Abstract
Background:
Pathology of the long head of the biceps tendon is a well-known cause of shoulder pain that is commonly managed with arthroscopic suprapectoral biceps tenodesis when conservative treatment fails.
Purpose:
To present an arthroscopic knotless suprapectoral biceps tenodesis technique known as “Loop ’n’ Tack” tenodesis and to report the clinical outcomes of patients with a minimum 2 years of follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective review of all patients who had undergone Loop ’n’ Tack tenodesis between January 2009 and May 2014 was completed. Charts were reviewed, and patients were contacted for demographic data, time from surgery, concomitant procedures, and workers’ compensation status, as well as visual analog scale for pain, American Shoulder and Elbow Surgeons (ASES), Single Assessment Numeric Evaluation, and University of California, Los Angeles (UCLA) scores.
Results:
Complete follow-up evaluations were performed for 59 of 68 patients (87%). Mean follow-up was 43 months. A majority (88%) of patients had at least 1 additional procedure performed at the time of biceps tenodesis. The mean ASES shoulder score improved from 42.6 preoperatively to 91.0 postoperatively (P < .001), and 54 of 59 patients (91.5%) had a good/excellent outcome, with a UCLA shoulder score >27 and ASES shoulder score >70. Three patients (5%) reported biceps cramping pain with overuse, and 2 (3.3%) reported intermittent anterior shoulder pain. No patients had developed a “Popeye” deformity at final clinical examination, and 97% reported that they were overall satisfied with the procedure.
Conclusion:
The Loop ’n’ Tack tenodesis technique results in a high rate of patient satisfaction, significant improvement in shoulder outcome scores, and a low incidence of postoperative pain, with no reoperations for biceps-related pathology.
Keywords: arthroscopic, biceps tenodesis, surgical technique, clinical outcomes
Pathology of the long head of the biceps tendon (LHB) is a well-established source of shoulder pain caused by various pathologies, such as inflammatory and degenerative tendinitis, chronic tendinopathy, partial tearing, subluxation, and dislocation of the tendon.2,5 Patient factors such as age, activity level, body habitus, occupation, sporting activities, medical comorbidities, and concomitant shoulder pathology must be considered to determine the best course of treatment.8 Nonoperative treatment (eg, physical therapy, activity modifications, anti-inflammatory medications, steroid injections) can be effective, although in cases refractory to conservative measures, surgical intervention has been shown to be safe and effective.1,13
Biceps tenotomy and tenodesis are the most common procedures performed for LHB lesions.6,9 Biceps tenotomy is a relatively simple and reproducible arthroscopic procedure that provides predictable pain relief with minimal postoperative rehabilitation.13 In general, biceps tenotomy is indicated for patients aged >60 years who do not perform manual labor or other high-demand activities.1,6,9,13 The disadvantages of biceps tenotomy include the risk of cosmetic deformity (ie, “Popeye” sign), fatigue with resisted elbow flexion and supination, and biceps muscle cramping.1,6,8,9,13 While there is no consensus in the literature regarding tenotomy versus tenodesis, biceps tenodesis has become the preferred technique to manage pathology of the LHB in younger, more active patients, who wish to avoid a cosmetic deformity despite longer rehabilitation time and increased technical difficulty.1,6,8,9,13,14
Biceps tenodesis can be performed through an open or an arthroscopic approach, and the tendon may be anchored in a proximal suprapectoral (above the groove), suprapectoral (below the groove), or distal subpectoral position.1,13,14 Early reports of failures with arthroscopic “above the groove” tenodesis techniques were attributed to persistent tenosynovitis and motion of the LHB that remains within the bicipital groove as a pain generator.3,12 Distal subpectoral fixation requires the use of an additional incision, and higher complication rates have been reported.7
The purpose of this study was to present an arthroscopic technique for tenodesis of the LHB above the bicipital groove that reduces tension on the LHB and can decrease the incidence of groove pain while providing outcomes comparable with those of previously described techniques. This “Loop ’n’ Tack” technique was developed as a simple way to efficiently perform tenodesis of the LHB within the glenohumeral joint space without having to locate the LHB in the subacromial space by taking down the transverse humeral ligament. We hypothesized that Loop ’n’ Tack tenodesis will eliminate anterior groove pain with minimal risk of LHB rupture and Popeye deformity. The clinical outcomes of a cohort with a minimum of 2-year follow-up are provided.
