Abstract
Purpose
Dental problems in young children are wide-spread and can negatively impact quality of life. We examined the effect of enrollment in North Carolina Early Head Start (EHS)—a federally funded early education program for children under three years of age and their families—on oral health-related quality of life (OHRQoL).
Methods
In this quasi-experimental study, we interviewed 479 EHS and 699 Medicaid matched parent–child dyads at baseline (children’s average age 10 months) and 24 months later. Parents reported OHRQoL using the Early Childhood Oral Health Impact Scale (ECOHIS), a 0–52 point scale with higher scores representing more negative impacts. We used a marginalized semicontinuous two-part model to estimate: (1) the effect of EHS on the probability of reporting any follow-up impacts (ECOHIS ≥ 1), and (2) the difference in overall mean ECOHIS follow-up scores. We controlled for baseline ECOHIS, language, and EHS and non-EHS group imbalances using a propensity score.
Results
At follow-up, negative OHRQoL impacts were more often reported by parents of non-EHS than EHS children (45 versus 37%, P < .01). In the adjusted model, EHS parents reported a lower odds of negative OHRQoL impacts (OR 0.70; 95% CI 0.52, 0.94). Mean adjusted ECOHIS scores were not significantly different (EHS: 1.59 ± 3.34 versus non-EHS: 2.11 ± 3.85, P > 0.05).
Conclusions
This study is the first to demonstrate that families of young children enrolled in EHS report improved OHRQoL compared to their non-enrolled peers. These results highlight the potential effectiveness of improving the quality of life of low-resource families through early childhood education.
Keywords: Early intervention, Quality of life, Child health services, Disparities, Oral health, Healthcare disparities
Introduction
Oral health-related quality of life (OHRQoL) can be defined as “the impact of oral disorders on aspects of everyday life that are important to patients and persons, with those impacts being of sufficient magnitude, whether in terms of severity, frequency or duration, to affect an individual’s perception of their life overall [1].” OHRQoL is not only “the absence of negative impacts of oral conditions on social life,” but also “a positive sense of dentofacial self-confidence” which mirrors both the absence of disease and promotion of health in the World Health Organization (WHO) definition of health [2, 3]. According to the WHO, “oral health affects general health by causing considerable pain and suffering and by changing what people eat, their speech and their quality of life and well-being [4].” The physical and psychological influences of oral conditions may have a particularly negative affect on children, who need nutrition and sleep for growth and development, are developing speech, have fewer coping skills for pain and discomfort than adults, and are developing social skills that may be affected by their appearance [5, 6].
Dental caries, the most common chronic disease in childhood, is associated with worse OHRQoL [7–12], especially when it is left untreated [11]. Dental caries in young children can be associated with high treatment costs and distress to the family, resulting in additional physical and psychological influences on the child and family [5, 6]. Dental treatment is associated with improved OHRQoL [13–16], but outcomes can vary by the characteristics of families seeking treatment, including socioeconomic status and oral health literacy [17, 18]. The impact of clinical conditions on OHRQoL also can extend to the process of accessing treatment, which in and of itself can have a negative impact on low-income families, particularly when access to care is limited as it is with dentistry [19, 20].
Early Head Start (EHS) is a national social program that potentially can improve the OHRQoL of low-income families and children birth to 3 years of age [21], a group at elevated risk for poor oral health [22]. EHS provides comprehensive family services and support, improves social and cognitive development long term [23–26], and operates according to comprehensive Federal performance standards that integrate oral health into daily programmatic activities [27]. As an extension of the Head Start program, EHS and Head Start share the same oral health performance standards related to tooth brushing with fluoridated toothpaste, oral health education, and determination of a child’s oral health status by a dental professional [27]. Yet to the authors’ knowledge, the effect of EHS on OHRQoL has not been examined.
The purpose of this study was to determine whether participation in EHS had an impact on the family’s OHRQoL. We hypothesized that EHS participation would improve OHRQoL because of its potential to: (1) reduce the occurrence of dental disease through preventive services it provides, and (2) facilitate access to dental providers who also can provide services that will reduce the burden of dental disease in children. The causal pathway for dental caries and OHRQoL is well established so a reduction in this disease should result in improved OHRQoL [10–12].
Methods
Overview of parent study design
We used data collected from the Zero Out Early Childhood Caries (ZOE) study, a pre-post 24-month longitudinal, prospective, non-randomized study to determine the effect of EHS on oral health outcomes in young children. In the ZOE study, the EHS group was compared with a control group of Medicaid-enrolled children not participating in EHS. Teachers and staff in EHS programs received didactic training in oral health and communication techniques totaling about two hours to bolster awareness of EHS performance standards and facilitate their implementation. The study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
Study population
Subjects were recruited to the ZOE study through a 3-step process described in detail in a previous publication [28]: (1) enrollment of EHS programs, (2) enrollment of parent– child dyads within EHS programs, and (3) enrollment of community-matched parent–child dyads to serve as controls. In step one, all North Carolina EHS programs were invited to participate; all except one were enrolled. In step two, parents of EHS children younger than 19 months were recruited by the research team from all participating EHS programs. In step three, Medicaid-enrolled children of the same age, language, and residential ZIP codes and their parents were randomly selected and recruited as the control group through direct mailings from the North Carolina Medicaid program. Our final sample included EHS and non-EHS parent–child dyads clustered within 25 of the 26 North Carolina EHS programs.
Trained personnel conducted in-person, computer-assisted, structured interviews with parents of eligible children at baseline and approximately 24 months later (the time children aged out of the EHS program). The outcome variable of interest, OHRQoL, was included during one-hour interviews at both baseline and follow-up. Follow-up QHRQoL scores were the primary outcome used in the analysis of EHS enrollment effects for this paper. Interviews were conducted in English or Spanish, as appropriate. Baseline interviews were conducted from September 2010 to July 2012 and follow-up interviews from November 2012 to March 2014. At follow-up, we interviewed the same parent–child dyads that participated in the baseline interview.
Conceptual framework
We used a general health-related quality of life conceptual model developed by Ferrans and colleagues (2005) in which both individual and environmental characteristics affect factors (biological function, symptoms, functional status, and general health perceptions) that in turn affect health-related quality of life [29]. We considered early childhood education programs to be part of the environmental characteristics domain that can affect children’s OHRQoL. For example, EHS programs provide multiple services for the child and parent (e.g., education, nutrition, tooth brushing, and dental healthcare referrals) that can impact children’s symptoms, functional status, and general health perceptions. These direct effects on the child and family are supported by an early education and childcare framework proposed by Friedman-Krauss and Barnett [30] and an ecological child development framework proposed by Bronfenbrenner [31].
Variable definitions
The main independent variable, EHS enrollment, was supplied by EHS staff and confirmed by the parent at the baseline enrollment screening and interview. It was treated as a binary variable.
