Abstract
Specialty care units (SCUs) in nursing homes (NHs) grew in popularity during the 1990s to attract residents while national policies and treatment paradigms changed. Alzheimer disease has consistently been the dominant form of SCU. This study explored the extent to which chain affiliation, which is common among NHs, affected SCU bed designation. Using data from the Online Survey Certification and Reporting (OSCAR) from 1996 through 2010 with 207 431 NH-year observations, we described trends and compared chain-affiliated NHs with independent NHs. Designation of beds for Alzheimer disease SCUs grew from 1996 to 2003 and then declined. At the peak, 19.6% of all NHs had at least one Alzheimer disease SCU bed. In general, chain affiliation promoted Alzheimer disease SCU bed designation across time, chain size, and NH profit status. During the period of largest growth from 1996 to 2003, the likelihood of designation of Alzheimer disease SCU beds was 1.55 percentage points higher among for-profit NHs affiliated with large chains than independent for-profit NHs (P < .001) and remained 1.28 percentage points higher from 2004 to 2010. However, chain-affiliated NHs generally had a lower percentage of residents with dementia than independent NHs. For example, although for-profit NHs affiliated with large chains had more Alzheimer disease SCU beds, they had nearly 3% fewer residents with dementia than independent NHs (P < .001). We conclude that organizational decisions to designate beds for Alzheimer disease SCUs may be related to marketing strategies to attract residents since adoption of Alzheimer disease SCUs has fluctuated over time, but did not appear driven by demand.
Keywords: Alzheimer disease, dementia, long-term care, nursing home chains, specialty care units
What do we already know about this topic?
Specialty Care Units (SCUs) within nursing homes (NHs) grew in popularity during the 1990s driven in part by Medicare’s prospective payment system for hospitals, medical advancements, treatment paradigm innovations, and as a means to attract residents and increase market share.
How does your research contribute to the field?
Little is known about how chain affiliation, which is common among NHs, affected SCU bed designation.
What are your research’s implications toward theory, practice, or policy?
We conclude that organizational decisions to designate beds for Alzheimer disease SCUs may be related to marketing strategies to attract residents since adoption of Alzheimer disease SCUs has fluctuated over time, but did not appear driven by demand.
Introduction
Alzheimer disease and dementia represent significant challenges in long-term care. More than 5 million older adults in the United States are affected by dementia and that number is rising with the aging of the population.1-3 Individuals with dementia often have substantial care needs, including wandering, behavioral changes, and the loss of independence on activities of daily living. Consequently, round-the-clock care is often required in the middle stages of the disease as family caregivers become overburdened.4 Caring for individuals with dementia has tremendous economic implications as well. The direct cost for health care, long-term care, and hospice services for older Americans with Alzheimer disease is approximately $259 billion annually, with the care provided by friends and family members valued at an additional $230 billion.5 Although all forms of long-term care are impacted, providing residential care to meet the needs of this population is a major challenge for nursing homes (NHs).
Specialty care units (SCUs) first appeared in the 1980s, growing in popularity during the 1990s driven in part by Medicare’s prospective payment system for hospitals, medical advancements, treatment paradigm innovations, and as a means to attract residents and increase market share.6,7 Many types of SCUs exist including those designed to provide specialized rehabilitation, hospice, ventilator/respiratory care, and treatment of Huntington disease, and AIDS. Units for treating Alzheimer disease and dementia are the most common, comprising more than 3 times as many units relative to any other type of SCU.8 Alzheimer disease SCUs include some common features such as housing residents with similar care needs, special staff training, or modifying the physical environment. Although state regulatory and certification policies vary, NHs require no recognition by federal regulatory authorities for SCU designation.9
More than half of NHs across the country are considered chain-affiliated (2 or more facilities), and this type of ownership structure has received considerable attention from policy makers and researchers. During the 1990s and 2000s, a substantial volume of acquisitions and divestitures occurred resulting in greater consolidation of NHs into chains.10-12 Chain-affiliated NHs have been shown to have more deficiencies, higher costs, and lower ratings associated with experiences of care compared with independent NHs.13-17 Because chain-owned NHs serve many thousands of older adults and may have standardized administrative, financial, and work practices across NHs, the decisions made by a chain are important in understanding financial performance and delivery of care.18
Little is known about the decisions by NHs to build or designate SCUs. Chain affiliation may support SCU development in a number of ways, potentially sharing costs across NHs or providing connections through which best practices are shared. Because NH financial performance is linked to organizational strategies that vary based on ownership/chain affiliation, decisions such as designating beds to a SCU may align similarly.19 For example, emphasis on cost control measures by chain-affiliated NHs may benefit from economies of scale. As such, competition for residents and better access to capital markets, particularly among large chain-affiliated NHs, may allow chains greater freedom to build or designate beds for SCUs.19,20 This may be done to improve quality and/or financial performance.21,22 Furthermore, differences have been shown in the organizational strategies of chain-affiliated NHs according to profit status, potentially impacting the ability to invest in SCUs or the motivation for doing so.19 However, although the growth of SCUs was forecasted to continue during the 2000s, their prevalence has not grown beyond a minority of NHs and has even declined in recent years.20 The presence of an Alzheimer disease SCU may be associated with better care quality, but the evidence base is lacking. In fact, attributing quality of care improvements to Alzheimer disease SCUs has been challenging.23 A greater understanding of the characteristics of organizations that have designated beds for SCUs over time has implications for understanding conceptual and organizational strategies for care delivery.
In this article, we describe the association of chain affiliation and the designation of specialty care within NHs with 3 objectives. First, we evaluate trends in the prevalence of SCUs nationwide and by chain affiliation. Second, using Alzheimer disease SCUs as an example, we determine whether chain-affiliated NHs were more likely to designate beds to SCUs than independent NHs over time. Finally, we compare parallel descriptive information on SCUs and the percentage of dementia residents within a NH.
