Abstract
Previous research has produced inconsistent results on whether education and ethnic disparities in body mass index (BMI) persist, widen, or diminish over time. The authors investigate how education and ethnicity, independently and conditionally, influence BMI trajectories during the transition to older adulthood. Employing random coefficient modeling, the authors analyzed eight biennial waves of data (1992–2006) from the Health and Retirement Study, a nationally representative longitudinal study of individuals born between 1931 and 1941. After adjusting for health behaviors and health status, education and ethnic disparities in BMI persisted for most groups, but narrowed between high-educated White men and both low-educated Hispanic men and high-educated Black men. As such, the findings generally support the persistent inequality interpretation. Therefore, even though interventions targeted at earlier points in the life course may be effective in reducing BMI disparities in later life, social and health policies directed at reducing obesity among older adults is also warranted.
Keywords: life course, cumulative, inequality, longitudinal analysis, race, education
Introduction
Obese persons are at increased risk of cardiovascular disease, hypertension, stroke, diabetes, disability, and premature mortality (Alley and Chang 2007; Ferraro, Thorpe, and Wilkinson 2003; Thorpe and Ferraro 2004; Wannamethee, Shaper, and Walker 2005); as such, obesity has become a major public health concern. The negative health consequences of obesity may be particularly pronounced among older adults. Prior research suggests that the transition to older adulthood is the period in the life course associated with the greatest risk of severe incident obesity (Ferraro et al. 2003), obese individuals are at significantly higher risk of becoming disabled across older ages (Reynolds, Saito, and Crimmins 2005), and obesity during older adulthood accelerates the onset of serious illnesses that place obese older adults at greater risk of early death (Thorpe and Ferraro 2004). Although obesity in mid- to late life is likely to have significant health consequences, we know little about how social factors shape changes in body mass index (BMI) during the transition to older adulthood.
Prior studies find that gender, ethnicity, and education affect the rate at which BMI changes over the adult life course (Baltrus et al. 2005; Burke et al. 1996; Clarke et al. 2009; D. S. Freedman et al. 2005; Gordon-Larsen et al. 2004; McTigue, Garrett, and Popkin 2002; Mujahid et al. 2005). Most studies of BMI change in adulthood have focused on younger adults and we have only limited and conflicting information about how these social factors affect BMI change among older adults. For example, Burke et al. (1996) found that among young adults, Black women were heavier at baseline and gained more weight than White women. Likewise, Clarke et al. (2009) reported that among individuals transitioning to midlife, BMI increased at a faster rate among the less educated, Blacks, and Hispanics. By contrast, Sheehan et al. (2003) found that among a national sample of adults aged 25 to 74 at baseline, Black women experienced a slower rate of increase in BMI than White women, but Black men experienced a faster rate of increase in BMI than White men. Among middle-aged women, Lewis et al. (2005) found that neither race nor education was associated with BMI change over time, whereas Mujahid et al. (2005) found that education was positively associated with increases in BMI over time among Black women transitioning to older adulthood. A few studies have also documented differences in the association between education and BMI by ethnicity and gender both cross-sectionally (Chang and Lauderdale 2005; Zhang and Wang 2005) and longitudinally (Burke et al. 1996; Mujahid et al. 2005). These prior findings indicate that ethnicity and education play an important role in how BMI changes across the life course.
Existing knowledge about how BMI disparities change or persist during the transition to older adulthood is hampered by the reliance on cross-sectional studies that confound period, cohort, and age effects or by the use of longitudinal studies that utilize only two data points (He and Baker 2004; Kahn and Williamson 1991) and hence cannot disentangle random fluctuations from true change (Singer and Willet 2003). The majority of studies that do exploit the longitudinal nature of their data (i.e., assess intraindividual change) often assess change in BMI during early adulthood and middle age (Clarke et al. 2009; Kimm et al. 2005; McTigue, Garrett, and Popkin 2002; Mosuwan, Tongkumchum, and Puetpaiboon 2000; Rzehak and Heinrich 2006; Wardle et al. 2006) but not during the transition to older adulthood. Moreover, the studies that have examined BMI change during the transition to older adulthood rely on community samples that may not be generalizable to the U.S. population (Baltrus et al. 2005; Guo et al. 1999; Lewis et al. 2005; Mujahid et al. 2005; Wolinksy et al. 2009). We therefore know little about how BMI changes as individuals enter older adulthood, a period of the life course in which individuals experience major life events, such as retirement and widowhood, as well as declines in health.
We seek to address these gaps in the literature by investigating whether ethnic and educational inequalities in BMI widen, diminish, or persist using a nationally representative sample of the U.S. population making the transition to older adulthood. We also examine if the relationship between education and BMI differs by ethnicity and gender.
Background
Overall, studies investigating the education-health gradient have often been based on the assumption that the influence of education on health is static; that is, disparities between highly educated individuals and less educated individuals are maintained over the life course. Recently, however, this assumption has been called into question. Both cross-sectional (Miech and Shanahan 2000; Ross and Wu 1996) and longitudinal studies (Clarke et al. 2009; House et al. 1994; Lynch 2003, 2006; Walsemann, Gee, and Geronimus 2009; Walsemann, Geronimus, and Gee 2008; Willson, Shuey, and Elder 2007) have documented widening health disparities by levels of education, at least through middle age. Often referred to as cumulative advantage/disadvantage (or CAD), Dannefer (2003) has described this phenomenon as the “systematic tendency for inter-individual divergence in a given characteristic (e.g., money, health, or status) with the passage of time” (p. 327). As it relates to health, CAD contends that early life disadvantage leads to the accumulation of additional disadvantages that place individuals at greater risk for the earlier onset of illness, thus leading to widening health disparities as individuals age (Dannefer 2003; O’Rand 1996). Related to CAD is the theory of cumulative inequality proposed by Ferraro and Shippee (2009), which argues that the accumulation of disadvantage and its resulting effects are not merely the inverse of cumulative advantage. Rather, the theory of cumulative inequality contends that advantage established in early life, such as being White or growing up in a wealthy family, results in the greater accumulation of opportunities and resources that put already advantaged individuals in a better position to delay the onset of illness. In comparison, disadvantage established in early life, such as being an ethnic minority or growing up in a poor family, is more likely to result in the greater accumulation of disadvantages over the life course that accelerate the aging process and disease onset (Ferraro and Shippee 2009).
Although there has been a clear increase in the number of studies investigating the ways in which health disparities widen, diminish, or persist across the life course as a function of ethnicity or education, few of these studies have focused on BMI. Of those that have, the results have been mixed. For example, in a longitudinal study by Clarke et al. (2009), Blacks, Hispanics, and high school graduates experienced greater increases in BMI from late adolescence to middle age compared to Whites and college graduates. As a result, the largest BMI disparities by ethnicity and education occurred at midlife. Similarly, Kahn and Williamson (1991) reported greater increases in BMI over a 10-year period among Black women as compared to White women and lower educated women as compared to highly educated women. No such effects were found among men. In comparison, Lewis et al. (2005) found no change in BMI disparities by race (i.e., Black vs. White) or education among a community-based sample of middle-aged women living in the United States.
In older adulthood, however, the cumulative effects of ethnicity and education on BMI may actually manifest as persistent or diminishing BMI disparities as the most disadvantaged groups experience earlier onset of disease and premature mortality (Ferraro and Shippee 2009; Lynch 2003). Unintentional weight loss often accompanies declines in health (Wallace and Schwartz 2002); thus, disadvantaged groups who earlier in the life course may have been at greater risk of obesity compared to advantaged groups could actually see a narrowing of the BMI gap as they enter older adulthood. In addition, as disadvantaged groups are selected out of the population through premature mortality, the remaining members of the population are typically healthier and more homogeneous. Indeed, some researchers contend that selective mortality is one of the main mechanisms explaining diminishing health disparities as individuals enter old age (Dupre 2007, 2008; Ferraro and Shippee 2009; Willson et al. 2007). Thus, although CAD would predict widening disparities in a given health condition with age, cumulative inequality theory would contend that persistent or diminishing BMI disparities by ethnicity or education may actually reflect processes of cumulative inequality that create compositional changes in the population (Ferraro and Shippee 2009).