The dependent variable, OHRQoL at follow-up, was measured using the 13-item early childhood oral health impact scale (ECOHIS), the most frequently used scale for assessing OHRQoL among preschool children and families [18, 32]. ECOHIS items (Table 1) queried parents about the frequency of lifetime impacts of dental problems or treatments (0 = never; 1 = hardly ever; 2 = occasionally; 3 = often; 4 = very often). The total score across the 13 items can range from 0 (best) to 52 (worst). In addition, separate sub-scores were calculated for the 9 items related to the child (range from 0 to 36) and the 4 items for the family (range from 0 to 16) [32]. Child impact included four domains (Child symptom, Child function, Child psychology, and Child self-image). Family impact comprised two domains (Parent distress and Family function). We excluded observations with missing responses to >2 child items or >1 family item (n = 22); otherwise, we performed simple imputation of the mean from the remaining items (baseline n = 128, follow-up n = 49).
Table 1.
Baseline child characteristics of the ZOE study population, by Early Head Start (EHS), and Non-Early Head Start (Non-EHS) groups
| EHS (n = 468) | Non-EHS (n = 688) | P valuea | |
|---|---|---|---|
| Characteristic | % | % | |
| Age (months) [mean, SD (range)] | 10.6, 4.8 (0–19) | 10.4, 4.6 (1–19) | 0.351 |
| Gender | 0.226 | ||
| Male | 54.17% | 50.4% | |
| Female | 45.9% | 49.6% | |
| Race and ethnicity | <0.001 | ||
| Non-Hispanic White | 17.5% | 36.8% | |
| Non-Hispanic Black | 37.8% | 19.5% | |
| Non-Hispanic Native American | 2.4% | 1.2% | |
| Non-Hispanic Other, Single Race/Ethnicity | 0.0% | 1.0% | |
| Non-Hispanic Other, Multiple Races/Ethnicities | 7.5% | 10.9% | |
| Hispanic | 34.2% | 30.4% | |
| Missing | 0.6% | 0.3% | |
| Language | 0.633 | ||
| English | 74.8% | 76.0% | |
| Spanish | 25.2% | 24.0% | |
| Enrolled in public health insurance | 0.441 | ||
| Yes | 98.3% | 98.8% | |
| No | 1.7% | 1.2% | |
| Physical, learning, or mental health limitations | 0.160 | ||
| Yes | 4.5% | 2.9% | |
| No | 94.9% | 95.8% | |
| Don’t know | 0.6% | 1.3% | |
| Ever been homeless or not had a regular place to live | 0.002 | ||
| Yes | 4.7% | 1.6% | |
| No | 95.1% | 98.3% | |
| Don’t know | 0.2% | 0.1% | |
| Number of children in the household under 5 years of age [mean, SD (range)] | 1.8, 1.0 (1–7) | 1.4, 0.6 (1–5) | <0.001 |
| Number of children in the household between 5 and 17 years of age [mean, SD (range)] | 1.0, 1.2 (0–5) | 0.7, 1.1 (0–5) | 0.0014 |
| Number of adults in the household over 17 years of age [mean, SD (range)] | 2.1, 1.0 (0–7) | 2.2, 1.0 (1–9) | 0.0044 |
N number of subjects in stratum, SD standard deviation
Note Due to rounding, percentages may not add to exactly 100%
The p-values are for Chi-square tests or t-tests comparing EHS and non-EHS groups. For the Chi-square test, “don’t know” and “missing” values were excluded, and categories were combined if the expected count for a particular cell was less than five to satisfy the test’s assumptions
The dental literature recommends the use of both prevalence and severity estimates when reporting OHRQoL [33–40]. Because they provide complimentary information that can improve the interpretation of quality of life data, we used both estimates as outcomes for this study. No convention for defining the prevalence of OHRQoL exists, particularly for young children, so we arbitrarily chose a threshold of ≥1 negative impacts due to any reason at the level of “hardly ever” or more frequently. This decision was made because of the high frequency of “never” responses for all of the ECOHIS items and the potential for improvement in measurement sensitivity of the ECOHIS in detecting negative impacts to OHRQoL. Because health-related QoL scales use other thresholds, we conducted a sensitivity analysis in which we set the threshold for prevalence at the level of “occasionally” or more frequently. Overall severity for OHRQoL was defined as the mean of all individual ECOHIS scores at follow-up.
We included two baseline covariates in the models because of their potential impact on follow-up OHRQoL: ECOHIS score and survey language (Spanish or English). The Spanish language version of ECOHIS has not been as widely used or tested as the English version, but its construct validity and internal consistency were demonstrated in a previous study [41]. A cross-sectional analysis of baseline interviews in the ZOE study found that Spanish-speaking parents reported a lower severity of ECOHIS impacts [28]. Because of the differences between the Spanish- and English-speaking families in the baseline scores, we included interview language (Spanish or English) in the analyses.
Analytical approach
We used descriptive statistics to explore the distribution of the children’s demographic characteristics and ECOHIS scores overall and by group.
Overview of regression modeling
We used an as-assigned “intent to treat” analysis of EHS because it is more generalizable and estimates the impact of EHS policies as implemented. For the analytic models, we controlled for clustering of subjects within EHS programs (n = 25) and estimated the impact of EHS on OHRQoL using random effects models. These clusters correspond to geographic areas (ZIP codes) where EHS and non-EHS study participants reside. Because of the random effect, prevalence was defined conditional on the residential ZIP code level as the probability that a representative child in EHS (or Non-EHS) in a ZIP code had a negative impact to OHRQoL. We controlled for baseline OHRQoL, survey language, and directly adjusted for a generalized boosted model propensity score covariate [42]. The propensity score adjusted for 47 observed characteristics that may be imbalanced between the EHS and non-EHS samples, which may in turn confound our estimates of the impact of EHS enrollment on OHRQoL.
Marginalized semicontinuous two-part model with random effects
We used a marginalized semicontinuous two-part model with random effects to estimate the effect of EHS on ECOHIS prevalence and mean ECOHIS severity scores at follow-up [43–45]. We used a semicontinuous model because our outcome, ECOHIS, has a large proportion of zeros (58%). The two-part model coupled a logistic model for the probability of any negative impact to OHRQoL with an exponential model to assess covariate effects on overall mean ECOHIS, thus providing straightforward interpretation while accounting for skewed distributions such as those with a significant number of zeros [44]. The difference between the marginalized semicontinuous two-part model and the traditional semicontinuous two-part model was that the former models the overall mean of ECOHIS that includes zeros while the latter models the mean of ECOHIS of the positive responses only. The first part of the two models was the same [46].
The first part of the marginalized semicontinuous model [43] was a logistic regression with random effects to examine the effect of the binary independent variable, EHS, on ECOHIS prevalence at follow-up (ECOHIS ≥ 1).
| (1) |
where πij was the probability of having any negative impact to OHRQoL (ECOHIS ≥ 1) at follow-up for the jth child in the ith EHS program cluster conditional on the cluster-specific effect, bi. The model had the following independent variables:
x1i = EHS enrollment (treatment indicator, dichotomous),
x2ij = any negative impact to OHRQoL (ECOHIS ≥ 1) at baseline (dichotomous),
x3ij = Survey language (dichotomous: Spanish, English),
x4ij = Generalized boosted model propensity score (continuous).