Methods
Loop ’n’ Tack Tenodesis: Surgical Technique
This technique can be performed in the beach-chair or lateral position, based on surgeon preference. Diagnostic arthroscopy is performed through a standard posterior portal. After pathology of the LHB is identified, an 18-gauge spinal needle is used to localize the anterior portal within the rotator interval directly over the biceps tendon, and a cannula is placed for passing suture.
A looped nonabsorbable FiberSnare suture (Arthrex) is passed around the biceps tendon (Figure 1). Externally, the free tail end is then dunked through the looped end, and the tail is pulled to cinch the loop over the biceps tendon near its insertion at the superior labrum (Figure 2). The free end is then passed into the joint (Figure 3). A tissue penetrator is then passed through the center of the biceps tendon, distal to the cinched loop, and the free end is grasped and pulled through the tendon (Figure 4), tacking the loop in place (Figure 5). The biceps tendon is cut at its insertion (Figure 6). The free end of the suture is then loaded into a PushLock suture anchor (Arthrex). A pilot hole is drilled at the most distally visualized portion of the intra-articular bicipital groove, just above the subscapularis tendon. The anchor is then seated with all slack taken out of the suture, allowing the tendon to translate distally within the bicipital groove, “tacking” the biceps in place (Figure 7). A cadaveric study demonstrated that the biceps tendon is translated distally a mean 30 mm with this technique (Kelly B, Schimoler P, Kharlamov A, Miller M, Akhavan S. “Biceps Tendon Motion Within the Bicipital Groove Before and After Suprapectoral, Intra-articular Tenodesis.” Presented at the AOSSM Annual Meeting, 2017).
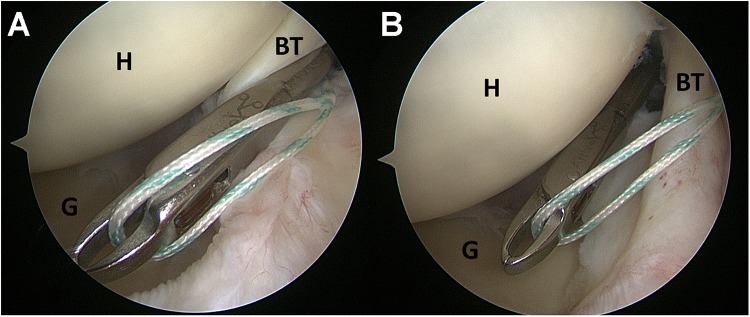
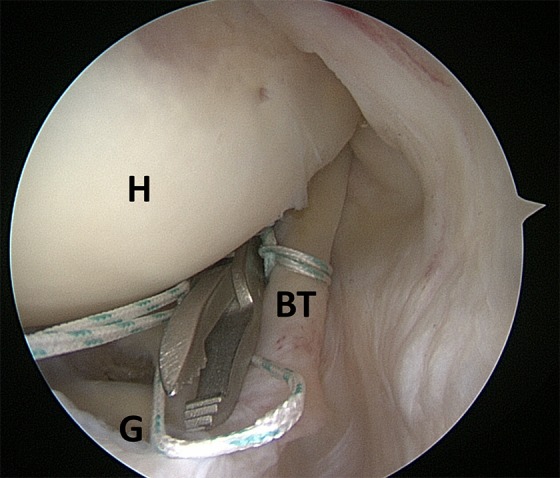
Figure 1.
Arthroscopic image of a left shoulder in a lateral decubitus position with a 30° arthroscope from the posterior portal (same orientation and position for all figures). (A) The end of a looped suture is passed around the biceps tendon (BT) from the superior labrum to the BT. (B) The suture is then pulled from inferior to the BT to complete passage around it. G, glenoid; H, humerus.
