Abstract
BACKGROUND
Anthroponotic cutaneous leishmaniasis (ACL) has long been a significant public health problem in northeastern Iran. The objective of this study was to determine the efficacy of deltamethrin-impregnated vs. nonimpregnated bed nets (NIBs) and curtains (NICs) in ACL control.
PATIENTS
Deltamethrin-impregnated bed nets (IBs) and curtains (ICs) with 25 mg ai/m2were distributed among 160 households in one district and NIBs and NICs were distributed among the same number of households in another district. A third district with a similar numbers of households served as a control. Health education messages were disseminated to ensure the population’s complicance with the proper use of bed nets and curtains. Sticky paper traps were used to assess the effect of insecticide-impregnated bed nets and curtains on the density of Phlebotomus sergenti. Deltamethrin susceptibility and also bioassay tests were carried out on the species by WHO standard method. Case findings were done by house-to-house visits once a season and all the inhabitants of the selected households in each district were examined.
RESULTS
IBs and ICs provided good protection against sandfly bites and reduced the transmission of ACL in the intervention district, while NIBs and NICs provided no protection. There was no significant difference in monthly density of P. sergenti indoors and outdoors among the districts (P>0.05). This species was susceptible to deltamethrin in the field population in the area. Bioassays confirmed that the nets treated with deltamethrin remained effective for more than 3 months.
CONCLUSION
Personal protection is an effective and sustainable means of preventing and controlling ACL and can reduce dependence on insecticides. We encourage the use of IBs and ICs to control ACL in other high-risk areas of Iran and Afghanistan during the active season of sandflies.
Anthroponotic cutaneous leishmaniasis (ACL) is a serious health problem in the Middle East, especially in Iran, Syria, Turkey and Afghanistan.1 Thousands of cases occur in large cities and in small towns in Iran. The main foci have been identified as Mashhad, Tehran, Kerman, Bam, Shiraz, and Neishabour.2,3 Anthroponotic cutaneous leishmaniasis has been known to be endemic in Mashhad in northeastern Iran3 since 1935 and careful studies have been carried out on the epidemiology of the disease in the city during the last seven decades. In 2002, the increasing number of cases of ACL has been of concern to the health authorities in the city of Mashhad. The increase in cases could well be attributed to the drought in recent years, the movement of a large number of people from the villages around the city to Mashhad, construction of cheap buildings near the mountainous areas, the increase in the population and the increase in the densities of the vector population (Phlebotomus sergenti), and the disposal of nonhygienic garbages among other things. Over 12 million Muslims (the majority Iranians) travel to the city from all over the world, mainly during summer. Following the establishment of the Sarakhs Free Zone and the reopening of the Silk Road, economic developments have emerged in the area. All of these nonimmune visitors are exposed to the bite of infected sandflies during the active season.4
The success of pyrethroid insecticide bed nets trials in controlling malaria in several African5 and Asian countries1 has encouraged researchers to use the same technique to control ACL in Afghanistan,6 Iran (Bam),7 Syria8 and Turkey.9 The use of pyrethroid-impregnated bed nets in the conditions prevailing in Bam (in a restricted area), Iran, i.e., very hot days during the summer but rather good weather at night, decreased the number of cases but did not interrupt the transmission.7 The use of impregnated bed nets and curtains in endemic areas with a cooler climate in summer where people sleep in rooms at night has not been evaluated in our country yet. Therefore further studies need to be undertaken in places like Mashhad or other similar foci in Iran.
METHODS
Study area
The city of Mashhad (36° 57′ N, 60° 38′ E), elevation 985 meters, is situated between two chains of mountains: the Hezar Masjed (altitude 3200 m) in the northeast and Binalud (altitude 3615 m) in the west and southwest. The area has cold winters and rather warm summers. In 2003, the maximum and minimum mean monthly temperatures were 35.5 °C and −0.6 °C in July and December, respectively. The total annual rainfall was 276.3 millimeters. The minimum mean monthly relative humidity was 32% (July and August) and the maximum was 93% (January). Mashhad is the center of the mighty province of Khorassan Razavi and the most important pilgrimage center in Iran with a population of about 2500 000 and an area of 200 sq km2. It was named Mashhad due to the martyrdom of Hazrat-e-Reza (the eighth Shiite Imam) in 817 AD. His tomb became a major pilgrimage site. Mashhad is the second largest and crowded city in Iran and lots of people live in about 40 suburbs of the city.