In particular, bi was a normally distributed random effect for each EHS program cluster (N = 25) where . The EHS cluster-specific odds ratio, eβ1, was the odds of having any negative impact to OHRQoL (ECOHIS ≥ 1) by a child in EHS relative to the odds for a child not in EHS, conditional on the EHS and non-EHS child being from the same geographic area.
The second part of the marginalized semicontinuous two-part model was
| (2) |
where νij was the overall mean ECOHIS score (including ECOHIS = 0) at follow-up for the jth child in the ith EHS program cluster conditional on the cluster-specific effect, di. Furthermore, (bi, di) were assumed to be bivariately normally distributed with the variance
where σ1 and σ2 are standard deviations of bi and di, respectively, and ρ was their correlation. The EHS cluster-specific mean ratio, eα1, was the multiplicative increase in mean OHRQoL for a child in EHS relative to the mean OHRQoL for a child not in EHS, conditional on the EHS and non-EHS child from the same geographic area.
We fit the model with both skew log-normal and generalized gamma distributions [45] and chose the model with the best fit based on the lowest Akaike information criterion (AIC). Maximum likelihood estimation of the semicontinuous model was performed using SAS/STAT® version 9.4 (SAS, 2013).
Results
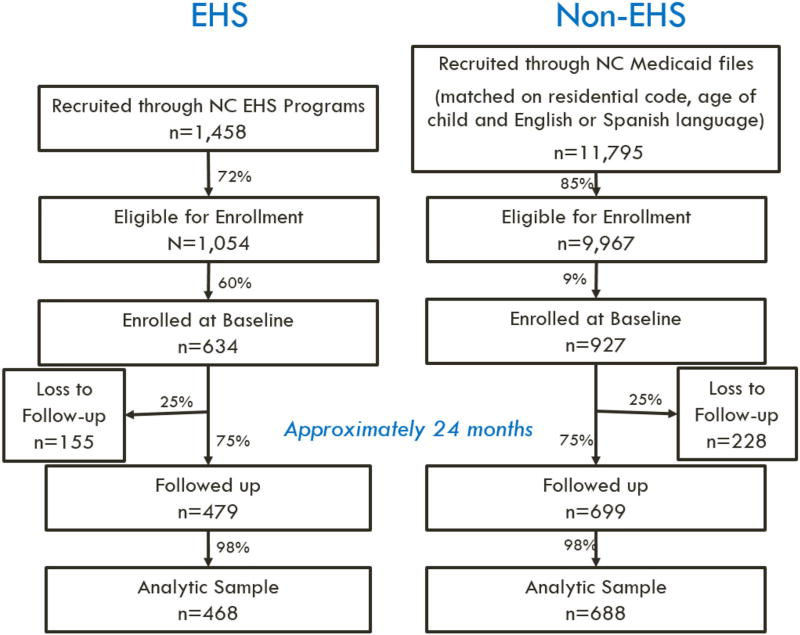
The ZOE study enrolled 1561 child–parent dyads (n = 634 EHS, n = 927 non-EHS), which included an estimated 60% of the eligible EHS sample and 9% of the eligible controls not enrolled in EHS (Fig. 1). Our final analytic sample with baseline and follow-up interviews included 468 parent–child dyads from EHS programs and 688 non-EHS controls (Fig. 1). Baseline characteristics of the EHS and non-EHS children were similar with respect to age, gender, enrollment in public health insurance, and physical, learning, or mental health limitations; however, more children in EHS had been homeless and belonged to minority race and ethnicity compared to children not enrolled in EHS (Table 1). On average, families with children in EHS had more children and fewer adults in the household compared to controls (Table 1).
Fig. 1.
Data collection for the Zero Out Early Childhood Caries (ZOE) study by EHS Group
For the child impact section of the ECOHIS, ‘pain in the teeth, mouth or jaws’ was the most frequently reported item by the parents at follow-up in both the EHS (19.9%) and non-EHS groups (27.0%) (Table 2). A reduction in negative impacts from baseline to follow-up occurred for this item in both the EHS (Baseline = 41.0%, Follow-up = 19.9%) and non-EHS groups (Baseline = 49.9%, Follow-up = 27.0%). The next most commonly reported ECOHIS items at follow-up were “How often has your child had trouble sleeping because of dental problems or dental treatments?” and “How often has your child been irritable or frustrated because of dental problems or dental treatments?” for both the EHS (9.0% and 17.5%, respectively) and non-EHS groups (13.2% and 24.6%, respectively). The responses to the questions were skewed because most participants responded ‘never’ to items in the ECOHIS instrument in both the EHS (80.1–98.1%) and non-EHS (73.0–97.2%) groups (Table 2).
Table 2.