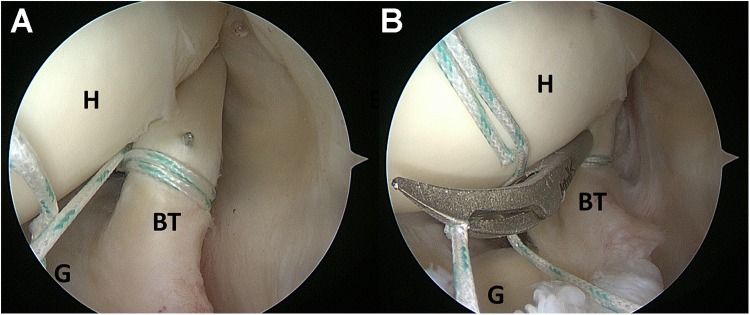
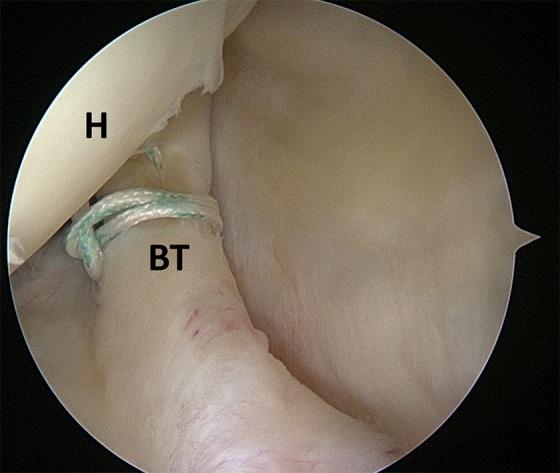
Figure 2.
The free end of the suture has been passed through the looped end and is cinched to the biceps tendon (BT) close to its insertion at the superior labrum. G, glenoid; H, humerus.
Figure 3.
The free end of the suture is being passed into the joint with excess slack. BT, biceps tendon; G, glenoid; H, humerus.
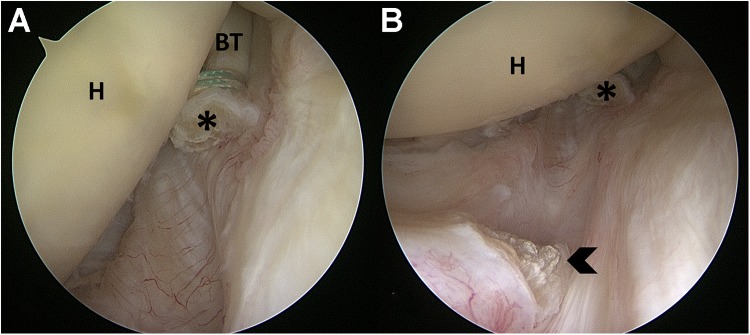
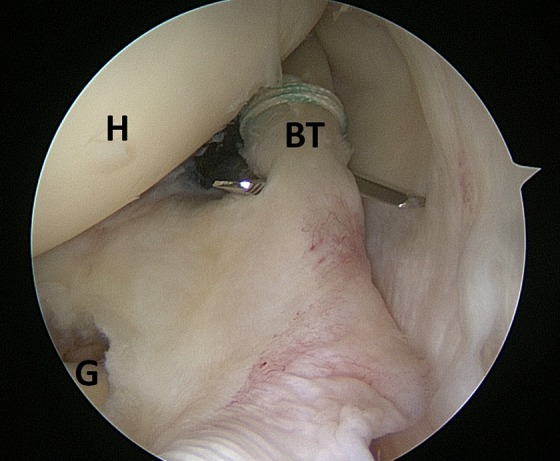
Figure 4.
(A) An arthroscopic tissue penetrator is being passed through the biceps tendon (BT). (B) The grasping mechanism of the tissue penetrator is used to grab the free end of the suture and pull it through the tendon. G, glenoid; H, humerus.
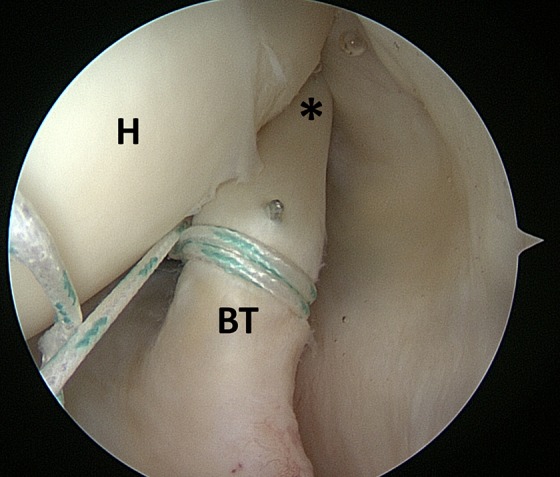
Figure 5.
The suture has been looped around the biceps tendon (BT) and is now tacked in place just distal to the loop. H, humerus.
Figure 6.