Declines in health may therefore play an important role in processes of cumulative inequality in BMI. Among younger aged samples, longitudinal studies typically do not adjust for health conditions that may be related to precipitous declines in health, such as cancer, stroke, or cardiovascular events (cf. Baltrus et al. 2005; Burke et al. 1999; Clarke et al. 2009; Gordon-Larsen et al. 2004; James et al. 2006; Kahn and Williamson 1991; McTigue et al. 2002), which are less likely to occur earlier in the life course. Similarly, longitudinal studies using middle-aged and older aged samples do not always fully adjust for these health conditions (cf. He and Baker 2004; Mujahid et al. 2005; Sheehan et al. 2003), even though processes of cumulative health inequality between advantaged and disadvantaged groups manifest as early as the mid-30s (Geronimus et al. 2001). Moreover, longitudinal studies that use only two observational points confound issues of mortality with compositional changes in the cohort or population (He and Baker 2004; Wolinsky et al. 2009). Thus, appropriate controls for health conditions and mortality selection are necessary in longitudinal studies of BMI change in older adults.
The theory of cumulative inequality also contends that inequality develops across multiple systems of stratification (Ferraro and Shippee 2009). However, most studies examining BMI disparities tend to treat education, ethnicity, and gender as independent social characteristics that contribute additively to these disparities. Yet, individuals sit at the nexus of multiple sources of inequality (Weber 2010), and it is the combination of these different sources of inequality that can lead to differential distribution of health risks in the population (Krieger et al. 1993; Williams and Collins 1995). By considering only the independent effects of these social characteristics, traditional approaches to studying disparities in BMI trajectories risk misestimating or misunderstanding the effects of ethnicity, education, and gender. For example, examining ethnic differences in BMI and BMI change without considering the additional component of gender variation would result in the mistaken conclusion that Blacks, in general, gain weight faster than Whites, when in fact this effect exists primarily among women (Baltrus et al. 2005; Burke et al. 1996; D. S. Freedman et al. 2005; Gordon-Larsen et al. 2004; Kahn and Williamson 1991; McTigue et al. 2002). Processes of cumulative inequality are therefore relevant for understanding BMI trajectories because the experience of multiple systems of inequality can establish these trajectories early in life, but may change over the adult life course as a function of how individuals experience their social inequality. In fact, some prior studies of BMI trajectories among older adults suggest interactions between some combination of gender, race, and education (He and Baker 2004; Mujahid et al. 2005), but the findings are somewhat inconsistent across studies.
The purpose of this study is to examine how BMI changes during the transition to older adulthood as a function of gender, ethnicity, and education. We contend that it is the combination of these social characteristics, in conjunction with age, that determines both exposure and vulnerability to factors thought to influence BMI. We examine two hypotheses. First, we hypothesize that ethnic and education disparities in BMI will persist or diminish as individuals enter older adulthood, given a higher prevalence of declining health among disadvantaged groups coupled with the expected compositional changes in our sample due to premature mortality among disadvantaged groups. Second, we hypothesize that education disparities in BMI will differ by ethnicity. We do not speculate as to the direction of the difference, as much of the research investigating ethnic differences in the relationship between education and BMI finds conflicting evidence as to the direction of the effect.
Our study builds upon prior work by (1) utilizing multiple waves of data from a longitudinal study spanning 14 years, (2) following a national sample of U.S. adults making the transition to older adulthood, and (3) accounting for differences in health behaviors and health status that may be associated with changes in BMI during the transition to older adulthood.
Method
Sample
We analyzed data from the Health and Retirement Study (HRS), a nationally representative longitudinal study of individuals born between 1931 and 1941. We utilized data from eight biennial waves of the HRS (1992–2006; RAND HRS Data 2008). We limited our analyses to respondents who self-reported as non–Hispanic White, non–Hispanic Black, or Hispanic (any race) and who reported information on their weight and height at least once. After exclusions, our sample consisted of 9,825 respondents (7,166 non–Hispanic Whites, 1,722 non–Hispanic Blacks, and 937 Hispanics). Most respondents (70.6%) provided at least seven waves of data, with approximately 60% providing data in all eight waves. Only 1% of the sample was excluded due to item nonresponse.
Over the course of the study 17% of respondents died. Males, Black females, the U.S.-born, the less educated, current smokers, respondents in poor/fair health, and those with more than one health condition experienced higher rates of mortality than White females, immigrants, the highly educated, nonsmokers, respondents in good/very good/excellent health, and those without a health condition. Baseline BMI was unrelated to mortality.
Analyses are unweighted because longitudinal weights were unavailable (Health and Retirement Study 2009); however, unweighted analyses produce unbiased coefficients if one includes the variables used to sample respondents (Winship and Radbill 1994).
Measures
Dependent variable
Respondents self-reported their height and weight in each survey year. We used this information to calculate body mass index as [(weight (kg)) / (height (m2))].
Ethnicity and education
To examine if the influence of education on BMI trajectories varies by ethnicity, we created six ethnicity/education dummy variables: White, ≥ 12 years of schooling (referent group); White, < 12 years of schooling; Black, ≥ 12 years of schooling; Black, < 12 years of schooling; Hispanic, ≥ 12 years of schooling; and Hispanic, < 12 years of schooling. More refined specifications of education—a four-category education variable (< 12 years, 12 years, 13–15 years, and 16 or more years) and a three-category education variable (< 12 years, 12 years, > 12 years)—yielded similar results. We used the two category specification of education for parsimony and because the distinction between having a high school education or greater versus having less than high school education is a meaningful comparison for older adults who entered the workforce at a time when most jobs were in manufacturing and a high school education was sufficient for securing middle-class jobs (Levy and Murnane 1992).
Covariates
Demographic, social, and economic characteristics include birth cohort (0 = 1931 to 1936 and 1 = 1937 to 1941), immigrant status (foreign-born vs. U.S.-born), and time-varying measures of retirement status (1 = retired, 0 = other), marital status (married, divorced/separated, widowed, other), and total household wealth (excluding IRAs) categorized as below the 25th percentile (< $43,920), between the 25th to 75th percentile ($43,920 to $329,131), and over the 75th percentile (> $329,131). Total household wealth reflects the amount of total assets net of all debt. Missing values on individual items used to create the total household wealth measure were imputed using an imputation algorithm described in detail elsewhere (St. Clair et al. 2008). We adjusted total household wealth at each measurement occasion to 2006 dollars to account for inflation. Indicators of attrition include a measure of the number of waves of data collection each respondent missed (zero to seven waves) and mortality (1 = died after 1992, 0 = alive as of 2006).
Because health behaviors and certain health conditions can result in either weight gain or weight loss, and because these behaviors and conditions are more likely to occur among disadvantaged groups, we included the following time-varying measures of health status and behaviors: self-reported health (poor/fair vs. good/very good/excellent), number of self-reported doctor diagnosed conditions (high blood pressure, diabetes, cancer, lung disease, heart disease, stroke, and arthritis), smoking status (current smoker vs. other), and drinking behavior (ever drinks vs. never drinks). The measures were assessed in each survey year and represent current health behaviors or conditions at the time of each survey. All covariates were interacted with age, our measure of time, to adjust for each covariate’s influence on the rate of BMI change.