Methods
Data
We used longitudinal, NH-level data from the Online Survey Certification and Reporting (OSCAR) system from 1996 to 2010. States are required to survey all federally certified NHs every 9 to 15 months to ensure compliance with federal regulatory requirements to receive payments from Medicare and Medicaid. Certified NHs represented approximately 96% of all NHs nationwide during the study period.24 Maintained by the Centers for Medicare and Medicaid Services (CMS), the OSCAR system contains information about NHs, their staffing, and aggregated resident characteristics from state surveys through 2012, when it was replaced by the Certification and Survey Provider Enhanced Reporting (CASPER) system and the Quality Improvement Evaluation System (QIES).
To determine NH-level SCU information, CMS Form 671 asks for the total number of beds, as well as (1) specific types of SCUs within the NH, and (2) the number of beds in each type of SCU. We constructed a variable to indicate the percentage of NH beds dedicated to Alzheimer disease SCUs for each NH. Similarly, CMS Form 672 asks for the total number of residents and a census of specific conditions including dementia. This enabled us to construct a variable of the percentage of residents with dementia for each NH.
Chain affiliation was based on information provided in CMS Form 671 in the text field “Name of Multi-Facility Organization” using methods previously described.25 Recognizing that chains of different sizes may adopt different strategies in providing SCU-related services, we created a variable based on the size of each chain. Although any NH with common ownership of at least one other facility is denoted as a “multi-facility organization” using this field, we considered chain affiliation only if 5 or more NHs shared a common owner. More specifically, small chains were defined as 5 to 10 NHs, medium chains 11 to 29 NHs, and large chains 30 or more NHs. All other NHs were considered independent. We considered chains with 2 to 4 NHs to adopt organizational strategies more like independent NHs than chains. Sensitivity analyses omitting this group altogether confirmed our results were robust to this definition.
To control for factors affecting the decision to designate beds as SCUs, we incorporated a number of control variables from the OSCAR data. They included profit status, total number of beds within a NH, occupancy rate, and payer mix (percentage of residents paying with Medicare, and percentage paying with Medicaid). All variables, including chain size, were based on OSCAR annual reporting and thus could change annually. We excluded NHs from Alaska, Hawaii, the District of Columbia, and Puerto Rico as data were incomplete for our study period. We excluded government-owned and hospital-affiliated NHs due to operational differences that can affect SCU designation. The final analytical sample included 207 431 NH-year observations with complete covariate information from 1996 to 2010, averaging approximately 13 830 NHs in operation each year.
Empirical Model
First, we described trends in SCUs over time; for Alzheimer disease SCUs, we also tracked trends by the number of NHs within a chain. Second, we estimated a series of 2-part regression models to examine the effects of chain affiliation on the designation of Alzheimer disease SCU beds. We used a 2-part model because there was a disproportionate number of NH-year observations (approximately 82%) that reported zero beds designated for Alzheimer disease SCU. The first part of the model estimated the extensive margin, the decision by a NH to have any beds designated to an Alzheimer disease SCU. The second part estimated the intensive margin, the number of beds designated, given any. We estimated a logit model in the first stage and an ordinary least squares (OLS) in the second. The results of the models were then combined to estimate the marginal effect of chain affiliation on the designation of Alzheimer disease SCU beds. The general model took the form:
where represented the percentage of beds designated for Alzheimer disease SCU for NH in year . Year fixed effects were included to account for time trends in the designation of SCU beds. State fixed effects were included to account for heterogeneity in state-level policies regarding SCU bed certification and regulation as well as other policies that may have impacted the decision to designate SCU beds. Robust standard errors were used to adjust for clustering within NH over time.
To consider the context in which Alzheimer disease SCU beds were designated, we considered analogous models for the percentage of NH residents with dementia. Unlike Alzheimer disease SCUs, the percentage of residents with dementia followed a normal distribution and was modeled using OLS regression to examine the effects of chain affiliation using the same covariates described above.
We conducted all our analyses stratified by chain size and profit status of the NH, because both are known to affect organizational decisions and performance.12 We compared the effect of chain versus independent incrementally by chain size in separate models. Finally, because the effect on SCU designation was observed to be nonuniform during our study period, we conducted our analyses to examine 2 distinct time periods: a period of growth from 1996 to 2003 and of decline from 2004 to 2010.
Results
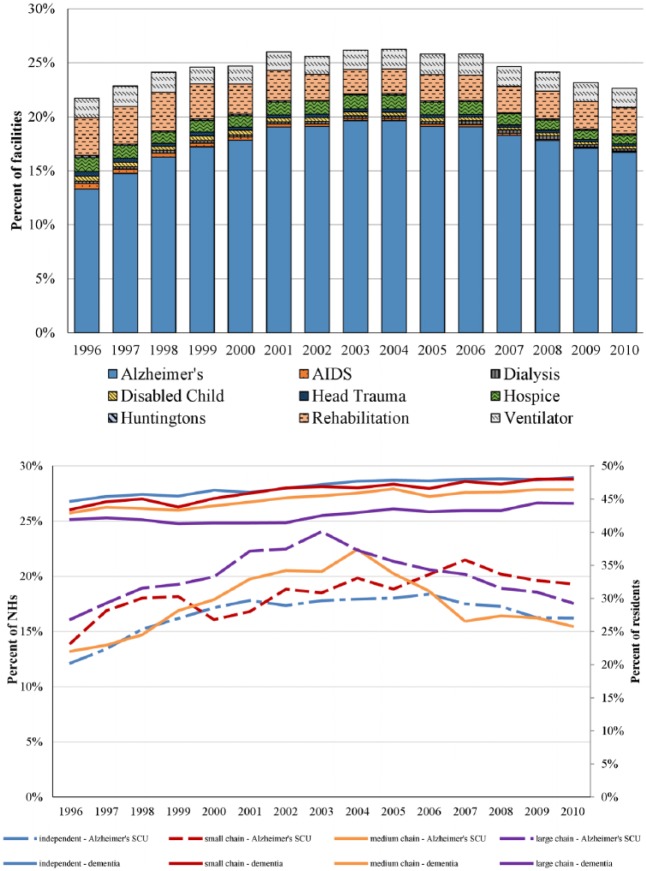
From 1996 to 2010, the share of NHs with any form of SCU ranged from a low of 21.7% in 1996 to a high of 26.3% in 2003 (Figure 1, top panel). Alzheimer disease SCU was the most common form of SCU throughout the time period, beginning at 13.3% of all NHs in 1996 and rising to 19.6% in 2003 at the peak. The second most prominent SCU category was for rehabilitation care, which was offered in approximately 5% of NHs across the study period. The bottom panel of Figure 1 shows the designation of Alzheimer disease SCUs by chain affiliation. The prevalence of beds designated for Alzheimer disease SCU by chain (and chain size) follows a similar pattern as seen for all SCUs, peaking around 2003 and declining in later years. Nursing homes affiliated with large chains were the most likely to have Alzheimer SCUs until 2007 when these SCUs became more prevalent in NHs affiliated with small chains. At the peak, 24.1% of NHs affiliated with large chains reported having any Alzheimer disease SCU beds. The rise and fall of Alzheimer disease SCUs was distinct from the linear increase in the percentage of total residents with dementia, which rose gradually from 43.7% of NH residents in 1996 to 47.1% of residents in 2010.
