Abstract
Native and artificial extracellular matrices (ECMs) have been widely applied in biomedical fields as one of the most effective components in tissue regeneration. In particular, ECM-based drugs are expected to be applied to treat diseases in organs relevant to urology, because tissue regeneration is particularly important for preventing the recurrence of these diseases. Native ECMs provide a complex in vivo architecture and native physical and mechanical properties that support high biocompatibility. However, the applications of native ECMs are limited due to their tissue-specificity and chemical complexity. Artificial ECMs have been fabricated in an attempt to create a broadly applicable scaffold by using controllable components and a uniform formulation. On the other hands, artificial ECMs fail to mimic the properties of a native ECM; consequently, their applications in tissues are also limited. For that reason, the design of a versatile, hybrid ECM that can be universally applied to various tissues is an emerging area of interest in the biomedical field.
Keywords: Extracellular matrix, Tissue regeneration, Versatile extracellular matrix, Urology
INTRODUCTION
The extracellular matrix (ECM) in animal cells is a vital extracellular scaffold that is composed of various protein components, such as fibronectin, laminin, collagen, proteoglycans, and other soluble molecules [1]. The constituent macromolecules of the ECM have structural and chemical properties that are functionally suited to their native functions in their respective tissues [2]. These multimolecular structures are interconnected with each other and build a complex 3-dimensional (3D) matrix network [3]. The ECM is a dynamic network that provides support and biomechanical cues to cells and is involved in signaling, homeostasis, differentiation, migration, and repair of a variety of tissues [4,5]. Both in physiological conditions and during disease development, the processes, structures, and properties of ECMs are remodeled in multiple ways [3,6,7].
Based on their source, ECMs can be classified as native ECMs, which are isolated from cells, tissues, or organs, and artificial ECMs, which are fabricated by mimicking the natural process of fibrillogenesis. In recent years, numerous studies on the role of native ECMs in biomedicine have been published, showing that native ECMs support 3D tissue culturing, promote wound healing, trigger stem cell differentiation, and have applications as drug screening tools. In particular, ECMs are expected to be applied to urology-related organs (i.e., the kidneys, adrenal glands, and reproductive organs) [7-14]. Native ECMs trigger stem cell differentiation and wound healing by seeding specific cells onto native tissues or cells [15-17]. The advantages of native ECMs lie in their ability to provide the necessary environmental cues to stimulate cell-based repair pathways and to promote adaptive remodeling toward functional recovery [18]. In addition, native ECMs can also be used as drug screening tools that support research into the molecular mechanisms of cancer cells by clinically and naturally mimicking the tumors’ microenvironments. Native ECMs have many applications because of their high biocompatibility, ability to replicate complex in vivo architectures, and native physical and mechanical properties. Nonetheless, the applications of native ECMs remain limited due to their tissuespecificity, multiple and heterogeneous components, and complex nonuniform structure [8,19-21]. The qualitative and quantitative chemical composition of a native ECM determines its viscoelastic character, mechanical properties, and native function [22,23]. Current studies are emphasizing the synthesis of scaffolds that mimic the chemical complexity and architecture of native ECMs in efforts to overcome their limitations.
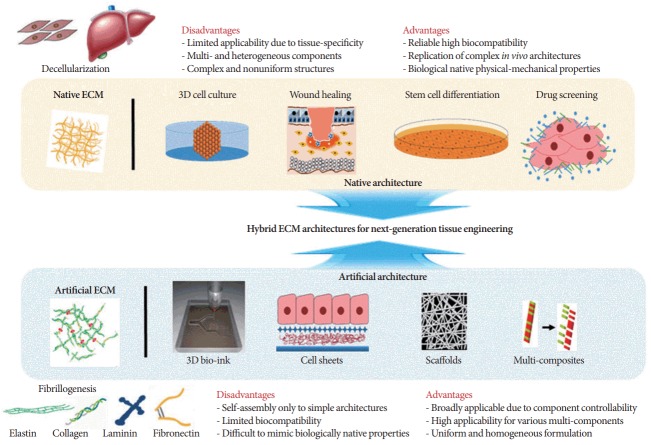
In previous studies, artificial scaffolds were successfully fabricated by adopting the processes of fibrillogenesis and morphogenesis that occur in the human body [7,24,25]. Current artificial ECMs that mimic native ECMs are composed of artificial polymers or selected components, such as elastin, collagen, laminin, and fibronectin. Such artificial scaffolds have a wide range of applications due to the controllability of their components, the useful properties of their various components, and their uniform formulations. However, artificial ECMs often have the disadvantage of failing to have the highly variable biochemical properties and architecture of the native ECM of each tissue. The simple architectures of artificial ECMs cause limited biocompatibility in tissue applications (Fig. 1). The challenges in achieving the high variability of native ECM for specific tissues have led to efforts to develop hybrid ECM architectures that can be applied to all tissues and organs. However, the lack of research characterizing the chemical complexity and components of the native ECM in each tissue has limited the development of hybrid ECMs. In this review, in order to highlight the crucial components for hybrid ECMs, we focus on the main differences between native and artificial ECMs in terms of chemical complexity, structure, synthesis, and purification. Although studies have yet to be conducted with the goal of designing versatile, hybrid ECM architectures, we are confident that attempts at research in this area will be made in the near future.
Fig. 1.
Hybrid extracellular matrix (ECM)-architecture for next-generation tissue engineering. The hybrid ECM, which can be broadly applied to all tissues and organs, is a strategy for adopting the advantages of native ECMs and artificial ECMs.
