Abstract
Background
In Inner Mongolia of China, traditional Mongolian medicine (TMM), traditional Chinese medicine (TCM), and western medicine (WM) are all supported by the government. This study compares the background and performance of these three types of medicines.
Methods
The World Health Organization's Six Building Blocks framework was used for the system review. Data were collected from literature review and key informant interviews. A cross-sectional survey was conducted in three types of hospitals at the provincial, municipal (city), and prefectural (county) levels from April to August, 2016. Eight hospitals were included and, within each one, patients from four outpatient departments were selected. A total of 1,322 patients were interviewed about their expectations and perceptions of the health service.
Results
Government support for TMM includes higher budget allocation and a higher reimbursement rate. TMM is preferred by Mongolian people, those living in pasturing areas, and those seeking treatment for musculoskeletal problems/injuries. Patients attending TMM hospitals had the highest expectations and perceptions of the health service in general. However, human resources and research capacity of TMM are relatively limited.
Conclusion
To further enhance the role of the popular TMM for local minority's health, human resources and research capacity strengthening are essential.
1. Introduction
China is a multiethnic country, containing no fewer than 56 ethnic minority groups. Inner Mongolia Autonomous Region, which is the most important settlement of Mongolian people in China, was the first established minority autonomous region of China. There are approximately 24 million people living in Inner Mongolia hosting 49 minority groups, the majority of which is the Mongol ethnicity.
Traditional medicine is an indigenous medicine that is used to maintain health and to prevent, diagnose, and treat physical and mental illnesses [1]. Traditional Chinese medicine (TCM) has been widely used in China for the past 3,000 years [2]. In Inner Mongolia, traditional Mongolian medicine (TMM) has been recognized as an important part of the healthcare system. It is a systematic theoretical system and has abundant resources of medicaments and special therapies [3]. It is an important component of the Chinese national medicine system and contributes a significant part to the wealth of world traditional medicine [4]. The three types of medicine are distributed uniformly across the province.
Research on TMM has mostly been confined to basic science and development of TMM products. Seldom research considered to review and describe the TMM health system, as well as evaluate the performance of health systems from the patient's perspective. In order to gain a better understanding of TMM, this study examined the national and Inner Mongolia health system in relation to TMM and evaluated the health system performance by patient survey. This will broaden consideration of TMM stakeholders to health system aspects. The objectives of this study are to review the health system related to TMM and to evaluate the health system's performance on the basis of patients' expectations and perceptions on the service they received from TMM hospitals compared with TCM and WM hospitals. The study was divided into two parts: a system review and a hospital-based patient survey.
2. Methodology
2.1. System Review
We based our review on the World Health Organization (WHO) six building blocks framework [5] which consists of (i) service delivery; (ii) health workforce; (iii) information; (iv) medical products and technologies; (v) financing and sustainability; and (vi) leadership and governance. These blocks of TMM were compared with those of TCM and WM. We also considered process elements (access, coverage, quality, and safety) and outcomes (improved health and health equity, responsiveness, social and financial risk protection, and improved efficiency).
In the literature review keyword search terms included “traditional Mongolian medicine”, “traditional Mongolian medicine health system”, or “traditional Mongolian medicine and traditional Chinese medicine”. Source of information included domestic and foreign papers, books, meeting reports, dissertations, publicly accessible government data, and national statistics. We also made use of data based on the health workforce and financial investments [6].
With a well-prepared guideline in Supplementary Materials (available here), we conducted in-depth interviews with key informants, including policy makers, presidents of the schools, and doctors and managers of TMM hospitals, to collect their perception of the TMM health system. Interviews were conducted by the principal investigator and two well-trained research assistants.
The decentralized information obtained by literature review and key informants interview was classified by using MAXqda.11 software and summarized by using the six building blocks framework. The comparison of six aspects across different types of medicine was shown in a concentrated table and description. The results were discussed under the evidence provided by patient survey.
2.2. Patient Survey
A cross-sectional survey was conducted in two cities: (1) Hohhot: the capital of Inner Mongolia, and (2) Baotou: a major industrial city. These two cities were chosen because they got enough number of hospitals and patients to allow our detailed comparison. Eight hospitals, four from Hohhot and four from Baotou, were chosen for the survey, including four TMM hospitals, two TCM hospitals, and two WM hospitals. We overselected TMM hospitals as TMM is the focus of this study. We selected hospitals from high (provincial) level to low (county) level to improve the generalizability of our results, to facilitate comparison between hospitals of different levels, and to achieve the required sample size in a timely fashion. Therefore among the TMM hospitals, one provincial level, one city-level, and two county-level hospitals were selected. The WM hospitals were all at the provincial level while, among the two selected TCM hospitals, one was a provincial level and one a city-level hospital.
For comparability across hospitals and to obtain a broad group of clients, in each selected hospital we sampled patients from four major departments, namely, the departments of gynecology, pediatrics, and orthopedics and cardiovascular department. All outpatients who were able to communicate, read, and write in either Chinese or Mongolian were eligible for the study. Exclusion criteria were cognitive or memory dysfunction, or severe mental illness, such as schizophrenia and serious depressive disorders.
We devised the questionnaire collecting data on socioeconomic characteristics and disease-related information. The part measuring patient's expectations and perceptions was adopted from a revised Chinese version of the SERVQUAL model [7] shown in Supplementary Materials, which has been well validated and widely used in China. In brief, this model assesses clients' evaluation based on the difference between their expectation and perception on health service. It consists of two parts, the patients were first asked about their expectations and then asked to state their perceptions. Both parts share the same set of 28 statements covering seven domains: tangibles, reliability, trust, responsiveness, humanized service, effectiveness, and economy. The level of patients' agreement with each statement is rated on a scale ranging from 1 (least agree) to 9 (most agree).
Patient interviews, using the above questionnaire, took place between April and August 2016 by 12 third-year medical students who were specially trained and employed as research assistants. The venue was the hall where the patients were waiting to pay or to have further tests. Eligible subjects were identified and approached by the nurses who explained the aims of the study and consent was requested from the patients if they were older than 18 years or from their parents/guardians otherwise. Interviews, each lasting approximately 30 minutes, took place in a quiet and private location near the waiting area.
The sample size was calculated using the comparison of two means formula as follows [8, 9]:
| (1) |
Using a type I error of 5% and a power of 80% to detect a difference in mean gap scores of 0.06 between two groups of patients and a standard deviation of 0.06 from a previous study [10], 35 patients were required in each hospital department. A design effect of 1.2 was used in order to compensate for similarity of the outcome variable within patients of the same hospital. Finally, the study included 1,344 patients as research. Finally, 1322 questionnaires are valid.