Figure 1.
Description.
Source. Authors’ analysis of Online Survey Certification and Reporting (OSCAR) data.
Note. Trends in SCUs over time. The top panel shows the percentage of NHs with SCUs by type. The lower panel shows the percentage of Alzheimer disease SCUs by chain-affiliation size (small 5-10 NHs, medium 11-29 NHs, and large ≥30 NHs) and percentage of dementia residents in the NH on the secondary axis. SCUs = specialty care units; NHs = nursing homes.
Table 1 displays annual descriptive characteristics by chain size and NH profit status for 3 key years, 1996, 2003, and 2010, which correspond to our study period’s beginning, end, and year with the highest prevalence of Alzheimer disease SCUs. Although nonprofit NHs represent a smaller percentage of all NHs, Alzheimer disease SCUs were more common within this organizational type. Most NH types increased the prevalence of Alzheimer disease SCU designation from 1996 to 2004 and subsequently declined from 2004 to 2010, with the exception of nonprofit NHs affiliated with small chains, which actually increased. The largest growth occurred among nonprofit NHs affiliated with large chains, as the prevalence of an Alzheimer disease SCU increased from 17.7% in 1996 to 31.7% in 2004 (79.1% relative increase); incidentally, this type of NH also experienced the largest decline, decreasing to 21.5% in 2010 (32.2% relative decrease).
Table 1.
Mean and Standard Deviation of Outcome Variables and Covariates in 1996, 2003, and 2010.
| Independent |
Size of affiliated chain |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Small |
Medium |
Large |
||||||||||
| 1996 | 2003 | 2010 | 1996 | 2003 | 2010 | 1996 | 2003 | 2010 | 1996 | 2003 | 2010 | |
| For-profit NHs | ||||||||||||
| Number of NHs | 5521 | 5092 | 5042 | 956 | 977 | 808 | 1296 | 1231 | 1490 | 466 | 3049 | 3039 |
| Has Alzheimer disease SCU (%) | 9.4 | 13.5 | 13.2 | 13.3 | 17.0 | 15.6 | 11.8 | 17.3 | 13.4 | 15.9 | 23.5 | 17.3 |
| Total percentage of overall beds in Alzheimer SCU | 2.5 (10.0) | 3.4 (10.7) | 3.4 (11.2) | 3.4 (11.5) | 4.7 (13.0) | 4.5 (13.3) | 2.8 (8.7) | 4.3 (10.9) | 3.5 (11.0) | 4.0 (11.4) | 5.7 (12.5) | 4.4 (11.7) |
| Conditional percentage of beds in Alzheimer SCU | 26.9 (20.0) | 25.1 (17.2) | 26.1 (19.1) | 25.9 (20.0) | 27.6 (19.2) | 28.6 (21.1) | 23.8 (12.1) | 24.6 (13.6) | 25.9 (18.2) | 25.2 (16.6) | 24.4 (14.6) | 25.3 (16.0) |
| Percentage residents with dementia | 44.2 (18.4) | 45.9 (18.6) | 46.9 (18.8) | 44.2 (18.4) | 46.7 (18.5) | 47.4 (17.9) | 42.8 (17.4) | 44.9 (18.4) | 45.7 (17.8) | 41.8 (17.0) | 42.7 (18.1) | 43.9 (17.2) |
| Total beds | 103.3 (60.6) | 108.0 (58.8) | 111.4 (59.7) | 106.5 (46.6) | 107.2 (47.2) | 107.3 (45.7) | 101.0 (48.1) | 102.8 (46.3) | 104.2 (44.9) | 114.2 (48.1) | 113.9 (44.5) | 113.0 (43.1) |
| Percentage occupancy | 87.5 (14.8) | 83.8 (15.1) | 82.2 (15.7) | 86.6 (13.8) | 83.4 (15.1) | 82.0 (14.7) | 86.6 (14.0) | 82.9 (14.7) | 80.6 (15.6) | 86.2 (14.1) | 85.4 (13.3) | 82.2 (15.1) |
| Percentage Medicaid primary payer | 70.7 (22.1) | 68.7 (20.8) | 63.5 (23.0) | 70.1 (18.6) | 67.3 (18.8) | 63.0 (20.8) | 68.9 (20.9) | 65.8 (21.0) | 61.6 (20.8) | 65.6 (20.2) | 65.9 (17.0) | 60.5 (20.0) |
| Percentage Medicare primary payer | 6.6 (12.1) | 9.8 (11.6) | 15.4 (16.3) | 8.0 (10.7) | 11.6 (10.7) | 15.8 (14.6) | 9.0 (12.3) | 13.5 (13.8) | 17.4 (15.7) | 12.6 (13.4) | 14.5 (10.1) | 18.6 (14.3) |