NATIVE AND ARTIFICIAL ECMs AND THEIR APPLICATIONS IN TISSUE ENGINEERING
Chemical Complexity and Tissue Variation of Native ECM
Native ECM represents a biomaterial scaffold that is generated from tissues or typical cells, such as fibroblasts, endothelial cells, keratinocytes, and mesenchymal stem cells, and is then purified. Recently, some studies have reported that both cancer cell lines and stromal cells deposited ECMs. The major constituents are fibrous proteins, such as collagen, fibronectin, laminin, and elastin, and nonfibrous proteins, such as proteoglycans and glycosaminoglycans, which are connected to each other to build a complex 3D matrix network [3,26]. Even though these components form the basic structure of native ECMs, the proportion of each component varies considerably across tissue types and can change considerably due to pathological conditions. In particular, the biosynthesis and structure of collagen are modified during remodeling of the ECM in several pathologies, including tumorigenesis. A further example of variability is furnished by the distribution of laminin isoforms, which vary greatly from tissue to tissue, suggesting that laminin has tissue-specific functions [8].
The ECM forms a tissue or an organ that has an enormous diversity of shapes and functions. Cell- and tissue-derived ECMs are present in various tissues in the human body, such as skin, cartilage, bones, teeth, and the extracellular space. More specifically, the structure, viscoelastic character, mechanical properties, and native functionality of an ECM are determined by its chemical complexity [22,23]. An ECM derived from a specific tissue, however, consists of a large variety of macromolecules, with not only a precise tissue-specific composition but also a particular architecture. Therefore, it is important to summarize and compare the chemical complexities of and variations in the ECMs in many different tissues. For example, as described in Table 1, the ECM of adipose tissue is mainly composed of collagen IV, while the ECMs of bone and teeth tissues are composed of calcified ECM compounds (Table 1). Collagen IV is specific to the ECM of human adipocytes, which controls the pathology of obesity-related diseases [27]. The ratio between elastin and collagen in the ECM derived from human adipocyte tissue determines its biomechanical properties [28]. Bones and teeth are composed of calcified ECM (Table 1), which undergo mineralization to support the structure. In contrast, the ECM in ligaments or tendons is mostly composed of collagen (75%–85% of dry tissue weight). Collagen forms a fibrous architecture that confers outstanding mechanical strength to tendons. Furthermore, collagen has been found to be the most abundant chemical in the ECM derived from human skin. Collagens I and III are major components of the interstitial matrix, while collagen IV is the major component of the basement membrane. A defect in fibrillogenesis can lead to abnormal collagen fibers, which, in turn, alter the properties of the skin, clinically manifesting as skin disease [29].
Table 1.
Chemical composition of extracellular matrix in human tissue
| Extracellular matrix tissue source | Component |
Reference | |||
|---|---|---|---|---|---|
| Fibronectin | Laminin | Collagen | Other components | ||
| Human mesenchymal stem cell | Fibronectin (FN1) | Laminin | Collagen I–II | Fibulin-1, fibrillin-1, filamin-A, perlecan | [42] |
| Collagen VI (α1), collagen VI (α2), collagen VI (α3), collagen XII (α1) | Periostin, tenascin C, transforming growth factor-betainduced protein ig-h3, transglutaminase 2, thrombospondin-1 versican | ||||
| Human adipocyte | Fibronectin (FN) (cold-insoluble globulin) | L aminin α2, laminin α4, laminin β1, laminin β2, laminin γ1 | Collagen I (α1), collagen I (α2), collagen III (α1), collagen IV* (α1), collagen V (α1), collagen VI (α1), collagen VI (α2), collagen VI (α3), collagen XIII (α1), collagen XIV (α1) (undulin), collagen XV (α1), collagen XVIII (α1) | Proteoglycan IV, agrecan, decortin, cartilage intermediate layer protein, mimecan (osteoglycin), nidogen 1 (entactin), nidogen 2 (osteonidogen), periostin, dermaportin, tenascin C and X | [29] |
| Fibulin-1 | |||||
| Human breast cancer | Oncofetal fibronectin | Laminin 111, laminin 332 | Collagen I, collagen III, collagen IV–V | Fibrilin, fibulin, elastin, epigrilin, entactin, vitronectin, proteoglycans, hyaluronan, glycoprotein | [35] |
| Ligament tissue | Fibronectin I | Laminin β1 | Collagen I, collagen III, collagen IV–VI, collagen XI–XII | Proteoglycans IV, versican, vibrilin I, decorin, bigylcan sulphated glyco-saminosglycans, elastin, small rich leucine protein | [43-46] |
| Lymphoid tissue | Fibronectin | Laminin α1, laminin α2, laminin α4, laminin α5, laminin γ, laminin β1, laminin β2, pan-laminin, laminin 332 | Collagen I, collagen III, collagen IV | Tenascin | [47,48] |
| Bone | Fibronectin, vitronectin | Laminin | Collagen I, collagen III | Osteopontin, osteocalcin, osteonectin, chondroitin sulphate, thrombospodin I, thrombospodin II, secreted protein acidic and rich in cysteine, R-spondin, bone sialoprotein, dentin matrix acidic phosphoprotein-1, matrix extracellular phosphoglycoprotein, matrix-gla protein, periostin, aspirin, biglycan, decoran, keratocan, matrix metallopreoteinase (MMP2 & 14) | [31,49] |
| Human corneal tissue (epithelial and stroma) | Fibronectin | Laminin 5 (α3β3γ2) | Collagen I–IX | K eratan sulphate, chondroitin sulphate, N-acetylglucosamine | [36,37,50] |
| Laminin 10 (α5β1γ1) | Collagen XII–XIV | ||||
| Collagen XVII–XVIII | |||||
| Skin tissue | Fibronectin (in basement membrane) | Laminin α3β3γ2 | Collagen I, III, IV–VII | E lastic fiber (elastin, microfibrilar component, fibrillar), glycosaminoglycans, heparan sulfate, nidogen | [32,51] |
| Laminin α5β1γ1 | |||||
The chemical complexity of a native ECM also determines the native function of the tissue. In human mesenchymal stem cells, the ECM supports stemness and enhances cell proliferation [30]. In particular, fibronectin plays the role of a mechanoregulator, translating the microenvironmental signals that regulate stem-cell differentiation [31]. In particular, fibronectin and collagen can be utilized as valuable markers of tumor development in urology-related organs, such as the bladder [32,33]. Similarly, hyaluronan and matricellular proteins are important constituents of metastatic niches in patients with breast cancer. Moreover, specific ECM molecules and their receptors or enzymatic modifiers play important roles in therapeutic resistance [34]. In human corneal tissue, the composition of the ECM influences fibroblast migration. Laminin-5- and laminin-10-mediated cell migration occurs through the binding of integrin α3β1 in corneal epithelial cells [35]. Fibronectin and chondroitin sulfate significantly increase migration; however, collagens V and VI serve as poor substrates for cell attachment, which is important for cell migration [35]. Dysregulation of the structure and chemical composition of the ECM leads to disease. For instance, urinary fibronectin concentrations were found to be significantly higher in patients with bladder cancer and lithiasis than in healthy individuals [36].
