Abstract
Introduction
Dengue is the most extensively spread mosquito-borne disease; endemic in more than 100 countries. Information about dengue disease burden, its prevalence, incidence and geographic distribution is critical in planning appropriate control measures against dengue fever. We conducted a systematic review and meta-analysis of dengue fever in India
Methods
We searched for studies published until 2017 reporting the incidence, the prevalence or case fatality of dengue in India. Our primary outcomes were (a) prevalence of laboratory confirmed dengue infection among clinically suspected patients, (b) seroprevalence in the general population and (c) case fatality ratio among laboratory confirmed dengue patients. We used binomial–normal mixed effects regression model to estimate the pooled proportion of dengue infections. Forest plots were used to display pooled estimates. The metafor package of R software was used to conduct meta-analysis.
Results
Of the 2285 identified articles on dengue, we included 233 in the analysis wherein 180 reported prevalence of laboratory confirmed dengue infection, seven reported seroprevalence as evidenced by IgG or neutralizing antibodies against dengue and 77 reported case fatality. The overall estimate of the prevalence of laboratory confirmed dengue infection among clinically suspected patients was 38.3% (95% CI: 34.8%–41.8%). The pooled estimate of dengue seroprevalence in the general population and CFR among laboratory confirmed patients was 56.9% (95% CI: 37.5–74.4) and 2.6% (95% CI: 2–3.4) respectively. There was significant heterogeneity in reported outcomes (p-values<0.001).
Conclusions
Identified gaps in the understanding of dengue epidemiology in India emphasize the need to initiate community-based cohort studies representing different geographic regions to generate reliable estimates of age-specific incidence of dengue and studies to generate dengue seroprevalence data in the country.
Author summary
Dengue fever, an extensively spread mosquito-borne disease, is endemic in more than 100 countries. Information about dengue disease burden, its prevalence and incidence and geographic distribution is necessary to guide in planning appropriate control measures including the dengue vaccine that has recently been licensed in a few countries. We performed a systematic review and meta-analysis of published studies in India on dengue. The overall estimate of the prevalence of laboratory confirmed dengue infection based on testing of more than 200,000 clinically suspected patients from 180 Indian studies was 38.3%. The pooled estimate of dengue seroprevalence in the general population and CFR among laboratory confirmed dengue patients was 56.9% and 2.6% respectively. There were no community-based studies reporting incidence of dengue. Our review also identified certain knowledge gaps about dengue epidemiology in the country. Identified gaps in the understanding of dengue epidemiology in India emphasize the need to initiate community-based cohort studies representing different geographic regions to generate reliable estimates of age-specific incidence of dengue and studies to generate dengue seroprevalence data in the country.
Introduction
Dengue is the most extensively spread mosquito-borne disease, transmitted by infected mosquitoes of Aedes species. Dengue infection in humans results from four dengue virus serotypes (DEN-1, DEN-2, DEN-3, and DEN-4) of Flavivirus genus. As per the WHO 1997 classification, symptomatic dengue virus infection has been classified into dengue fever (DF), dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS). The revised WHO classification of 2009 categorizes dengue patients according to different levels of severity as dengue without warning signs, dengue with warning signs (abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, liver enlargement, increasing haematocrit with decreasing platelets) and severe dengue [1,2,3]. Dengue fever is endemic in more than 100 countries with most cases reported from the Americas, South-East Asia and Western Pacific regions of WHO [1]. In India, dengue is endemic in almost all states and is the leading cause of hospitalization. Dengue fever had a predominant urban distribution a few decades earlier, but is now also reported from peri-urban as well as rural areas [4,5]. Surveillance for dengue fever in India is conducted through a network of more than 600 sentinel hospitals under the National Vector Borne Disease Control Program (NVBDCP) [6], Integrated Disease Surveillance Program (IDSP) [7] and a network of 52 Virus Research and Diagnostic Laboratories (VRDL) established by Department of Health Research [8]. In 2010, an estimated 33 million cases had occurred in the country [9]. During 2016, the NVBDCP reported more than 100,000 laboratory confirmed cases of dengue [6]. It is therefore possible that dengue disease burden is grossly under-estimated in India.
High dengue disease burden and frequent outbreaks result in a serious drain on country’s economy and stress on the health systems. In India, case detection, case management, and vector control are the main strategies for prevention and control of dengue virus transmission [6]. A new dengue vaccine is now available and several vaccines are in the process of development [10, 11, 12]. Information about dengue disease burden, its prevalence, incidence and geographic distribution is necessary in decisions on appropriate utilization of existing and emerging prevention and control strategies. With this background, we conducted a systematic review and meta-analysis to estimate the disease burden of dengue fever in India. We also reviewed serotype distribution of dengue viruses in circulation, and estimated case fatality ratios as well as proportion of secondary infections.
Methods
Search strategy and selection criteria
This systematic review is registered in PROSPERO (Reg. No. CRD 42017065625). We searched Medline (PubMed), Cochrane Central, WHOLIS, Scopus, Science Direct, Ovid, Google Scholar, POPLINE, Cost-Effectiveness Analysis (CEA) Registry and Paediatric Economic Database Evaluation (PEDE) databases for articles published up to 2017. The main search terms included incidence, prevalence, number of reported cases, mortality, disease burden, cost of illness, or economic burden of dengue in India. The complete search strategy is described in S1 Appendix. Back referencing of included studies in bibliography was also done to identify additional studies.