Data were double-entered in Epidata version 3.1 and analysed using R version 3.1.2 [11]. Patients' background information was summarized using descriptive statistics. The scores were analysed in two aspects: (1) expectation scores were subtracted from perception scores of the same individual yielding a gap score, (2) comparisons of expectation, perception, and gap scores across different types of medicine and different levels of hospitals were conducted. Boxplots were used to display the results. Analysis of variance was used to test differences in service quality across groups. The relationships between the patient's expectation, perception, and gap scores with the three hospital types and levels were determined using multivariate linear regression models after adjusting for patients demographic, socioeconomic, and disease-related factors.
3. Results
3.1. Results of System Review
Table 1 compares major aspects (modified from WHO's six building blocks) of TMM, TCM, and WM. The entries in the first column of the table correspond to the following headings.
Table 1.
Comparison of the TMM health system with TCM and WM health systems in Inner Mongolia based on the six building blocks framework.
| Building block | Details | Traditional Mongolian medicine | Traditional Chinese medicine | Western medicine | References |
|---|---|---|---|---|---|
| History | Inherited by or introduced in Inner Mongolia | Inherited by Mongolia between the 13th and 16th centuries. | Originated in China about 3,000 years ago. | Introduced into China and Inner Mongolia in the early 19th century. | [12–16] |
| Establishment of the first hospital | 1940s | 1900s | 1830s | [12, 14, 15] | |
| Year of establishment of the first faculty (start of undergraduate program) | 1958 | 1958 | 1956 | [12, 17–19] | |
| Regulations | “Regulation of TMM and TCM in Inner Mongolia”, the first local laws and regulations about traditional medicine came in 2001. The new version came in 2010. | “Regulation of TCM of People's Republic of China” came in 2003. | Drug Administration Law of China in 2008. Regulations of Medical Institutions in 2005. Regulations of Medical Accidents in 2008. |
[14, 20, 21] | |
|
| |||||
| Service delivery | Percentage of hospitals providing this kind of medical service in 2015 | 16% | 19% | 74% | ∗ |
| Number of beds in 2015 | 15,649 | 14,146 | 84,280 | ∗ | |
| Level of coverage | Partial. In some areas, township and village levels are covered by neither TMM nor TCM | Complete (all levels) | ∗ | ||
| Number of outpatients in 2015 (million) | 7.6 | 6.3 | 34 | ∗ | |
| Number of inpatients in 2015 (million) | 0.3 | 0.3 | 2.1 | ∗ | |
| Clinical department | Modern medical science department classification; some TMM hospitals have a special clinical section, such as TMM therapy section. | [22] | |||
| Language in service | Chinese or Mongolian | Chinese | Chinese | [23] | |
| Diagnostic and treatment process | Requires a deep communication with patients. | Accurate diagnosis by using advanced medical equipment and laboratory tests. | [24, 25] | ||
| Acceptance by people ∗∗ | Generally accepted by most minority groups, 25% of Han people never used or never heard of TMM. | Accepted by most people but seen as a supplement of WM. | Accepted by most people as the main health service provider. | [26–28] | |
|
| |||||
| Health workforce | Health workforce in 2015 (thousand) | 17 | 15 | 101 | ∗ |
| Workforce per thousand population in 2015 | 0.7 | 0.6 | 4.05 | ∗ | |
| Educational model | (i) University only. (a) 5-year Bachelor. (b) 3-year Master or standardized training (ii) Alternative apprentice training |
(i) University only. (a) 5-year Bachelor (b) 3-year Master or standardized training. |
[24, 29, 30] | ||
| Number of schools | 2 | 2 | 4 | [31–34] | |
| Number of undergraduate students per year | 500 | 500 | 1200 | [17–19, 31–34] | |
| Pass rate of National Practicing Physician Qualifications Test | 60% | 60% | 62% | [35] | |
|
| |||||
| Health information system | Information for planning, monitoring, and evaluation | By Health and Family Planning Commission and TCM and TMM Administration. | By Health and Family Planning Commission and Public Hospital Reform Office. | [36] | |
| Health information system outside the National Health Information System | Under the support and guidance of Health and Family Planning Commission; TMM and TCM information systems, including a unified translation standards of minority languages. | Under the support and guidance of Health and Family Planning Commission and Public Hospital Reform Office. | [36, 37] | ||
| Library system | Library of Inner Mongolia University National network. |
National and international medical network of electronic link. | [36, 37] | ||
|
| |||||
| Medical products and technologies | Number of medicaments used in China | More than 2,200 kinds, in which 1,342 are regularly used. | More than 2,500 kinds, including twelve large varieties of prescriptions and preparations. | More than 2,740 medical products normally used. | [22, 38] |
| Evaluation of medicine | Good effect on many kinds of diseases, preeminent performance on orthopedics. | Becoming more prominent in the growing challenge of noncommunicable diseases. Slow in action but more thorough in “curing the root of the problem” with few side effects. | Good at diagnosis and treatment, especially for serious or urgent diseases, considered to be “more powerful and quick” but may cause significant side effects. | [22, 26, 39] | |
| Standardization | In 1986, 322 medicaments were put in the Medicine Standard of Inner Mongolia but only 57 in 1998. | Already had medicaments standard in China. Three medicaments were approved by the FDA to undergo further clinical trials before 2016. | FDA approved more than 10,000 drugs. | [12, 40–42] | |
| Market value (RMB) | Small market share with 3 billion yuan in 2010. | 400 billion yuan in 2005 across the whole country. | More than 2,000 billion yuan in 2015 across the whole country. | [22, 43, 44] | |
|
| |||||
| Financing and sustainability | Total revenue in 2015 (million RMB) | 4.8 | 3.6 | 30.2 | ∗ |
| Government subsidy (%) | 27.5 | 24.7 | 13.7 | ∗ | |
| Staff cost paid by the government (%) | 100 | 80 | 0 | [22] | |
| Proportion of reimbursement from health insurance from basic level to high level | Varies from 80%-30% | Varies from 60%-20% | [22, 45] | ||
| Number of items listed in the Medicare Insurance Reimbursement Catalog 2017 | 88 | 1,238 | 1,297 | [46] | |
|
| |||||
| Leadership/ governance |
Administrative department of Health and Family Planning of Inner Mongolia | TMM and TCM Administrations were set up in the provincial and municipal levels from 2007. | Medical Reform Office Public Hospital Reform Office. |
[22] | |
| Items of autonomy of the Inner Mongolia Autonomous Region Government | Establish the standard for TMM drugs, technology, and hospitals. Establish and negotiate health insurance reimbursement catalog. | Province-specific health insurance reimbursement catalog. | [21] | ||
| Research promotion priority | Biomedical | Biomedical | Clinical and Public Health, Public Hospital Reform | [22] | |
a∗Calculated from Health Information Reporting System of Inner Mongolia in 2015.
b∗∗See Table 3.
cWM: Western medicine; TCM: Traditional Chinese medicine; TMM: Traditional Mongolian medicine; TM: Traditional medicine;
IMMU: Inner Mongolia Medical University; FDA: Food and Drug Administration
History. The inheritance of TMM in Inner Mongolia was much later than the origination of TCM in China whereas WM was introduced many centuries later. Formal training of the medical profession in all three types started after the 1949 revolution [12]. Rapid progress in regulation was made after the turn of the millennium when China's economy strengthened.