In the fabrication of a native ECM from cell- and tissue-derived ECMs, decellularization is an important process for removing cells from the scaffold without disturbing the chemical complexity and the mechanical structure of the matrix, including its microstructure and stiffness. Decellularized ECM scaffolds have broad applications in tissue engineering, wound healing, and disease modeling [9,16,18,37-40]. The characteristics of those decellularized ECM scaffolds, such as their good biocompatibility, nontoxic catabolites, and microinflammatory characteristics, as well as their regenerative ability, hold great potential for tissue engineering and wound healing [40]. The decellularization of sterilized porcine bladder and urologic ECM as a material for bladder scaffolding and lower urinary tract reconstruction has shown promising results [41]. Therefore, it has potential applications in general tissue engineering, and especially in the treatment of stress urinary incontinence [42]. Furthermore, a decellularized ECM can favorably support 3D cell culture setups that mimic the microenvironment of cancer, with potential applications in cancer modeling for drug screening [38].
Artificial ECM as a Broadly Applicable Scaffold
Currently, in the field of tissue engineering, increasing interest is emerging in artificial ECMs for remodeling, regenerating, or replacing damaged tissues and organs. Artificial ECMs that are appropriately prepared can physically mimic native ECMs and can functionally support cell growth and maintain homeostasis [13]. Many different types of ECM scaffolds have been constructed using a variety of materials, ranging from tissue- and cell-derived materials to synthetic biomaterials [9]. Artificial ECMs have many advantages in terms of reproducibility and cost compared to native ECMs. However, compared to tissue- or cell-derived ECMs, artificial ECMs may not be fully biocompatible and biofunctional [43,44]. Therefore, artificial ECMs should be designed by adopting the real chemical complexity and structure (scaffold) of a native ECM. In nature, native ECMs are fundamentally made by a process known fibrillogenesis, suggesting that it is possible, in principle, to synthesize complex ECM architectures using these biochemical reactions.
Previous studies, in fact, revealed that artificial ECMs could be constructed using a fibrillogenesis-mimicking reaction and could successfully support cardiomyocytes and neonatal neurons [24,25]. Roy et al. [45], by directly coupling the open heparin-binding fibronectin III1 fragment (FNIII1H) to the integrinbinding domain (FNIII8–10), developed a fibronectin matrix mimetic that had regulatory effects similar to those of ECM fibronectin on cell function. This matrix supported cell spreading, growth, migration, and contraction through a FNIII1H-dependent mechanism to a greater extent than cellular fibronectin [46]. A similar result was reported by Dubey and Mequanint [47], who conjugated fibronectin onto highly porous 3D poly (carbonate) urethane scaffolds through grafted poly (acrylic acid) spacers on the urethane backbone; this modified scaffold promoted coronary artery smooth muscle cells better than a scaffold without fibronectin conjugation. Adding fibronectin to elastin-like protein also enhanced endothelial cell and mesenchymal stem cell compatibility through increased cell adsorption and viability [48]. Moreover, fibronectin and hydroxyapatite coatings increased the efficiency of fibroblast attachment and cellular activities [49]. A fibronectin-based artificial matrix was also successfully constructed on a titanium surface using an electro-dropping technique. This engineered matrix significantly promoted preosteoblast proliferation and had potential bone regeneration applications [50]. In injured bladders, fibronectin showed higher adherence, proving that it exerted a protective effect in hybrid urologic tissue engineering applications [51,52]. The ability of fibronectin to incorporate a myriad of substrates and to direct cell proliferation makes it a favorable candidate for use as a bioactive material in cell culture and tissue regeneration.
Laminin-derived peptides and laminin-peptide-conjugated scaffolds are also considered to be promising materials for tissue engineering [11,30,53]. Because laminin exists in various types of isoforms in each tissue, incorporating an integrated laminin isoform into the scaffold has been considered as a strategy for overcoming the variability of the artificial matrix. Incorporating laminin into the scaffold could reduce inflammation and foster re-epithelialization, differentiation, angiogenesis, and cell migration [54,55]. Laminin absorbed into micropattern surface poly (L-lactic acid) nanofibers enhanced neuron viability [56]. The coupled laminin and other chemical cues exerted synergistic effects to enhance directional neurite outgrowth. Another strategy for producing an artificial cell-mimicking basement membrane for a cell-derived ECM involves isolating a number of lamin-inderived peptides and coating them with chitosan and alginate [57]. The laminin-coated scaffold improved the infiltration of human-induced pluripotent stem cells, promoting the recovery and differentiation of neurons [58,59].