The biceps tendon (BT) is cut with a curved arthroscopic scissor at its insertion on the superior labrum, with care to not cut the suture. G, glenoid; H, humerus.
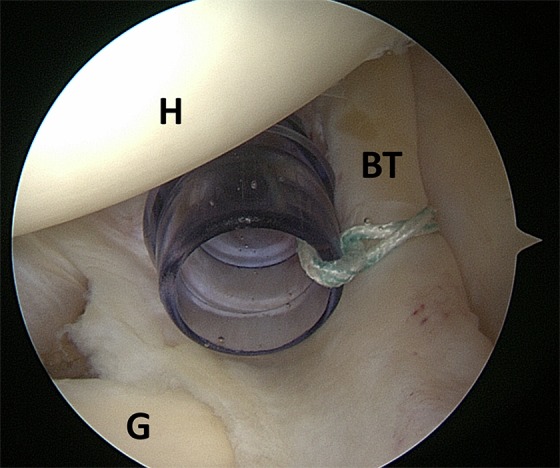
Figure 7.
(A) The biceps tendon (BT) has been secured with a suture anchor at the most distally visualized portion of the intra-articular bicipital groove to tack the BT in place. The cut end of the BT is marked with asterisks. (B) The cut end of the BT is seen distally translated from its original insertion at the superior labrum, marked with a chevron. H, humerus.
This technique can be performed with an intact rotator cuff. In cases where the rotator cuff is torn (supraspinatus or subscapularis), the suture can be incorporated into a SwiveLock anchor (Arthrex) that is used in the rotator cuff repair construct.
Postoperative Rehabilitation Protocol
In a cadaveric biomechanical study, there was minimal motion of the biceps tendon within the bicipital groove with shoulder and elbow range of motion via this technique (Kelly et al., “Biceps Tendon Motion”). As such, in cases of isolated biceps tenodesis, patients are allowed to perform immediate shoulder and elbow range of motion. For comfort, they are placed in a sling for 1 week. When this technique is combined with another procedure (eg, rotator cuff repair), the other procedure typically dictates the rehabilitation protocol.
Clinical Evaluation
After approval by an institutional review board, a retrospective chart review was completed of all patients who had undergone Loop ’n’ Tack tenodesis by the senior author (S.A.) between January 2009 and May 2014. With Current Procedural Terminology filters, 68 patients were identified. Each chart was reviewed for demographic data, time to follow-up, concomitant procedures, workers’ compensation status, preoperative visual analog scale (VAS) for pain and American Shoulder and Elbow Surgeons (ASES) scores, treatment failure, and postoperative complications. Treatment failure was defined as rupture of the tenodesis, resulting in a Popeye deformity or biceps cramping pain, or persistent anterior shoulder “groove” pain. Patients were excluded if any portion of the surgery was performed open or if they were not available for a follow-up phone interview.
Patients were then contacted by phone for a follow-up survey, and the VAS, ASES, Single Assessment Numeric Evaluation (SANE), and University of California, Los Angeles (UCLA) shoulder scores were collected. Patients who complained of shoulder pain were brought in for a follow-up clinical evaluation.
Statistical Analysis
Statistical analysis was performed with Microsoft Excel. The VAS, ASES, SANE, and UCLA scores were compared with Mann-Whitney U test for nonparametric data sets.
Results
Table 1 summarizes the patient demographic data. The age of patients ranged from 26 to 76 years, with a mean of 51.6 years. Follow-up surveys were completed by 59 of the 68 patients (87%). The mean follow-up was 43 months (range, 24-79 months). In this cohort of patients, indications for biceps tenodesis included partial-thickness tears of the LHB, symptomatic LHB tendinitis with inflamed LHB seen at diagnostic arthroscopy, chronic LHB tendinopathy with thickened LHB seen at diagnostic arthroscopy, type 2 and type 4 SLAP (superior labrum anterior-posterior) tears, medially subluxated or dislocated LHB with associated subscapularis tear, and failed SLAP repair. Of the 59 patients, 52 (88%) had at least 1 additional procedure at the time of biceps tenodesis (Table 2).
TABLE 1.
Demographic Data
| Patient Characteristic | Mean ± SD or n (%) |
|---|---|
| Age, y | 51.6 ± 9.8 |
| Male | 34 (57.6) |
| Dominant arm | 41 (69.4) |
| Tobacco users | 18 (30.5) |
| Workers’ compensation | 10 (16.9) |
TABLE 2.