Frequencies of responses to items in the oral health-related quality of life scale, early childhood oral health impact scale (ECOHIS), for the ZOE study population at 24-month follow-up and baseline (EHS n = 468, Non-EHS n = 688, N = 1156)
| ECOHIS instrument item | ECOHIS response (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Never | Hardly Ever | Occasionally | Often | Very Often | Missinga | |||||||
|
|
|
|
|
|
|
|||||||
| EHS (%) |
Non- EHS (%) |
EHS (%) |
Non- EHS (%) |
EHS (%) |
Non- EHS (%) |
EHS | Non- EHS (%) |
EHS | Non- EHS (%) |
EHS | Non- EHS (%) |
|
| 24-month follow-up | ||||||||||||
| 1. How often has your child had pain in the teeth, mouth or jaws? | 80.1 | 73.0 | 9.4 | 13.7 | 8.1 | 11.2 | 1.1 | 1.0 | 0.4 | 0.7 | 0.9 | 0.4 |
| How often has your child … because of dental problems or dental treatments? | ||||||||||||
| 2. Had difficulty drinking hot or cold beverages | 96.4 | 93.2 | 2.8 | 4.1 | 0.6 | 1.9 | 0.2 | 0.3 | 0.0 | 0.4 | 0.0 | 0.1 |
| 3. Had difficulty eating some foods | 92.5 | 91.4 | 5.1 | 4.1 | 1.7 | 2.8 | 0.4 | 0.9 | 0.0 | 0.6 | 0.2 | 0.3 |
| 4. Had difficulty pronouncing any words | 94.7 | 94.0 | 2.6 | 2.3 | 1.1 | 1.2 | 0.2 | 1.0 | 0.2 | 0.7 | 1.3 | 0.7 |
| 5. Missed preschool, daycare or school | 93.2 | 97.2 | 5.1 | 2.2 | 1.5 | 0.4 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.1 |
| 6. Had trouble sleeping | 91.0 | 86.8 | 4.9 | 7.6 | 3.8 | 5.1 | 0.0 | 0.4 | 0.0 | 0.0 | 0.2 | 0.1 |
| 7. Been irritable or frustrated | 82.5 | 75.4 | 8.3 | 13.2 | 7.5 | 10.0 | 0.9 | 0.6 | 0.6 | 0.6 | 0.2 | 0.1 |
| 8. Avoided smiling or laughing | 96.6 | 96.7 | 2.1 | 2.8 | 0.6 | 0.3 | 0.0 | 0.1 | 0.0 | 0.0 | 0.6 | 0.1 |
| 9. Avoided talking | 97.0 | 97.1 | 1.9 | 2.0 | 0.6 | 0.3 | 0.0 | 0.3 | 0.0 | 0.0 | 0.4 | 0.3 |
| How often have you or another family member … because of your child’s dental problems or treatments? | ||||||||||||
| 10. Been upset | 93.8 | 89.1 | 2.6 | 4.5 | 3.4 | 5.1 | 0.2 | 0.7 | 0.0 | 0.4 | 0.0 | 0.1 |
| 11. Felt guilty | 92.7 | 89.7 | 2.4 | 3.5 | 3.0 | 4.1 | 1.5 | 2.0 | 0.4 | 0.6 | 0.0 | 0.1 |
| 12. Taken time off from work | 87.8 | 86.8 | 6.4 | 7.1 | 4.1 | 5.1 | 1.1 | 0.7 | 0.6 | 0.3 | 0.0 | 0.0 |
| 13. How often has your child had dental problems or dental treatments that had a financial impact on your family? | 98.1 | 95.9 | 1.3 | 3.2 | 0.2 | 0.7 | 0.2 | 0.1 | 0.2 | 0.0 | 0.0 | 0.0 |
| Baseline | ||||||||||||
| 1. How often has your child had pain in the teeth, mouth or jaws? | 59.0 | 50.1 | 8.1 | 7.3 | 19.0 | 28.2 | 8.3 | 9.7 | 4.5 | 4.1 | 1.1 | 0.6 |
| How often has your child … because of dental problems or dental treatments? | ||||||||||||
| 2. Had difficulty drinking hot or cold beverages | 93.6 | 92.0 | 4.5 | 4.4 | 0.6 | 1.7 | 0.2 | 0.3 | 0.0 | 0.3 | 1.1 | 1.3 |
| 3. Had difficulty eating some foods | 90.2 | 89.1 | 5.8 | 4.7 | 2.8 | 4.2 | 0.4 | 0.7 | 0.2 | 0.1 | 0.6 | 1.2 |
| 4. Had difficulty pronouncing any words | 95.5 | 96.4 | 1.9 | 1.5 | 0.2 | 0.9 | 0.0 | 0.0 | 0.4 | 0.0 | 1.9 | 1.3 |
| 5. Missed preschool, daycare or school | 94.4 | 98.3 | 2.4 | 1.3 | 1.9 | 0.3 | 0.6 | 0.0 | 0.2 | 0.0 | 0.4 | 0.1 |
| 6. Had trouble sleeping | 74.4 | 66.4 | 7.5 | 10.2 | 13.5 | 18.5 | 3.6 | 3.2 | 0.9 | 1.0 | 0.2 | 0.7 |
| 7. Been irritable or frustrated | 60.9 | 51.7 | 10.5 | 9.9 | 19.7 | 27.0 | 5.8 | 8.9 | 3.0 | 2.3 | 0.2 | 0.1 |
| 8. Avoided smiling or laughing | 90.8 | 88.7 | 6.0 | 5.8 | 2.6 | 4.7 | 0.6 | 0.6 | 0.0 | 0.1 | 0.0 | 0.1 |
| 9. Avoided talking | 95.7 | 94.8 | 2.4 | 3.5 | 0.9 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | 1.1 | 0.6 |
| How often have you or another family member … because of your child’s dental problems or treatments? | ||||||||||||
| 10. Been upset | 90.2 | 84.9 | 3.6 | 6.4 | 4.5 | 6.8 | 1.3 | 1.2 | 0.2 | 0.4 | 0.2 | 0.3 |
| 11. Felt guilty | 94.4 | 91.7 | 0.9 | 3.2 | 3.6 | 3.3 | 0.6 | 0.7 | 0.4 | 0.9 | 0.0 | 0.1 |
| 12. Taken time off from work | 93.8 | 94.8 | 2.6 | 2.6 | 2.6 | 2.2 | 0.6 | 0.3 | 0.4 | 0.1 | 0.0 | 0.0 |
| 13. How often has your child had dental problems or dental treatments that had a financial impact on your family? | 98.5 | 98.0 | 1.1 | 1.6 | 0.4 | 0.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
Child impact: Items 1–9, Family impact: Items 10–13. Child symptom domain = 1; Child function domain = 2–5; Child psychology = 6, 7; Child self-image domain = 8, 9; Parent distress domain = 10, 11; Family function domain = 12, 13
Missing values were imputed with the mean score of the remaining items
Effect of EHS on ECOHIS Prevalence
The unadjusted ECOHIS prevalence at follow-up was lower for EHS compared to non-EHS families (37 vs. 45%, P <0.01), indicating that EHS families were less likely to experience negative impacts on their OHRQoL (Table 3). We also found a statistically significant difference at follow-up in the unadjusted prevalence between EHS and non-EHS groups for overall child impact scores, child symptoms, child psychology, and parent distress (Table 3).
Table 3.