Collagen type I is a component that is commonly used to construct ECM-mimicking scaffolds in tissue engineering. Yuan et al. [60] designed a scaffold of collagen type I hydrogel that had fewer immunogenicity effects on engineered cartilage based on chondrocytes, thus making it a potential biomaterial for use in tissue engineering. Collagen-based collagen fiber and bioglass show good biocompatibility and promote the spread, as well as the proliferation, of bone marrow cells; thus, they are considered to form an ideal scaffold for bone tissue engineering [61]. A collagen-in-hydroxyapatite scaffold complex that increased cell attachment was reported by Villa et al. [62]. Nanosilver-embedded collagen scaffolds coated with either laminin or laminin and fibronectin have also been reported to be effective in promoting axonal regeneration and recovery [63]. The growth rates of German Landrace urothelial cells and smooth muscle cells were significantly higher on collagen-composed scaffolds. This growth behavior showed that these collagen scaffolds were adequate for urologic tissue regeneration [64,65].
Artificial biopolymers and composites, such as chitosan, alginate, silk, fibrin and hydrogels, are promising biomaterials that promote wound healing due to their appropriate properties for tissue regeneration. Chitosan, in a scaffold combination, is one of the most widely used materials that support the reconnection of cultured Schwann cells. Cells seeded on chitosan scaffolds produced higher amounts of laminin and collagen IV than those grown on a plane, thereby creating favorable conditions for nerve regeneration [60,66]. Moreover, a chitosan scaffold with incorporated collagen I has been proposed as a potential material for wound healing [67]. Another scaffold that has been widely used in tissue engineering is silk fibroin, which has been used clinically in surgical silk sutures for years. However, the nanofibrous structure of ECMs remains a challenge to fabricate [68]. As a solution to this problem, chitosan and silk fibroin have been merged to yield better cell-culture performance [69]. A chitosan hybrid ECM was developed to improve adhesion capacity in comparison with alginate (polysaccharide isolated from seaweed) polymer fibers [70]. Another biomaterial scaffold was derived from gelatin in a collagen scaffold; that scaffold was found to have better physical properties than a scaffold of collagen only [71]. Furthermore, fibrin is another biopolymer with characteristics suggesting that it may have the potential to mimic a functional ECM; furthermore, it is associated with other ECM components [72,73].
Overall, artificial ECMs have broader applications, such as 3D bio-inks, cell sheets, scaffolds, and multicomposites, owing to the controllability of their components and their uniform formulation. However, when an artificial ECM fails to adopt the highly variable biochemical characteristics and architecture of native ECM in each tissue, it has limited biocompatibility in tissue applications (Fig. 1).
CONCLUSION AND FUTURE PERSPECTIVES
A number of strategies that rely on different targets of the disease have been pursued to prevent and kill cancer cells. Most anticancer drug candidates fail to be approved for clinical applications because of inadequacies in the study of the molecular mechanism of cancer progression, identification of therapeutic targets, and tests of drug candidates using tissue culture models that cannot precisely mimic the native microenvironment. Drug candidates often reveal in vitro cytotoxicity with a loss of in vivo activity, and in many cases, this results from a poor understanding of the effects of chemoresistance in the environment of cancer [74]. A 2-dimensional (2D) cell culture cannot mimic the real environment in which cancer cells grow and proliferate. Therefore, constructing an appropriate cell culture system, similar to the actual microenvironment, is important if the gap between in vitro and in vivo experiments in preclinical trials is to be removed. Three-dimensional cell cultures are more natively and clinically similar to the native environment of cancer cells than 2D models. Even though the idea of 3D culturing is not novel, some difficulties in mimicking a native ECM biophysically and biochemically still remain [75,76].
Biomaterial scaffolds have been applied for wound healing, restoration and reconstruction. These biomaterial scaffolds have good biocompatibility, nontoxic catabolites, microinflammatory characteristics, and regenerative ability, which give them great potential for use in tissue repair [39]. Both natural polymers and ECMs exhibit the ability to regenerate cells. Native ECMs derived from adipocyte stem cells have been reported to exert a regenerative effect on chronic wounds [16]. Cell-derived, native ECMs are also regularly used in tissue engineering applications because they have the advantages of allowing pathogen-controllable ECM harvesting and providing the same geometries and porosities without the limitation of poor cell penetration. Other advantages of cell-derived ECMs include the possibility for them to be anchored with ECMs from other cells and to be prepared from autologous cells [77,78]. Native ECMs have been shown to support adhesion, to promote cell proliferation and differentiation, and to facilitate tissue regeneration in cartilage and in esophageal and skin cells [15,79,80]. The challenge in tissue regeneration is that tissues must match between the recipient and the donor in order to avoid immune rejection [12,81,82]. Therefore, methods have been developed to decellularize tissue and whole organs, leaving the native ECM to create tissue and wholeorgan scaffolds that can be reseeded with host cells.
Recently, artificial ECMs composed of artificial polymers or selected controllable components and with uniform and homogenous formulations have been fabricated and shown to have possible applications in various tissues. Even with these advances, it is difficult to mimic native ECMs, which have complex chemical and architectural structures that are tissue-specific. In particular, ECM-based tissue engineering is promising in the field of urology, in response to the need to regenerate anatomic and functional tissues, and we believe that these approaches will provide alternative cures to millions of people suffering from urologic incontinence or cancers [83-85]. The advantages and limitations of each system provide a direction for new research. If an artificial ECM can be fabricated with a precise and diverse combination of components, the native ECM can provide a complex structure. The combination of these 2 systems is predicted to yield a new versatile, hybrid ECM system. Understanding the structures and functions of ECMs in each tissue, controlling the fibrillogenesis mechanism using individual ECM components, and the recent development of new tools for bio-printing and imaging will greatly help to implement such a hybrid ECM in tissue engineering in the near future.