Analytic Approach
To assess how multiple sources of inequality contribute to differences in BMI trajectories, we examined the effect of ethnicity and education on BMI trajectories in gender-stratified analyses. Our analyses proceeded as follows. First, we examined the distribution of sociodemographic and health characteristics of the sample and present the results for each ethnicity and gender group. Next, we estimated two-level random coefficient models to investigate the extent to which ethnicity and education are associated with BMI over time. In our models, age in each survey year represents time. To facilitate interpretation of the model’s intercept, we centered age at 62, the median age of our sample, and modeled age as [(age − 62) / 10]. Thus, a one-unit increase in the age coefficient represents change in BMI over a decade. We tested for nonlinearity of BMI change by including a quadratic age variable in our models, but this term was not significant.
Model 1 examined the association between our primary predictor variables (i.e., ethnicity/education, age, and ethnicity/education by age interaction terms) and our dependent variable, after adjusting for birth cohort and immigrant status. Model 2 included additional adjustment for time-varying measures of retirement status, wealth, and marital status to test if economic and social resources mediate the association between ethnicity/education and BMI trajectories. Given prior research that suggests that selective mortality can bias studies attempting to examine processes of cumulative inequalities in health (Dupre 2007, 2008; Ferraro and Shippee 2009; Ferraro, Shippee, and Schafer 2009), as well as research that finds certain health behaviors and health conditions contribute to weight gain or loss, our final model adjusted for time-varying measures of current smoking and drinking status, self-rated health, health conditions, as well as mortality and unit nonresponse to determine if the combined effects of ethnicity and education on BMI at age 62 and over time were attenuated once other correlated measures of health behaviors, health conditions, and attrition were included (model 3).
To examine how ethnicity and education are associated with BMI and changes in BMI over time, we included interactions between age and each of the ethnicity/education dummy variables. Nonsignificant differences in the interactions between age and ethnicity/education indicate persistent disparities in BMI; positive coefficients indicate widening disparities in BMI; and negative coefficients indicate diminishing disparities in BMI. We also determined if the effect of education on BMI and BMI change differed by ethnicity by examining the association of education with baseline BMI and BMI change within ethnic groups.
We employed the following random coefficients model:
| (1) |
where Yit is BMI for respondent i at time t and assumes that conditional on ζ0i and ζ1i, Yi1, to Ynt are independent; t = 1, …, Ti is the number of occasions on which respondent i was observed, and i = 1, …, n; Xi′ is a vector of time-invariant covariates (e.g., ethnicity/education); Z′it is a vector of time-varying covariates (e.g., age, age × ethnicity/education); ζ0i and ζ1i are random effects that represent unobserved heterogeneity for respondent i, and are assumed to be normally distributed with mean 0; and εit is the random within-person error of prediction for respondent i at time t. We also assume that the random effects ζ0i and ζ1i are independent of εit and that all random components are independent of the vector of covariates (Singer and Willet 2003). Random coefficient models were specified using xtmixed in Stata v10 (Stata Corp. 2007).
Results
We present sample characteristics by ethnic/gender groups in Table 1. Black and Hispanic women reported significantly higher mean BMI scores compared to White women. We found no ethnic differences among men. Regardless of gender, Blacks and Hispanics completed less education, had less total household wealth, were more likely to report fair/poor health, and were less likely to drink alcohol compared to Whites. Black and Hispanic women and Black men reported a higher mean number of health conditions and were less likely to be married compared to their White counterparts, whereas Hispanic men reported a lower mean number of health conditions compared to White men. Hispanic women were less likely to smoke than White females, and Black males were more likely to smoke than White males. Hispanics were more likely to be foreign-born than Whites. Regardless of ethnicity, men generally had more total household wealth than women. Additional details about the sample can be found in Table 1.
Table 1.
Sample Characteristics by Gender and Ethnicity, Health and Retirement Study (N = 9,825)a
| Females | Males | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| White (n = 3,751) | Black (n = 1,010) | Hispanic (n = 518) | White (n = 3,415) | Black (n = 712) | Hispanic (n = 419) | |
| Mean body mass index (BMI)b | 26.9 | 30.3‡ | 28.5‡ | 27.7† | 27.7† | 28.0 |
| Education | ||||||
| < 12 years | 23.3 | 45.7‡ | 68.0‡ | 23.8 | 47.5‡ | 63.7‡ |
| ≥12 years | 76.7 | 54.3‡ | 32.0‡ | 76.2 | 52.5‡ | 36.3‡ |
| Age (in years) | 61.9 | 61.6‡ | 61.5‡ | 61.8 | 61.5 | 61.4 |
| Marital statusb | ||||||
| Married | 67.3 | 37.9‡ | 57.5‡ | 81.4† | 62.3†‡ | 77.5† |
| Divorced/ Separated | 12.6 | 26.4‡ | 19.2‡ | 9.2† | 17.9†‡ | 12.1† |
| Widowed | 15.4 | 26.7‡ | 16.3 | 3.3† | 7.4†‡ | 4.2† |
| Other | 4.7 | 9.0‡ | 7.0‡ | 6.1† | 12.4†‡ | 6.2 |
| Retiredb | 44.2 | 45.0 | 28.2‡ | 48.5† | 48.1 | 40.5†‡ |
| Total household wealthb | ||||||
| < $43,920 | 19.1 | 50.7‡ | 50.6‡ | 14.8† | 43.6†‡ | 43.8†‡ |
| $43,920 to $329,131 | 51.2 | 44.4‡ | 41.9‡ | 52.0 | 48.5†‡ | 48.9† |
| > $329,131 | 29.7 | 4.9‡ | 7.4‡ | 33.2† | 7.9†‡ | 7.3‡ |
| Self-rated healthb | ||||||
| Fair/poor | 19.9 | 38.1‡ | 52.8‡ | 19.1 | 36.5‡ | 38.1†‡ |
| Excellent/very good/good | 80.1 | 61.9‡ | 47.2‡ | 80.9 | 63.5‡ | 61.9†‡ |
| Mean number of health conditionsb | 1.42 | 1.81‡ | 1.55‡ | 1.38 | 1.54†‡ | 1.22†‡ |
| Smoking statusb | ||||||
| Current smoker | 19.6 | 17.5 | 14.4‡ | 20.1 | 28.3†‡ | 21.2† |
| Nonsmoker | 80.4 | 82.5 | 85.6‡ | 79.9 | 71.7†‡ | 78.8† |
| Drinking behaviorb | ||||||
| Ever drinks | 50.3 | 31.0‡ | 26.7‡ | 63.6† | 54.3†‡ | 57.4†‡ |
| Never drinks | 49.7 | 69.0‡ | 73.3‡ | 36.4† | 45.7†‡ | 42.6†‡ |
| Birth cohort | ||||||
| 1931–1936 | 51.5 | 52.7 | 45.2‡ | 52.6 | 52.7 | 46.3‡ |
| 1937–1941 | 48.5 | 47.3 | 54.8‡ | 47.4 | 47.3 | 53.7‡ |
| Immigrant | 4.6 | 5.0 | 54.8‡ | 3.9 | 5.5 | 52.5† |
| Died | 12.3 | 20.8‡ | 12.5 | 18.8 | 29.8‡ | 20.0 |
| Mean number of missing waves | 1.09 | 1.17 | 1.56‡ | 1.49† | 1.84†‡ | 2.15†‡ |
All indicators dummy coded and estimates can be interpreted as percentages, unless otherwise noted.
Time-varying indicators. Indicators are measured at every survey wave, but estimates presented in Table 1 are averaged across survey interval for ease of presentation.
Significant (at p < .05) sex differences within ethnicity (reference = female), two-tailed test.
Significant (at p < .05) ethnic differences within sex (reference = White), two-tailed test.