The most infected part of the city is called the Aabo-Bargh area in the southwest, which is an old endemic focus in the city. This area includes 29 quarters with a population of 82 200. Cases of the disease are reported from all quarters with some having a high percentage of reported cases during 1999–2002. Treatment of cases with Glucantime (meglumine antimoniate) and sometimes with topical paramomycin ointment, a broad spectrum antibiotic, in health centers and clinics has intensified. The community is familiar with the disease by its local name (Salak). The parasite has been identified as Leishmania tropica. Humans are the main reservoir host but infected dogs have also been reported in the city. The vector is most probably Phlebotomus sergenti; natural infections have been observed but characterization of the parasite in the sandfly has not been achieved.3,10,11
Impregnation and distribution of bed nets and curtains
Three districts (Shaghayegh, Honar, and Vakilabad) were selected randomly in the Aab-o-Bargh area. In each district, 160 households near each other and with a similar prevalence of ACL (1.9–2.6% for active lesions and 24.5–30.5% for scars) were recruited for the study. According to our previous study in 2002, the incidence of the disease was similar in these districts: 30.3, 36.2 and 29.8 per thousand, respectively (Institute of Public Health Research, unpublished data). In addition, treatments were randomly performed in corresponding districts. All households enrolled in Shaghayegh received impregnated bed nets and curtains (IBs and ICs); Households in Honar received non-impregnated bed nets and curtains (NIBs and NICs) and Vakilabad was the control area.
White polyester bed nets and curtains (mesh size 156 holes/inch2, 25 holes/cm2, 75 denier) made by a factory in Tehran were impregnated with deltamelthrin SC 5% (K-Othrine); 25 mg ai/m2 following the method described by WHO, in 2002(25). After weighing the bed nets they were soaked and the extra water was squeezed out. Then the bed net was weighed again to check the quantity of water absorbed. Next, the total surface of the net was divided to find how much water was absorbed by one square meter of each type. After calculating the amount of the insecticide, the final solution was prepared in a big plastic basin. Water and insecticide were mixed thoroughly by a large glass rod. The net was put in an empty plastic basin and the insecticide solution was added gently, allowing the net to soak for several minutes while turning it constantly with a wooden stick. Then the net was lifted and wringed gently. After impregnation, the nets were laid on plastic sheets in the shade to partially dry. They were then hung on a wire in the shade for several hours to dry completely. The impregnated bed nets were then carefully wrapped in black nylon bags and labeled with the size (single, double and family size) and the date of impregnation. They were kept in a cool, dry storage place until the time of distribution.
The same method of impregnation (K-Othrine; 25 mg ai/m2) was used for curtain material. IBs (single, double and family size) and NIBs were distributed to all the selected households in the intervention area according to their needs in April 2003 and people were encouraged to use them from sunset to sunrise the next morning. The number of bed nets distributed to each household was proportionate to the size and structure of the family (Table 1). Windows of all houses in Shaghayegh were covered with ICs and windows of all houses in Honar were covered with NICs at the same time. ICs were hung at the doorways of houses in Shaghayegh and NICs were hung at the doorways of houses in Honar.
Table 1.
Amount, type and number of distributed curtains and bed nets, Aab-o-Bargh area, Mashhad, Iran, 2003.
| Settlements | Total population | Population of 160 households | Curtain (m2) | Bed nets types | Application type | ||
|---|---|---|---|---|---|---|---|
| Single | Double | Family | |||||
| Shaghayegh | 1355 | 621 | 1283.5 | 17 | 122 | 139 | IBs, ICs |
| Honar | 1029 | 609 | 866 | 17 | 147 | 107 | NIBs, NICs |
| Vakilabad | 3912 | 741 | - | - | - | - | Control |
| Total | 6296 | 1971 | 2149.5 | 34 | 269 | 246 | - |
IBs: impregnated bed nets, ICs: impregnated curtains, NIBs: non-impregnated bed nets, NICs: non-impregnated curtains
Health education
Health education messages were relayed to the study population in the intervention districts (Shaghayegh and Honar) to encourage the use of bed nets and curtains. The role of sand flies in transmission of the diseases was explained to people on several occasions face-to-face (women and men) and in focus groups (women) during distribution of bed nets and curtains. The staff drew attention to the importance of using bed nets and hanging the curtains on the doorways when sleeping to protect themselves and their children from leishmaniasis. Schools were visited and teachers were urged to educate their students on the importance of using bed nets and curtains to protect themselves from sandfly bites. Seven to 10 households were checked at random during the night each week by two staff members to ensure that the bed nets and curtains were used. No intervention was done in the district of Vakilabad, as the control area.