| Nonprofit NHs | ||||||||||||
| Number of NHs | 2557 | 2629 | 2457 | 285 | 350 | 372 | 188 | 297 | 286 | 249 | 232 | 214 |
| Has Alzheimer disease SCU (%) | 18.0 | 26.1 | 22.4 | 16.1 | 22.6 | 27.2 | 22.9 | 33.0 | 25.9 | 17.7 | 31.0 | 21.5 |
| Percentage of overall beds in Alzheimer SCU | 4.4 (11.7) | 6.5 (13.6) | 5.7 (12.7) | 3.8 (10.4) | 5.8 (12.4) | 6.7 (13.1) | 6.0 (13.4) | 7.4 (12.2) | 6.0 (12.3) | 3.4 (8.3) | 6.4 (10.6) | 4.5 (9.5) |
| Conditional percentage of beds in Alzheimer SCU | 24.3 (16.8) | 25.1 (15.7) | 25.3 (14.8) | 23.6 (14.0) | 25.6 (13.2) | 24.7 (13.5) | 26.1 (16.0) | 22.6 (10.6) | 23.1 (13.6) | 19.5 (8.6) | 20.8 (8.2) | 20.9 (8.7) |
| Percentage residents with dementia | 45.6 (17.8) | 49.7 (18.5) | 51.1 (18.2) | 43.8 (18.0) | 47.4 (18.7) | 49.5 (18.3) | 43.8 (16.8) | 48.0 (16.2) | 50.3 (15.3) | 43.1 (13.8) | 39.7 (15.8) | 51.3 (12.3) |
| Total beds | 111.8 (77.7) | 109.8 (76.4) | 105.6 (75.1) | 105.6 (58.7) | 96.4 (48.4) | 100.7 (53.0) | 108.5 (52.9) | 104.8 (52.7) | 98.0 (45.4) | 85.6 (40.8) | 79.6 (37.6) | 75.5 (35.6) |
| Percentage occupancy | 91.2 (13.2) | 88.8 (13.4) | 87.2 (13.6) | 88.5 (13.1) | 87.3 (13.2) | 84.8 (14.0) | 90.3 (11.5) | 85.3 (14.5) | 84.9 (13.8) | 91.8 (7.7) | 88.2 (10.3) | 81.4 (14.8) |
| Percentage Medicaid primary payer | 56.3 (26.1) | 55.5 (25.2) | 50.3 (26.3) | 58.5 (26.4) | 52.7 (24.7) | 49.2 (23.9) | 53.7 (24.9) | 59.7 (22.7) | 56.7 (24.9) | 59.9 (13.2) | 57.4 (12.3) | 53.3 (16.3) |
| Percentage Medicare primary payer | 7.2 (13.8) | 10.0 (14.3) | 14.9 (16.8) | 9.4 (16.7) | 12.3 (14.0) | 16.4 (14.2) | 8.7 (10.5) | 11.1 (9.9) | 13.5 (11.2) | 4.7 (5.5) | 6.7 (6.5) | 10.1 (10.8) |
Source. Authors’ analysis of Online Survey Certification and Reporting (OSCAR) data.
Note. Chain size defined as small 5 to 10 NHs, medium 11 to 29 NHs, and large ≥30 NHs. NHs = nursing homes; SCU = specialty care unit.
Table 2 shows the regression results for chain affiliation across organization types and model specifications for the defined time periods, including 2-part logit and OLS regression coefficients, the expected value of Alzheimer disease SCU beds, and the combined marginal effect of chain affiliation. Compared with independent NHs, for-profit chain-affiliated NHs had an increased likelihood of designated beds for Alzheimer disease SCUs during 1996 to 2003. During this time period, the largest effect of chain affiliation was observed among for-profit NHs affiliated with large chains, indicating that if all for-profit independent NHs became affiliated with large chains, the prevalence of Alzheimer disease SCU beds would increase by 1.55 percentage points, P < .001 (39.9% relative increase). The statistically significant effect of chain affiliation within for-profit NHs persisted during 2004 to 2010 only for small and large chains. Notably, the decline by medium chains was not statistically different from independent NHs. Conversely, the only statistically significant effect of chain affiliation among nonprofit NHs was among medium chains from 1996 to 2003, with a combined marginal effect of 1.48, P < .001 (26.1% relative increase).
Table 2.
Effect of Chain Affiliation Versus Independent NHs on the Likelihood and Percentage of Beds Designated to Alzheimer Disease Specialty Care and the Percentage of Residents With Dementia, by Size and Profit Status.