Random Coefficient Models
We first examined how ethnicity and education were associated with BMI at age 62 and over time among women (Table 2, column 1), net of birth cohort and immigrant status. Whites with 12 years or more of schooling served as the referent group. At age 62, all ethnicity/education groups reported higher BMIs than White women with 12 or more years of schooling. Black and Hispanic women, regardless of education, reported higher BMIs than White women. Lower educated women (< 12 years of schooling) experienced higher BMIs than women with 12 or more years of schooling, regardless of ethnicity. These findings suggest that among women in our sample, the association between education and BMI at age 62 was equivalent across ethnicity. Over time, Black women, regardless of education, experienced a slower rate of change in BMI than White women with 12 or more years of schooling, as did Hispanic women with less than 12 years of schooling (b = −0.53). We also found cohort differences in BMI among our sample; women in the younger cohort (1937–1941) had higher BMIs at age 62 (b = 0.70) and experienced more rapid increases in BMI over a 10-year period (b = 0.61) than women in the older cohort (1931–1936).
Table 2.
Estimates From Random Coefficient Models for Body Mass Index (BMI) Stratified by Gender, Health and Retirement Study (HRS; 1992–2006)a
| Females (n = 5,279) | Males (n = 4,546) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |||||||
|
|
|
|
|
|
|
|||||||
| b | SE | b | SE | b | SE | b | SE | b | SE | b | SE | |
| At age 62 | ||||||||||||
| Intercept | 26.42 | 0.13*** | 26.41 | 0.13*** | 26.68 | 0.14*** | 27.44 | 0.11*** | 27.43 | 0.11*** | 27.52 | 0.12*** |
| White, ≥ 12 yearsb | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| White, < 12 years | 1.02 | 0.21*** | 1.02 | 0.21*** | 1.13 | 0.21*** | 0.20 | 0.17 | 0.22 | 0.17 | 0.34 | 0.17* |
| Black, ≥ 12 years | 3.01 | 0.26*** | 3.07 | 0.26*** | 3.04 | 0.25*** | 0.03 | 0.24 | 0.11 | 0.24 | 0.20 | 0.24 |
| Black, < 12 years | 4.10 | 0.26*** | 4.18 | 0.28*** | 4.17 | 0.28*** | −0.32 | 0.25 | −0.21 | 0.25 | −0.06 | 0.25 |
| Hispanic, ≥ 12 years | 1.31 | 0.46** | 1.33 | 0.46*** | 1.41 | 0.45** | 0.10 | 0.38 | 0.15 | 0.38 | 0.15 | 0.37 |
| Hispanic, < 12 years | 2.54 | 0.35*** | 2.57 | 0.35*** | 2.61 | 0.35*** | 0.75 | 0.31* | 0.81 | 0.31** | 0.91 | 0.31** |
| Birth cohort 1937–1941c | 0.70 | 0.15*** | 0.70 | 0.15*** | 0.61 | 0.15*** | 0.66 | 0.13*** | 0.67 | 0.13*** | 0.59 | 0.13*** |
| Rate of change | ||||||||||||
| Age 62d | 0.60 | 0.07*** | 0.60 | 0.07*** | 0.53 | 0.08*** | 0.41 | 0.06*** | 0.43 | 0.07*** | 0.48 | 0.05*** |
| (White, ≥ 12 Years) × Age | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| (White, < 12 Years) × Age | −0.17 | 0.12 | −0.09 | 0.12 | 0.01 | 0.12 | −0.06 | 0.11 | −0.05 | 0.11 | 0.04 | 0.11 |
| (Black, ≥ 12 Years) × Age | −0.33 | 0.14* | −0.27 | 0.14 | −0.24 | 0.14 | −0.41 | 0.15** | −0.40 | 0.15** | −0.34 | 0.15* |
| (Black, < 12 Years) × Age | −0.37 | 0.16* | −0.24 | 0.16 | −0.11 | 0.16 | −0.32 | 0.16* | −0.32 | 0.16* | −0.20 | 0.16 |
| (Hispanic, ≥ 12 Years) × Age | −0.26 | 0.25 | −0.22 | 0.25 | −0.12 | 0.25 | 0.10 | 0.22 | 0.08 | 0.22 | 0.11 | 0.22 |
| (Hispanic, < 12 Years) × Age | −0.53 | 0.20** | −0.41 | 0.20* | −0.27 | 0.20 | −0.58 | 0.19** | −0.58 | 0.19** | −0.45 | 0.19* |
| Birth Cohort 1937–1941 × Age | 0.61 | 0.08*** | 0.57 | 0.09*** | 0.56 | 0.09 | 0.41 | 0.08*** | 0.32 | 0.08*** | 0.26 | 0.08** |
| Log likelihood | −77,933.8 | −77,906.4 | −77,725.4 | −54,622.8 | −54,575.1 | −54,402.7 | ||||||
| SD (u0i) | 5.41 | 5.41 | 5.32 | 4.20 | 4.19 | 4.14 | ||||||
| SD (u1i) | 2.26 | 2.25 | 2.20 | 1.92 | 1.91 | 1.86 | ||||||
| Person-period observations | 32,682 | 25,397 | ||||||||||
| Mean number of observations | 6.2 (minimum = 1, maximum = 8) | 5.6 (minimum = 1, maximum = 8) | ||||||||||
Model 1 also adjusted for immigrant status. Model 2 also adjusted for time-varying measures of current retirement status, current marital status, and current total household wealth. Model 3 also adjusted for time-varying measures of current smoking, current drinking, current self-rated health, and current number of health conditions, as well as unit nonresponse and mortality. All covariates, except for immigrant status, mortality, and unit nonresponse, were centered at their grand means. All covariates were interacted with age.
≥ 12 years and < 12 years refers to years of schooling completed.
Reference group: 1931–1936 cohort.
Age is modeled as [(age − 62) / 10] for main effects and interactions.
p ≤ 0.05,
p ≤ 0.01,
p ≤ 0.001.
Next, given that processes of cumulative inequality are hypothesized to affect health through the accumulation of social and economic resources, we further adjusted for time-varying indicators of retirement status, total household wealth, and marital status, which were each interacted with age (Table 2, column 2). Although the inclusion of these indicators did little to alter the relationship between ethnicity and education on BMI at age 62, it did attenuate the effect of ethnicity and education on BMI change among Black women at each educational level. Hispanic women with less than 12 years of schooling continued to experience a slower rate of BMI change (b = −0.41, p < .05) compared to White women with 12 years or more of schooling.
Our final model (model 3) included additional adjustment for time-varying measures of smoking, drinking, self-rated health, number of health conditions, as well as unit nonresponse and mortality. Inclusion of these covariates did little to explain the higher BMIs of Black and Hispanic women at age 62 as compared to White women. The overall rate of change was attenuated from model 2 (b = 0.60) to model 3 (b = 0.53), as was the rate of change for Hispanic women with less than 12 years of schooling (b = −0.41, model 2; b = −0.27, p > .05, model 3).
We followed the same model building approach for men as we did for women. Net of immigrant status and birth cohort, the only statistically significant difference in BMI at age 62 was among Hispanic men with less than 12 years of schooling. This group experienced higher BMIs (b = 0.75) as compared to White men with 12 years or more of schooling (model 1, column 4). These findings suggest that neither ethnicity nor education were strongly related to BMI at age 62 among White or Black men. However, education was associated with BMI change among Hispanic men. Like women, men experienced an increase in BMI over a 10-year period (b = 0.41), whereas Black men, regardless of education, experienced a slower rate of change in BMI compared to White men with 12 years or more of schooling, as did Hispanic men with less than 12 years of schooling (b = −0.53). We also found a significant cohort effect; men in the younger cohort reported higher BMIs at age 62 and a more rapid increase in their BMIs over a 10-year period compared to men in the older cohort.