Footnotes
Fund/Grant Support
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (2018R1A6A1A03024940), and the Human Resources Program in Energy Technology of the Korea Institute of Energy Technology Evaluation and Planning (No. 20174010201150).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
·Full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis: KS
·Study concept and design: KS
·Acquisition of data: AS, HTN
·Analysis and interpretation of data: AS, HTN, KS
·Drafting of the manuscript: AS, HTN
·Critical revision of the manuscript for important intellectual content: KS
·Obtained funding: KS
·Administrative, technical, or material support: YJ
·Study supervision: KS
REFERENCES
- 1.Halper J, Kjaer M. Basic components of connective tissues and extracellular matrix: elastin, fibrillin, fibulins, fibrinogen, fibronectin, laminin, tenascins and thrombospondins. Adv Exp Med Biol. 2014;802:31–47. doi: 10.1007/978-94-007-7893-1_3. [DOI] [PubMed] [Google Scholar]
- 2.Mouw JK, Ou G, Weaver VM. Extracellular matrix assembly: a multiscale deconstruction. Nat Rev Mol Cell Biol. 2014;15:771–85. doi: 10.1038/nrm3902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Theocharis AD, Skandalis SS, Gialeli C, Karamanos NK. Extracellular matrix structure. Adv Drug Deliv Rev. 2016;97:4–27. doi: 10.1016/j.addr.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Davis NF, Cunnane EM, Quinlan MR, Mulvihill JJ, Lawrentschuk N, Bolton DM, et al. Biomaterials and regenerative medicine in urology. Adv Exp Med Biol. 2018 Jan 17; doi: 10.1007/5584_2017_139. [Epub]. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Perez F, Udina E, Navarro X. Extracellular matrix components in peripheral nerve regeneration. Int Rev Neurobiol. 2013;108:257–75. doi: 10.1016/B978-0-12-410499-0.00010-1. [DOI] [PubMed] [Google Scholar]
- 6.Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol. 2014;15:786–801. doi: 10.1038/nrm3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han S, Shin Y, Jeong HE, Jeon JS, Kamm RD, Huh D, et al. Constructive remodeling of a synthetic endothelial extracellular matrix. Sci Rep. 2015;5:18290. doi: 10.1038/srep18290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iorio V, Troughton LD, Hamill KJ. Laminins: roles and utility in wound repair. Adv Wound Care (New Rochelle) 2015;4:250–63. doi: 10.1089/wound.2014.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhong SP, Zhang YZ, Lim CT. Tissue scaffolds for skin wound healing and dermal reconstruction. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2010;2:510–25. doi: 10.1002/wnan.100. [DOI] [PubMed] [Google Scholar]
- 10.Clark RA, An JQ, Greiling D, Khan A, Schwarzbauer JE. Fibroblast migration on fibronectin requires three distinct functional domains. J Invest Dermatol. 2003;121:695–705. doi: 10.1046/j.1523-1747.2003.12484.x. [DOI] [PubMed] [Google Scholar]
- 11.Reimers K, Liebsch C, Radtke C, Kuhbier JW, Vogt PM. Silks as scaffolds for skin reconstruction. Biotechnol Bioeng. 2015;112:2201–5. doi: 10.1002/bit.25654. [DOI] [PubMed] [Google Scholar]
- 12.Chen G, Qi Y, Niu L, DI T, Zhong J, Fang T, et al. Application of the cell sheet technique in tissue engineering. Biomed Rep. 2015;3:749–57. doi: 10.3892/br.2015.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim Y, Ko H, Kwon IK, Shin K. Extracellular matrix revisited: roles in tissue engineering. Int Neurourol J. 2016;20(Suppl 1):S23–9. doi: 10.5213/inj.1632600.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matoka DJ, Cheng EY. Tissue engineering in urology. Can Urol Assoc J. 2009;3:403–8. doi: 10.5489/cuaj.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanai N, Yamato M, Okano T. Cell sheets engineering for esophageal regenerative medicine. Ann Transl Med. 2014;2:28. doi: 10.3978/j.issn.2305-5839.2014.03.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyldig K, Riis S, Pennisi CP, Zachar V, Fink T. Implications of extracellular matrix production by adipose tissue-derived stem cells for development of wound healing therapies. Int J Mol Sci. 2017 May 31;18(6) doi: 10.3390/ijms18061167. pii: E1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guneta V, Zhou Z, Tan NS, Sugii S, Wong MTC, Choong C. Recellularization of decellularized adipose tissue-derived stem cells: role of the cell-secreted extracellular matrix in cellular differentiation. Biomater Sci. 2017;6:168–78. doi: 10.1039/c7bm00695k. [DOI] [PubMed] [Google Scholar]
- 18.Rijal G, Li W. A versatile 3D tissue matrix scaffold system for tumor modeling and drug screening. Sci Adv. 2017;3:e1700764. doi: 10.1126/sciadv.1700764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LeBleu VS, Macdonald B, Kalluri R. Structure and function of basement membranes. Exp Biol Med (Maywood) 2007;232:1121–9. doi: 10.3181/0703-MR-72. [DOI] [PubMed] [Google Scholar]
- 20.Yue B. Biology of the extracellular matrix: an overview. J Glaucoma. 2014;23(8 Suppl 1):S20–3. doi: 10.1097/IJG.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miner JH, Yurchenco PD. Laminin functions in tissue morphogenesis. Annu Rev Cell Dev Biol. 2004;20:255–84. doi: 10.1146/annurev.cellbio.20.010403.094555. [DOI] [PubMed] [Google Scholar]