| Size of affiliated chain |
||||||
|---|---|---|---|---|---|---|
| Small |
Medium |
Large |
||||
| 1996-2003 | 2004-2010 | 1996-2003 | 2004-2010 | 1996-2003 | 2004-2010 | |
| For-profit NHs | ||||||
| Number of NH-year observations | 48 856 | 41 820 | 51 189 | 45 520 | 65 649 | 55 873 |
| Model 1a: Designation of Alzheimer SCU (logit) | ||||||
| Chain affiliation vs independent | .24 (.07)*** | .28 (.07)*** | .22 (.07)*** | .10 (.07) | .51 (.05)*** | .40 (.06)*** |
| Total beds per NH | .01 (.001)*** | .01 (.001)*** | .01 (.001)*** | .01 (.001)*** | .01 (.0006)*** | .01 (.0006)*** |
| Percentage occupancy | .001 (.002) | .01 (.002)*** | −.001 (.002) | .005 (.002)** | .0006 (.001) | .008 (.002)*** |
| Percentage Medicaid primary payer | −.01 (.001)*** | −.01 (.002)*** | −.01 (.001)*** | −.005 (.002)*** | −.02 (.001)*** | −.01 (.002)*** |
| Percentage Medicare primary payer | .001 (.002) | −.004 (.003) | .003 (.002) | −.004 (.003) | −.002 (.002) | −.01 (.003)** |
| Percentage of residents with dementia | .03 (.002)*** | .04 (.002)*** | .03 (.002)*** | .04 (.002)*** | .03 (.001)*** | .04 (.001)*** |
| Model 1b: Designation of Alzheimer SCU (OLS) | ||||||
| Chain affiliation vs independent | −.56 (.95) | 1.19 (.99) | −.97 (.84) | −.19 (.89) | .27 (.71) | .52 (.72) |
| Total beds per NH | −.10 (.01)*** | −.10 (.01)*** | −.09 (.01)*** | −.10 (.01)*** | −.10 (.01)*** | −.09 (.01)*** |
| Percentage occupancy | .03 (.02) | .03 (.03) | .01 (.02) | −.05 (.02)** | .02 (.02) | .04 (.02)** |
| Percentage Medicaid primary payer | .01 (.03) | −.003 (.04) | .004 (.03) | −.003 (.04) | −.01 (.02) | −.02 (.03) |
| Percentage Medicare primary payer | .15 (.07)** | .04 (.07) | .13 (.07)** | .03 (.05) | .11 (.05)** | −.03 (.05) |
| Percentage of residents with dementia | .36 (.03)*** | .31 (.03)*** | .32 (.03)*** | .29 (.03)*** | .30 (.03)*** | .26 (.03)*** |
| Expected percentage of Alzheimer SCU beds | 3.39 (.10) | 3.73 (.11) | 3.31 (.10) | 3.59 (.10) | 3.88 (.09) | 4.01 (.10) |
| Combined marginal effect of chain affiliation | 0.59 (.23)** | 1.01 (.27)*** | .45 (.21)** | .25 (.23) | 1.55 (.20)*** | 1.28 (.21)*** |
| Model 2: Percentage of residents with dementia (OLS) | ||||||
| Chain affiliation vs independent | −.02 (.33) | .11 (.39) | −1.17 (.31)*** | −1.59 (.33)*** | −2.88 (.26)*** | −2.99 (.29)*** |
| Total beds per NH | −.02 (.003)*** | −.02 (.003)*** | −.02 (.003)*** | −.02 (.003)*** | −.02 (.002)*** | −.02 (.003)*** |
| Percentage occupancy | .06 (.01)*** | .08 (.01)*** | .07 (.01)*** | .08 (.01)*** | .05 (.01)*** | .06 (.01)*** |
| Percentage Medicaid primary payer | −.08 (.009)*** | −.12 (.01)*** | −.08 (.01)*** | −.13 (.01)*** | −.08 (.01)*** | −.11 (.01)*** |
| Percentage Medicare primary payer | −.31 (.01)*** | −.36 (.02)*** | −.32 (.01)*** | −.36 (.02)*** | −.22 (.01)*** | −.34 (.02)*** |
| Nonprofit NHs | ||||||
| Number of NH-year observations | 23 317 | 20 337 | 22 745 | 19 874 | 22 793 | 19 422 |
| Model 1a: Designation of Alzheimer SCU (logit) | ||||||
| Chain affiliation vs independent | −.02 (.12) | .14 (.11) | .37 (.12)*** | .25 (.12)** | .28 (.15)* | .23 (.15) |
| Total beds per NH | .01 (.0008)*** | .01 (.001)*** | .01 (.001)*** | .01 (.001)*** | .01 (.001)*** | .01 (.001)*** |
| Percentage occupancy | .01 (.003)*** | .02 (.003)*** | .01 (.003)*** | .02 (.003)*** | .01 (.003)*** | .02 (.003)*** |
| Percentage Medicaid primary payer | −.01 (.002)*** | −.01 (.002)*** | −.01 (.002)*** | −.01 (.002)*** | −.01 (.002)*** | −.01 (.002)*** |
| Percentage Medicare primary payer | −.003 (.003) | −.002 (.003) | −.002 (.003) | −.003 (.003) | −.002 (.003) | −.002 (.003) |
| Percentage of residents with dementia | .03 (.002)*** | .03 (.002)*** | .03 (.002)*** | .03 (.002)*** | .03 (.002)*** | .03 (.002)*** |
| Model 1b: Designation of Alzheimer SCU (OLS) | ||||||
| Chain affiliation vs independent | .02 (1.15) | .06 (1.02) | .23 (1.15) | −1.03 (1.07) | −.06 (1.10) | −2.10 (1.17)* |
| Total beds per NH | −.05 (.005)*** | −.05 (.005)*** | −.05 (.005)*** | −.05 (.005)*** | −.05 (.005)*** | −.05 (.005)*** |
| Percentage occupancy | −.05 (.03) | .04 (.03)* | −.05 (.03) | .01 (.02) | −.05 (.03) | .02 (.03) |
| Percentage Medicaid primary payer | −.03 (.02) | −.04 (.02)* | −.04 (.02)* | −.07 (.02)*** | −.03 (.02) | −.04 (.02) |
| Percentage Medicare primary payer | .15 (.05)*** | .12 (.05)** | .14 (.04)*** | .08 (.06) | .15 (.05)*** | .10 (.06) |
| Percentage of residents with dementia | .25 (.05)*** | .19 (.04)*** | .24 (.05)*** | .18 (.05)*** | .24 (.05)*** | .16 (.04)*** |
| Expected percentage of Alzheimer SCU beds | 5.48 (.17) | 6.09 (.18) | 5.68 (.17) | 6.18 (.18) | 5.48 (.17) | 6.00 (.18) |
| Combined marginal effect of chain affiliation | −.06 (.48) | .55 (.51) | 1.48 (.57)*** | .71 (.56) | 1.00 (.64) | .32 (.65) |
| Model 2: Percentage of residents with dementia (OLS) | ||||||
| Chain affiliation vs independent | −.14 (.60) | −.84 (.62) | −.08 (.65) | −.12 (.65) | −4.49 (.78)*** | −6.22 (.92)*** |
| Total beds per NH | .01 (.003)*** | .02 (.004)*** | .01 (.003)*** | .02 (.004)*** | .01 (.003)*** | .02 (.004)*** |
| Percentage occupancy | .14 (.02)*** | .14 (.02)*** | .14 (.02)*** | .14 (.02)*** | .13 (.02)*** | .12 (.02)*** |
| Percentage Medicaid primary payer | −.11 (.01)*** | −.12 (.02)*** | −.11 (.01)*** | −.12 (.01)*** | −.10 (.01)*** | −.11 (.01)*** |
| Percentage Medicare primary payer | −.35 (.02)*** | −.39 (.02)*** | −.35 (.02)*** | −.39 (.02)*** | −.34 (.02)*** | −.29 (.02)*** |
Note. Effects shown for models with the primary predictor of chain-affiliated versus independent NHs. Stratified models denoted in columns contain independent NHs and chains of that size small (5-10 NHs), medium (11-29 NHs), or large (≥30 NHs). Stratified models in rows considered NHs that were for-profit and nonprofit. All models adjusted for covariates presented, along with year and state fixed effects. Standard errors were clustered to account for repeated observations among NHs over time. Marginal effects from 2-part model (logit, OLS) presented at the mean of other covariates. NHs = nursing homes; SCU = specialty care unit; OLS = ordinary least squares.