Concomitant Surgical Proceduresa
| Procedure | n (%) |
|---|---|
| Rotator cuff | |
| Repair | 28 (47.5) |
| Cuff debridement | 6 (10.2) |
| Subscapularis repair | 12 (20.3) |
| Labrum | |
| Repair | 2 (3.3) |
| Debridement | 28 (47.5) |
| SLAP repair | 3 (5.0) |
| Acromioplasty | 33 (55.9) |
| Distal clavicle excision | 27 (45.8) |
| Humeral head microfracture | 1 (1.7) |
aPatients had multiple concomitant procedures (ie, total >100%). SLAP, superior labrum anterior-posterior.
Table 3 summarizes the pre- and postoperative outcome scores. Of 59 patients, 54 (91.5%) had a good/excellent result, with a UCLA score >27 and ASES score >70. At final clinical follow-up, no patients developed a Popeye deformity. Three patients (5%) reported biceps cramping pain with overuse. Two patients (3.3%) cited intermittent anterior shoulder pain related to impingement symptoms and were successfully treated with subacromial steroid injections and physical therapy. Only 1 patient required a return to the operating room for a failed massive rotator cuff repair, for an overall reoperation rate of 1.7%. This patient had an intact biceps tenodesis at the time of surgery. The remaining 58 of 59 (97%) patients reported that they were satisfied overall with the procedure and would have the operation again.
TABLE 3.
Outcome Scoresa
| Outcome Score | Mean ± SD | Minimum | Median | Maximum | P Value |
|---|---|---|---|---|---|
| ASES | |||||
| Preoperative | 42.6 ± 15.6 | 6.7 | 46.6 | 66.7 | |
| Postoperative | 91.0 ± 13.3 | 51.7 | 100 | 100 | <.001 |
| VAS for pain | |||||
| Preoperative | 6.8 ± 2.0 | 1 | 7 | 10 | |
| Postoperative | 1.1 ± 1.7 | 0 | 0 | 6 | <.0001 |
| SANE: postoperative | 93.3 ± 11.3 | 50 | 100 | 100 | |
| UCLA: postoperative | 32.4 ± 4.0 | 18 | 35 | 35 |
aASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; UCLA, University of California, Los Angeles; VAS, visual analog scale.
In a subgroup analysis comparing patients who had rotator cuff repair or labrum repair at the time of biceps tenodesis versus patients who did not have either, there were no significant differences in preoperative VAS or ASES scores or postoperative outcome scores (Table 4).
TABLE 4.
Outcome Scores in Subgroup Analysisa
| Rotator Cuff Repair or Labrum Repair, n (%) or Mean ± SD | |||
|---|---|---|---|
| Yes | No | P Value | |
| Patients | 36 (61) | 23 (39) | |
| ASES | |||
| Preoperative | 41.5 ± 15.0 | 44.3 ± 16.8 | .260 |
| Postoperative | 91.6 ± 13.3 | 90.0 ± 14.0 | .333 |
| VAS for pain | |||
| Preoperative | 6.8 ± 2.0 | 6.8 ± 2.2 | .495 |
| Postoperative | 1.0 ± 1.5 | 1.3 ± 2.0 | .266 |
| SANE: postoperative | 94.8 ± 10.2 | 91.0 ± 12.7 | .116 |
| UCLA: postoperative | 32.6 ± 3.8 | 32.0 ± 4.3 | .269 |
aASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Ten patients with workers’ compensation were included in this cohort. In a subgroup analysis based on workers’ compensation status, we found statistically significantly worse postoperative VAS, ASES, SANE, and UCLA scores in the workers’ compensation group (Table 5).
TABLE 5.