Entomological surveillance
Three houses were chosen in each district and sandflies were collected biweekly from ten fixed sites in each house (bedrooms, storerooms, toilets) using 30 sticky traps (castor oil coated white papers 20×35 cm) from the beginning (April) to the end (November) of the active season. The same number of sticky traps were also used for collection of sandflies from outdoors (courtyards). Sticky traps were placed before sunset and collected on the following morning, before sunrise. The sandfly species were determined by professional entomologists.
The susceptibility of P sergenti to 0.025% deltamethrin was studied in field surveys, following the WHO standard methods. Sandflies were collected from indoors by aspirator in Honar (NIBs and NICs) and Vakilabad (control) and were transferred to the laboratory at Mashhad Health Center. Testing was carried out there, free from any insecticidal contamination. The treated sandflies were held between 23°C and 26°C, and a relative humidity about 75%. The area was sprayed with lambdacyhalothrin (tradename, Icon) (10% WP) at a rate of 50 mg/m2, with one round in June 2000. Bioassay tests were conducted in July, August and September 2003, 3, 8 and 12 weeks after impregnation of bed nets, respectively, on fed females of P. sergenti adults collected from Honar (NIBs + NICs) and Vakilabad (control), by the WHO standard method.13
Studies on human infection
A census was taken on all 480 households (160 in each district) with data collected from one of the parents of the household for all household residents including age and sex, relationship to household head, past and present history of ACL and details of any current lesions (number, date and place of acquisition). In each case with active lesions, smears were prepared, fixed by methanol and then examined later in Tehran, after staining with Giemsa. The results of microscopic examinations of active lesions were recorded on the related forms.
Case finding was done by house-to-house visits once every season during the last weeks of June, September, December 2003 and March and June 2004, and all the inhabitants of the selected households were examined in each district. Only new cases of ACL, i.e., the number of patients with new lesions were recorded on each visit. Yearly incidence of the disease was determined separately in each district during July 2003 to July 2004, because of the long incubation period of ACL. Cases found during April to the end of June 2003 were excluded. Persons with scars were also excluded when the yearly incidence of the disease was calculated. Inclusion criteria were persons with active lesions.
Statistical analysis
The data were entered in SPSS 5 and analysed using SPSS 11.5 and STATA 8.0. Graphs were prepared in Excel. A one-sided Fisher’s exact test was used to compare the incidence rate of ACL in each district for two consecutive years. The same test was also used to compare the incidence rate between Shaghayegh (IBs, ICs) and Vakilabad (control), Shaghayegh and Honar (NIBs, NICs), and Honar and Vakilabad. The Kruskal-Wallis test was used to compare the density of P sergenti indoors and outdoors in each intervention district compared with the control area. A P<0.05 was considered statistically significant.
RESULTS
Comparison of incidence rates of ACL in each district before and after intervention showed a significant difference in the district of Shaghayegh (Table 2) where the IBs and ICs were used. However, in the district of Honar, despite use of NIBs and NICs, non-significant differences were observed versus the incidence in 2002. Similarly, there were no significant differences in incidence in the control area before and after intervention. Significant differences were also observed in incidence rates of the disease between the district of Shaghayegh (IBs, ICs) and Vakilabad (control) and between Shaghayegh and Honar (NIBs, NICs) during June 2003 to June 2004 (Table 2). Non-significant differences were observed between Honar and Vakilabad.
Table 2.