Estimates from model 2 yielded comparable results to those found in model 1, even after additional adjustment for time-varying indicators of retirement status, total household wealth, and current marital status. After further adjustment for time-varying measures of smoking, drinking, self-rated health, number of health conditions, as well as unit nonresponse and mortality (model 3), the findings were generally equivalent, except that White men with less than 12 years of schooling experienced higher BMI at age 62 (b = 0.34) than White men with 12 or more years of schooling, whereas BMI change among Black men with less than 12 years of schooling was no longer significantly different from White men with 12 or more years of schooling. The results also revealed that education was more strongly associated with BMI change among Hispanic men as compared to White men.
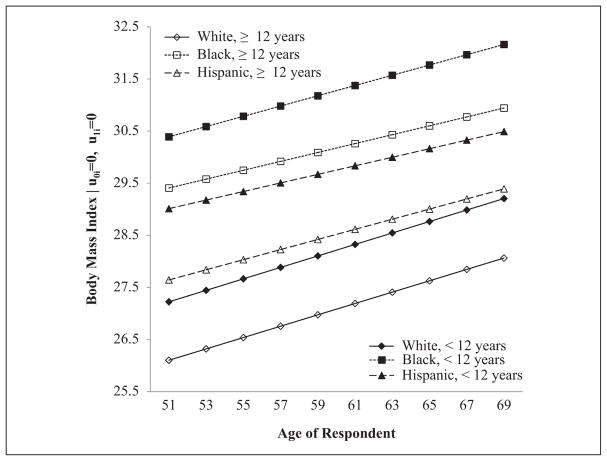
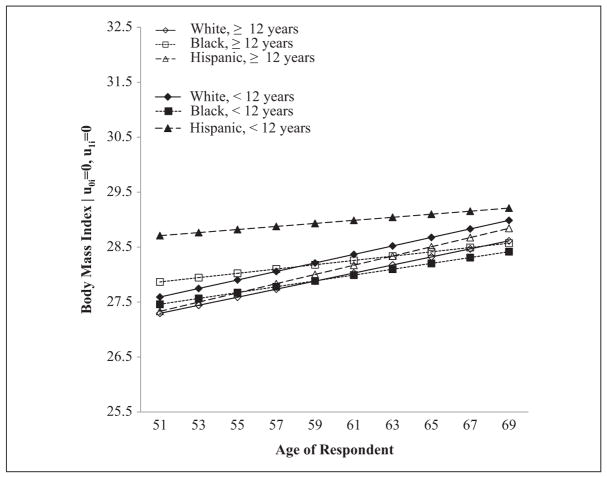
Average BMI trajectories for the youngest cohort of women (Figure 1) and men (Figure 2) are presented by ethnicity/education groups. Disparities by education/ethnicity appear most prominent for women and reflect persistent BMI disparities during the study period. The trajectories also document the strikingly higher levels of BMI found among the most educated Black women compared to the least educated White women. Among men, disparities between education/ethnic groups were narrower than those found among women. The trajectories also show that the gap between Hispanics with less than 12 years of schooling and Whites with 12 or more years of schooling narrowed over the study period, from 1.41 BMI units (i.e., 9.6 lbs/4.4 kg for an average height man; based on unit conversions from Williamson 1993) at age 51 to 0.60 BMI units (i.e., 4.1 lbs/1.9 kg for an average height man) at age 69 (p > .05 at age 69). The gap between Black men with 12 or more years of schooling and their White counterparts also narrowed over the study period, from 0.57 BMI units (i.e., 3.9 lbs/1.8 kg) at age 51 to −0.04 BMI units (i.e., −0.27 lbs/−0.13 kg) at age 69 (p > .05 at age 69).
Figure 1.
Average body mass index (BMI) trajectories for female respondents in 1937–1941 cohort, by ethnicity and education (model 3)
Note: Average trajectories based on model 3 estimates. All covariates except for immigrant status, mortality, and attrition were centered at their grand mean.
Figure 2.
Average body mass index (BMI) trajectories for male respondents in 1937–1941 cohort, by ethnicity and education (model 3)
Note: Average trajectories based on model 3 estimates. All covariates except for immigrant status, mortality, and attrition were centered at their grand mean.
Discussion
Our findings of ethnic and education disparities in BMI during the transition to older adulthood generally provide support for our two hypotheses. First, after adjusting for mortality, health conditions, and health behaviors, BMI disparities persisted across ethnic and education groups for women but narrowed between White men with 12 or more years of schooling and both Hispanic men with less than 12 years of schooling and Black men with 12 or more years of schooling. Thus, we find support for our hypothesis that BMI disparities persist or diminish during the transition to older adulthood. Second, the association between education and BMI trajectories differed only for His-panic men. Thus, we found partial support for our second hypothesis that the relationship between education and BMI would vary by ethnicity.
Our findings can be situated within the larger body of work that has examined how health disparities change or persist as a function of ethnicity and education. The theory of cumulative advantage/disadvantage contends that as the advantaged age, they are more likely to accumulate a reserve of economic and social resources that can assist them in avoiding or delaying the onset of illness or disability (Ross and Wu 1996). As such, health trajectories between advantaged and disadvantaged groups are expected to diverge with age (Dannefer 2003). Ferraro and Shippee (2009) have argued, however, that selective mortality results in greater homogeneity in a population. Because disadvantaged groups experience less longevity than advantaged groups, selective mortality is a likely explanation for diminishing education and ethnic disparities at older ages (Dupre 2007, 2008; Farmer and Ferraro 2005). In addition, among older adults, higher rates of serious illnesses among obese individuals appear to increase the risk of premature mortality (Thorpe and Ferraro 2004).
Our results suggest that selective mortality, health behaviors, and health conditions may partially explain diminishing disparities in BMI between Hispanic women with less than 12 years of schooling and White women with 12 years or more of schooling. That is, after controlling for mortality, health behaviors, and health conditions, these disparities persisted but did not diminish. Among men, however, adjusting for these additional covariates did little to explain the diminishing disparities found between White men with 12 or more years of schooling and their Black counterparts or Hispanic men with less than 12 years of schooling. Although we adjusted for mortality that occurred during the course of the study, we could not account for selective mortality that occurred prior to baseline assessment. Thus, it is possible that our sample had already experienced some level of increasing homogeneity due to selective mortality. Additional studies that follow individuals from early adulthood through late life are therefore needed to fully understand how education and ethnicity impact BMI disparities across the life course.
In addition to selective mortality, our findings may be influenced by higher levels of declining health among disadvantaged groups. Given that certain illnesses (e.g., cancer) are often accompanied by precipitous weight loss (Wallace and Schwartz 2002), the significantly slower rate of increase in BMI that we found among Blacks with 12 years or more of schooling and Hispanic men with less than 12 years of schooling may reflect the higher rates of certain illnesses experienced by ethnic minority groups in the United States and individuals with lower education. We adjusted for a number of health measures (i.e., self-rated health, total number of health conditions); however, these measures may not adequately account for rapidly progressing illnesses that are associated with weight loss.
Among women, the association between education and BMI was fairly consistent across ethnicity. That is, education was associated with lower BMI at age 62, but was generally unrelated to BMI change. Lewis et al. (2005) also found that education was inversely associated with baseline BMI among a community sample of middle-aged Black and White women but was unrelated to changes in BMI over a four-year period. Alternatively, findings from another longitudinal study of individuals making the transition to older adulthood documented an inverse association between education and baseline BMI for White and Black women but found that education was unrelated to BMI change for White women and positively associated with BMI change among Black women (Mujahid et al. 2005).
Among men, the association between education and BMI varied by ethnicity. Education was inversely associated with BMI at age 62 among Whites and Hispanics and positively associated with BMI change only among Hispanics. Mujahid et al. (2005) reported similar findings for White men but found that among Black men education was positively associated with baseline BMI and this positive association was maintained over time. We know of no longitudinal studies that have examined differential effects of education among Hispanic men making the transition to older adulthood.