Outcome Scores in Subgroup Analysisa
| Workers’ Compensation, n (%) or Mean ± SD | |||
|---|---|---|---|
| No | Yes | P Value | |
| Patients | 49 (83) | 10 (17) | |
| ASES | |||
| Preoperative | 43.9 ± 15.6 | 36.1 ± 14.7 | .111 |
| Postoperative | 92.5 ± 12.5 | 83.2 ± 15.0 | .028 |
| VAS for pain | |||
| Preoperative | 6.9 ± 2.1 | 6.6 ± 2.0 | .346 |
| Postoperative | 0.9 ± 1.6 | 2.2 ± 1.9 | .020 |
| SANE: postoperative | 94.8 ± 10.5 | 86.3 ± 12.9 | .026 |
| UCLA: postoperative | 32.9 ± 3.7 | 30.0 ± 4.8 | .019 |
aASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Discussion
LHB tenodesis is widely accepted as treatment for a variety of LHB pathologies; however, the ideal technique and location for tenodesis remain controversial in the literature. Some authors believe that removal of the majority of the LHB and its associated tenosynovium from the bicipital groove is important to avoid persistent anterior shoulder pain.3,5,12 Sanders et al12 reported a reoperation rate of 45% following LHB tenodesis in a proximal “above the groove” position, versus 8% below the bicipital groove. They also noted higher reoperation rates if the biceps sheath was left intact as compared with tenodesis in which the sheath was released. These authors suggested that the higher failure rates after proximal LHB tenodesis are caused by persistent tenosynovitis and pain generated by the LHB within the bicipital groove.
Friedman et al5 similarly reported a reoperation rate of 35.7% after proximal arthroscopic tenodesis, as opposed to 2.7% after distal open tenodesis below the bicipital groove. They also found a significantly lower reoperation rate if the biceps sheath was released versus if it was left intact, and they attributed failures to persistent inflammation and irritation of the LHB within the bicipital groove.
Other investigators found no increase in residual anterior shoulder pain with suprapectoral “above the groove” tenodesis. With the largest cohort, Brady et al4 reported on 1083 patients who underwent a proximal “above the groove” LHB tenodesis at the articular margin. They reported significant improvement in objective and subjective outcome scores as well as pain scores. They documented an overall reoperation rate of 4.1%, although only 4 cases (0.4%) were for biceps-related issues. These authors preferred this technique for the ease of the procedure, the ability to use the LHB tenodesis construct in the repair of other shoulder pathology, the ability to appropriately tension the LHB, and the lack of significant complications.
In our current study, we found an overall reoperation rate of 1.7% (related to a recurrent rotator cuff tear) and no reoperations for biceps-related pathology. Regarding persistent shoulder pain after proximal tenodesis, only 2 patients (3.3%) reported intermittent anterior shoulder pain (related to impingement symptoms) and were successfully treated with subacromial steroid injections and physical therapy. Additionally, 3 patients (5%) experienced biceps cramping with overuse. Overall, we found a significant improvement in pain, with a mean postoperative VAS score of 1.1, which is consistent with the existing literature.1,4
In comparison with other described techniques, the primary advantage of Loop ’n’ Tack tenodesis is the technical ease of the procedure. This technique is performed entirely with visualization from the posterior portal in the glenohumeral joint, in contrast to other arthroscopic techniques, which require visualization from the subacromial space with extensive debridement.7 This can be performed with an intact rotator cuff, or the suture can be incorporated as part of a medial row anchor for supraspinatus or subscapularis tendon repair, making this a versatile procedure.
Previous authors emphasized the importance of appropriate tensioning of the LHB.4 In a biomechanical study of this technique, the LHB was actually taken off of tension, and the tendon was distalized a mean 30.5 mm (Kelly et al., “Biceps Tendon Motion”). This amount of distalization may translate the inflamed portion of the LHB out of the groove. Additionally, we found minimal motion of the LHB within the groove, thus minimizing the risk of recurrent inflammation and pain. Clinically, we found that this amount of distalization does not result in a cosmetic Popeye deformity and that it has a low risk of biceps cramping pain (5%) with overuse. However, should the surgeon wish to minimize the amount of distalization of the biceps, this can easily be done by grasping the tendon closer to the top of the subscapularis (Figure 8). Doing so will slightly increase the tension of the biceps, as compared with that of the Loop ’n’ Tack technique described here. However, given that the tendon is not placed in a bony tunnel, overtensioning of the biceps would be unlikely even if it is grabbed more distally.
Figure 8.
Arthroscopic image of a left shoulder in a lateral decubitus position with a 30° arthroscope from the posterior portal. The tissue penetrator may be passed through the biceps tendon (BT) in a more distal position (asterisk) to secure the BT without distalizing it. H, humerus.
In this series, we did not experience any postoperative complications or ruptures of the tenodesis. This is an additional advantage of an all-arthroscopic technique compared with open subpectoral tenodesis, in which complications such as humeral fractures, musculocutaneous nerve palsy, brachial plexopathy, and wound infections have been reported.1,10,11 Additionally, while this series included only patients who successfully underwent Loop ’n’ Tack tenodesis, there is a potential risk of intraoperative suture pullout from the tendon. In such cases, because the entirety of the LHB is preserved with this technique, arthroscopic “below the groove” suprapectoral tenodesis or an open subpectoral tenodesis remains as a salvage option.