Comparison of incidence (per thousands) of anthroponotic cutaneous leishmaniasis in the intervention and control areas, Mashhad, Iran, June 2003 to June 2004.
| Area | District | Bed net and curtain type | Population | Number with active lesion | Incidence 2004 | Incidence 2002 (before intervention) |
|---|---|---|---|---|---|---|
| Intervention | Shaghayegh | IBs, ICs | 580 | 2 | 6.9* | 30.3† |
| Honar | NIBs, NICs | 569 | 11 | 30.6 | 36.2 | |
| Control | Vakilabad | - | 699 | 18 | 28.6 | 29.8 |
P=0.025 vs. Vakilabad, P=0.028 vs. Honar;
P=0.015 vs. incidence in 2004
The most highly infected age group was ≥25 years with a rate of 33.3% in the control area (Table 3). The ulcer rate was 22.2% for individuals under 10 years of age in the control area. Treatment was provided for the 32 subjects with a parasitological diagnosis of leishmaniasis. In the district of Shaghayegh, 1.5% of the households had washed the bed nets, 87.3% of the households used the bed nets regularly and 69.4% of the households put up the bed nets at sleeping time (10:00–12:00 PM). Only 7.4% put them up at sunset; 71.6% of the households used the bed nets in rooms while 20.1% used them in the courtyards and 98.5% of the households kept the bed nets in the room during the day. About 88% of the inhabitants knew the breeding places of sandflies and method of transmission of the disease to humans. In the district of Honar, 92% of the households used the bed nets regularly and 80% of the households put up the bed nets at sleeping time (10:00–12:00 PM), but 8% put them up at sunset; 80% of the households used the bed nets in rooms while 14% used them in the courtyards and 99.2% of the households kept the bed nets in rooms during the day. Almost 91% of the inhabitants knew the breeding places of sandflies and method of transmission of the disease to humans.
Table 3.
Age distribution of ulcers in intervention and control areas during the study period, Mashhad, Iran June 2003 to June 2004.
| Age (years) | Shaghayegh | Honar | Vakilabad (control) | |||
|---|---|---|---|---|---|---|
| n | n | n | ||||
| 0–4 | 0 | 0 | 1 | 9.1 | 2 | 11.1 |
| 5–9 | 2 | 100 | 2 | 18.2 | 2 | 11.1 |
| 10–14 | 0 | 0 | 0 | 0 | 3 | 16.7 |
| 15–19 | 0 | 0 | 1 | 9.1 | 1 | 5.6 |
| 20–24 | 0 | 0 | 2 | 18.2 | 4 | 22.2 |
| ≥25 | 0 | 0 | 5 | 45.4 | 6 | 33.3 |
| All ages | 2 | 100 | 11 | 100 | 18 | 100 |
Values are percent of total cases.
Density of sandflies
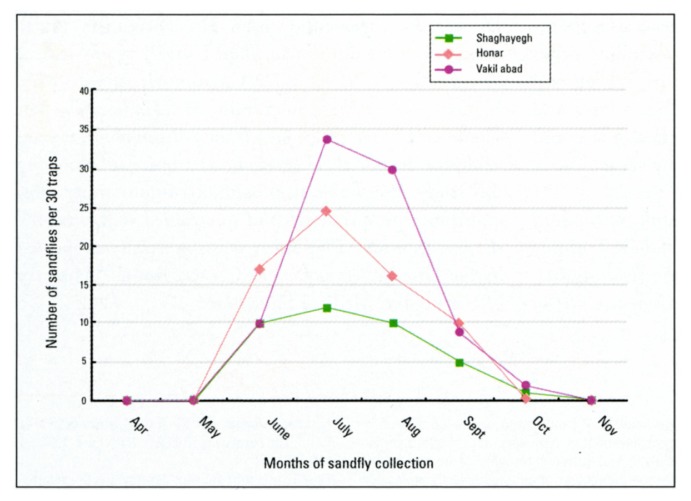
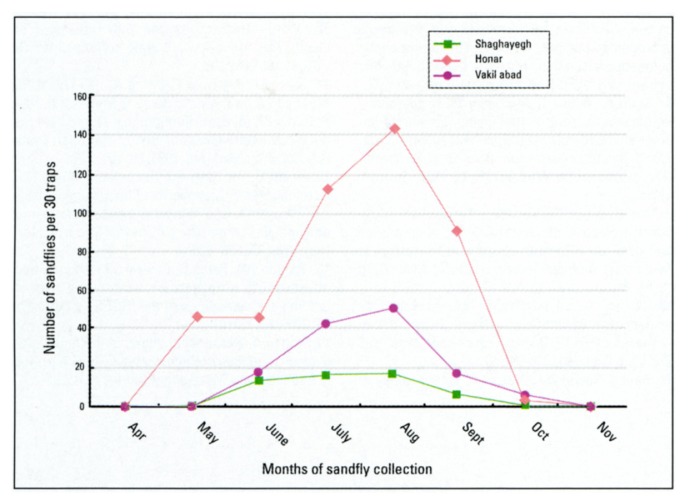
During April to November 2003, 1531 adult sandflies (1160 from outdoors and 371 from indoor resting places) were collected and identified. The following four species were found in bedrooms, warehouses and privacies: P. sergenti (93%), P. papatasi (4.8%), P. caucasicus (1.1%), and S. sintoni (1.1%). Outdoors (in courtyards), P. sergenti (95.9%), P. papatasi (1.8%), P. caucasicus (1.4%) and S. sintoni (0.9%) were collected. The most common sandfly of indoor and outdoor resting places was P. sergenti. This species appeared in April or May and disappeared in November. There was one peak in the density curve of P. sergenti outdoors and indoors in July or August (Figures 1, 2), although differences between months were non-significant by the Kruskal-Wallis test. In general, there was no significant difference in monthly density of P. sergenti in indoors and outdoors among the villages. No sandfly was found in the area during November to March due to cold weather.
