Highlights
-
•
Paraganglioma is sometimes suspected as lymph node metastasis or lymph node recurrence of various malignant tumors.
-
•
Retroperitoneoscopic surgery is a valid approach to treat the tumor, located above the renal vein.
-
•
Resection using retroperitoneoscopic surgery without catecholamine-related complications is possible.
Keywords: Endometrial cancer, Laparoscopy, Paraganglioma, Retroperitoneal approach, Transperitoneal approach
1. Introduction
Paraganglioma is a rare, catecholamine-producing tumor that mostly arises from the paraaortic ganglion. In contrast, tumors that arise from the adrenal medulla are widely known as pheochromocytomas (Erickson et al., 2001). While some cases of paraganglioma are detected after manifestation of symptoms, including hypertension, hyperglycemia, and headache, others are discovered incidentally during preoperative imaging for other diseases; it is sometimes suspected as an alternative diagnosis for lymph node metastasis in gynecological malignancies (Chishima et al., 2010; Phillips et al., 1982). Currently, many types of endometrial cancer are treated by laparoscopic surgery (Walker et al., 2012). There are two different approaches to this surgery: a transperitoneal approach and a retroperitoneal approach, both are used for treating gynecologic malignancies (O'Hanlan et al., 2015). In the transperitoneal approach, it is necessary to place the organs such as the small intestine and omentum in the upper abdomen to allow for good exposure of the paraaortic area. The retroperitoneal approach, on the other hand, is advantageous since the retroperitoneal cavity can be reached without coming into contact with these organs. Besides gynecological malignancies, many adrenal tumors, including pheochromocytomas, are treated by a retroperitoneoscopic approach (Bittner et al., 2013). We report a case of endometrial cancer and high-level paraaortic paraganglioma that were resected using retroperitoneoscopic surgery without catecholamine-related complications.
2. Case presentation
A 45-year-old woman presented to our hospital owing to irregular genital bleeding; she had no other symptoms, including headache and hypertension. A tumor was mainly located in the uterine body with a polypoid tumor that was prolapsed from the uterine ostium. The patient was diagnosed with grade 1 endometrial adenocarcinoma by biopsy. Magnetic resonance imaging (MRI) revealed tumor invasion into more than half of the myometrial layer (Fig. 1A); however, cervical stromal invasion and uterine adnexa metastasis were not observed. Positron emission tomography-computed tomography (PET-CT) revealed abnormal accumulation of fluoro-deoxyglucose (FDG) in the upper part of the paraaortic lymph node region (Fig. 1B). Initially, abnormal accumulation of FDG was suspected to indicate lymph node metastasis of endometrial cancer. However, since it was at a position associated with the level of the pancreas around the paraaortic region, it was difficult to diagnose the patient with typical lymph node metastasis. The next step was to distinguish this presentation from that of a paraganglioma. Elevation of catecholamine levels was not observed upon endocrinological examination, but 123I-metaiodobenzylguanidine (123I-MIBG) scintigraphy revealed abnormal accumulation of 123I-MIBG, consistent with the site of abnormal FDG accumulation. Based on these observations, a paraaortic tumor was diagnosed, which was suspected to be a paraganglioma. The patient was administered preoperative administration of doxazosin (0.5 mg/day), α-receptor blocker, and sufficient replacement fluid (2000 mL/day). Resection of the tumors was performed using retroperitoneoscopic surgery with the patient in the supine position under general anesthesia and epidural anesthesia. The paraaortic lymph node located in between the renal vein and the abdominal aortic bifurcation, the high-level paraaortic tumor that was indicative of paraganglioma or lymph node metastasis, and the left pelvic lymph node were resected via this retroperitoneal approach (Fig. 2). The right pelvic lymph node, uterus, and uterine adnexa were resected via a transperitoneal approach. Using a retroperitoneoscopic surgical approach for removing the tumor, we performed composite resection of the high-level paraaortic tumor that coalesced with the retroperitoneum. As we excised the tumor and its adhering retroperitoneal tissue, we were able to observe the caudate lobe of the liver (Fig. 3). The operation time was 9 h 35 min, and the time taken to remove the paraganglioma was 59 min. The bleeding volume was 200 mL; therefore, a blood transfusion was not necessary. Surgery was performed without any complications, and the pathological tumor diagnosis was T1aN0M0 grade 2 endometrial adenocarcinoma (myometrial invasion was close to 50%) and paraganglioma. The patient was discharged from the hospital on postoperative day 9 and has been followed up without adjuvant therapy.