significant at the 90%, 95%, and 99% confidence levels, respectively.
As shown by the individual model coefficients, chain affiliation increased the extensive margin rather than the intensive margin. Chain-affiliated NHs were more likely to designate any beds for Alzheimer disease SCUs, but did not designate more beds conditional upon any. Notably, the percentage of residents with Medicaid as the primary payer was associated with a small decrease in any Alzheimer disease SCU bed designation, an effect that was observed in nearly all models. The percentage of residents with Medicare as primary payer had no effect on any designation, but in several model specifications was associated with an increased number of beds designated for Alzheimer disease SCUs, particularly in the early period.
Table 2 also displays results from OLS regression modeling the percentage of residents with dementia. Chain affiliation was associated with lower percentage of dementia residents across all models, but statistically significant only among for-profit NHs affiliated with medium chains and large chains regardless of NH profit status. The largest effect was observed among for-profit NHs affiliated with large chains, where the percentage of residents with dementia was 4.5% and 6.2% lower than independent NHs during 1996 to 2003 and 2004 to 2010, respectively.
Discussion
Alzheimer disease SCU designation experienced a steady rise from 1996 until 2004, and then subsequently declined. Our analyses revealed 3 important findings. First, Alzheimer disease SCU designation varied by chain size, NH profit status, and time. Chain affiliation had little effect on the designation of beds for Alzheimer disease SCUs among nonprofit NHs, but was associated with greater designation among for-profit NHs, especially large chains during 1996 to 2004. Second, chain affiliation promoted designation of beds for Alzheimer disease SCU by increasing the likelihood of having at least one designated bed, but—conditional on any designated beds—did not result in a greater percentage of overall beds in a NH. Third, chain-affiliated NHs had lower percentages of residents with dementia. We conclude that organizational decisions to designate beds for Alzheimer disease SCUs may be related to marketing strategies to attract residents, which have fluctuated over time, but does not appear driven by demand.
Organizational strategies by for-profit and nonprofit NHs and the implications on quality of care and financial performance have been previously investigated in detail.14,19,26 Several conceptual frameworks and theories have been used to classify NHs by their strategic behavior, including Miles and Snow typology,27 Porter’s generic strategies,28 and entrepreneurial orientation.29 In general, nonprofit NHs are expected to be more customer focused, have better quality of care, and be more innovative.30 Although NHs vary in the autonomy and ability to make decisions such as offering beds designated within SCUs, we expected commonalities among for-profits versus nonprofits and by chain affiliation and chain size. Although for-profit NHs were the dominant organizational type, we observed a greater likelihood of nonprofit NHs to designate beds for Alzheimer disease SCU than for-profit NHs. However, nonprofit chain-affiliated NHs were generally more similar to independent NHs relative to for-profits, since only medium chains during 1996 to 2003 showed a statistically significant difference. Among for-profit NHs, chain affiliation promoted the designation of beds for Alzheimer disease SCUs. In particular, among for-profit NHs, it was those affiliated with large chains that were the most likely to designate beds for Alzheimer disease SCUs. The use of Alzheimer disease SCUs may fulfill different strategic objectives based on profit status and chain affiliation and chain size. For example, NHs affiliated with large chains may have greater resources to invest in Alzheimer disease SCUs given their size and ability to aggressively pursue different sources of revenue.19,31
The magnitude of the association between chain affiliation and Alzheimer disease SCU bed designation decreased over time for all but small chains, regardless of NH profit status. In fact, while large and medium chains retreated, small chains appeared to increase Alzheimer disease SCU designation. The most dramatic decline in the effect of chain affiliation was among medium chains. Relative to independent NHs, medium chains were more likely to designate beds for Alzheimer disease SCUs regardless of NH profit status from 1996 to 2003. However, in the latter time period, the magnitude of the effect diminished substantially and was similar to independent NHs. It is not clear whether there are unique characteristics of medium chains or how this organizational grouping may have changed over time that would explain this observation. It was beyond the scope of our current analysis to measure competition in the current analysis, but differences observed across chain size may indicate responses to competition and attempts to gain market access. Greater market competition increases the likelihood of SCU designation, but to the extent this occurs over time and by chain size has not been investigated.32 Further research should investigate market characteristics and competition to determine what pressures NH chains are responding to in the decision to provide SCUs. In particular, the source and response to competition for certain types of residents (eg, private pay) could help explain decisions by NH organizational type.