Figure 1.
Monthly density of P. sergenti in the Shaghayegh (deltamethrin-impregnated bed nets and curtains), Honar (non-impregnated bed nets and curtains), and Vakilabad (control) districts (indoors), Mashhad, Iran 2003.
Figure 2.
Monthly density of P. sergenti in the Shaghayegh (deltamethrin-impregnated bed nets and curtains), Honar (non-impregnated bed nets and curtains), and Vakilabad (control) districts (outdoors), Mashhad, Iran 2003.
Susceptibility tests and bioassays
Sixteen series of susceptibility tests were carried out on 309 fed P. sergenti. The mortality rates for 0.025% deltamethrin after 2, 4, 7.5, 15, 30 and 60 minutes of exposure time followed by 24 hours of recovery time were 100%. We concluded that P. sergenti is susceptible to deltamethrin in the field population in this area. The mortality of P. sergenti (wild-caught, fed females) was 100% until the end of week 12 (Table 4). It was impossible to continue this study from week 12 onwards because of the decrease in the density of P. sergenti due to rains and cold weather in the area.
Table 4.
Results of the bioassays showing percentage mortality of wild-caught P. sergenti females after 3 minutes contact and 24 hour-observation with bed nets treated with 25 mg ai/m2 deltamethrin, Mashhad, Iran 2003.
| Weeks after impregnation | Temperature (min–max, °C) | % relative humidity | % mortality after 24 hours | Control |
|---|---|---|---|---|
| 3 | 22–29 | 75 | 100 (38) | 0 (28) |
| 8 | 24–30 | 76 | 100 (52) | 0 (22) |
| 12 | 22–28 | 76 | 100 (50) | 0 (28) |
Figures in parenthesis are number of sandflies tested.
DISCUSSION
This is the first report from Iran on the effectiveness of deltamethrin-impregnated bed nets and curtains to prevent ACL in an endemic area with a cool climate in summer where people sleep in rooms at night. Previous studies on the control of ACL were carried out in Syria, Afghanistan, Iran (Bam in a restricted area, very hot days during summer) and Turkey.8,6,7,9 Our evaluation shows that the use of both deltamethrin-impregnated bed nets and curtains can provide good personal protection from the bites of sandflies and subsequently reduce the transmission of ACL, but NIBs and NICs do not provide any protection against the disease. It should be mentioned that around 7% of the households in each district were lost during part of the follow up visits, but as this phenomenon occurred in all districts it does not affect the comparative results. The results of this study support the conduct of large-scale field trials in an epidemiologically similar area of Iran and also neighbouring countries.