- 22.Schaefer L, Schaefer RM. Proteoglycans: from structural compounds to signaling molecules. Cell Tissue Res. 2010;339:237–46. doi: 10.1007/s00441-009-0821-y. [DOI] [PubMed] [Google Scholar]
- 23.Tomasetti L, Breunig M. Preventing obstructions of nanosized drug delivery systems by the extracellular matrix. Adv Healthc Mater. 2018;7 doi: 10.1002/adhm.201700739. [DOI] [PubMed] [Google Scholar]
- 24.Ahn S, Lee KY, Parker KK, Shin K. Formation of multi-component extracellular matrix protein fibers. Sci Rep. 2018;8:1913. doi: 10.1038/s41598-018-20371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahn S, Deravi LF, Park SJ, Dabiri BE, Kim JS, Parker KK, et al. Self-organizing large-scale extracellular-matrix protein networks. Adv Mater. 2015;27:2838–45. doi: 10.1002/adma.201405556. [DOI] [PubMed] [Google Scholar]
- 26.Frantz C, Stewart KM, Weaver VM. The extracellular matrix at a glance. J Cell Sci. 2010;123(Pt 24):4195–200. doi: 10.1242/jcs.023820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mariman EC, Wang P. Adipocyte extracellular matrix composition, dynamics and role in obesity. Cell Mol Life Sci. 2010;67:1277–92. doi: 10.1007/s00018-010-0263-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alkhouli N, Mansfield J, Green E, Bell J, Knight B, Liversedge N, et al. The mechanical properties of human adipose tissues and their relationships to the structure and composition of the extracellular matrix. Am J Physiol Endocrinol Metab. 2013;305:E1427–35. doi: 10.1152/ajpendo.00111.2013. [DOI] [PubMed] [Google Scholar]
- 29.Uitto J, Olsen DR, Fazio MJ. Extracellular matrix of the skin: 50 years of progress. J Invest Dermatol. 1989;92(4 Suppl):61S–77S. doi: 10.1111/1523-1747.ep13075039. [DOI] [PubMed] [Google Scholar]
- 30.Rakian R, Block TJ, Johnson SM, Marinkovic M, Wu J, Dai Q, et al. Native extracellular matrix preserves mesenchymal stem cell “stemness” and differentiation potential under serum-free culture conditions. Stem Cell Res Ther. 2015;6:235. doi: 10.1186/s13287-015-0235-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li B, Moshfegh C, Lin Z, Albuschies J, Vogel V. Mesenchymal stem cells exploit extracellular matrix as mechanotransducer. Sci Rep. 2013;3:2425. doi: 10.1038/srep02425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Menendez V, Fernandez-Suarez A, Galan JA, Perez M, Garcia-Lopez F. Diagnosis of bladder cancer by analysis of urinary fibronectin. Urology. 2005;65:284–9. doi: 10.1016/j.urology.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 33.Brunner A, Tzankov A. The role of structural extracellular matrix proteins in urothelial bladder cancer (review) Biomark Insights. 2007;2:418–27. doi: 10.4137/bmi.s294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oskarsson T. Extracellular matrix components in breast cancer progression and metastasis. Breast. 2013;22 Suppl 2:S66–72. doi: 10.1016/j.breast.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 35.Filenius S, Hormia M, Rissanen J, Burgeson RE, Yamada Y, Araki-Sasaki K, et al. Laminin synthesis and the adhesion characteristics of immortalized human corneal epithelial cells to laminin isoforms. Exp Eye Res. 2001;72:93–103. doi: 10.1006/exer.2000.0933. [DOI] [PubMed] [Google Scholar]
- 36.Alias-Melgar A, Neave-Sanchez E, Suarez-Cuenca JA, Morales-Covarrubias J. Association of urine oncofetal fibronectin levels with urology’s most common disorders. Ann Clin Lab Sci. 2013;43:420–3. [PubMed] [Google Scholar]
- 37.Mazza G, Rombouts K, Rennie Hall A, Urbani L, Vinh Luong T, Al-Akkad W, et al. Decellularized human liver as a natural 3D-scaffold for liver bioengineering and transplantation. Sci Rep. 2015;5:13079. doi: 10.1038/srep13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoshiba T, Lu H, Kawazoe N, Chen G. Decellularized matrices for tissue engineering. Expert Opin Biol Ther. 2010;10:1717–28. doi: 10.1517/14712598.2010.534079. [DOI] [PubMed] [Google Scholar]
- 39.Fischer I, Westphal M, Rossbach B, Bethke N, Hariharan K, Ullah I, et al. Comparative characterization of decellularized renal scaffolds for tissue engineering. Biomed Mater. 2017;12:045005. doi: 10.1088/1748-605X/aa6c6d. [DOI] [PubMed] [Google Scholar]
- 40.Da LC, Huang YZ, Xie HQ. Progress in development of bioderived materials for dermal wound healing. Regen Biomater. 2017;4:325–34. doi: 10.1093/rb/rbx025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosario DJ, Reilly GC, Ali Salah E, Glover M, Bullock AJ, Macneil S. Decellularization and sterilization of porcine urinary bladder matrix for tissue engineering in the lower urinary tract. Regen Med. 2008;3:145–56. doi: 10.2217/17460751.3.2.145. [DOI] [PubMed] [Google Scholar]
- 42.Simoes IN, Vale P, Soker S, Atala A, Keller D, Noiva R, et al. Acellular urethra bioscaffold: decellularization of whole urethras for tissue engineering applications. Sci Rep. 2017;7:41934. doi: 10.1038/srep41934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sreejit P, Verma RS. Natural ECM as biomaterial for scaffold based cardiac regeneration using adult bone marrow derived stem cells. Stem Cell Rev. 2013;9:158–71. doi: 10.1007/s12015-013-9427-6. [DOI] [PubMed] [Google Scholar]