Service Delivery. TMM and TCM have a similar small share in service delivery. The health service provided by WM hospitals is around three times that of TMM and TCM hospitals combined. WM is the backbone of health services since it covers all levels of health care.
Health Workforce. Despite policy to accelerate training of TMM and TCM health personnel during the last 10 years, currently, the combined health workforce is still only one-third that of WM. The two types of traditional medicines combined also have a smaller workforce training capacity and productivity than those of WM. To compensate for the shortage, apprenticeship training for TMM is still formally accepted [24]. However, trainees have to pass the license examination before being allowed to provide medical services and the pass rate for TMM candidates is lower [35].
Health Information System. All types of hospitals have to submit their basic information, including institutions, facilities, health workforce, and health service, to the unitized medicine information system [37]. The TCM and TMM administrations in Inner Mongolia have the responsibility of producing, analysing, disseminating, reporting, and using this information related to TMM. A TMM literature information center is located in Inner Mongolia Medical University and is responsible for the collection, collation, and publication of TMM literature. The government is currently building a TMM information system with unified translation standards of minority languages [37]. This may or may not be similar to TMM in Mongolia and other countries where people of Mongol ethnicity reside.
Medical Products and Technologies. The numbers of medicaments within each of the three types of medicines are comparable. TMM has its preeminent performance in the field of orthopedics, which was largely necessitated by horse riding and nomadic lifestyles of the people [13]. Production of the TMM industry was limited by substandard research, which was much slower than for TCM. Its market share was only 0.75 percent of TCM and 0.15 percent of WM [43]. Most of the effective TMM medicaments and formulations were abandoned in the standardization [47]. Medicaments and formulations with standard licenses produced by companies were refused by TMM hospitals. On the other hand, formulations produced in TMM hospital laboratories are not allowed by the government to be sold to the public.
Financing and Sustainability. TMM hospitals have one-third higher revenue than their TCM counterpart. WM hospitals, however, have revenue nearly four times higher than the other two combined. TMM hospitals are heavily subsidized in terms of budget allocation, staff salaries, and reimbursement from the health insurance system. However, the number of items reimbursable is less than 10% of those in TCM and WM hospitals.
Leadership/Governance. Responsibilities of TMM and TCM administrators include provision of special policies and development planning on the basis of the principles of national policies and the health situation of people in Inner Mongolia [22]. Management functions include designing the system framework and designing the standards and drugs catalog, guidance, and oversight, which are all unified to facilitate better coordination [22]. On the basis of these responsibilities and functions, the government can better promote the development of TMM, protect the Mongolian culture, and provide equal rights for all ethnic minorities to develop. However research projects supporting TMM and TCM have mainly been biomedical (basic science) in nature whereas clinical trials and public health are mostly confined to WM.
3.2. Results of Patient Survey
The basic characteristics of the study hospitals are shown in Table 2. Four provincial hospitals were selected from Hohhot city, two offering western medicine and one each offering traditional Chinese medicine and traditional Mongolian medicine. The four hospitals from Baotou city, two city-level and two county-level, all offered traditional medicine.
Table 2.
Summary characteristics of the study hospitals.
| City | Level | Sample hospital | Type of medicine offered | Number of outpatients per year | Number of study subjects |
|---|---|---|---|---|---|
| Hohhot | Provincial | A | WM | 1,431,420 | 165 |
| B | WM | 1,369,180 | 168 | ||
| C | TCM | 279,910 | 163 | ||
| D | TMM | 534,460 | 163 | ||
| Baotou | City | E | TCM | 48,940 | 168 |
| F | TMM | 147,870 | 167 | ||
| County | G | TMM | 99,340 | 163 | |
| H | TMM | 35,600 | 165 |
aWM: Western medicine; TCM: Traditional Chinese medicine; TMM: Traditional Mongolian medicine.
A comparison of characteristics of respondents attending Western medicine, traditional Chinese medicine, and traditional Mongolia medicine hospitals is shown in Table 3. The study sample had mean age of around early thirties and was predominated by females (63%). Higher ratio for female was due to the fact that one of the sample departments was gynecology. The TMM hospitals had higher proportions of older patients, Mongolian people, patients with lower education, and residents living in pasturelands. TCM hospitals had a higher proportion of poorer patients and those not currently employed. Patients attending WM hospitals were more educated and tended to reside in a different locality from the hospital where they sought treatment. The distributions of marital, occupational, and insurance status were more or less balanced.
Table 3.
Demographic characteristics of study sample (N=1,322).