Characteristics of the oral health-related quality of life scale, early childhood oral health impact scale (ECOHIS), for the ZOE study population at 24-month follow-up and baseline
| ECOHIS instrument and subscale (No. items) | EHS (n = 468) | Non-EHS (n = 688) | ||
|---|---|---|---|---|
|
|
|
|||
| Prevalence (%)a | Severityb | Prevalence (%)a | Severityb | |
| 24-Month follow-up | ||||
| Overall scale (13)d,* | 36.8 | 1.59 (3.34) | 45.3 | 2.11 (3.85) |
| Child overall (9)d,* | 32.1 | 1.11 (2.43) | 40.6 | 1.46 (2.75) |
| Child symptoms (1)d,* | 19.9 | 0.31 (0.70) | 27.0 | 0.42 (0.78) |
| Child function (4) | 15.4 | 0.31 (1.00) | 15.0 | 0.40 (1.28) |
| Child psychology (2)d,* | 17.7 | 0.41 (1.01) | 25.7 | 0.57 (1.13) |
| Child self-image (2) | 4.5 | 0.08 (0.40) | 4.4 | 0.07 (0.43) |
| Family overall (4) | 17.7 | 0.48 (1.30) | 21.9 | 0.65 (1.54) |
| Parent distress (2)c,* | 9.6 | 0.25 (0.87) | 14.7 | 0.39 (1.11) |
| Family function (2) | 12.6 | 0.24 (0.73) | 14.2 | 0.26 (0.71) |
| Baseline | ||||
| Overall scale (13)c,* | 51.7 | 3.13 (4.52) | 59.0 | 3.80 (4.70) |
| Child overall (9)c,* | 50.6 | 2.71 (3.75) | 58.1 | 3.28 (3.83) |
| Child symptoms (1)d,** | 41.0 | 0.90 (1.23) | 49.8 | 1.09 (1.24) |
| Child function (4) | 17.1 | 0.36 (1.00) | 15.8 | 0.34 (1.00) |
| Child psychology (2)d,** | 41.0 | 1.28 (1.88) | 49.6 | 1.61 (1.97) |
| Child self-image (2) | 10.7 | 0.18 (0.60) | 12.6 | 0.24 (0.72) |
| Family overall (4) | 16.0 | 0.42 (1.23) | 19.5 | 0.52 (1.31) |
| Parent distress (2)c,* | 12.6 | 0.29 (0.91) | 17.7 | 0.41 (1.06) |
| Family function (2) | 7.1 | 0.13 (0.54) | 6.3 | 0.11 (0.47) |
EHS early head start
Prevalence: ≥ 1 impacts (number of observations, percentage)
Severity: Mean sum of scores (standard deviation)
P < 0.05 for Chi-square test comparing the prevalence of ≥ 1 impacts between the EHS and non-EHS groups
P < 0.01 for Chi-square test comparing the prevalence of ≥ 1 impacts between the EHS and non-EHS groups
P < 0.05 for t-test comparing the severity (mean ECOHIS score) between the EHS and non-EHS groups
P < 0.01 for t-test comparing the severity (mean ECOHIS score) between the EHS and non-EHS groups
The adjusted model with the generalized gamma distribution had a lower AIC compared to the skew log-normal distribution, and was therefore chosen as the model with the better fit. In the adjusted results, we continued to find a statistically significant difference between the EHS and non-EHS families in ECOHIS prevalence. When controlling for baseline ECOHIS score, survey language, and the propensity score covariate, children enrolled in EHS had lower odds of having any negative impacts to their OHRQoL compared to non-EHS families within the same cluster (aOR 0.70; 95% CI 0.52, 0.94) (Table 4). In terms of marginal effects, EHS enrollment was associated with a 10.0% point (95% CI −16.8, −3.2) decrease in the probability of having any negative impact to OHRQoL compared to non-EHS families at follow-up. Little difference was found in the results when ECOHIS prevalence was dichotomized as “never/hardly ever” versus “occasionally/often/very often” (aOR 0.73, 95% CI 0.52, 1.01).
Table 4.
Generalized gamma marginalized semicontinuous two-part model on the effect of early head start (EHS) on the overall mean early childhood oral health impact scale (ECOHIS) score (N = 1,156)
| Parameter | Parameter estimate |
Model-based standard error |
Empirical standard errors |
Exponentiation of parametera |
95% Confidence intervala |
|
|---|---|---|---|---|---|---|
| Probability of having an any impacts (ECOHIS ≥ 1) | Odds ratio | |||||
| EHS | α1 | −0.36* | 0.15 | 0.14 | 0.70* | 0.52, 0.94 |
| ECOHIS Score at Baseline | α2 | 0.63** | 0.13 | 0.14 | 1.88** | 1.41, 2.51 |
| Survey Language | α3 | 0.35* | 0.16 | 0.17 | 1.42* | 1.00, 2.01 |
| Propensity Score | α3 | 0.22 | 0.38 | 0.29 | 1.25 | 0.69, 2.27 |
| Constant | α0 | –0.93** | 0.21 | 0.20 | 0.39** | 0.26, 0.59 |
| Overall mean ECOHIS score | Mean ratio | |||||
| EHS | β1 | −0.19 | 0.13 | 0.16 | 0.82 | 0.59, 1.15 |
| ECOHIS score at baseline | β2 | 0.43** | 0.11 | 0.11 | 1.54** | 1.24, 1.92 |
| Survey language | β3 | 0.13 | 0.14 | 0.16 | 1.14 | 0.82, 1.59 |
| Propensity score | β4 | −0.04 | 0.32 | 0.33 | 0.96 | 0.48, 1.92 |
| Constant | β0 | 0.34 | 0.21 | 0.19 | 1.40 | 0.95, 2.07 |
| Σ | 0.82** | 0.03 | 0.03 | |||
| κ | −0.32* | 0.14 | 0.15 | |||
| ρ | 0.93** | 0.12 | 0.06 | |||
| θ1 | 0.27* | 0.09 | 0.09 | |||
| θ2 | 0.28* | 0.09 | 0.12 | |||
ECOHIS with random effects for each of the 25 EHS clusters. Akaike Information Criterion 3866.5, Log Likelihood 3836.5
P < 0.05,
P < 0.01
For model with empirical standard errors
Effect of EHS on ECOHIS Severity
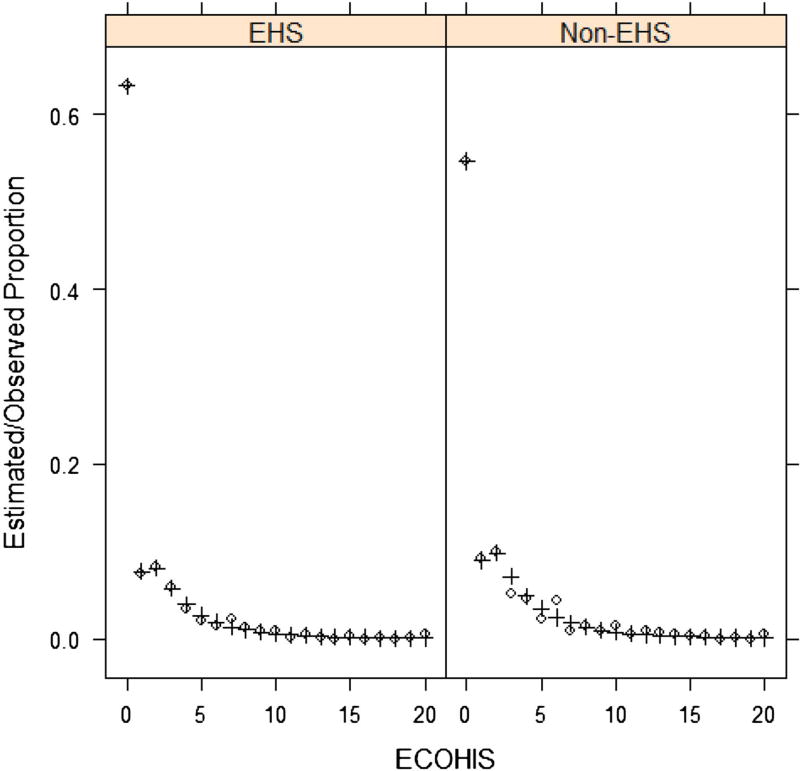
Children in EHS had lower ECOHIS severity scores than non-EHS children at baseline (3.13 vs. 3.80, P = 0.02) and follow-up (1.59 vs. 2.11, P = 0.02) (Fig. 2; Table 3). Differences between EHS and non-EHS families also were found in unadjusted severity scores for child impacts overall (P = 0.03) and for child symptoms (P = 0.01) and child psychology domains (P = 0.02) (Table 3). Similar to prevalence, the unadjusted severity score for parent distress was lower in the EHS group compared to the non-EHS group (P = 0.02) (Table 3). ECOHIS severity scores also decreased similarly for both groups from baseline to follow-up: 49% for EHS [3.13 to 1.59] and 44% for non-EHS [3.80 to 2.11] (Table 3).