- 44.Aamodt JM, Grainger DW. Extracellular matrix-based biomaterial scaffolds and the host response. Biomaterials. 2016;86:68–82. doi: 10.1016/j.biomaterials.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roy DC, Wilke-Mounts SJ, Hocking DC. Chimeric fibronectin matrix mimetic as a functional growth- and migration-promoting adhesive substrate. Biomaterials. 2011;32:2077–87. doi: 10.1016/j.biomaterials.2010.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roy DC, Hocking DC. Recombinant fibronectin matrix mimetics specify integrin adhesion and extracellular matrix assembly. Tissue Eng Part A. 2013;19:558–70. doi: 10.1089/ten.tea.2012.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dubey G, Mequanint K. Conjugation of fibronectin onto three-dimensional porous scaffolds for vascular tissue engineering applications. Acta Biomater. 2011;7:1114–25. doi: 10.1016/j.actbio.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 48.Ravi S, Caves JM, Martinez AW, Haller CA, Chaikof EL. Incorporation of fibronectin to enhance cytocompatibility in multilayer elastin-like protein scaffolds for tissue engineering. J Biomed Mater Res A. 2013;101:1915–25. doi: 10.1002/jbm.a.34484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pendegrass CJ, El-Husseiny M, Blunn GW. The development of fibronectin-functionalised hydroxyapatite coatings to improve dermal fibroblast attachment in vitro. J Bone Joint Surg Br. 2012;94:564–9. doi: 10.1302/0301-620X.94B4.27698. [DOI] [PubMed] [Google Scholar]
- 50.Subbiah R, Du P, Van SY, Suhaeri M, Hwang MP, Lee K, et al. Fibronectin-tethered graphene oxide as an artificial matrix for osteogenesis. Biomed Mater. 2014;9:065003. doi: 10.1088/1748-6041/9/6/065003. [DOI] [PubMed] [Google Scholar]
- 51.See WA, Rohlf DP, Crist SA. In vitro particulate adherence to fibronectin: correlation with in vivo particulate adherence to sites of bladder injury. J Urol. 1992;147:1416–23. doi: 10.1016/s0022-5347(17)37585-7. [DOI] [PubMed] [Google Scholar]
- 52.Uchida N, Sivaraman S, Amoroso NJ, Wagner WR, Nishiguchi A, Matsusaki M, et al. Nanometer-sized extracellular matrix coating on polymer-based scaffold for tissue engineering applications. J Biomed Mater Res A. 2016;104:94–103. doi: 10.1002/jbm.a.35544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Riederer I, Bonomo AC, Mouly V, Savino W. Laminin therapy for the promotion of muscle regeneration. FEBS Lett. 2015;589:3449–53. doi: 10.1016/j.febslet.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 54.Domogatskaya A, Rodin S, Tryggvason K. Functional diversity of laminins. Annu Rev Cell Dev Biol. 2012;28:523–53. doi: 10.1146/annurev-cellbio-101011-155750. [DOI] [PubMed] [Google Scholar]
- 55.Neal RA, Lenz SM, Wang T, Abebayehu D, Brooks BP, Ogle RC, et al. Laminin- and basement membrane-polycaprolactone blend nanofibers as a scaffold for regenerative medicine. Nanomater Environ. 2014;2:1–12. doi: 10.2478/nanome-2014-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Koh HS, Yong T, Chan CK, Ramakrishna S. Enhancement of neurite outgrowth using nano-structured scaffolds coupled with laminin. Biomaterials. 2008;29:3574–82. doi: 10.1016/j.biomaterials.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 57.Yamada Y, Hozumi K, Aso A, Hotta A, Toma K, Katagiri F, et al. Laminin active peptide/agarose matrices as multifunctional biomaterials for tissue engineering. Biomaterials. 2012;33:4118–25. doi: 10.1016/j.biomaterials.2012.02.044. [DOI] [PubMed] [Google Scholar]
- 58.Khayyatan F, Nemati S, Kiani S, Hojjati Emami S, Baharvand H. Behaviour of human induced pluripotent stem cell-derived neural progenitors on collagen scaffolds varied in freezing temperature and laminin concentration. Cell J. 2014;16:53–62. [PMC free article] [PubMed] [Google Scholar]
- 59.Jurga M, Dainiak MB, Sarnowska A, Jablonska A, Tripathi A, Plieva FM, et al. The performance of laminin-containing cryogel scaffolds in neural tissue regeneration. Biomaterials. 2011;32:3423–34. doi: 10.1016/j.biomaterials.2011.01.049. [DOI] [PubMed] [Google Scholar]
- 60.Yuan T, Zhang L, Li K, Fan H, Fan Y, Liang J, et al. Collagen hydrogel as an immunomodulatory scaffold in cartilage tissue engineering. J Biomed Mater Res B Appl Biomater. 2014;102:337–44. doi: 10.1002/jbm.b.33011. [DOI] [PubMed] [Google Scholar]
- 61.Long T, Yang J, Shi SS, Guo YP, Ke QF, Zhu ZA. Fabrication of three-dimensional porous scaffold based on collagen fiber and bioglass for bone tissue engineering. J Biomed Mater Res B Appl Biomater. 2015;103:1455–64. doi: 10.1002/jbm.b.33328. [DOI] [PubMed] [Google Scholar]
- 62.Villa MM, Wang L, Rowe DW, Wei M. Effects of cell-attachment and extracellular matrix on bone formation in vivo in collagen-hydroxyapatite scaffolds. PLoS One. 2014;9:e109568. doi: 10.1371/journal.pone.0109568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ding T, Lu WW, Zheng Y, Li Zy, Pan Hb, Luo Z. Rapid repair of rat sciatic nerve injury using a nanosilver-embedded collagen scaffold coated with laminin and fibronectin. Regen Med. 2011;6:437–47. doi: 10.2217/rme.11.39. [DOI] [PubMed] [Google Scholar]