| WM (N=333) | TCM (N=331) | TMM (N=658) | |
|---|---|---|---|
| Gentle | |||
| Male | 119 (35.7) | 116 (35.1) | 255 (38.8) |
| Female | 214 (64.3) | 215 (64.9) | 403 (61.2) |
|
| |||
| Age (mean, SD) | 32.2 (21.2) | 31.9 (21.0) | 34.3 (22.5) |
|
| |||
| Nationality | |||
| Han | 282 (84.7) | 297 (89.7) | 518 (78.7) |
| Mongolian | 44 (13.2) | 23 (6.9) | 131 (19.9) |
| Others | 7 (2.1) | 11 (3.3) | 9 (1.4) |
|
| |||
| Completed education level | |||
| Primary school or less | 111 (33.4) | 122 (36.9) | 280 (42.6) |
| Secondary school | 110 (33.0) | 119 (36.0) | 236 (35.9) |
| Diploma or higher | 112 (33.6) | 90 (27.1) | 142 (21.5) |
|
| |||
| Marital status | |||
| Single | 137 (41.1) | 123 (37.2) | 237 (36.0) |
| Married | 180 (54.1) | 194 (58.6) | 401 (60.9) |
| Others | 16 (4.8) | 14 (4.2) | 20 (3.1) |
|
| |||
| Occupational group | |||
| None | 161 (48.3) | 183 (55.3) | 332 (50.5) |
| Private | 88 (26.5) | 91 (27.5) | 208 (31.6) |
| Public | 84 (25.2) | 57 (17.2) | 118 (17.9) |
|
| |||
| Insurance status | |||
| None | 17 (5.1) | 33 (10.0) | 53 (8.1) |
| UEBMIS | 112 (33.6) | 70 (21.1) | 156 (23.7) |
| URBMIS | 73 (21.9) | 99 (29.9) | 142 (21.6) |
| NRCMIS | 96 (28.9) | 105 (31.7) | 275 (41.8) |
| Others | 35 (10.5) | 24 (7.3) | 32 (4.8) |
|
| |||
| Monthly family income | |||
| None | 66 (19.8) | 126 (38.1) | 150 (22.8) |
| ≤ 4000 | 149 (44.8) | 143 (43.2) | 377 (57.3) |
| > 4000 | 118 (35.4) | 62 (18.7) | 131 (19.9) |
|
| |||
| Area of residence† | |||
| Local | 226 (67.9) | 279 (84.3) | 565 (85.9) |
| Not Local | 107 (32.1) | 52 (15.7) | 93 (14.1) |
|
| |||
| Registered area of residence | |||
| Urban | 214 (64.3) | 202 (61.0) | 354 (53.8) |
| Rural | 114 (34.2) | 125 (37.8) | 239 (36.3) |
| Pasturelands | 5 (1.5) | 4 (1.2) | 65 (9.9) |
|
| |||
| Disease/health problem | |||
| Cardiovascular and blood | 87 (26.1) | 81 (24.5) | 166 (25.2) |
| Musculoskeletal and injuries | 74 (22.2) | 81 (24.5) | 173 (26.3) |
| Genitourinary system and gestation | 55 (16.5) | 67 (20.2) | 115 (17.5) |
| Respiratory system | 68 (20.4) | 46 (13.9) | 86 (13.1) |
| Other | 33 (9.9) | 15 (4.5) | 28 (4.3) |
| Digestive system | 3 (0.9) | 17 (5.1) | 24 (3.6) |
| Eyes, ears, and skin | 4 (1.2) | 3 (0.9) | 29 (4.4) |
| Metabolism, nervous system, and mental health problems | 4 (1.2) | 16 (4.8) | 11 (1.7) |
| Cancer | 3 (0.9) | 4 (1.2) | 20 (3.0) |
| Newborn and congenital anomaly | 0 (0.0) | 1 (0.3) | 4 (0.6) |
| Infectious diseases | 2 (0.6) | 0 (0.0) | 2 (0.3) |
|
| |||
| Symptoms | |||
| Fever / Cough | 77 (23.2) | 62 (18.7) | 80 (12.2) |
| Pain | 124 (37.2) | 110 (33.1) | 268 (40.7) |
| Palpitations | 28 (8.4) | 23 (6.9) | 53 (8.1) |
| Others | 84 (25.2) | 118 (35.7) | 220 (33.4) |
| None | 20 (6.0) | 18 (5.4) | 37 (5.6) |
|
| |||
| Repeat symptom | |||
| Yes | 165 (49.5) | 177 (53.5) | 292 (44.4) |
| No | 168 (50.5) | 154 (46.5) | 366 (55.6) |
|
| |||
| Duration of symptoms | |||
| ≤3 days | 105 (31.5) | 120 (36.3) | 222 (33.7) |
| 4-30 days | 133 (39.9) | 120 (36.3) | 252 (38.3) |
| >30 days | 95 (28.6) | 91 (27.4) | 184 (28.0) |
|
| |||
| Reason for choosing hospital | |||
| Distance | 75 (22.5) | 80 (24.2) | 233 (35.4) |
| Finance | 16 (4.8) | 22 (6.6) | 38 (5.8) |
| Quality | 210 (63.1) | 172 (52.0) | 309 (46.9) |
| Attitude/Trust/Others | 32 (9.6) | 57 (17.2) | 78 (11.9) |
|
| |||
| Patient status | |||
| New patient | 224 (67.3) | 178 (53.8) | 444 (67.5) |
| Established patient | 109 (32.7) | 153 (46.2) | 214 (32.5) |
a†Relative to the hospital where the patient sought treatment.
bWM: Western medicine; TCM: Traditional Chinese medicine; TMM: Traditional Mongolian medicine. UEBMIS: Urban Employees Basic Medical Insurance System; URBMIS: Urban Residence Basic Medical Insurance System; NRCMIS: New Rural Cooperative Medical Insurance System; SD: standard deviation.
On clinical aspects, four groups of diseases (cardiovascular diseases and diseases of the blood, musculoskeletal problems and injuries, diseases of the genitourinary system and gestation, and diseases of the respiratory system) accounted for 83% of all study patients. The distribution of diseases by medicine type was generally balanced except that TMM hospitals had a relatively higher proportion of patients with musculoskeletal problems and injuries, TCM hospitals had a higher proportion of patients with diseases of the genitourinary system, and WM hospitals had a higher proportion of patients with cardiovascular, blood, and respiratory system diseases. TCM hospitals tended to have a higher proportion of established patients. In general, the majority of the patients visited the hospitals for the first time and with symptoms lasting for 4-30 days. The quality of health service was the main reason for choosing the particular hospital among all patients.
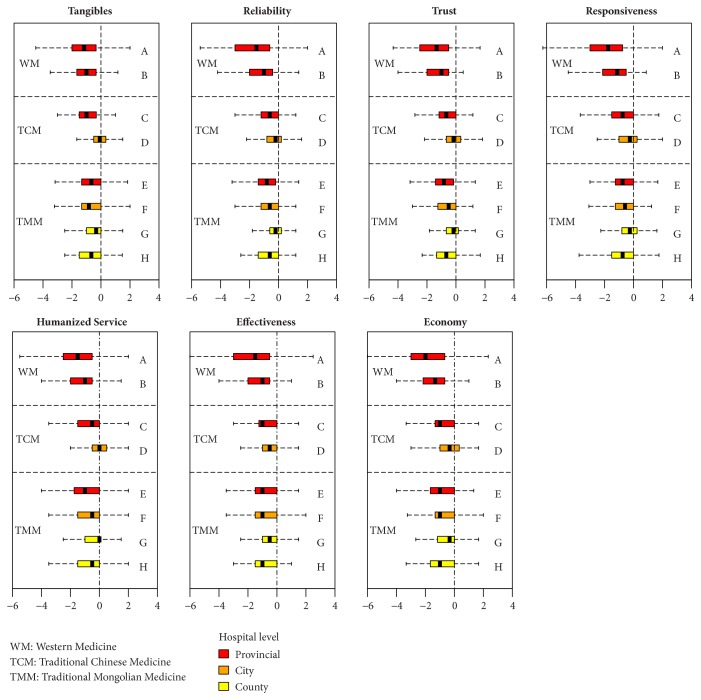
Figure 1 shows a comparison of patient's expectations of the health services by type and level of hospital.
Figure 1.
Comparison of patient's expectations of health services by type and level of hospital (N=1,322).