Although there was a reduction in the density of P. sergenti indoors and outdoors in the intervention areas compared with the control area (Figure 1, 2), the Kruskal-Wallis test showed non-significant differences among different months. Phlebotomus sergenti is common both in houses and out of doors in the Aab-o-Bargh area, which is located close to the mountains. The species is mostly found in wild form and resting places include caves, crevices, under rocks, bird holes and similar places. Presumably, the sandflies feed on hosts other than humans, which would explain why sandfly populations, particularly those outdoors, do not seem to have been reduced. There was also no strong evidence in similar studies15,14,7,9,8 that the use of pyrethroid-impregnated bed nets had an impact on reducing the mean total density of P. papatasi or P. sergenti between intervention areas compared with the control areas. However, dead insects, including sandflies, were found in the morning on and around the treated bed nets during survey team visits to households in the intervention settlements.
We observed no side effects of the pyrethroid impregnated bed nets and curtains and none was reported among the interviews during the follow-up study. It was impossible to continue bioassay tests in October and onwards in the field surveys due to the cold weather, but susceptibility tests and bioassays showed that P. sergenti was perfectly susceptible to deltamethrin and the bed nets and curtains treated with this insecticide remained effective for 3 months and more. In a trial for controlling cutaneous leishmaniasis vectors in Colombia, the effectiveness of lambdacyhalothrin on bed nets persisted for 4 months.16
The low cost and simplicity of impregnated bed nets and curtains (approximately US $5.5 for a bed net, plus 25 cents per impregnation) means that their use could be sustainable in the study area of Iran and elsewhere, given that local people recognize the nuisance and dangers of sandflies and other biting flies, and are amenable to the use of treated nets. In addition to local sustainability, impregnated bed nets and curtains have the advantage of being portable and they require no specialized equipment or trained personnel.
Although, this method reduced significantly the transmission of the disease in the study area, transmission will continue rapidly as before6 after cessation of use. In this study, most of inhabitants accepted the impregnated bed nets, but 80% put them up when they went to sleep (10.00 to 12.00 p.m.), whereas Nadim reported in 1972 that maximum sandfly activity, especially at the end of the active season, occurs in the first three hours of the night.17 Therefore, people received infective bites before going under the bed nets.
At the present time, in the absence of a suitable vaccine, personal protection by impregnated bed nets and curtains are an effective and suitable means of preventing and controlling ACL. We feel that the results of this trial justify the more widespread use of impregnated bed nets and curtains in controlling other similar foci such as the northern part of Tehran and Neishabur (Iran) and the cities of Kabul, Herat and Kandahar (Afghanistan) because their climatic and other environmental conditions are the same.
Acknowledgements
Authors wish to extend their sincere thanks to the staff of the leishmaniasis laboratory at the Isfahan Training and Health Research Center during the field studies. The authors are also indebted to Dr. Gooya, Chief of Disease Management Center, Dr. Parizadeh, under Secretary of Health in Mashhad University of Medical Sciences, Dr. Mojtabavi, Dr. Gazani, Mr. Sanati, Mrs. Boozarjomehri, Mrs. Sohailinia, Mr. Hadizadeh, Mr. Yazdi and other colleagues from Mashhad provincial health center for their excellent assistance in achieving this study. We thank all inhabitants in our study communities who answered and questioned and accepted the intervention. This study was financially supported by the Disease Management Center, Iranian Ministry of Health and Medical Education.