- 64.Leonhauser D, Vogt M, Tolba RH, Grosse JO. Potential in two types of collagen scaffolds for urological tissue engineering applications - Are there differences in growth behaviour of juvenile and adult vesical cells? J Biomater Appl. 2016;30:961–73. doi: 10.1177/0885328215610824. [DOI] [PubMed] [Google Scholar]
- 65.Liu Y, Bharadwaj S, Lee SJ, Atala A, Zhang Y. Optimization of a natural collagen scaffold to aid cell-matrix penetration for urologic tissue engineering. Biomaterials. 2009;30:3865–73. doi: 10.1016/j.biomaterials.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 66.Lin CY, Li LT, Su WT. Three dimensional chitosan scaffolds influence the extra cellular matrix expression in Schwann cells. Mater Sci Eng C Mater Biol Appl. 2014;42:474–8. doi: 10.1016/j.msec.2014.05.063. [DOI] [PubMed] [Google Scholar]
- 67.Duffy GP, McFadden TM, Byrne EM, Gill SL, Farrell E, O’Brien FJ. Towards in vitro vascularisation of collagen-GAG scaffolds. Eur Cell Mater. 2011;21:15–30. doi: 10.22203/ecm.v021a02. [DOI] [PubMed] [Google Scholar]
- 68.Gu Y, Zhu J, Xue C, Li Z, Ding F, Yang Y, et al. Chitosan/silk fibroin-based, Schwann cell-derived extracellular matrix-modified scaffolds for bridging rat sciatic nerve gaps. Biomaterials. 2014;35:2253–63. doi: 10.1016/j.biomaterials.2013.11.087. [DOI] [PubMed] [Google Scholar]
- 69.Ko E, Lee JS, Kim H, Yang SY, Yang D, Yang K, et al. Electrospun silk fibroin nanofibrous scaffolds with two-stage hydroxyapatite functionalization for enhancing the osteogenic differentiation of human adipose-derived mesenchymal stem cells. ACS Appl Mater Interfaces. 2018;10:7614–25. doi: 10.1021/acsami.7b03328. [DOI] [PubMed] [Google Scholar]
- 70.Iwasaki N, Yamane ST, Majima T, Kasahara Y, Minami A, Harada K, et al. Feasibility of polysaccharide hybrid materials for scaffolds in cartilage tissue engineering: evaluation of chondrocyte adhesion to polyion complex fibers prepared from alginate and chitosan. Biomacromolecules. 2004;5:828–33. doi: 10.1021/bm0400067. [DOI] [PubMed] [Google Scholar]
- 71.Grover CN, Cameron RE, Best SM. Investigating the morphological, mechanical and degradation properties of scaffolds comprising collagen, gelatin and elastin for use in soft tissue engineering. J Mech Behav Biomed Mater. 2012;10:62–74. doi: 10.1016/j.jmbbm.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 72.Williams C, Budina E, Stoppel WL, Sullivan KE, Emani S, Emani SM, et al. Cardiac extracellular matrix-fibrin hybrid scaffolds with tunable properties for cardiovascular tissue engineering. Acta Biomater. 2015;14:84–95. doi: 10.1016/j.actbio.2014.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barsotti MC, Felice F, Balbarini A, Di Stefano R. Fibrin as a scaffold for cardiac tissue engineering. Biotechnol Appl Biochem. 2011;58:301–10. doi: 10.1002/bab.49. [DOI] [PubMed] [Google Scholar]
- 74.Holle AW, Young JL, Spatz JP. In vitro cancer cell-ECM interactions inform in vivo cancer treatment. Adv Drug Deliv Rev. 2016;97:270–9. doi: 10.1016/j.addr.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 75.Cui H, Nowicki M, Fisher JP, Zhang LG. 3D bioprinting for organ regeneration. Adv Healthc Mater. 2017 Jan;6(1) doi: 10.1002/adhm.201601118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014;32:773–85. doi: 10.1038/nbt.2958. [DOI] [PubMed] [Google Scholar]
- 77.Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453:314–21. doi: 10.1038/nature07039. [DOI] [PubMed] [Google Scholar]
- 78.Lu H, Hoshiba T, Kawazoe N, Koda I, Song M, Chen G. Cultured cell-derived extracellular matrix scaffolds for tissue engineering. Biomaterials. 2011;32:9658–66. doi: 10.1016/j.biomaterials.2011.08.091. [DOI] [PubMed] [Google Scholar]
- 79.Liu M, Zeng X, Ma C, Yi H, Ali Z, Mou X, et al. Injectable hydrogels for cartilage and bone tissue engineering. Bone Res. 2017;5:17014. doi: 10.1038/boneres.2017.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wassenaar JW, Boss GR, Christman KL. Decellularized skeletal muscle as an in vitro model for studying drug-extracellular matrix interactions. Biomaterials. 2015;64:108–14. doi: 10.1016/j.biomaterials.2015.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Moschouris K, Firoozi N, Kang Y. The application of cell sheet engineering in the vascularization of tissue regeneration. Regen Med. 2016;11:559–70. doi: 10.2217/rme-2016-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grounds MD. Obstacles and challenges for tissue engineering and regenerative medicine: Australian nuances. Clin Exp Pharmacol Physiol. 2018;45:390–400. doi: 10.1111/1440-1681.12899. [DOI] [PubMed] [Google Scholar]
- 83.Feil G, Daum L, Amend B, Maurer S, Renninger M, Vaegler M, et al. From tissue engineering to regenerative medicine in urology: the potential and the pitfalls. Adv Drug Deliv Rev. 2011;63:375–8. doi: 10.1016/j.addr.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 84.Aragon IM, Imbroda BH, Lara MF. Cell therapy clinical trials for stress urinary incontinence: current status and perspectives. Int J Med Sci. 2018;15:195–204. doi: 10.7150/ijms.22130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Adamowicz J, Kowalczyk T, Drewa T. Tissue engineering of urinary bladder-current state of art and future perspectives. Cent European J Urol. 2013;66:202–6. doi: 10.5173/ceju.2013.02.art23. [DOI] [PMC free article] [PubMed] [Google Scholar]