Inconsistencies between our findings and the findings reported by Mujahid and colleagues (2005) may be in part due to differences in the sampling frame. Whereas we use a nationally representative sample of White, Black, and Hispanic individuals making the transition to older adulthood, Mujahid et al. (2005) used a sample drawn from four community sites—two of the community samples were virtually all White and one of the community samples was entirely Black. Research suggests that neighborhood and community contexts affect individual obesity risk (cf. Do et al. 2007; Glass, Rasmussen, and Schwartz 2006; Grafova et al. 2008), thus, studies that rely on community samples may not be generalizable to the U.S. population.
When examining the joint effects of education and ethnicity, the results did not follow a consistent pattern. For more highly educated Black men (e.g., 12 or more years of schooling), declines in BMI occurred more rapidly than for their White counterparts. If BMI declines are in part related to illness, one might expect that lower educated Black men would experience more rapid declines in BMI, as is the case for lower educated Hispanic men. However, for some health outcomes researchers have documented that the greatest health disparities between Black and White individuals occur at the highest levels of socioeconomic status (Farmer and Ferraro 2005). While support for such effects is limited, it is possible that as individuals transition to older adulthood, education may provide greater protection against declining health among Whites than among Blacks, which could in turn prevent precipitous declines in BMI among Whites.
Significant differences in BMI trajectories also emerged by birth cohort. While previous studies have reported similar trends (Flegal et al. 1998, 2002; Ogden et al. 2006), our findings are quite striking given that birth cohorts in our sample at most differed by 5 years. Indeed, after 10 years, an “average” White woman with 12 years or more of schooling would be 6.8 pounds (2.2 kilograms) heavier if she were in the younger cohort rather than the older cohort. This gap would be 5.8 pounds (2.6 kilograms) for an “average” White man with 12 or more years of schooling. Thus, obesity prevalence among older adults is likely to increase rapidly as younger cohorts transition to older adulthood.
Although prior research suggests that BMI declines at older ages, our findings did not bear this pattern out (Flegal et al. 2002; Sheehan et al. 2003; Wallace and Schwartz 2002). One possible explanation for this difference is the age range represented in our sample. Half of our sample had not yet turned 70 at the last wave of data collection, the age at which population-level declines in weight become detectable (Wallace and Schwartz 2002).
Our results should be considered in light of study limitations. We were unable to adjust for differences in disability or physical activity, which are known correlates of obesity, because these items were not measured consistently across time in the HRS (St. Clair et al. 2008). Survey items pertaining to disability (e.g., activities of daily living, instrumental activities of daily living, and functional limitations) underwent significant modifications across the survey intervals. Rather than exclude data from waves with inconsistent disability measures, as other studies have done (V. A. Freedman et al. 2008), we chose to retain baseline observations and to not adjust for disability. Although it would have been preferable to adjust for disability status, we did not want to introduce other, unknown biases into our models by using inconsistent time-varying measures. Likewise, questions about physical activity underwent extensive changes across multiple waves of data collection. Including physical activity measures would have therefore violated a major assumption in longitudinal data analysis—that the variables were measured consistently across time (Singer and Willet 2003).
Our study also utilized self-reported measures of height and weight, which likely underestimates the true weight of respondents, particularly at the extreme of the weight distribution. Given that we compared individuals with themselves over time, the effects of underreporting weight should be minimized (Bowman and DeLucia 1992; Kuskowska-Wolk, Bergstrom, and Bostrom 1992). Although prior longitudinal studies focusing on the transition to older adulthood have used clinically based measures of height and weight (Lewis et al. 2005; Mujahid et al. 2005; Sheehan et al. 2003; Wolinksy et al. 2009), these studies either relied on community samples that may not be generalizable to the U.S. population or excluded Hispanics from the analyses (Sheehan et al. 2003). Thus, even though we were unable to utilize clinically based measures of height and weight, our use of a nationally representative sample provides insight into social processes affecting BMI change in the general U.S. population of older adults.
Finally, our results were based on respondents born between 1931 and 1941 who were living in the United States in 1992 and thus can only be generalized to this population. Because the meaning of education has changed over time (Levy and Murnane 1992), the extent to which education affects BMI trajectories may depend on birth cohort. Thus, the association between education and BMI trajectories that we observed in this study may not hold for younger or older cohorts of U.S. adults.
Conclusion
The purpose of our study was to examine the influence of ethnicity and education on BMI and BMI change during the transition to late life. Our results highlight the continued need to investigate processes of cumulative inequality across a range of health behaviors and health outcomes in order to more fully understand how inequality gets “under the skin.” Indeed, given the increased risk of poor health and premature mortality in disadvantaged groups, cumulative inequality in health may manifest not only as widening health disparities as has been traditionally thought, but also manifest as persistent or diminishing disparities depending on the health indicator and the period of life under investigation. Moreover, our results emphasize the potential for accelerated increases in BMI during the transition to older adulthood among successive cohorts, as well as the importance of ethnicity and education in BMI risk.
Our findings suggest that ethnic and education disparities generally persist during the transition to older adulthood. However, previous longitudinal studies have found widening BMI disparities by education and ethnicity among younger adults (Burke et al. 1996; Clarke et al. 2009). Taken together, this suggests that ethnic and education disparities are established early in life and widen and persist across much of the life course. Thus, there are likely multiple points in the life course when population-level interventions could effectively reduce or eliminate social disparities in BMI. For example, increasing access to postsecondary education among young, disadvantaged adults may reduce obesity disparities later in life by allowing them the opportunity to accumulate social and economic resources that can promote healthy lifestyle behaviors. Given that a greater proportion of middle-aged adults are returning to school to attain higher education (Choy 2002), expanding access to postsecondary education among nontraditional students may also result in the reduction of obesity disparities at older ages. Additional longitudinal studies are needed, however, to establish a solid body of evidence that can be used to identify which points in the life course population-level interventions could be used to address BMI disparities at older ages.
Acknowledgments
We would like to thank Phillipa Clarke, Gilbert Gee, and Mindi Spencer for providing us with helpful comments and suggestions on earlier drafts of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research and/ or authorship of this article:
This research was supported, in part, by National Institute of Aging Training grant P30 AG012846-14 to the Population Studies Center, University of Michigan.
Biographies
Katrina M. Walsemann is an assistant professor at the University of South Carolina, Department of Health Promotion, Education, and Behavior. Her research focuses on how different forms of social stratification can influence health and racial health disparities during key developmental periods and/or cumulatively across the life course.
Jennifer A. Ailshire is an NIA postdoctoral fellow at the Andrus Gerontology Center at the University of Southern California, School of Gerontology. Her research focuses on the social determinants of health disparities and the health effects of negative and positive experiences in the neighborhood and family.
