdominal CT scan showed a contrast-enhancing mass in the upper pole of the right kidney (Figure 2). Biopsy of the dermatologic lesions showed trichodiscoma and BHD syndrome diagnosis was confirmed by the identification of a mutation in the folliculin gene, encoded by FLCN. The patient underwent laparoscopic partial nephrectomy and the lesion was diagnosed as renal cell carcinoma with oncocytic and chromophobe components. No recurrence was detected at a 9-month follow-up period. The patient’s written informed consent for publication was obtained.
Figure 1. a,b.
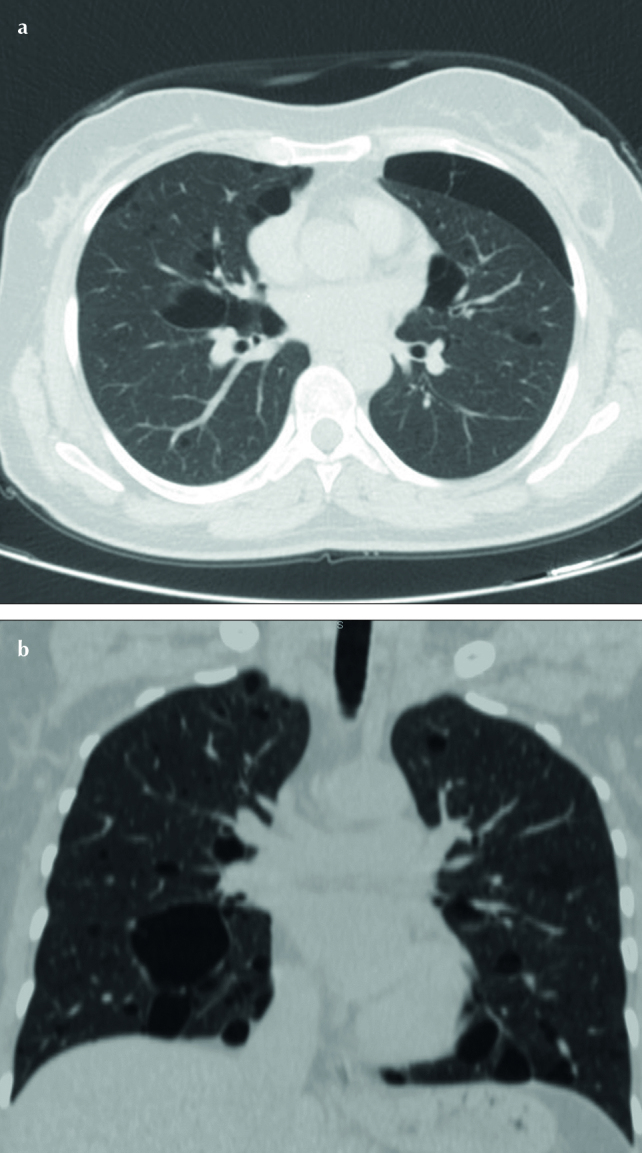
(a) Axial CT image of patient demonstrates a limited pneumothorax in the left lung, (b) coronal reformatted CT scan of patient shows bilateral, multiple thin walled cysts, especially in the lower lobes
Figure 2.