Fig. 1.
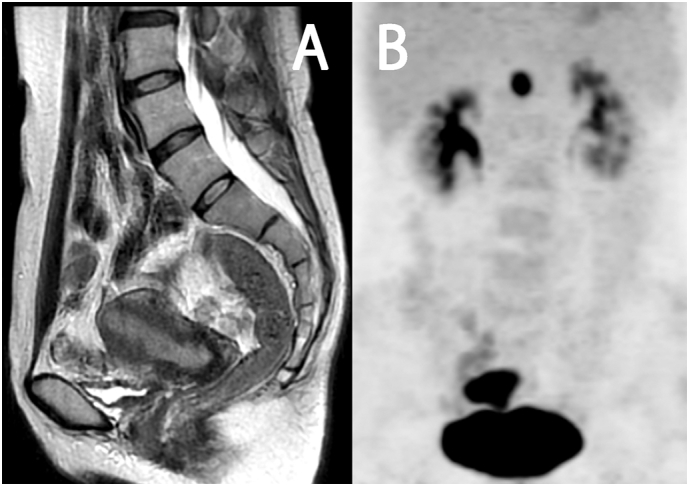
(A) T2-weighted pelvic magnetic resonance imaging (MRI) in the sagittal plane. The tumor invaded into the more than half of the myometrium and developed in polyps, although cervical stromal invasion was not observed. (B) Positron emission tomography-computed tomography (PET-CT) image, confirming fluoro-deoxyglucose (FDG) accumulation in the paraaortic region, in the upper level of left kidney.
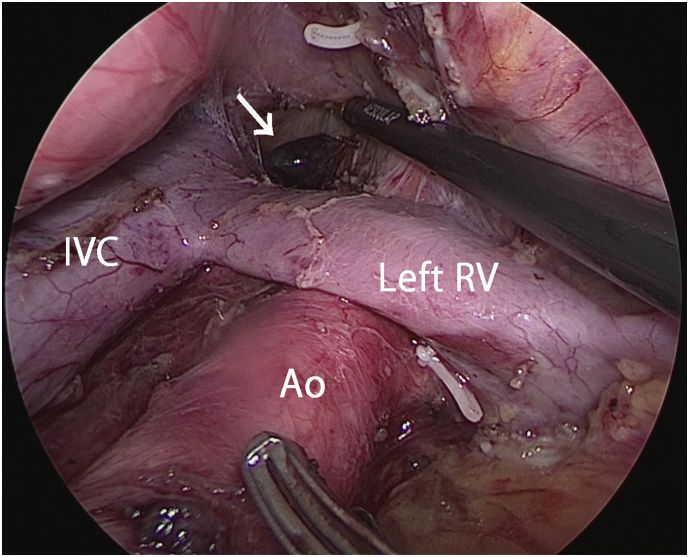
Fig. 2.
Paraaortic lymph node dissection via a retroperitoneal approach. The paraganglioma was on the cranial side of the left renal vein (arrow).
IVC, inferior vena cava; Ao, aorta; RV, renal vein.
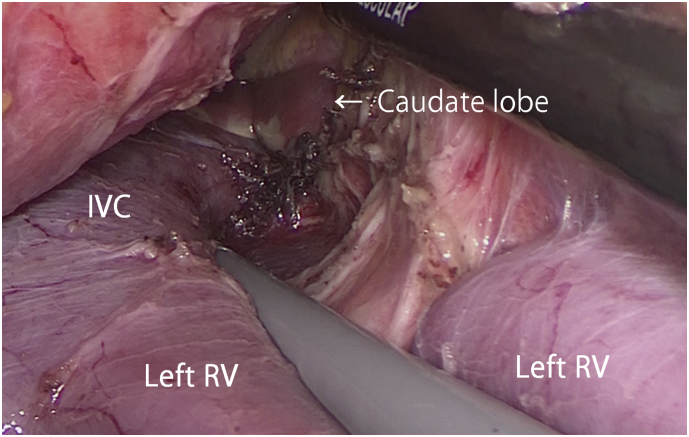
Fig. 3.
After removal of the paraganglioma, the caudate lobe of the liver was observed (arrow).