Fig. 2.
Proportion of early head start (EHS) and Non-EHS with each early childhood oral health impact scale (ECOHIS) score (N = 1156). ECOHIS scores at 20 represent all higher observations (total seven participants). Circles represent the observed values and Pluses represent the estimated values using the generalized gamma marginalized semicontinuous two-part model
After adjusting for baseline ECOHIS scores, survey language, and the propensity score covariate, overall mean ECOHIS severity scores among children in EHS were not significantly different at follow-up from those not enrolled in EHS within the same cluster (adjusted mean ratio = 0.82; 95% CI 0.59, 1.15) (Table 4).
Discussion
We undertook this study to determine the impact that enrollment in EHS has on the OHRQoL and their families. We found improvement in OHRQoL prevalence (ECOHIS ≥ 1) in the EHS group compared to non-EHS group of Medicaid-enrolled children, which suggests that EHS enrollment might have had an impact on OHRQOL. But the effect size for prevalence was small and no reduction in ECOHIS severity scores could be attributed to the EHS enrollment.
We conclude that EHS participation positively affected OHRQoL prevalence, in that the odds of having any negative impacts to OHRQoL was 10% less at follow-up for those enrolled in EHS compared to those not enrolled. The influence of EHS on ECOHIS prevalence is supported by Ferrans and colleagues’ conceptual model [29]. According to our application of the model, EHS staff provide a supportive environment that reduces oral health-related symptoms, which improves functional status and general health perceptions for the child. This supportive environment includes daily oral health practices by EHS staff, such as tooth brushing with fluoridated toothpaste, oral health education of families, and services that facilitate and encourage child dental visits [21].
However, the observed effect size for the reduction in prevalence is small, and the analysis of severity scores, one of our two primary outcomes, does not support an EHS effect. Although different at a statistically significant level in the unadjusted analysis, we found the mean number of impacts from child dental experiences to be similar in EHS and non-EHS groups in the adjusted analysis.
Two additional aspects of OHRQoL severity scores provide countervailing arguments for EHS enrollment having a major effect on OHRQoL. Although OHRQoL scores differed between EHS and non-EHS at a statistically significant level at baseline and at follow-up, scores declined by about the same magnitude over the 24-month study period in both groups. Mean ECOHIS scores decreased from 3.13 per child overall at the baseline interview to 1.59 at follow-up for the EHS group; from 3.80 to 2.11 for the non-EHS group. Another study similarly observed a decrease in OHRQoL severity over an 11-month period for children of 0 to 6 years of age in an untreated control group in Australia [48, 49]. Findings from our study supported by others could be interpreted to mean that some factor other than EHS was contributing to the improvement in OHRQoL. Some potential explanations for a decrease in scores for young children in both groups may be related to teething as infants, decreased worry, and distress in parents as they obtain more information and experience in child rearing, and less constant caretaking by the parent with the child’s enrollment in childcare programs.
A second aspect of the OHRQoL scores that could point to the absence of an EHS effect relates to the items in ECOHIS that seem to be important. Three items contributed significantly to the difference in OHRQoL scores between the EHS and non-EHS groups (pain, trouble sleeping, and irritable or frustration). These items could be related to biological factors that can provide temporary and important negative impacts on OHRQoL, but ones not routinely considered for interventions in early education and childcare programs [10–12]. In this high-risk population, however, pain probably is largely the consequence of dental caries, a preventable process. Therefore, mitigating their impact in the EHS group is desirable.
The absence of a statistically significant difference in the adjusted severity scores between EHS and non-EHS children may reflect the low overall mean scores at follow-up when the children were approximately 36 months old. The unadjusted mean ECOHIS scores were less than 3 for both the EHS and non-EHS groups while the ECOHIS has a possible range from 0 to 52. Our results suggest that families in this study reported a small number of negative impacts to OHRQoL. With low severity scores overall, it would be difficult to achieve a statistically significant lower score, and thus reveal an impact of EHS on OHRQoL severity.
Our study has significance beyond its contributions to the effect of EHS programs on oral health outcomes. Low ECOHIS severity scores are preferred because they indicate fewer and less severe impacts of oral health problems. The low scores observed in this study are particularly noteworthy considering that the sample was drawn from a non-care seeking Medicaid population. Low frequency and severity of OHRQoL impacts also were found in other non-care seeking populations of children slightly older than those in this study [12, 17, 47].
To our knowledge, no other studies have evaluated the effect of an early childhood educational program on OHRQoL. Further, we were unable to find literature on the effects of early education programs on general health-related quality of life. OHRQoL is a cornerstone of dental health care because it influences health-seeking behavior and health practices. It is especially important in early education and childcare studies, when participating low-income families face major challenges in everyday life. Federally funded social programs, such as EHS, represent a critical structure through which benefits can be delivered to socioeconomically and clinically vulnerable families. This study adds to the growing body of literature on the short-and long-term benefits of comprehensive early childcare education, both overall and specific to dentistry in particular [24, 25, 50].
We believe this study to be the first one to apply marginalized semicontinuous two-part modeling with random effects, extending the marginalized semicontinuous two-part model for cross-sectional data [44] to clustered data. This approach is new to dental research, and this innovation is preferred, in our opinion, because it evaluates the effect of an early childhood education program using statistical techniques that determine overall treatment effects in a manner that is conceptually beneficial to and computationally convenient for dentistry and early education research.
Limitations
There are several limitations to this study. First, lack of random assignment of parent–child dyads to EHS and control groups can result in biased effect estimates. However, we used a Medicaid control group in which child–parent dyads were randomly selected from predetermined strata and used propensity scores during data analysis to overcome this limitation. Second, although the ECOHIS is a validated measure of OHRQoL, few studies have evaluated its performance longitudinally [48, 49], and the equivalence of the English and Spanish ECOHIS scores has not been well established for very young children. A previous study suggested some differences between English-and Spanish-speaking samples [28]. Future research is needed to establish the comparability between the English and Spanish ECOHIS. Thirdly, EHS programs are heterogeneous, and the participation of each family in EHS is unique. Although we accounted for the heterogeneity of each EHS program with random effects in our analysis, the oral health effects of EHS may also depend on the type of EHS program, length of enrollment in EHS, and other characteristics of EHS programs that were not included in the models. Additionally, future research is needed to determine whether the difference in impacts between the EHS and non-EHS groups is clinically significant. There is a need to define the minimally important difference for oral health impacts in children, particularly to inform the dichotomization of OHRQoL prevalence in future research. One strength of the ECOHIS instrument is that it is parent-reported, which suggests that differences between the EHS and non-EHS groups are meaningful to the parent.