REFERENCES
- 1.Laison R, Shaw JJ. Evolution, classification and geographical distribution. In: Peters W, Killick-Kendrick R, editors. In the Leishmaniasis in Biology and Medicine. Vol. 1. Academic Press; London: 1986. pp. 1–120. [Google Scholar]
- 2.Nadim A, Javadian E, Seyedi-Rashti MA. Epidemiology of leishmaniasis in Iran. In: Ardehali S, et al., editors. Leishmania parasites and leishmaniasis. second edition. Iran University Press; 1994. pp. 176–208. (In Farsi) [Google Scholar]
- 3.Nadim A, Seyedi-Rashti MA, Faghih MA. Epidemiology of cutaneous leishmaniasis in Iran: B. Khorassan. Part III: Human infection. Bull Soc Path Exot. 1969;62:702–710. [PubMed] [Google Scholar]
- 4.Yaghoobi-Ershadi MR, Akhavan AA, Zahraei-Ramazani AR, Abai MR, Ebrahimi B, Vafaei-Nezhad R, Hanafi-Bojd AA, Jafari R. Epidemiological study in a new focus of cutaneous leishmaniasis in the Islamic Republic of Iran. EMHJ. 2003;9:816–826. [PubMed] [Google Scholar]
- 5.Alonso PL, Lindsay SW, Armstrong Schellenberg JRM, Keita K, Gomez P, Shenton FC, Hill AG, David PH, Fegan G, Greenwood BM. A malaria control trial using insecticide-treated bed nets and targeted chemoprophylaxis in a rural area of the Gambia, West Africa. Trans Roy Soc Trop Med Hyg. 1993;87(Supp 2):37–44. doi: 10.1016/0035-9203(93)90174-o. [DOI] [PubMed] [Google Scholar]
- 6.Reyburn H, Ashford R, Mohsen M, Hewitt S, Rowland M. A randomized controlled trial of insecticide-treated bed nets and chadors or top sheets, and residual spraying of interior rooms for the prevention of cutaneous leishmaniasis in Kabul, Afghanistan. Trans Roy Soc Trop Med Hyg. 2000;94:361–366. doi: 10.1016/s0035-9203(00)90104-4. [DOI] [PubMed] [Google Scholar]
- 7.Nadim A, Motabar M, Houshmand B, Keyghobadi K, Aflatonian MR. WHO/LEISH/95. Vol. 37. Geneva: 1995. Evaluation of Pyrethroid impregnated bed nets for control of anthroponotic cutaneous leishmaniasis in Bam (Islamic Republic of Iran) p. 21. [Google Scholar]
- 8.Tayeh A, Jalouk L, Al-Khiami M. WHO/LEISH/97. World Health Organization, Division of Control of Tropical Diseases; Geneva: 1997. A cutaneous leishmaniasis control trial using pyrethroid-impregnated bed nets in villages near Aleppo, Syria; p. 41. [Google Scholar]
- 9.Alten B, Caglar SS, Kayans S, Simsek M. Evaluation of protective efficacy of K-O-TAB impregnated bed nets for cutaneous leishmaniasis control in South-east Anatolia-Turkey. J Vector Ecol. 2003;28:53–64. [PubMed] [Google Scholar]
- 10.Nadim A, Seyedi-Rashti MA, Mesghali A. Epidemiology of cutaneous leishmanisis in Iran. B. Khorassan Part IV. Distribution of sand flies. Bull Soc Path Exot. 1971;64:865–870. [PubMed] [Google Scholar]
- 11.Seyedi-Rashti MA, Nadim A. Epidemiology of cutaneous leishmanisis in Iran. B. Khorassan area Part I: The reservoirs. Bull Soc Path Exot. 1967;60:510–518. [PubMed] [Google Scholar]
- 12.WHO. Instructions for determining the susceptibility or resistance of adult black flies, sand flies and biting midges to insecticides, unpublished W.H.O. document. WHO/VBC/81. 1981;810:1–6. [Google Scholar]
- 13.WHO. Instructions for the Bio-assay of insecticidal deposits on wall surfaces. WHO/VBC/81. 1981;812:1–6. [Google Scholar]
- 14.Stich AH, Maxwell CA, Haji A, Haji Daudi M, Machano Ame Y, Mussa Juma K, Metteelli A, Haji H, Curtis CF. Insecticide-impregnated bed nets reduce malaria transmission in rural Zanzibar. Trans Roy Soc Trop Med Hyg. 1994;88:150–154. doi: 10.1016/0035-9203(94)90271-2. [DOI] [PubMed] [Google Scholar]
- 15.Dolan G, Ter Kuile FO, Jacoutot V, White NJ, Luxemburger C, Malankirii L, Chonogsuphajaisiddhi T, Nosten F. Bed nets for prevention of malaria and anemia in pregnancy. Trans Roy Soc Trop Med Hyg. 1993;87:620–626. doi: 10.1016/0035-9203(93)90262-o. [DOI] [PubMed] [Google Scholar]
- 16.Parado RH, Ferro C, Davies CR. Efficacy and effectiveness of insecticide treated bed nets in Colombia. Proceedings of the ISOPS-V; April 17–21 2005; pp. 73–74. [Google Scholar]
- 17.Nadim A. Seasonal changes of the hourly activity of sand flies of Rhombomys opimus burrows in Isfahan, Iran. Trop Geogr Med. 1972;24:382–384. [PubMed] [Google Scholar]