3. Discussion
In this case, we were able to safely resect both the endometrial cancer and the high-level paraaortic paraganglioma in a single operation, using a minimally invasive retroperitoneoscopic approach with only 59 additional minutes of operating time.
For paragangliomas, laparotomy is currently the recommended mode of treatment since they are more likely to be malignant than adrenal pheochromocytomas (Lenders et al., 2014). In recent years, there have been reports on the use of adapted laparoscopic surgery for paraganglioma owing to the developments in surgical techniques and laparoscopic instruments. Although laparoscopic surgery for paraganglioma extends the total operating time in comparison to laparotomy, bleeding is usually minimal and the duration of the postoperative hospital stay is generally short (Ping et al., 2016; Wang et al., 2014). Compared to laparoscopic surgery, retroperitoneoscopic surgery has the advantage of a short operation time, in addition to a short postoperative recovery period to regain intestinal motility (Xu et al., 2015).
In our hospital, advanced endometrial cancer patients undergo paraaortic lymph node dissection using retroperitoneoscopic surgery. This is on the basis of a report by Todo et al. who indicated that prognosis is improved by performing paraaortic lymph node dissection for advanced endometrial cancer (Todo et al., 2010). The advantages of using a retroperitoneal approach in paraaortic lymph node dissection are that the intestinal tract does not interfere with the surgical field, and that surgery can be performed without lowering the head.
In this case, lymph node enlargement was not observed using CT, but lymph node metastasis of endometrial cancer was suspected based on PET-CT. Since the renal vein is located near the upper end of the regional lymph nodes involved in endometrial cancer, we have no references reporting the frequency of lymph node metastasis occurring superior to the renal vein. On the other hand, it was also reported that the most common site of occurrence of extra-adrenal pheochromocytoma is the superior paraaortic region between the diaphragm and lower renal poles (Whalen et al., 1992). One study mentioned that out of 297 paragangliomas, 205 were in the head and neck region, and 92 were below the neck (Erickson et al., 2001). From this information, we considered a diagnosis other than lymph node metastasis and, paraganglioma was suggested as a differential diagnosis. Therefore, by performing endocrinological examination and 123I-MIBG scintigraphy, it was possible to strongly suspect paraganglioma before surgery. However, we could not completely deny the possibility of lymph node metastasis of endometrial cancer; therefore, it was essential that the paraaortic tumor was resected at the same time as the endometrial cancer. During the perioperative period, it was necessary to exercise caution even though a nonfunctional paraganglioma was suspected, because there was a possibility of inducing catecholamine elevation by surgical intervention. By providing preoperative treatment with an α-receptor blocker and sufficient replacement fluid, and by performing the tumor resection with the patient in the supine position (required for the retroperitoneoscopic surgery), we were able to avoid adverse events in this case.
The features identifying this case to be suitable for a single surgical procedure are as follows: Firstly, the tumor was on the cranial side of the retroperitoneal operative field for paraaortic lymphadenectomy in endometrial cancer, and the surgical field was easy to broaden. Secondly, it was easier to find the smaller tumor using the approach from the retroperitoneal caudal side to the cranial side. Thirdly, the tumor nutrition vessels, which mostly arose from the dorsal side of the tumor, were easy to shear. This case report has some limitations. Despite performing a minimally invasive surgery, the patient had a long hospital stay, which was partially due to regulations involving Japan's health-insurance system. The long duration was also due to performing a careful lymphadenectomy, during which 77 lymph nodes were resected with no operative complications.
This case suggests that using retroperitoneoscopic surgery can effectively treat intra-pelvic disease and disease of the upper segment of the kidney in a single operation. At the time of writing, the patient has not experienced a recurrence of either endometrial cancer or paraganglioma. Although careful follow-up will be required in this case, we believe that retroperitoneoscopic surgery for paraaortic tumors mimicking endometrial cancer metastasis is an effective minimally invasive treatment strategy.
Conflict of interest statement
The authors have no conflicts of interest to disclose.
Author contribution
Conception and design of study: K. Nakao, T. Hoshiba.
Acquisition of data: H. Banno, T. Kondo, H. Sasaki.
Analysis and/or interpretation of data: K. Nakao.
Drafting the manuscript: K. Nakao.
Review and editing the manuscript: K. Nakao, S. Hirabuki, T. Hoshiba.