We conclude that families of young children enrolled in EHS exhibit a small improvement in OHRQoL prevalence (ECOHIS ≥ 1) compared to their non-enrolled peers. However, further work is needed to better understand the negative impacts that a small change in the prevalence of OHRQoL might have on the lives of young, low-income children and their families, as well as the mechanism through which EHS might improve OHRQoL. Future work also is needed to investigate the impact of EHS on parent characteristics that can ultimately improve OHRQoL.
Acknowledgments
This research is supported by a grant from the National Institute of Dental and Craniofacial Research, Prevention of Dental Caries in Early Head Start Children, #R01 DE018236. This research was partially supported by a National Research Service Award Post-Doctoral Traineeship from the Agency for HealthCare Research and Quality sponsored by The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, #T32 HS000032.
Footnotes
Disclosures None of the authors has any financial interest related to the article.
Disclaimers The views expressed in the article are those of the authors and do not necessarily reflect the views of the National Institute of Dental and Craniofacial Research or the University of North Carolina at Chapel Hill.
References
- 1.Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure? Community Dentistry and Oral Epidemiology. 2007;35(6):401–411. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 2.Slade G. Assessment of oral health-related quality of life. In: Inglehart M, Magramain R, editors. oral health-related quality of life. Carol Stream: Quintessence; 2002. p. 29. [Google Scholar]
- 3.World Health Organization. [Accessed 3 June, 2016];World health organization definition of health. 2003 http://www.who.int/about/definition/en/print.html.
- 4.Sheiham A. Oral health, general health and quality of life. Bulletin of the World Health Organization. 2005;83(9):641. [PMC free article] [PubMed] [Google Scholar]
- 5.Oral Health in America: A report of the Surgeon General. Rockville, MD: U.S Department of Health and Human Services; 2000. [Google Scholar]
- 6.Locker D. Concepts of oral health, disease and the quality of life. In: Slade G, editor. Measuring oral health and quality of life. Chapel Hill: University of North Carolina, Dental Ecology; 1997. [Google Scholar]
- 7.Barbosa TS, Gaviao MB. Oral health-related quality of life in children: part II. Effects of clinical oral health status. A systematic review. International Journal of Dental Hygine. 2008;6(2):100–107. doi: 10.1111/j.1601-5037.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- 8.Onoriobe U, Rozier RG, Cantrell J, King RS. Effects of enamel fluorosis and dental caries on quality of life. Journal of Dental Research. 2014;93(10):972–979. doi: 10.1177/0022034514548705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abanto J, Tello G, Bonini GC, Oliveira LB, Murakami C, Bonecker M. Impact of traumatic dental injuries and malocclusions on quality of life of preschool children: A population-based study. International Journal of Paediatric Dentistry. 2015;25(1):18–28. doi: 10.1111/ipd.12092. [DOI] [PubMed] [Google Scholar]
- 10.Kramer PF, Feldens CA, Ferreira SH, Bervian J, Rodrigues PH, Peres MA. Exploring the impact of oral diseases and disorders on quality of life of preschool children. Community Dentistry and Oral Epidemiology. 2013;41(4):327–335. doi: 10.1111/cdoe.12035. [DOI] [PubMed] [Google Scholar]
- 11.Scarpelli AC, Paiva SM, Viegas CM, Carvalho AC, Ferreira FM, Pordeus IA. Oral health-related quality of life among Brazilian preschool children. Community Dentistry and Oral Epidemiology. 2013;41(4):336–344. doi: 10.1111/cdoe.12022. [DOI] [PubMed] [Google Scholar]
- 12.Wong HM, McGrath CP, King NM, Lo EC. Oral health-related quality of life in Hong Kong preschool children. Caries Research. 2011;45(4):370–376. doi: 10.1159/000330231. [DOI] [PubMed] [Google Scholar]
- 13.Almaz ME, Sonmez IS, Oba AA, Alp S. Assessing changes in oral health-related quality of life following dental rehabilitation under general anesthesia. Journal of Clinical Pediatric Dentistry. 2014;38(3):263–267. [PubMed] [Google Scholar]
- 14.Jankauskiene B, Virtanen JI, Kubilius R, Narbutaite J. Oral health-related quality of life after dental general anaesthesia treatment among children: A follow-up study. BMC Oral Health. 2014;14:81. doi: 10.1186/1472-6831-14-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cantekin K, Yildirim MD, Cantekin I. Assessing change in quality of life and dental anxiety in young children following dental rehabilitation under general anesthesia. Pediatric Dentistry. 2014;36(1):12E–17E. [PubMed] [Google Scholar]
- 16.Klaassen MA, Veerkamp JS, Hoogstraten J. Young children’s oral health-related quality of life and dental fear after treatment under general anaesthesia: A randomized controlled trial. European Journal of Oral Sciences. 2009;117(3):273–278. doi: 10.1111/j.1600-0722.2009.00627.x. [DOI] [PubMed] [Google Scholar]
- 17.Divaris K, Lee JY, Baker AD, Vann WFJ. Caregivers’ oral health literacy and their young children’s oral health-related quality-of-life. Acta Odontologica Scandinavica. 2012;70(5):390–397. doi: 10.3109/00016357.2011.629627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar S, Kroon J, Lalloo R. A systematic review of the impact of parental socio-economic status and home environment characteristics on children’s oral health related quality of life. Health and Quality of Life Outcomes. 2014;12:41. doi: 10.1186/1477-7525-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mofidi M, Rozier RG, King RS. Problems with access to dental care for Medicaid-insured children: What caregivers think. American Journal of Public Health. 2002;92(1):53–58. doi: 10.2105/ajph.92.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mofidi M, Zeldin LP, Rozier RG. Oral health of Early Head Start children: A qualitative study of staff, parents, and pregnant women. American Journal of Public Health. 2009;99(2):245–251. doi: 10.2105/AJPH.2008.133827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Early Head Start National Resource Center, Office of Head Start, Administration for Children and Families, U. S. Department of Health and Human Services. [Accessed 3 June, 2016];About Early Head Start. 2016 http://eclkc.ohs.acf.hhs.gov/hslc/tta-system/ehsnrc/about-ehs/about.html#about.
- 22.The Early Head Start National Resource Center, Office of Head Start, Administration for Children and Families, U. S. Department of Health and Human Services. [Accessed 3 June, 2016];Early Head Start program facts for fiscal year 2012. 2014 https://www.acf.hhs.gov/sites/default/files/occ/ehs_program_fact_sheet_fy_2012.pdf?nocache=1365609925.
