Pachygyria is a neuronal migration disorder characterized by reduced and broad cerebral gyri.1 The regions of the brain with pachygyria have an abnormally thick cortex that lacks normal folding and has deficient layering. The role of inheritance has been speculated in its causation, but no definite genetic locus has been identified.2,3 The clinical manifestations of pachygyria range from marked hypotonia to frank seizure. Several etiological factors have been described, including cytomegalovirus infection, prenatal cocaine exposure, metabolic disorder and syndromic forms.4–9 However, an extensive literature search showed no previous report on an association of pachygyria with Down syndrome/trisomy 21.
CASE
The baby boy was the second of twins, delivered by cesarean section secondary to breech presentation. The first twin was delivered vaginally. The gestational age was 285/7 weeks. The mother was a 19-year-old woman, gravida 3, para 0111. Antenatal ultrasonography confirmed the twin gestation with anterior placentas and two sacs (dizygotic, dichorionic). The serology for hepatitis, syphilis and HIV were negative. She was rubella immune and denied use of any illicit drugs. She was tocolyzed with magnesium sulfate. Two doses of betamethasones were given and she also received erythromycin and ampicillin prior to delivery. The labor was uneventful. The baby cried soon after birth. The Apgar score was 7 and 9 at one and five minutes, respectively. Birth weight was 1315 grams, length was 35 cm and head circumference was 28 cm, all appropriate for gestational age.
Physical examination showed a hypotonic baby with upslanting eyes, simian creases and flat facies. The chest was clear with a soft systolic murmur. The abdomen was soft and no other deformity was noted. Initial investigation showed normal blood cell counts and electrolytes. Further investigations, including the cytogenetic studies, showed a karyotype of 47, XY, + 21. The echocardiogram revealed small patent ductus arteriosus and the renal ultrasound was normal. On day 38 of life (sixth week chronological age or 35 weeks postmenstrual age /corrected age) some athetoid movements were noted in addition to the previously observed hypotonia. After neurology consultation, a magnetic resonance imaging (MRI) was obtained that showed generalized pachygyria with no evidence of a basal ganglia lesion or midline defects (Figures 1–3). The electroencephalogram (EEG) showed low voltage activity of 2–3 Hz with no epileptic activity.
Figure 1.
MRI of the brain, coronal image.
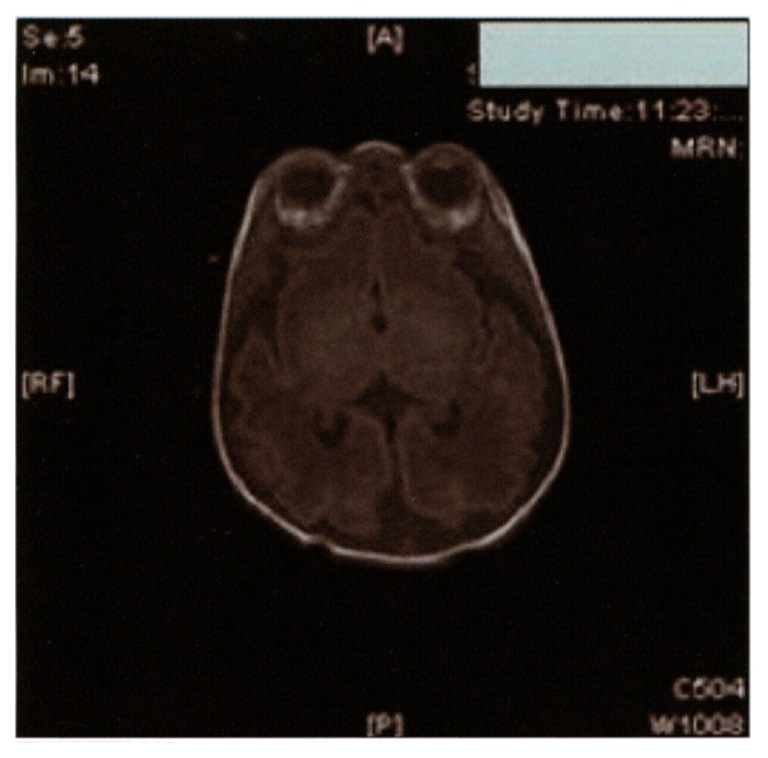
Figure 2.
MRI brain, axial image.
Figure 3.
MRI brain, sagittal image.
The baby remained on minimal supplemental oxygen until day 26 of life and was then weaned to room air. The baby was stable on mostly oral feeding and gaining weight. The head circumference was 32 cm. The eye examination showed a mature retina and the baby passed the hearing test.