Informed consent
The patient provided informed consent, and the research protocol was approved by the Ishikawa Prefectural Central Hospital Review Board (No. 1085).
References
- Bittner J.G., Gershuni V.M., Matthews B.D., Moley J.F., Brunt L.M. Risk factors affecting operative approach, conversion, and morbidity for adrenalectomy: a single-institution series of 402 patients. Surg. Endosc. 2013;27:2342–2350. doi: 10.1007/s00464-013-2789-7. [DOI] [PubMed] [Google Scholar]
- Chishima F., Tamura M., Nakazawa T., Sugitani M., Hirano D., Yoshikawa T., Fuchinoue F., Nemoto N., Yamamoto T. Paraaortic paraganglioma arising in an ovarian carcinoma patient mimicking lymph node metastasis. J. Obstet. Gynaecol. Res. 2010;36:204–208. doi: 10.1111/j.1447-0756.2009.01094.x. [DOI] [PubMed] [Google Scholar]
- Erickson D., Kudva Y.C., Ebersold M.J., Thompson G.B., Grant C.S., van Heerden J.A., Young W.F. Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J. Clin. Endocrinol. Metab. 2001;86:5210–5216. doi: 10.1210/jcem.86.11.8034. [DOI] [PubMed] [Google Scholar]
- Lenders J.W., Duh Q.Y., Eisenhofer G., Gimenez-Roqueplo A.P., Grebe S.K., Murad M.H., Naruse M., Pacak K., Young W.F. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2014;99:1915–1942. doi: 10.1210/jc.2014-1498. [DOI] [PubMed] [Google Scholar]
- O'Hanlan K.A., Sten M.S., O'Holleran M.S., Ford N.N., Struck D.M., McCutcheon S.P. Infrarenal lymphadenectomy for gynecological malignancies: two laparoscopic approaches. Gynecol. Oncol. 2015;139:330–337. doi: 10.1016/j.ygyno.2015.09.019. [DOI] [PubMed] [Google Scholar]
- Phillips J.G., Orr J.W., Grizzle W., Hatch K.D., Shingleton H.M. An extra-adrenal pheochromocytoma mimicking lymph node metastasis from a cervical cancer. Gynecol. Oncol. 1982;13:416–422. doi: 10.1016/0090-8258(82)90081-6. [DOI] [PubMed] [Google Scholar]
- Ping W., Hongzhou M., Jie Q., Taile J., Hao P., Dan X., Jun C., Shuo W. Laparoscopic resection of retroperitoneal paragangliomas: a comparison with conventional open surgical procedures. J. Endourol. 2016;30:69–74. doi: 10.1089/end.2015.0399. [DOI] [PubMed] [Google Scholar]
- Todo Y., Kato H., Kaneuchi M., Watari H., Takeda M., Sakuragi N. Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL study): a retrospective cohort analysis. Lancet. 2010;375:1165–1172. doi: 10.1016/S0140-6736(09)62002-X. [DOI] [PubMed] [Google Scholar]
- Walker J.L., Piedmonte M.R., Spirtos N.M., Eisenkop S.M., Schlaerth J.B., Mannel R.S., Barakat R., Pearl M.L., Sharma S.K. Recurrence and survival after random assignment to laparoscopy versus laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group LAP2 Study. J. Clin. Oncol. 2012;30:695–700. doi: 10.1200/JCO.2011.38.8645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Li Y., Xiao N., Duan J., Yang N., Bao J., Mi J. Retroperitoneoscopic resection of primary paraganglioma: single-center clinical experience and literature review. J. Endourol. 2014;28:1345–1351. doi: 10.1089/end.2014.0345. [DOI] [PubMed] [Google Scholar]
- Whalen R.K., Althausen A.F., Daniels G.H. Extra-adrenal pheochromocytoma. J. Urol. 1992;147:1–10. doi: 10.1016/s0022-5347(17)37119-7. [DOI] [PubMed] [Google Scholar]
- Xu W., Li H., Ji Z., Yan W., Zhang Y., Xiao H., Zhang X., Liu G. Comparison of retroperitoneoscopic versus transperitoneoscopic resection of retroperitoneal paraganglioma: a control study of 74 cases at a single institution. Medicine (Baltimore) 2015;94 doi: 10.1097/MD.0000000000000538. [DOI] [PMC free article] [PubMed] [Google Scholar]