The median expectation scores for all hospitals ranged from 7.8 to 8.8 and the overall mean expectation score was 8.2. Patients attending WM hospitals had a higher expectation than those attending TCM and TMM hospitals (p = 0.001). Patients who attended provincial level hospitals had the highest expectation, followed by city-level and county-level hospitals. There were also variations in expectation within hospitals offering the same type of medicine, particularly TMM hospitals.
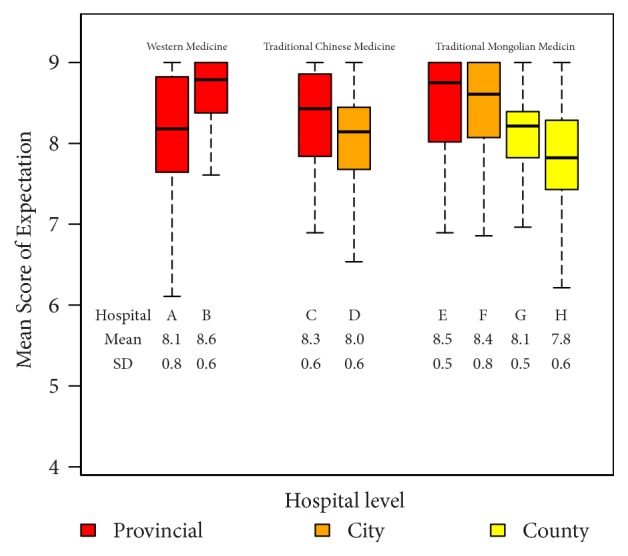
Figure 2 shows a comparison of patient's perceptions of the health services by type and level of hospital.
Figure 2.
Comparison of patient's perceptions of health services by type and level of hospital (N=1,322).
Patient's perceptions of the quality of healthcare services differed from that of their expectations. Patients attending WM hospitals had a lower perception compared to patients attending TCM and TMM hospitals (p <0.001). Among the TCM and TMM hospitals, patients attending city-level hospitals had a higher perception of health services than the others.
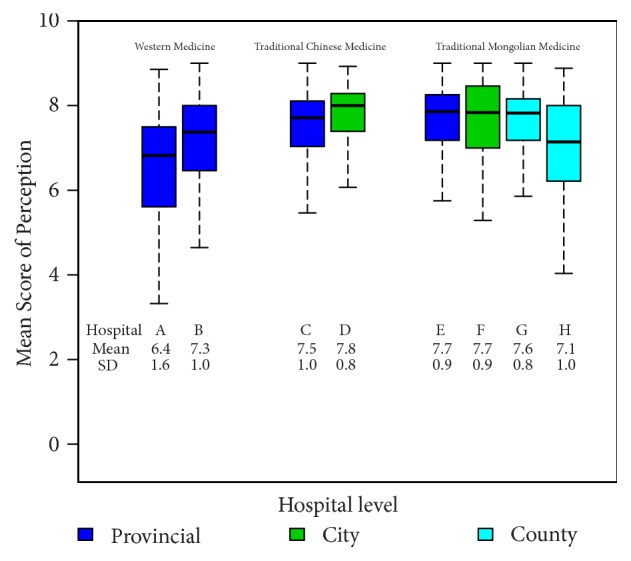
Figure 3 shows a comparison of the difference between patient's expectations and their perceptions of the health services (the gap score) by type and level of hospital. A negative value indicates that patient's perceptions were below their expectations. Due to relatively high expectation scores, most hospitals had negative gap scores. The largest negative gap score was seen in WM hospitals (mean difference: -1.6). TCM and TMM hospitals had a median difference of zero indicating that patient's perceptions tended to match their expectations.
Figure 3.
Comparison of patient's gap scores by type and level of hospital (N=1,322).
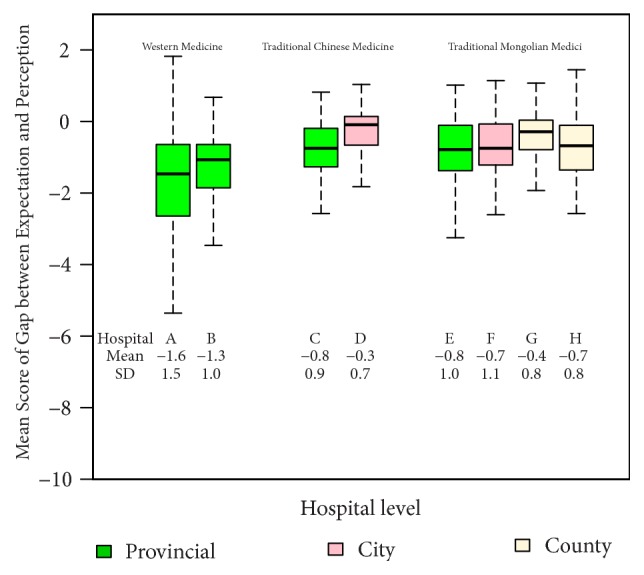
Figure 4 compares the gap scores for the seven quality of service domains stratified by hospital type. Median gap scores for all domains were less than zero, with WM hospitals having noticeably lower scores compared to the other hospitals. Health service perceptions of patients attending city-level TCM hospitals were higher than zero for most domains.
Figure 4.
Comparison of patient's gap scores for quality of service domains by type and level of hospital (N=1,322).
Table 4 shows adjusted coefficients and their 95% confidence intervals of factors from the final linear regression models predicting patients' expectations, perceptions, and gap. The models included 12 variables, but only results for medicine type and hospital level, the main focus of this analysis, are presented.
Table 4.
Final linear regression models presenting factors associated with expectation, perception, and gap (N=1,322).
| Factor | Expectation | Perception | Gap | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Adj. coeff. (95% CI) | P value (t-test) |
P value (F-test) |
Adj. coeff. (95% CI) | P value (t-test) |
P value (F-test) |
Adj. coeff. (95% CI) | P value (t-test) |
P value (F-test) |
|
|
| |||||||||
| Type of medicine: ref.=TMM | < 0.001 | < 0.001 | < 0.001 | ||||||
| WM | -0.16 (-0.28,-0.05) | 0.006 | -0.66 (-0.84,-0.47) | < 0.001 | -0.50 (-0.67,-0.32) | < 0.001 | |||
| TCM | -0.28 (-0.38,-0.18) | < 0.001 | -0.05 (-0.22,0.11) | 0.517 | 0.21 (0.05,0.36) | 0.009 | |||
| Level of hospital: ref.=Provincial | < 0.001 | < 0.001 | < 0.001 | ||||||
| City | -0.12 (-0.23,-0.02) | 0.023 | 0.23 (0.06,0.40) | 0.009 | 0.31 (0.15,0.47) | < 0.001 | |||
| County | -0.53 (-0.66,-0.41) | < 0.001 | -0.12 (-0.32,0.08) | 0.231 | 0.35 (0.17,0.52) | < 0.001 | |||
aTMM: Traditional Mongolian medicine. TCM: Traditional Chinese medicine. WM: Western medicine.
bNote: The expectation model was adjusted for marital status, occupation, insurance status, monthly family income, duration of symptoms, and patient status.