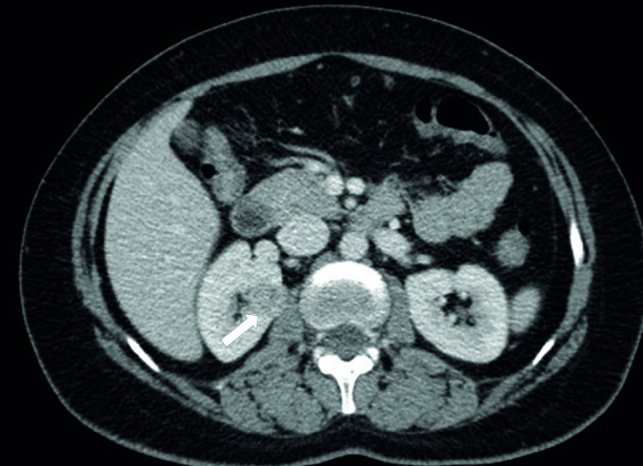
Abdominal CT shows a well-defined, hypodense mass (white arrows) in the upper pole of the right kidney
DISCUSSION
Birt-Hogg-Dube syndrome commonly presents with the clinical triad of skin lesions, pulmonary cysts with an increased risk of pneumothorax, and renal neoplasms. The syndrome is an autosomal dominant disorder arising from germline mutations in the folliculin (FLCN) gene. The FLCN gene is expressed in skin, nephrons, and type 1 pneumocytes. Its functions are not well-known, although it is reported as a tumor suppressor gene elsewhere [2,3]. Since it is a very rare disorder the diagnosis of BHD syndrome can frequently be delayed. The skin manifestations of BHD include fibrofolliculomas, trichodiscomas, and acrochordons. Renal findings can range from benign cysts to malignant tumors, and are often multiple and bilateral [1,3]. The risk of renal cancer is estimated to be seven times higher in patients with BHD syndrome and the prevalence of kidney lesions and lung cysts are about 34% and 84%, respectively [3]. Patients with BHD syndrome should be informed the increased incidence of kidney tumors and should be recommended yearly abdominal ultrasound or CT scan screening. Kunogi et al. [4] showed that none of the 21 patients in their study had skin or renal lesions. Therefore, BHD syndrome cannot be excluded simply because there are no kidney or skin lesions. Family history, bilateral, multiple lung cysts in the basal regions of the lung, and skin and renal lesions are typical for BHD syndrome, as in our patient.
Thyroid nodules, parotid oncocytoma, colonic polyposis, angiolipoma, parathyroid adenoma, flecked chorioretinopathy, neurothekeoma, meningioma, breast cancer, tonsil cancer, colorectal cancer, sarcoma, lung cancer, melanoma, basal cell carcinoma, and squamous cell carcinoma have been reported to be associated with BHD syndrome in case reports and case series [5–7]. However, these relations are not clear. Interestingly, a prolactin secreting pituitary adenoma was present in our case (Figure 3). To the best of our knowledge, there are no reports about an association between BHD syndrome and prolactin secreting pituitary adenoma in the literature yet. This association could be coincidental. Additional studies and reports that investigate this relationship is required.
Figure 3.
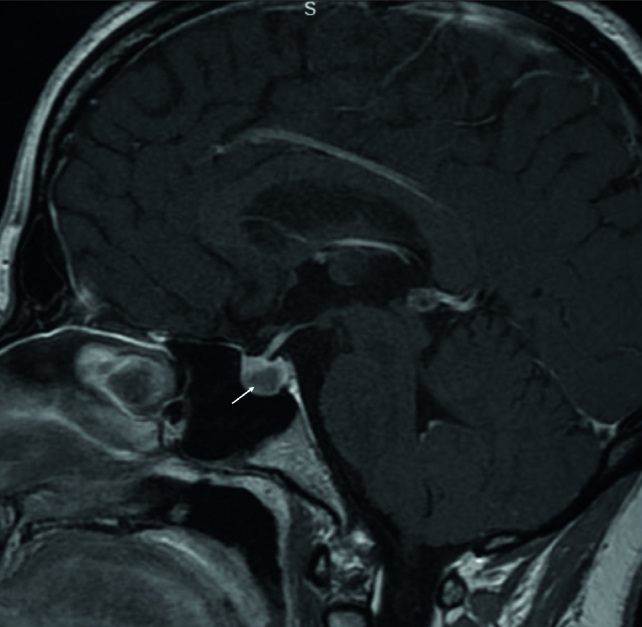
Sagittal post-gadolinium T1-weighted pituitary magnetic resonance image shows hypointense, well-defined pituitary adenoma (white arrow)
Spontaneous pneumothorax is a possible clinical manifestation of BHD syndrome, with a high risk of recurrence. The risk of pneumothorax is estimated to be 50 times higher in patients with BHD syndrome. First presentation of a BHD patient may be with spontaneous pneumothorax [4]. Cysts in BHD syndrome are usually well defined, thin walled, mainly oval and lentiform shaped, usually multiple and bilaterally located and distributed among the lower zone and subpleural regions, as in our case [1].