Footnotes
Authors’ Note
This study is based on publically available data and was classified as exempt by the University of South Carolina’s Institutional Review Board.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Alley Dawn E, Chang Virgina W. The Changing Relationship of Obesity and Disability, 1988–2004. Journal of the American Medical Association. 2007;298:2020–027. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- Baltrus Peter T, Lynch John W, Everson-Rose Susan, Raghunathan Trivellore E, Kaplan George A. Ethnicity, Life-course Socioeconomic Position, and Body Weight Trajectories Over 34 years: The Alameda County Study. American Journal of Public Health. 2005;95:1595–601. doi: 10.2105/AJPH.2004.046292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowman Robert, DeLucia Janice. Accuracy of Self-reported Weight: A Meta-analysis. Behavior Therapy. 1992;23:637–55. [Google Scholar]
- Burke GL, Bild DE, Hilner JE, Folsom AR, Wagenknecht LE, Sidney S. Differences in Weight Gain in Relation to Race, Gender, Age and Education in Young Adults: The CARDIA Study. Ethnicity & Health. 1996;1:327–35. doi: 10.1080/13557858.1996.9961802. [DOI] [PubMed] [Google Scholar]
- Chang Virginia W, Lauderdale Diane S. Income Disparities in Body Mass Index and Obesity in the United States, 1971–2002. Archives of Internal Medicine. 2005;165:2122–128. doi: 10.1001/archinte.165.18.2122. [DOI] [PubMed] [Google Scholar]
- Choy Susan. Non-traditional Undergraduates: Findings From the “Condition of Education, 2002”. Washington, DC: National Center for Educational Statistics; 2002. [Google Scholar]
- Clarke Philippa, O’Malley Patrick M, Johnston Lloyd D, Schulenberg John E. Social Disparities in BMI Trajectories Across Adulthood by Gender, Ethnicity and Lifetime Socio-economic Position: 1986–2004. International Journal of Epidemiology. 2009;38:499–509. doi: 10.1093/ije/dyn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannefer Dale. Cumulative Advantage/Disadvantage and the Life Course: Cross-fertilizing Age and Social Science Theory. The Journals of Gerontology Series B Psychological Sciences and Social Sciences. 2003;58B:S327–37. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- Do Phuong D, Dubowitz Tamara, Bird Chloe E, Lurie Nicole, Escarce Jose J, Finch Brian K. Neighborhood Context and Ethnicity Differences in Body Mass Index: A Multilevel Analysis using the NHANES III Survey (1988–1994) Economics and Human Biology. 2007;5:179–203. doi: 10.1016/j.ehb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre Matthew E. Educational Differences in Age-related Patterns of Disease: Reconsidering the Cumulative Disadvantage and Age-as-leveler Hypotheses. Journal of Health and Social Behavior. 2007;48:1–15. doi: 10.1177/002214650704800101. [DOI] [PubMed] [Google Scholar]
- Dupre Matthew E. Educational Differences in Health Risks and Illness Over the Life Course: A Test of Cumulative Disadvantage Theory. Social Science Research. 2008;37:1253–266. doi: 10.1016/j.ssresearch.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Farmer Melissa M, Ferraro Kenneth F. Are Racial Disparities in Health Conditional on Socioeconomic Status? Social Science & Medicine. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F, Shippee Tetyana P. Aging and Cumulative Inequality: How Does Inequality Get Under the Skin? Gerontologist. 2009;49:333–43. doi: 10.1093/geront/gnp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro Kenneth F, Shippee Tetyana P, Schafer Markus H. Cumulative Inequality Theory for Research on Aging and the Life Course. In: Bengston VL, Gans D, Putney NM, Silverstein M, editors. Handbook of Theories of Aging. New York: Springer; 2009. pp. 413–33. [Google Scholar]
- Ferraro Kenneth F, Thorpe Roland J, Wilkinson Jody A. The Life Course of Severe Obesity: Does Childhood Overweight Matter? The Journals of Gerontology Series B Psychological Sciences and Social Sciences. 2003;58B:S110–19. doi: 10.1093/geronb/58.2.s110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Caroll MD, Kuczmarski RJ, Johnson CL. Overweight and Obesity in the United States: Prevalence and Trends, 1960–1994. International Journal of Obesity. 1998;22:39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- Flegal Katherine M, Carroll Margaret D, Ogden Cynthia L, Johnson Clifford L. Prevalence and Trends in Obesity Among US Adults, 1999–2000. Journal of the American Medical Association. 2002;288:1723–727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- Freedman David S, Khan Laura Kettel, Serdula Mary K, Dietz William H, Srinivasan Sathanur R, Berenson Gerald S. Racial Differences in the Tracking of Childhood BMI to Adulthood. Obesity Research. 2005;13:928–35. doi: 10.1038/oby.2005.107. [DOI] [PubMed] [Google Scholar]
- Freedman Vicki A, Martin Linda G, Schoeni Robert F, Cornman Jennifer C. Declines in Late-life Disability: The Role of Early- and Mid-life Factors. Social Science and Medicine. 2008;66:1588–602. doi: 10.1016/j.socscimed.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T, Bound John, Waidmann Timothy A, Colen Cynthia G, Steffick Dianne. Inequality in Life Expectancy, Functional Status, and Active Life Expectancy Across Selected Black and White Populations in the United States. Demography. 2001;38:227–51. doi: 10.1353/dem.2001.0015. [DOI] [PubMed] [Google Scholar]
- Glass Thomas A, Rasmussen Meghan D, Schwartz Brian S. Neighborhoods and Obesity in Older Adults—The Baltimore Memory Study. American Journal of Preventive Medicine. 2006;31:455–63. doi: 10.1016/j.amepre.2006.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen Penny, Adair Linda S, Nelson Melissa C, Popkin Barry M. Five-year Obesity Incidence in the Transition Period Between Adolescence and Adulthood: The National Longitudinal Study of Adolescent Health. American Journal of Clinical Nutrition. 2004;80:569–75. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- Grafova Irina B, Freedman Vicki A, Kumar Rizie, Rogowski Jeannette. Neighborhoods and Obesity in Later Life. American Journal of Public Health. 2008;98:2065–071. doi: 10.2105/AJPH.2007.127712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Shumei S, Zeller Christine, Chumlea William Cameron, Siervogel Roger M. Aging, Body Composition, and Lifestyle: The Fels Longitudinal Study. American Journal of Clinical Nutrition. 1999;70:405–11. doi: 10.1093/ajcn/70.3.405. [DOI] [PubMed] [Google Scholar]
- He Xiaoxing Z, Baker David W. Changes in Weight Among a Nationally Representative Cohort of Adults Aged 51 to 61, 1992 to 2000. American Journal of Preventive Medicine. 2004;27:8–15. doi: 10.1016/j.amepre.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. Sampling Weights: Revised for Tracker 2.0 and Beyond. University of Michigan; Ann Arbor, MI: 2009. Retrieved November 20, 2009 ( http://hrsonline.isr.umich.edu/sitedocs/wghtdoc.pdf) [Google Scholar]
- House James S, Lepkowski James M, Kinney Ann M, Mero Richard P, Kessler Ronald C, Regula Herzog A. The Social Stratification of Aging and Health. Journal of Health and Social Behavior. 1994;35:213–34. [PubMed] [Google Scholar]
- James Sherman A, Fowler-Brown Angela, Raghunathan Trevillore E, Van Hoewyk John. Life-course Socioeconomic Position and Obesity in African American Women: The Pitt County Study. American Journal of Public Health. 2006;96:554–60. doi: 10.2105/AJPH.2004.053447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn Henry S, Williamson David F. Is Race Associated With Weight Change in US Adults After Adjustment for Income, Education, and Marital Factors? American Journal of Clinical Nutrition. 1991;53:1566S–570S. doi: 10.1093/ajcn/53.6.1566S. [DOI] [PubMed] [Google Scholar]