- 23.Love JM, Brooks-Gunn J. Getting the most out of early head start: What has been accomplished and what needs to be done. In: Haskins R, Barnett WS, editors. Investing in young children: New directions in federal preschool and early childhood policy. Rutgers: Brookings and National Institute for Early Education Research; 2010. pp. 29–37. [Google Scholar]
- 24.Love JM, Chazan-Cohen R, Raikes H, Brooks-Gunn J. What makes a difference: Early Head Start evaluation findings in a developmental context. Monographs of the Society for Research in Child Development. 2013;78(1):1–173. doi: 10.1111/j.1540-5834.2012.00699.x. [DOI] [PubMed] [Google Scholar]
- 25.Love JM, Kisker EE, Ross C, et al. The effectiveness of Early Head Start for 3-year-old children and their parents: Lessons for policy and programs. Developmental Psychology. 2005;41(6):885–901. doi: 10.1037/0012-1649.41.6.88. [DOI] [PubMed] [Google Scholar]
- 26.Kranz AM, Rozier RG, Zeldin LP, Preisser JS. Oral health activities of Early Head Start teachers directed toward children and parents. Journal of Public Health Dentistry. 2011;71(2):161–169. doi: 10.1111/j.1752-7325.2011.00245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Head Start Bureau, Administration on Children, Youth and Families, U.S. Department of Health and Human Services. [Accessed 3 June 2016];Oral health—RevisionACF-PI-HS-06-03. 2006 http://eclkc.ohs.acf.hhs.gov/hslc/standards/PIs/2006/resour_pri_00109_122006.html.
- 28.Born CD, Divaris K, Zeldin LP, Rozier RG. Influences on preschool children’s oral health-related quality of life as reported by English and Spanish-speaking parents and caregivers. Journal of Public Health Dentistry. 2016 doi: 10.1111/jphd.12152. [DOI] [PubMed] [Google Scholar]
- 29.Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. Journal of Nursing Scholarship. 2005;37(4):336–342. doi: 10.1111/j.1547-5069.2005.00058.x. [DOI] [PubMed] [Google Scholar]
- 30.Friedman-Krauss A, Barnett WS. National Institute for Early Education Research Policy Brief, Tech. Rep. 25. New Brunswick, NJ: National Institute for Early Education Research; 2013. Early childhood education: Pathways to better health. [Google Scholar]
- 31.Bronfenbrenner, Urie. Toward an experimental ecology of human development. American Psychologist. 1977;32(7):513–531. [Google Scholar]
- 32.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children’s oral health: The early childhood oral health impact scale (ECOHIS) Health and Quality of Life Outcomes. 2007;5:6. doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gherunpong S, Tsakos G, Sheiham A. The prevalence and severity of oral impacts on daily performances in Thai primary school children. Health and Quality of Life Outcomes. 2004;2:57. doi: 10.1186/1477-7525-2-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kida IA, Astrom AN, Strand GV, Masalu JR, Tsakos G. Psychometric properties and the prevalence, intensity and causes of oral impacts on daily performance (OIDP) in a population of older Tanzanians. Health and Quality of Life Outcomes. 2006;4:56. doi: 10.1186/1477-7525-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Slade GD, Nuttall N, Sanders AE, Steele JG, Allen PF, Lahti S. Impacts of oral disorders in the United Kingdom and Australia. British Dental Journal. 2005;198(8):489–493. doi: 10.1038/sj.bdj.4812252. [DOI] [PubMed] [Google Scholar]
- 36.Soe KK, Gelbier S, Robinson PG. Reliability and validity of two oral health related quality of life measures in Myanmar adolescents. Community Dental Health. 2004;21(4):306–311. [PubMed] [Google Scholar]
- 37.Tsakos G, Allen PF, Steele JG, Locker D. Interpreting oral health-related quality of life data. Community Dentistry and Oral Epidemiology. 2012;40(3):193–200. doi: 10.1111/j.1600-0528.2011.00651.x. [DOI] [PubMed] [Google Scholar]
- 38.Batista MJ, Lawrence HP, de Sousa Mda L. Impact of tooth loss related to number and position on oral health quality of life among adults. Health and Quality of Life Outcomes. 2014;12:165. doi: 10.1186/s12955-014-0165-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lu HX, Xu W, Wong MC, Wei TY, Feng XP. Impact of periodontal conditions on the quality of life of pregnant women: A cross-sectional study. Health and Quality of Life Outcomes. 2015;13:67. doi: 10.1186/s12955-015-0267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Truong A, Higgs P, Cogger S, Jamieson L, Burns L, Dietze P. Oral health-related quality of life among an Australian sample of people who inject drugs. Journal of Public Health Dentistry. 2015;75(3):218–224. doi: 10.1111/jphd.12092. [DOI] [PubMed] [Google Scholar]
- 41.Talekar B, Rozier R, Zeldin L. Spanish version of the early childhood oral health impact scale. Journal of Dentistry Research. 2005;84:2653. [Google Scholar]
- 42.Burgette JM, Preisser JS, Rozier RG. Propensity score weighting: an application to an early head start dental study. Journal of Public Health Dentistry. 2016;76(1):17–29. doi: 10.1111/jphd.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith VA, Neelon B, Preisser JS, Maciejewski ML. A marginalized two-part model for longitudinal semicontinuous data. Statistical Methods in Medical Research. 2015 doi: 10.1177/0962280215592908. [DOI] [PubMed] [Google Scholar]
- 44.Smith VA, Preisser JS, Neelon B, Maciejewski ML. A marginalized two-part model for semicontinuous data. Statistics in Medicine. 2014;33(28):4891–4903. doi: 10.1002/sim.6263. [DOI] [PubMed] [Google Scholar]
- 45.Smith VA, Preisser JS. Direct and flexible marginal inference for semicontinuous data. Statistical Methods in Medical Research. 2015 doi: 10.1177/0962280215602290. [DOI] [PubMed] [Google Scholar]
- 46.Olsen MK, Schafer JL. A two-part random-effects model for semicontinuous longitudinal data. Journal of the American Statistical Association. 2001;96(454):730–745. [Google Scholar]
- 47.Goettems ML, Ardenghi TM, Romano AR, Demarco FF, Torriani DD. Influence of maternal dental anxiety on oral health-related quality of life of preschool children. Quality of Life Research. 2011;20(6):951–959. doi: 10.1007/s11136-010-9816-0. [DOI] [PubMed] [Google Scholar]
- 48.Arrow P. Responsiveness and sensitivity of the early childhood oral health impact scale to primary dental care for early childhood caries. Community Dentistry and Oral Epidemiology. 2016;44(1):1–10. doi: 10.1111/cdoe.12183. [DOI] [PubMed] [Google Scholar]
- 49.Arrow P, Klobas E. Child oral health-related quality of life and early childhood caries: A non-inferiority randomised control trial. Australian Dental Journal. 2016;61(2):227–235. doi: 10.1111/adj.12352. [DOI] [PubMed] [Google Scholar]
- 50.Campbell P, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, et al. Early childhood investments substantially boost adult health. Science. 2014;343(6178):1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]