Heterogeneity in state regulations and variations in the interpretation of the definition of what constitutes an SCU has prevented definitive demonstration of care quality improvements as a result of designation.23 Therefore, it is not clear whether NHs provide care in SCUs with the intention of improving quality of care. However, combining residents with similar care needs together in a unit may improve the efficiency of care, resulting in improved financial performance. As a result, the designation of additional SCU beds should increase with the percentage of dementia residents in the NH. We did not observe this effect; although the percentage of residents with dementia was associated with increased Alzheimer disease SCU bed designation generally, our analyses showed chain affiliation was inversely associated with the percentage of dementia residents. This suggests chains are not designating beds to increase the capacity to care for more dementia residents, which has grown in demand. It could be that the decision to designate beds to an SCU is a strategy to maximize private-pay revenue, as previously suggested.33,34 Indeed, although chain affiliation had the greatest effect among for-profit NHs affiliated with large chains, we observed an inverse relationship with the percentage of Medicaid and Medicare payers. The use of SCUs could be one way NH chains develop tailored services and programs to improve marketing and respond to customer preferences, particularly among residents who are private payers.35 Given our finding that chains increase the likelihood of having any Alzheimer disease SCU beds, but not the number of beds, we posit designation is done as a way to market services targeted at the needs of a specific population—namely, private-pay residents with Alzheimer disease or dementia. Furthermore, large chains and for-profit NHs are expected to more aggressively pursue innovative services to increase revenue consistent with a resource dependence perspective.19,36 This adaptive response has been previously observed with the implementation of subacute/rehabilitation care.37
We must note some limitations of our analysis. Outside of NH deficiencies, all OSCAR data are self-reported by the NH and could be subject to errors in reporting. Due to the lack of a consistent definition of a SCU, the question asked by CMS could be subject to differences in interpretation. Although some states have sought to specify care attributes of specialty Alzheimer care, we could find no uniform distinctions used nationwide. In addition, the directions on CMS Form 671 requesting information about SCU beds specify that “they need not be certified or recognized by regulatory authorities.”9 Chain affiliations could have been misclassified, again because we have relied on self-reports of chain affiliation from text entered in the OSCAR data. Moreover, the question in Form 671 asks about “Multi-facility membership” which can mean a health care system consisting of NHs and hospitals or other agencies, and not necessarily what “chains” would mean in a corporate framework, which we had assumed. However, extensive steps were taken to reduce miscoding resulting from typographical errors, abbreviations, and alternative names. Furthermore, the accuracy of the percentage of residents with dementia could be subject to self-reporting errors and may have varied over time as recognition of dementia has changed. We were unable to consider differences based on subtypes or severity of dementia.
Conclusions
We observed a lack of sustained growth and an eventual decline in the prevalence of NHs with Alzheimer disease SCUs during the late 1990s and 2000s. Across our study period, it is evident that chain-affiliated NHs were more likely to adopt SCUs. However, medium and large chains drove not only the pattern of increasing prevalence over time but also the decreasing prevalence over the latter part of the study period. Differences across chain size and NH profit status suggest decisions to provide this care may be related to more detailed competitive factors beyond the scope of our current analyses. Future research efforts should elucidate the relationship of SCU designation and financial performance, both as a predictor and outcome following creation of an SCU.
Supplemental Material
Supplemental material, Combined_Model_for_SCU_Revision_tables for Nursing Home Chain Affiliation and Its Impact on Specialty Service Designation for Alzheimer Disease by Justin Blackburn, Qing Zheng, David C. Grabowski, Richard Hirth, Orna Intrator, David G. Stevenson and Jane Banaszak-Holl in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the National Institute on Aging (NIA) R01-AG042418: Health Consequences of Corporate Changes in the Nursing Home Industry. Additional support was provided by the Agency for Healthcare Research and Quality (K12 HS023009) to JB.
ORCID iD: Justin Blackburn  https://orcid.org/0000-0002-1811-2081
https://orcid.org/0000-0002-1811-2081
References
- 1. Langa KM, Larson EB, Crimmins EM, et al. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177(1):51-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1-2):125-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63-75. [DOI] [PubMed] [Google Scholar]
- 4. Gaugler J, Yu F, Krichbaum K, Wyman JF. Predictors of nursing home admission for persons with dementia. Med Care. 2009;47(2):191-198. [DOI] [PubMed] [Google Scholar]
- 5. Alzheimer’s Association. 2017 Alzheimer’s disease facts and figures. Alzheimers Dement. 2017;13(4):325-373. [Google Scholar]
- 6. Zinn JS, Mor V. Nursing home special care units: distribution by type, state, and facility characteristics. Gerontologist. 1994;34(3):371-377. [DOI] [PubMed] [Google Scholar]
- 7. Lai CKY, Yeung JHM, Mok V, Chi I. Special care units for dementia individuals with behavioural problems. Cochrane Database Syst Rev. 2009;7(4):CD006470. [DOI] [PubMed] [Google Scholar]
- 8. Bellelli G, Frisoni GB, Bianchetti A, et al. Special care units for demented patients: a multicenter study. Gerontologist. 1998;38(4):456-462. [DOI] [PubMed] [Google Scholar]