The differential diagnosis of multiple pulmonary cysts includes centrilobular emphysema, lymphangioleiomyomatosis, pulmonary Langerhans cell histiocytosis, lymphocytic interstitial pneumonitis, and neurofibromatosis type 1. Centrilobular emphysema occurs in upper lobes of smokers, and has no discernable walls. Lymphangioleiomyomatosis is characterized by multiple thin walled, multiple, round, well circumscribed cysts, which are distributed diffusely throughout the lungs in reproductive women. Langerhans cell histiocytosis may present with a combination of both nodules and bizarre shaped cysts, and it tends to spare lung bases and costophrenic angles. A few scattered perivascular lung cysts associated with ground-glass opacities, centrilobular nodules and septal thickening are seen in lymphocytic interstitial pneumonitis, which is usually related with other autoimmune and connective tissue diseases. Multiple lung cysts may also be seen in neurofibramatosis type 1, which has characteristic skin lesions [1,5,7]. BHD syndrome is a rare genetic disorder with an increased risk of renal tumors. The prompt and accurate diagnosis is necessary for appropriate management of patients and genetic counseling. Presence of recurrent pneumothorax in a patient with typical skin lesions should raise the suspicion of BHD syndrome, and CT of the chest and abdomen should be performed to rule out lung cysts and renal lesions. In addition, BHD syndrome and pituitary adenoma was evident in our case. Therefore, we think that BHD syndrome and pituitary adenoma may exist together. Additional studies and reports are needed to show this possible relationship.
Footnotes
Informed Consent: Written informed consent was obtained from the patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - E.K., H.G.Y., M.D.; Design - E.K., H.G.Y., M.D.; Supervision - F.U.; Resource - E.K., H.G.Y., M.D.; Materials - E.K., H.G.Y., M.D.; Data Collection and/or Processing - E.K., H.G.Y., M.D.; Analysis and/or Interpretation - F.U.; Literature Search - F.U.; Writing - E.K., F.U.; Critical Reviews - F.U.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Burkett A, Coffey N, Tomiak E, et al. Recurrent spontaneous pneumothoraces and bullous emphysema. A novel mutation causing Birt-Hogg-Dube syndrome. Respir Med Case Rep. 2016;19:106–8. doi: 10.1016/j.rmcr.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noppen M, De Keukeleire T. Pneumothorax. Respiration. 2008;76:121–7. doi: 10.1159/000135932. [DOI] [PubMed] [Google Scholar]
- 3.Toro JR, Wei MH, Glenn GM, et al. BHD mutations, clinical and molecular genetic investigations of Birt-Hogg-Dubé syndrome: a new series of 50 families and a review of published reports. J Med Genet. 2008;45:321–31. doi: 10.1136/jmg.2007.054304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunogi M, Akiyoshi T, Gunji Y, et al. Mutation analysis of the Birt-Hogg-Dubé gene in patients with multiple lung cysts. Am J Respir Crit Care Med. 2009;179:A4398. [Google Scholar]
- 5.Maffe A, Toschi B, Circo G, et al. Constitutional FLCN mutations in patients with suspected Birt-Hogg-Dube syndrome ascertained for non-cutaneous manifestations. Clin Genet. 2011;79:345–54. doi: 10.1111/j.1399-0004.2010.01480.x. [DOI] [PubMed] [Google Scholar]
- 6.Chung JY, Ramos-Caro FA, Beers B, et al. Multiple lipomas, angiolipomas, and parathyroid adenomas in a patient with Birt-Hogg-Dube syndrome. Int J Dermatol. 1996;35:365–7. doi: 10.1111/j.1365-4362.1996.tb03642.x. [DOI] [PubMed] [Google Scholar]
- 7.Gupta N, Sunwoo BY, Kotloff RM. Birt-Hogg-Dubé Syndrome. Clin Chest Med. 2016;37:475–86. doi: 10.1016/j.ccm.2016.04.010. [DOI] [PubMed] [Google Scholar]