The perception model was adjusted for nationality, marital status, occupation, insurance status, monthly family income, residential status, type of disease, duration of symptoms, and reason for choosing the hospital.
The gap model was adjusted for nationality, education level, monthly family income, current residence, duration of symptoms, reason for choosing the hospital, and patient status.
Patients attending TMM hospitals had the highest level of expectation and perception; however, their overall evaluation of the health service quality (the gap scores) was lower than patients attending TCM hospitals. Patients attending WM hospitals were the most dissatisfied with the quality of the health service.
4. Discussion
Data from health information systems indicated that TMM plays important roles in health services. It is vibrant and accepted by the minority groups with preeminent performance on orthopedics. Compared with TCM and WM, health service capacity of TMM was limited by a less number of hospitals, less health workforce, weaker educational capacity, and behindhand research. However, it receives a higher subsidy from regular government investment and reimbursement schemes.
Our survey significantly assists our understanding of how local people perceive the three health systems. It revealed the popularity of TMM among respondents who were of Mongol ethnicity and living in pasturelands. The survey also highlights more important roles of TMM in serving musculoskeletal problems of outpatients. Our study revealed that the clients of TMM hospitals had the highest level of expectation and were also more likely to have higher perceptions than clients of the other two hospital types.
The regular utilization of traditional medicine as a component of a health system is accepted by half the population of many developed and developing countries [26, 48–53]. In our study setting, traditional medicine is not only popular but also strongly supported by the government. The proportion of services provided by TMM in Inner Mongolia is more substantive than that of Thai Traditional medicine in Thailand but smaller than Ayurveda in India [54, 55].
Coexistence of the three medicine subsystems in the same community may initiate competition for patients between the hospitals, especially in a small service market [22]. It also forms a competitive relationship in resources, especially human resources. The large hospitals will capture health personnel working in TMM or TCM hospitals due to their financial strength. This mobility of health workforce usually happens from lower level to higher level hospitals. As a result, inadequate health services in rural China [56] are therefore not confined to WM but also traditional medicine.
The prevailing dominance of WM over traditional medicines in China, including TCM, is seen in most of its provinces as well as in other countries [27, 57, 58]. With advanced technology, the expectations of the majority of patients attending WM hospitals are relatively high. Their overwhelming numbers of patients and inadequate subsidy from the government also fuel the deteriorating doctor-patient relationship [59] which is evidenced by their low perception scores in our study. This weakness in the mainstream health system needs to be corrected.
Not all people who are ill need to see a doctor. Self-treatment for minor ailments with safe and effective over-the-counter products can be useful in many cases and it is a common practice worldwide [60]. On one hand, TCM products, which often do not have proof of safety or efficacy, are heavily advertised on public media. On the other hand, TMM products have a very narrow clientele due to poor scientific research and poor market mechanisms. These deficiencies need to be addressed by policy-makers. To promote TMM, it is therefore necessary to incorporate scientific research into TMM to improve its efficacy and safety. This would further strengthen pride and acceptance of local people.
This study showed that patients' expectations of health service quality are higher than their perceptions, a result seen in other studies from Iran [61], Turkey [62], and Taiwan [63]. However, on multivariate analysis, patients visiting traditional medicine hospitals had positive gap scores, indicating that the health service quality of these hospitals was higher than the western medicine hospitals. Traditional medicine has the potential to improve the overall quality and become an important supplement to Western medicine, especially on humanized service aspects.
Finally, traditional medicines, which are rooted in indigenous medical practice, have accumulated a large number of drugs and contain valuable experience. There have been many successful cases for western medicine to find new ideas, treatments, and drugs from the rich resources of traditional medicine [47, 64]. If traditional medicine systems are lost, countries, especially developing ones, will lose their self-reliability, their culture, and their identity [65].
5. Conclusion
In Hohhot and Baotou cities of Inner Mongolia, Traditional Mongolian medicine is well accepted by the government and citizens. It has the potential to improve its overall quality and become an indispensable supplement in the whole health service system. Continued protection and promotion of its development by investment, government policies, education, and biomedical and health systems research will be needed.
Acknowledgments
The authors thank the Health and Family Planning Commission of Inner Mongolia for providing data. This study received financial support from Key Research Base of Humanities and Social Science of Inner Mongolia Autonomous Region of China and Prince of Songkla University.
Data Availability
The data used to support the findings of the system review in this study were provided by Health Information Reporting System (HIRS) of Inner Mongolia Autonomous Region under license, and so cannot be made freely available. Access to these data will be considered by the author upon request, with permission of Health and Family Planning Commission of the Inner Mongolia. The data used to support the findings of the survey in this study were supported by the Key Research Base of Humanities and Social Science of Inner Mongolia Autonomous Region, and so cannot be made freely available. Access to these data will be considered by the author upon request, with permission of Health Management School of Inner Mongolia Medical University.
Additional Points
Limitations of This Study. The study was based on a small sample of hospitals of Inner Mongolia. Domination of females in our sample indicated a higher proportion of them using health services but may also imply an underrepresentation of males in the sample.
Ethical Approval
The study was approved by the Research Ethical Committee of the Faculty of Medicine, Prince of Songkla University (reference no. SUB-EC 58-290-18-5) on December 9, 2015. All data collection processes were approved by the study hospitals.
Disclosure
The interpretation and conclusions contained herein do not represent those of Inner Mongolia Health and Family Planning Commission.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Authors' Contributions
Virasakdi Chongsuvivatwong, Yancun Fan, and Min Li conceived the research idea. Min Li reviewed the literature and interview notes. Yancun Fan and Min Li conducted the survey and collected the data. Virasakdi Chongsuvivatwong, Edward B. McNeil, and Min Li analysed the data. Min Li interpreted the results and wrote the first draft of the manuscript. Virasakdi Chongsuvivatwong and Edward B. McNeil added critical comments and made revisions to the interpretations of results and to the final manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Key Research Base of Humanities and Social Science of Inner Mongolia Autonomous Region of China and Prince of Songkla University.
Supplementary Materials
Supplementary Appendix 1: key informants interview guideline (english version).
Supplementary Appendix 2: patient survey questionnaire (english version).