There are several weaknesses in the current study, including its retrospective nature, the participation of a single surgeon, and the conducting of final follow-up surveys via phone interview. To minimize the risk of bias, all phone interviews were conducted by the first author (R.A.D.), who was not the treating surgeon. Additionally, all patients who reported pain were brought in for clinical evaluation. While no patients had developed a Popeye deformity at final clinical follow-up and were questioned specifically about this during phone interview, it is possible that patients may have unrecognized cosmetic deformity. Thirteen percent of patients were lost to follow-up, which may also introduce selection bias. Last, there were confounding variables in the patient outcomes, as 88% had concomitant pathology addressed at the time of LHB tenodesis. This likely had a substantial impact on the improvement in the patient-reported outcome scores that were observed. For this reason, we specifically reported on the postoperative incidence of anterior groove pain and cosmetic Popeye deformity, as the focus of this study was to assess the effectiveness of Loop ’n’ Tack tenodesis in avoiding the negative sequelae of biceps tenotomy.
Conclusion
The Loop ’n’ Tack biceps tenodesis technique results in a high rate of patient satisfaction, significant improvement in shoulder outcome scores, and a low incidence of postoperative pain, with no reoperations for biceps-related pathology.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: D.N. has received educational support from Smith & Nephew and CDC Medical and hospitality payments from Zimmer Biomet and Arthrex. J.M.P. is a consultant for Arthrex and has been a paid speaker/presenter for Arthrex and Zimmer Biomet. S.A. is a consultant for Arthrex and has been a paid speaker/presenter for Arthrex.
Ethical approval for this study was obtained from the Allegheny Health Network.
References
- 1. Abraham VT, Tan BH, Kumar VP. Systematic review of biceps tenodesis: arthroscopic versus open. Arthroscopy. 2016;32(2):365–371. [DOI] [PubMed] [Google Scholar]
- 2. Ahrens PM, Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg Br. 2007;89:1001–1009. [DOI] [PubMed] [Google Scholar]
- 3. Becker DA, Cofield RH. Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis: long-term results. J Bone Joint Surg Am. 1989;71:376–381. [PubMed] [Google Scholar]
- 4. Brady PC, Narbona P, Adams CR, et al. Arthroscopic proximal biceps tenodesis at the articular margin: evaluation of outcomes, complications, and revision rate. Arthroscopy. 2015;31(3):470–476. [DOI] [PubMed] [Google Scholar]
- 5. Friedman DJ, Dunn JC, Higgins LD, Warner JJ. Proximal biceps tendon: injuries and management. Sports Med Arthrosc Rev. 2008;16(3):162–169. [DOI] [PubMed] [Google Scholar]
- 6. Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 2009;37(4):828–833. [DOI] [PubMed] [Google Scholar]
- 7. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43:1077–1083. [DOI] [PubMed] [Google Scholar]
- 8. Hanypsiak BT, DeLong JM, Guerra JJ. Proximal biceps tendon pathology In DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice. Philadelphia, PA: Saunders/Elsevier, 2015;569–584. [Google Scholar]
- 9. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20(2):326–332. [DOI] [PubMed] [Google Scholar]
- 10. Ma H, Van Heest A, Glisson C, Patel S. Musculocutaneous nerve entrapment: an unusual complication after biceps tenodesis. Am J Sports Med. 2009;37(12):2467–2469. [DOI] [PubMed] [Google Scholar]
- 11. Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–768. [DOI] [PubMed] [Google Scholar]
- 12. Sanders B, Lavery KP, Pennington S, Warner JJP. Clinical success of biceps tenodesis with and without release of the transverse humeral ligament. J Shoulder Elbow Surg. 2012;21:66–71. [DOI] [PubMed] [Google Scholar]
- 13. Werner BC, Evans CL, Holzgrefe RE, et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42(11):2583–2590. [DOI] [PubMed] [Google Scholar]
- 14. Werner BC, Holzgrefe RE, Brockmeier SF. Arthroscopic surgical techniques for the management of proximal biceps injuries. Clin Sports Med. 2016;35:113–135. [DOI] [PubMed] [Google Scholar]