DISCUSSION
The MRI of a premature neonate reflects their stage of CNS development.10 An MRI obtained at 24 weeks will be similar for that of a lissencephalic full-term infant and that of a 28–32 week premature neonate will look like a full term with pachygyria. Thus, it could be arguable that the pachygyria observed in the case could just be due to the prematurity. In fact, the MRI in the case was done at the postnatal age of 38 days (at about 35 weeks postmenstrual age) suggesting that pachygyria may not be just a reflection of a very premature brain.
The brains of children with Down syndrome have been shown to be of smaller volume, but no definite neuronal defect was found.12 The exact etiology for the neurological involvement including hypotonia and mental retardation associated with Down syndrome remains a mystery. Thus it will be interesting to find out if the association observed is coincidental or there is some common underlying genetic basis. Although the case presented above was a twin exposed to same prenatal and maternal conditions, a completely different genetic makeup may explain the dizygosity with occurrence of the trisomy 21 in one. We did not perform the brain MRI on the other twin, as by the time we discovered pachygyria he was discharged from the hospital.
The exact pathology for hypotonia and neurological symptoms in a patient with Down syndrome is not well understood and these symptoms usually never get investigated as compared to central nervous system symptoms noted otherwise. Thus, this case report might be used as an example in looking further into the CNS lesions and structural pathology in Down syndrome. MRI of brain has been described as an excellent diagnostic tool for brain pathology.11 Thus, in light of the association observed in our case, we recommend routine use of MRI of the brain in all Down syndrome neonates so that more can be known about the association between structural brain lesions and the CNS symptomatology frequently observed in infants with trisomy 21. In addition, cytogenetic studies should be done to look at the genetic basis of this interesting observation.
Acknowledgment
We would like to thank the staff at John Stroger Hospital, Chicago involved in taking care of the infant and would like to extend our special gratitude to the radiology department for its help in providing the images.
REFERENCES
- 1.Volpe JJ. Neurology of the Newborn. 4th edition. Chapter 2. W B Saunders Company; Philadelphia: 2001. pp. 45–99. [Google Scholar]
- 2.Al-Qudah AA. Clinical patterns of neuronal migrational disorders and parental consanguinity. J Trop Pediatr. 1998;44:351–4. doi: 10.1093/tropej/44.6.351. [DOI] [PubMed] [Google Scholar]
- 3.Ramirez D, Lammer EJ, Johnson CB, Peterson CD. Autosomal recessive frontotemperal pachygyria. Am J Med Genet A. 2004;124:231–4. doi: 10.1002/ajmg.a.20388. [DOI] [PubMed] [Google Scholar]
- 4.Malm G, Grondahl EH, Lewensohn-Fuchs I. Congenital cytomegalovirus infection: a retrospective diagnosis in a child with pachygyria. Pediatr Neurol. 2000;22:407–8. doi: 10.1016/s0887-8994(00)00126-0. [DOI] [PubMed] [Google Scholar]
- 5.Gomez-Anson B, Ramsey RG. Pachygyria in a neonate with prenatal cocaine exposure: MR features. J Comput Assist Tomogr. 1994;18:637–9. doi: 10.1097/00004728-199407000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Levin ML, Lupski JR, Carpenter RJ, Jr, Gerson LP, Greenberg F. An additional case of pachygyria, joint contractures and facial abnormalities. Clin Dysmorphol. 2:365–8. 993. [PubMed] [Google Scholar]
- 7.Takano T, Aotani H, Takeuchi Y. Asymmetric arthrogryposis multiplex with focal pachygyria. Pediatr Neurol. 2001;25:247–9. doi: 10.1016/s0887-8994(01)00293-4. [DOI] [PubMed] [Google Scholar]
- 8.Retcher JM, Bye AM, Nayanar V, Wilcken B. Non-ketotic hyperglycenemia presenting as pachygyria. J Inherit Metab Dis. 1995;18:665–8. doi: 10.1007/BF02436754. [DOI] [PubMed] [Google Scholar]
- 9.Kieslich M, Fuchs S, Vlaho S, Masich U, Boehles H. Midline developmental anomalies in Down syndrome. J Child Neurol. 2002;17:460–2. doi: 10.1177/088307380201700614. [DOI] [PubMed] [Google Scholar]
- 10.Girard N, Raybaud C, Poncet M. In vivo MR study of brain maturation in normal fetuses. Am J Neuroradiol. 1995;16:407–13. [PMC free article] [PubMed] [Google Scholar]
- 11.Pinter JD, Eliez S, Schmitt JE, Capone GT, Reiss AL. Neuroanatomy of Down’s syndrome: a high resolution MRI study. Am J Psychiatry. 2001;158:1659–65. doi: 10.1176/appi.ajp.158.10.1659. [DOI] [PubMed] [Google Scholar]
- 12.Osborn RE, Byrd SE, Naidich TP, Bohan TP, Friedman H. MR imaging of neuronal migration disorders. Am J Neuroradiol. 1988;9:1101–6. [PMC free article] [PubMed] [Google Scholar]