References
- 1.World Health Organization (WHO) WHO Traditional Medicine Strategy 2002-2005. UN; 2002. [Google Scholar]
- 2.Yu F., Takahashi T., Moriya J., et al. Traditional chinese medicine and kampo: a review from the distant past for the future. Journal of International Medical Research. 2006;34(3):231–239. doi: 10.1177/147323000603400301. [DOI] [PubMed] [Google Scholar]
- 3.Zhou B. Thinking of the acceleration in the development and research of Mongolian Medicines in Inner Mongolia. Journal of Medicine & Pharmacy of Chinese Minorities. 2003;10(3):p. 45. [Google Scholar]
- 4.Pitschmann A., Purevsuren S., Obmann A., et al. Traditional Mongolian medicine: history and status quo. Phytochemistry Reviews. 2013;12(4):943–959. doi: 10.1007/s11101-013-9321-5. [DOI] [Google Scholar]
- 5.World Health Organization (WHO) Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. 2007. [Google Scholar]
- 6.Health Information Reporting System (HIRS) of Inner Mongolia n.d
- 7.Niu H. Study on Medical Service Quality Assessment Model Based on SERVQUAL. Huazhong University of Science and Teachnology; 2006. [Google Scholar]
- 8.Bernard R. Fundamentals of Biostatistics. 5th 2002. [Google Scholar]
- 9.Ngamjarus C. C V. n4Studies: Sample size and power calculations for iOS. The Royal Golden Jubilee Ph.D. Program [Ph.D. thesis] Golden Jubilee Ph.D. Program—The Thailand Research Fund & Prince of Songkla University; 2014. [Google Scholar]
- 10.Tang N. One Hospital Service Quality Assessment And Improvement Based On SERVQUAL Scale [Master, thesis] Nan Hua University; 2013. [Google Scholar]
- 11.Team R. C. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 12.Bi L., Wu Y., Chang F. Inherit and develop Mongolian Medicine and drugs, and further accelerate its research and exploitation. Jounal of Inner Mongolia Medical College. 2007;29:186–189. [Google Scholar]
- 13.Jigmed B. Survey on Mongolian medical science history. Journal of Medicine & Pharmacy of Chinese Minorities. 2007:1–5. [Google Scholar]
- 14.Zhuge M. Promote national heritage, benefit mankind. Guangming Dly. 2006;8 [Google Scholar]
- 15.Wang Z. John Glasgow Kerr and introduce western medicine into China. Chinese Journal of Medical History. 2003;33:96–99. [Google Scholar]
- 16.Park H.-L., Lee H.-S., Shin B.-C., et al. Traditional medicine in China, Korea, and Japan: a brief introduction and comparison. Evidence-Based Complementary and Alternative Medicine. 2012;2012:9. doi: 10.1155/2012/429103.429103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The introduction of TMM Faculty of Inner Mongolia Medical University. TMM Faculty of Inner Mongolia Medical University 2017. https://myyxy.immu.edu.cn/xygk/xyjj.htm.
- 18.The introduction of TCM Faculty of Inner Mongolia Medical University. TCM Faculty of Inner Mongolia Medical University 2017. https://zyxy.immu.edu.cn/info/1002/2092.htm.
- 19.The introduction of Basic Medicine Faculty of Inner Mongolia Medical University. Basic Medical Faculty of Inner Mongolia Medical Universtiy 2016. https://jcyxy.immu.edu.cn/xygk/xyjj.htm.
- 20.News about the new version of “Regulation of TMM&TCM in Inner Mongolia Autonomous Region” in 2010. Government of Inner Mongolia Autonomous Region 2010. http://www.xywy.com/yp/zlfl/201008/10/691470.html.
- 21.Policy Publicity of Health and Family Planning Commission of Inner Mongolia Autonomous Region. Health and Family Planning Commission of Inner Mongolia Autonomous Region 2017. http://www.nmgwjw.gov.cn/webappnew/zcfg/?fwfl.
- 22.Wu L. Vigorous development of Mongolian medicine in Inner Mongolia. Journal of Medicine & Pharmacy of Chinese Minorities. 2010;16:1–6. [Google Scholar]
- 23.Wang L. Qirenwangqige: special attention need to be paid to the problems of TMM in medical reform in China. China Medical Herald. 2011;8:p. 8. [Google Scholar]
- 24.Bao W. Inheritance and innovation of Mongolian medicine. Journal of Medicine & Pharmacy of Chinese Minorities. 2014;8:58–60. [Google Scholar]
- 25.Yang Z. The defects and reflections on the development of modern medical science. Chinese Journal of Diagnostic (Electronic Ed) 2013 [Google Scholar]
- 26.Lam T. P. Strengths and weaknesses of traditional Chinese medicine and Western medicine in the eyes of some Hong Kong Chinese. Journal of Epidemiology and Community Health. 2001;55(10):762–765. doi: 10.1136/jech.55.10.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chung V. C., Lau C. H., Yeoh E. K., Griffiths S. M. Age, chronic non-communicable disease and choice of traditional Chinese and western medicine outpatient services in a Chinese population. BMC Health Services Research. 2009;9 doi: 10.1186/1472-6963-9-207.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu X. Research on the present situation and existing problems of Mongolian medicine industry in inner mongolia. China's Health Industry. 2015;12:16–18. [Google Scholar]
- 29.The Basic Information of Inner Mongolia Medical University. Inner Mongolia Medical University; 2016. [Google Scholar]
- 30.Li Y., Shi Z., Ao X., Dong P., Bai Y., Liu X. A survey of Mongolian medicine traditional knowledge in inner mongolia. Journal of Medicine & Pharmacy of Chinese Minorities. 2017;23:68–70. [Google Scholar]
- 31.The Basic Information of Education Program of Inner Mongolia Medical University. Inner Mongolia Medical University; 2017. http://souky.eol.cn/HomePage/school_des/437/437.html. [Google Scholar]
- 32.The Basic Information about the Faculty of Medicine of Inner Mongolia University of Science and Technology. Inner Mongolia University of Science and Technology; 2016. http://www.imust.cn/xxgk.htm. [Google Scholar]
- 33.The Introduction of TMM Faculty of Inner Mongolia University for Nationalities. Inner Mongolia University for Nationalities; 2017. http://219.225.148.48:8080/pub/mgxxy/xygk/index.htm. [Google Scholar]
- 34.The Basic Information of Medical School of Chifeng University. Chifeng University; 2015. http://web.cfxy.cn/yxy/yxgk/16399.htm. [Google Scholar]
- 35.Basic Information about the National Practicing Physician Qualifications Test. http://news.koolearn.com/20161009/1097931.html, 2016.