- 9. Department of Health and Human Services. Long Term Care Facility Application for Medicare and Medicaid. Centers for Medicare and Medicaid Services; Date unknown. https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/Downloads/CMS671.pdf. Accessed August 18, 2017 [Google Scholar]
- 10. Banaszak-Holl J, Berta WB, Bowman DM, Baum JAC, Mitchell W. The rise of human service chains: antecedents to acquisitions and their effects on the quality of care in US nursing homes. Manage Decis Econ. 2002;23:261-282. [Google Scholar]
- 11. Grabowski DC, Hirth RA, Intrator O, et al. Low-quality nursing homes were more likely than other nursing homes to be bought or sold by chains in 1993-2010. Health Aff. 2016;35(5):907-914. [DOI] [PubMed] [Google Scholar]
- 12. Grabowski DC, Stevenson DG. Ownership conversion and nursing home performance. Health Serv Res. 2008;43(4):1184-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein D. Does investor-ownership of nursing homes compromise the quality of care? Am J Public Health. 2001;91:1452-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Serv Res. 2012;47(1):106-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kai Y, Li Y, Intrator O, Stevenson D, Hirth R, Grabowski D, Banaszak-Holl J. Do nursing home chain size and proprietary status affect experiences with care? Med Care. 2016;54:229-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O’Neill C, Harrington C, Kitchener M, Saliba D. Quality of care in nursing homes: an analysis of the relationships among profit, quality, and ownership. Med Care. 2003;41:1318-1330. [DOI] [PubMed] [Google Scholar]
- 17. US Government Accountability Offices. CMS’s Specific Focus Facility Methodology Should Better Target the Most Poorly Performing Facilities Which Tend to Be Chain Affiliated and For-Profit. GAO-09-689. Washington, DC: GAO; 2009. http://www.gao.gov/new.items/d09689.pdf. Accessed 2017. [Google Scholar]
- 18. Kamimura A, Banaszak-Holl J, Berta W, Baum JAC, Weigelt C, Mitchell W. Do corporate chains affect quality of care in nursing homes? the role of corporate standardization. Health Care Manage Rev. 2007;32(2):168-178. [DOI] [PubMed] [Google Scholar]
- 19. Weech-Maldonado R, Laberge A, Pradhan R, Johnson CE, Yang Z, Hyer K. Nursing home financial performance: the role of ownership and chain affiliation. Health Care Manage Rev. 2012;37(3):235-245. [DOI] [PubMed] [Google Scholar]
- 20. Banaszak-Holl J, Zinn JS, Mor V. The impact of market and organizational characteristics of nursing care facility service innovation: a resource dependency perspective. Health Serv Res. 1996;31(1):97-117. [PMC free article] [PubMed] [Google Scholar]
- 21. Weech-Maldonado R, Neff G, Mor V. Does quality of care lead to better financial performance? the case of the nursing home industry. Health Care Manage Rev. 2003;28(3):201-216. [DOI] [PubMed] [Google Scholar]
- 22. Weech-Maldonado R, Neff G, Mor V. The relationship between quality of care and financial performance in nursing homes. J Health Care Finance. 2003;29(3):48-60. [PubMed] [Google Scholar]
- 23. Gruneir A, Lapane KL, Miller SC, Mor V. Does the presence of a dementia special care unit improve nursing home quality? J Aging Health. 2008;20(7):837-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing home staffing and its relationship to deficiencies. J Gerontol B Psychol Sci Soc Sci. 2000;55(5):S278-S287. [DOI] [PubMed] [Google Scholar]
- 25. Hirth RA, Zheng Q, Grabowski DC, Stevenson DG, Intrator O, Banaszak-Holl J. The effects of chains on the measurement of competition in the nursing home industry [published online ahead of print April 1, 2017]. Med Care Res Rev. Accessed November 29, 2017 doi: 10.1177/1077558717701771. [DOI] [PubMed] [Google Scholar]
- 26. Comondore VR, Devereaux PJ, Zhou Q, et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. BMJ. 2009;339:b2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Miles RE, Snow CC. Organizational Strategy, Structure, and Process. New York, NY: McGraw-Hill; 1978. [PubMed] [Google Scholar]
- 28. Porter M. Competitive Strategy. New York, NY: Free Press; 1980. [Google Scholar]
- 29. Davis J, Brannon D, Zinn J, Mor V. Strategy, structure, and performance in nursing facilities. Adv Health Care Manag. 2000;2(1):291-313. [Google Scholar]
- 30. Davis JA, Marino LD, Aaron JR, Tolbert CL. An examination of entrepreneurial orientation, environmental scanning, and market strategies of nonprofit and for-profit nursing home administrators. Nonprofit Volunt Sect Q. 2011;40(1):197-211. [Google Scholar]
- 31. Castle NG. Innovation in nursing homes: which facilities are the early adopters. Gerontologist. 2001;41(2):161-172. [DOI] [PubMed] [Google Scholar]
- 32. Gruneir A, Lapane KL, Miller SC, Mor V. Long-term care market competition and nursing home dementia special care units. Med Care. 2007;45(8):739-745. [DOI] [PubMed] [Google Scholar]
- 33. Castle NG. Impact of establishing an Alzheimer’s special care unit in a nursing home on facility occupancy and payer mix. Alzheimer Dis Assoc Disord. 2007;21(3):191-198. [DOI] [PubMed] [Google Scholar]
- 34. Castle NG. Special care units and their influence on nursing home occupancy characteristics. Health Care Manage Rev. 2008;33(1):79-91. [DOI] [PubMed] [Google Scholar]
- 35. Calhoun JG, Banaszak-Holl J, Hearld LR. Current marketing practices in the nursing home sector. J Healthc Manag. 2006;51(3):185-202. Accessed November 29, 2017 [PubMed] [Google Scholar]
- 36. Pfeffer J, Salancik GR. The External Control of Organizations: A Resource Dependence Perspective. New York, NY: Harper & Row; 1978. [Google Scholar]
- 37. Zinn JS, Mor V, Feng Z, Intrator O. Doing better to do good: the impact of strategic adaptation on nursing home performance. Heath Serv Res. 2007;42(3):1200-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Combined_Model_for_SCU_Revision_tables for Nursing Home Chain Affiliation and Its Impact on Specialty Service Designation for Alzheimer Disease by Justin Blackburn, Qing Zheng, David C. Grabowski, Richard Hirth, Orna Intrator, David G. Stevenson and Jane Banaszak-Holl in INQUIRY: The Journal of Health Care Organization, Provision, and Financing