- Kimm Sue YS, Glynn Nancy W, Obarzanek Eva, Kriska Andrea M, Daniels Stephen R, Barton Bruce A, Liu Kiang. Relation Between the Changes in Physical Activity and Body Mass Index During Adolescence: A Multicentre Longitudinal Study. The Lancet. 2005;366:301–07. doi: 10.1016/S0140-6736(05)66837-7. [DOI] [PubMed] [Google Scholar]
- Krieger N, Rowley D, Hermann AA, Avery B, Phillips MT. Racism, Sexism, and Social Class: Implications for Studies of Health, Disease, and Well-being. American Journal of Preventive Medicine. 1993;9:82–122. [PubMed] [Google Scholar]
- Kuskowska-Wolk A, Bergstrom R, Bostrom G. Relationship Between Questionnaire Data and Medical Records of Height, Weight, and Body Mass Index. International Journal of Obesity. 1992;16:1–9. [PubMed] [Google Scholar]
- Levy Frank, Murnane Richard J. U.S. Earnings Levels and Earnings Inequality: A Review of Recent Trends and Proposed Explanations. Journal of Economic Literature. 1992;30:1333–381. [Google Scholar]
- Lewis Tene T, Everson-Rose Susan A, Sternfeld Barbara, Karavolos Kelly, Wesley Deidre, Powell Lynda H. Race, Education, and Weight Change in a Biracial Sample of Women at Midlife. Archives of Internal Medicine. 2005;165:545–51. doi: 10.1001/archinte.165.5.545. [DOI] [PubMed] [Google Scholar]
- Lynch Scott M. Cohort and Life Course Patterns in the Relationship Between Education and Health: A Hierarchical Approach. Demography. 2003;40:309–33. doi: 10.1353/dem.2003.0016. [DOI] [PubMed] [Google Scholar]
- Lynch Scott M. Explaining Life Course and Cohort Variation in the Relationship Between Education and Health: The Role of Income. Journal of Health and Social Behavior. 2006;47:324–38. doi: 10.1177/002214650604700402. [DOI] [PubMed] [Google Scholar]
- McTigue Kathleen M, Garrett Joanne M, Popkin Barry M. The Natural History of the Development of Obesity in a Cohort of Young U.S. Adults Between 1981 and 1998. Annals of Internal Medicine. 2002;136:857–64. doi: 10.7326/0003-4819-136-12-200206180-00006. [DOI] [PubMed] [Google Scholar]
- Miech Richard A, Shanahan Michael J. Socioeconomic Status and Depression Over the Life Course. Journal of Health and Social Behavior. 2000;41:162–76. [Google Scholar]
- Mo-suwan L, Tongkumchum P, Puetpaiboon A. Determinants of Overweight Tracking From Childhood to Adolescence: A 5-year Follow-up Study of Hat Yai Schoolchildren. International Journal of Obesity. 2000;24: 1642–647. doi: 10.1038/sj.ijo.0801432. [DOI] [PubMed] [Google Scholar]
- Mujahid Mahasin S, Diez Roux Ana V, Borrell Luisa N, Javier Nieto F. Cross-sectional and Longitudinal Associations of BMI With Socioeconomic Characteristics. Obesity Research. 2005;13:1412–421. doi: 10.1038/oby.2005.171. [DOI] [PubMed] [Google Scholar]
- Ogden Cynthia L, Carroll Margaret D, Curtin Lester R, McDowell Margaret A, Tabak Carolyn J, Flegal Katherine M. Prevalence of Overweight and Obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295:1549–555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- O’Rand Angela M. The Precious and the Precocious: Understanding Cumulative Disadvantage and Cumulative Advantage Over the Life Course. Gerontologist. 1996;36:230–38. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- RAND HRS Data. RAND HRS Data, Version H. Santa Monica, CA: RAND Center for the Study of Aging; 2008. Retrieved March 1, 2009 ( http://www.rand.org/labor/aging/dataprod.html) [Google Scholar]
- Reynolds Sandra L, Saito Yasuhiko, Crimmins Eileen M. The Impact of Obesity on Active Life Expectancy in Older American Men and Women. The Gerontologist. 2005;45:438–44. doi: 10.1093/geront/45.4.438. [DOI] [PubMed] [Google Scholar]
- Ross Catherine E, Wu Chialing. Education, Age, and the Cumulative Advantage in Health. Journal of Health and Social Behavior. 1996;37:104–20. [PubMed] [Google Scholar]
- Rzehak P, Heinrich J. Development of Relative Weight, Overweight and Obesity From Childhood to Young Adulthood. A Longitudinal Analysis of Individual Change of Height and Weight. European Journal of Epidemiology. 2006;21:661–72. doi: 10.1007/s10654-006-9051-8. [DOI] [PubMed] [Google Scholar]
- Sheehan TJ, DuBrava S, DeChello LM, Fang Z. Rates of Weight Change for Black and White Americans Over a Twenty Year Period. International Journal of Obesity. 2003;27:498–504. doi: 10.1038/sj.ijo.0802263. [DOI] [PubMed] [Google Scholar]
- Singer Judith D, Willet John B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Stata Corp. Stata Statistical Software. Release 10.0. College Station, TX: 2007. [Google Scholar]
- St Clair Patricia, Blake Darlene, Bugliari Delia, Chien Sandy, Hayden Orla, Hurd Michael, Ilchuk Serhii, Kung Fuan-Yue, Miu Angela, Panis Constantijn, Pantoja Philip, Rastegar Afshin, Rohwedder Susann, Roth Elizabeth, Carroll Joanna, Zissimopoulos Julie. RAND HRS Data Documentation Version H. Santa Monica, CA: RAND Center for the Study of Aging; 2008. [Google Scholar]
- Thorpe Roland J, Ferraro Kenneth F. Aging, Obesity, and Mortality: Misplaced Concern About Obese Older People? Research on Aging. 2004;26:108–29. doi: 10.1177/0164027503258738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace Jeffrey I, Schwartz Robert S. Epidemiology of Weight Loss in Humans With Special Reference to Wasting in the Elderly. International Journal of Cardiology. 2002;85:15–21. doi: 10.1016/s0167-5273(02)00246-2. [DOI] [PubMed] [Google Scholar]
- Walsemann Katrina M, Gee Gilbert C, Geronimus Arline T. Ethnic Differences in Trajectories of Depressive Symptoms: Disadvantage in Family Background, High School Experiences, and Adult Characteristics. Journal of Health and Social Behavior. 2009;50:82–98. doi: 10.1177/002214650905000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsemann Katrina M, Geronimus Arline T, Gee Gilbert C. Accumulating Disadvantage Over the Life Course: Evidence From a Longitudinal Study Investigating the Relationship Between Educational Advantage in Youth and Health in Middle-age. Research on Aging. 2008;30:169–99. [Google Scholar]
- Wannamethee S Goya, Gerald Shaper A, Walker Mary. Overweight and Obesity and Weight Change in Middle Aged Men: Impact on Cardiovascular Disease and Diabetes. Journal of Epidemiology and Community Health. 2005;59:134–39. doi: 10.1136/jech.2003.015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle Jane, Brodersen Naomi Henning, Cole Tim J, Jarvis Martin J, Boniface David R. Development of Adiposity in Adolescence: Five Year Longitudinal Study of an Ethnically and Socioeconomically Diverse Sample of Young People in Britain. British Medical Journal. 2006;332:1130–135. doi: 10.1136/bmj.38807.594792.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber Lynn. Understanding Race, Class, Gender, and Sexuality: A Conceptual Framework. New York: Oxford University Press; 2010. [Google Scholar]
- Williams David R, Collins Chiquita. US Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995;21:349–86. [Google Scholar]
- Williamson David F. Descriptive Epidemiology of Body Weight and Weight Change in U.S. Adults. Annals of Internal Medicine. 1993;119:646–49. doi: 10.7326/0003-4819-119-7_part_2-199310011-00004. [DOI] [PubMed] [Google Scholar]
- Willson Andrea E, Shuey Kim M, Elder Glen H., Jr Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health. American Journal of Sociology. 2007;112:1886–924. [Google Scholar]
- Winship Christopher, Radbill Larry. Sampling Weights and Regression Analysis. Sociological Methods and Research. 1994;23:230–57. [Google Scholar]
- Wolinsky Fredric D, Andresen Elena M, Malmstrom Theodore K, Schootman Mario, Philip Miller J, Miller Douglas K. Three-year Measured Weight Change in the African American Health Study. Journal of Aging and Health. 2009;21:231–43. doi: 10.1177/0898264308328949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Qi, Wang Youfa. Trends in the Association Between Obesity and Socioeconomic Status in U.S. Adults: 1971 to 2000. Obesity Research. 2004;12:1622–632. doi: 10.1038/oby.2004.202. [DOI] [PubMed] [Google Scholar]