- 36.Shan M., Galatu H. Construction of information resources based on sustainable development of traditional Mongolian medicine. Chinese Journal of Medical Library and Information Science. 2015;24:24–25. [Google Scholar]
- 37.Bi L., Wu Y. Accelerating creative research on traditional monglian medicine and its development strategies. Journal of Inner Mongolia Medical College. 2007;29:1–7. [Google Scholar]
- 38.Committee NP. Pharmacopoeia of the People’s Republic of China (The First Part), 2010
- 39.Dong Z., Phillips M. R. Evolution of China's health-care system. The Lancet. 2008;372:1715–1716. doi: 10.1016/S0140-6736(08)61351-3. [DOI] [PubMed] [Google Scholar]
- 40.Liu T. Traditional Chinese Medicine Industry Standard · TCM diagnosis and treatment standard of People ’s Republic of China. Publishing. Beijing: Science and Technology Literature; 2006. [Google Scholar]
- 41.Bi L., Wu Y. Present situation and significance of quality standardization of Mongolian medicine. Journal of Inner Mongolia Medical College. 2008;30:36–38. [Google Scholar]
- 42.Miou S. TCM approved by FDA to go further clinical trials. English.news.cn. http://news.xinhuanet.com/english/2015-06/27/c_134361182.htm, 2015.
- 43.Xu G. How does Mongolian medicine break through the medical turmoil? China Medical Herald. 2006;3:60–62. [Google Scholar]
- 44.Zhi Y. Analysis on the Current Situation of China’s Pharmaceutical Industry Market Operation. http://www.chyxx.com/industry/201604/406446.htm, 2016.
- 45.The proportion and scope of medical insurance in Inner Mongolia Autonomous Region in 2017. Ministry of Human Resources and Social Sercurity of the People’s Republich of China. http://www.kuaiji.com/weixin/3436870, 2017.
- 46.Medical Insurance Reimbursement catalog 2017. Minist Hum Resour Soc Secur People’s Repub China. http://www.gov.cn/xinwen/2017-02/23/content_5170392.htm, 2017.
- 47.Fan R., Holliday I. Which medicine? Whose standard? Critical reflections on medical integration in China. Journal of Medical Ethics. 2007;33(8):454–461. doi: 10.1136/jme.2006.017483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Eisenberg D. M., Davis R. B., Ettner S. L., et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. The Journal of the American Medical Association. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 49.MacLennan A. H., Wilson D. H., Taylor A. W. Prevalence and cost of alternative medicine in Australia. The Lancet. 1996;347(9001):569–573. doi: 10.1016/s0140-6736(96)91271-4. [DOI] [PubMed] [Google Scholar]
- 50.Inta A., Shengji P., Balslev H., Wangpakapattanawong P., Trisonthi C. A comparative study on medicinal plants used in Akha's traditional medicine in China and Thailand, cultural coherence or ecological divergence? Journal of Ethnopharmacology. 2008;116(3):508–517. doi: 10.1016/j.jep.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 51.Lev E. Ethno-diversity within current ethno-pharmacology as part of Israeli traditional medicine—a review. Journal of Ethnobiology and Ethnomedicine. 2006;2, article 4 doi: 10.1186/1746-4269-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patwardhan B., Warude D., Pushpangadan P., Bhatt N. Ayurveda and traditional Chinese medicine: a comparative overview. Evidence-Based Complementary and Alternative Medicine. 2005;2(4):465–473. doi: 10.1093/ecam/neh140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peltzer K. Utilization and practice of traditional/complementary/alternative medicine (TM/CAM) in South Africa. African Journal of Traditional, Complementary and Alternative Medicines. 2009;6(2):175–185. [PMC free article] [PubMed] [Google Scholar]
- 54.Legal status of traditional medicine and complementary/ alternative medicine: a worldwide review. World Health Organisation. 2001:1–199. [Google Scholar]
- 55.Mukherjee P. K. Evaluation of Indian traditional medicine. Drug Information Journal. 2001;35(2):623–632. doi: 10.1177/009286150103500235. [DOI] [Google Scholar]
- 56.Liu Y., Hsiao W. C., Eggleston K. Equity in health and health care: the Chinese experience. Social Science & Medicine. 1999;49(10):1349–1356. doi: 10.1016/S0277-9536(99)00207-5. [DOI] [PubMed] [Google Scholar]
- 57.Muhajarine N., Neudorf C., Martin K. Concurrent consultations with physicians and providers of alternative care: results from a population-based study. Canadian Journal of Public Health. 2000;91(6):449–453. doi: 10.1007/BF03404827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thomas K., Coleman P. Use of complementary or alternative medicine in a general population in Great Britain. Results from the National Omnibus survey. Journal of Public Health. 2004;26(2):152–157. doi: 10.1093/pubmed/fdh139. [DOI] [PubMed] [Google Scholar]
- 59.Zhao L., Zhang X., Bai G., Wang Y. Violence against doctors in China. The Lancet. 2014;384(9945):p. 744. doi: 10.1016/S0140-6736(14)61436-7. [DOI] [PubMed] [Google Scholar]
- 60.Wazaify M., Shields E., Hughes C. M., McElnay J. C. Societal perspectives on over-the-counter (OTC) medicines. Journal of Family Practice. 2005;22(2):170–176. doi: 10.1093/fampra/cmh723. [DOI] [PubMed] [Google Scholar]
- 61.Zarei A., Arab M., Froushani A. R., Rashidian A., Tabatabaei S. M. G. Service quality of private hospitals: the Iranian Patients' perspective. BMC Health Services Research. 2012;12(1) doi: 10.1186/1472-6963-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Çaha H. Service quality in private hospitals in Turkey. Journal of Economic and Social Research. 2007;9:55–69. [Google Scholar]
- 63.Lin D., Sheu I., Pai J., et al. Measuring patient's expectation and the perception of quality in LASIK services. Health and Quality of Life Outcomes. 2009;7(1):p. 63. doi: 10.1186/1477-7525-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tu Y. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nature Medicine. 2011;17(10):1217–1220. doi: 10.1038/nm.2471. [DOI] [PubMed] [Google Scholar]
- 65.Akerele O. The best of both worlds: bringing traditional medicine up to date. Social Science & Medicine. 1987;24(2):177–181. doi: 10.1016/0277-9536(87)90250-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix 1: key informants interview guideline (english version).
Supplementary Appendix 2: patient survey questionnaire (english version).
Data Availability Statement
The data used to support the findings of the system review in this study were provided by Health Information Reporting System (HIRS) of Inner Mongolia Autonomous Region under license, and so cannot be made freely available. Access to these data will be considered by the author upon request, with permission of Health and Family Planning Commission of the Inner Mongolia. The data used to support the findings of the survey in this study were supported by the Key Research Base of Humanities and Social Science of Inner Mongolia Autonomous Region, and so cannot be made freely available. Access to these data will be considered by the author upon request, with permission of Health Management School of Inner Mongolia Medical University.