Review approach
The search results were initially imported to Zotero software (Version 4.0.29.5) and duplicate records were removed. During title screening, we examined relevant studies from various databases. Our inclusion criterion was studies reporting dengue infection in India, not restricted to setting, design, purpose and population. Titles thus selected were subjected to abstract screening. Studies were considered eligible for further examination in full text if their abstracts reported incidence, prevalence, number of reported cases, mortality or the burden of dengue fever anywhere in India. Studies reporting complications of dengue, serotype details of dengue virus as well as seroprevalence of dengue were also included. Using a pre-designed data extraction form, two reviewers extracted details from selected studies independently. The data, which differed between the reviewers, were resolved by consensus. Information about the year of publication, study setting (hospital/laboratory based, or community-based), study location, study period, laboratory investigations, number of suspected patients tested and positives, age distribution of cases, and details of dengue serotypes were abstracted (S1 Dataset).
The primary outcome measures of interest were (a) prevalence (proportion) of laboratory confirmed dengue infection among clinically suspected patients in hospital/laboratory based or community-based studies, (b) seroprevalence of dengue in the general population and (c) case fatality ratio among laboratory confirmed dengue patients. The diagnosis of acute dengue infection among the clinically suspected patients was based on any of the following laboratory criteria: (a) detection of non-structural protein-1 (NS1) antigen, (b) Immunoglobulin M (IgM) antibodies against dengue virus (c) haemagglutination inhibition (HI) antibodies against dengue virus, (d) Real-time polymerase chain reaction (RT-PCR) positivity or (e) virus isolation. Seroprevalence of dengue was based on detection of IgG or neutralizing antibodies against dengue virus. Studies providing prevalence (proportion) of laboratory confirmed dengue infection among clinically suspected patients were classified into (a) hospital/laboratory-based surveillance studies and (b) outbreak investigations or hospital/laboratory-based surveillance studies when the outbreak was ongoing in the area, as mentioned in the original research paper. Studies regarding outbreak investigations considered an increase in number of reported cases of febrile illness in a geographical area, as the criteria for defining an outbreak. The outbreak investigations included one or more of the following activities: active search for case-patients in the community, calculation of attack rates for suspected case-patients, confirmation of aetiology and entomological investigations. For the case fatality ratio, the numerator included reported number of deaths due to dengue and denominator as laboratory confirmed dengue patients.
Our secondary outcomes of interest were the following: (a) proportion of primary and secondary infections among the laboratory confirmed dengue patients. This classification was made based on the information about dengue serology provided in the paper. Primary dengue infection was defined as acute infection, as indicated by qualitative detection of NS1 antigen, and/or IgM or HI antibodies or RT-PCR positivity and absence of IgG antibodies against dengue virus. A case of acute infection as defined above, in presence of IgG antibodies, was considered as secondary dengue infection [2,13,14]. Some of the studies used the ratio of IgG to IgM antibodies as the criteria for differentiating primary and secondary infections [14]; (b) distribution of predominant and co-circulating dengue virus serotypes; (c) proportion of severe dengue infections based on WHO 1997 or WHO 2009 criteria [1,2]. The category of severe dengue infection included patients with DHF and DSS as per the WHO 1997 classification as well as severe dengue infections classified as per the WHO 2009 classification and (d) cost of illness, which included reported direct and indirect costs associated with dengue hospitalization.
Risk of bias
The risk of bias was assessed using a modified Joanna Briggs Institute (JBI) appraisal checklist for studies reporting prevalence data [15] and essential items listed in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [16]. The criteria for assessing bias primarily included methods for selecting participants, methods for laboratory testing, and outcome variables (Supplementary file S2 Appendix).
Statistical analysis
We conducted quantitative synthesis to derive meta-estimates of primary and secondary outcomes (severity of disease and primary/ secondary infections) and qualitative synthesis to describe the serotype distribution and economic burden due to dengue. We followed Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines [17]. For each study, primary outcomes (prevalence of acute infection, seroprevalence and CFR) were summarized as proportion and their 95% confidence intervals were computed. We used logit and inverse logit transformations for variance stabilization of proportions [18]. Binomial–Normal mixed effects regression model was used to estimate the pooled proportion of dengue infections. Forest plots were used to display pooled estimates. Heterogeneity was tested using likelihood ratio test. Funnel plots with logit prevalence on x-axis and standard errors on y-axis and Egger’s test were used to evaluate publication bias. Independent variables potentially associated with the prevalence of laboratory confirmed dengue were included as fixed-effects in univariate and multivariate binomial meta-regression models. P <0.05 was considered statistically significant. Sensitivity analysis was carried out by leaving out one study at a time in the order of publication to check for consistency of pooled estimates. Analyses were performed in the R statistical programming language using the ‘metafor’ package [19,20].
Results
Characteristics of included studies
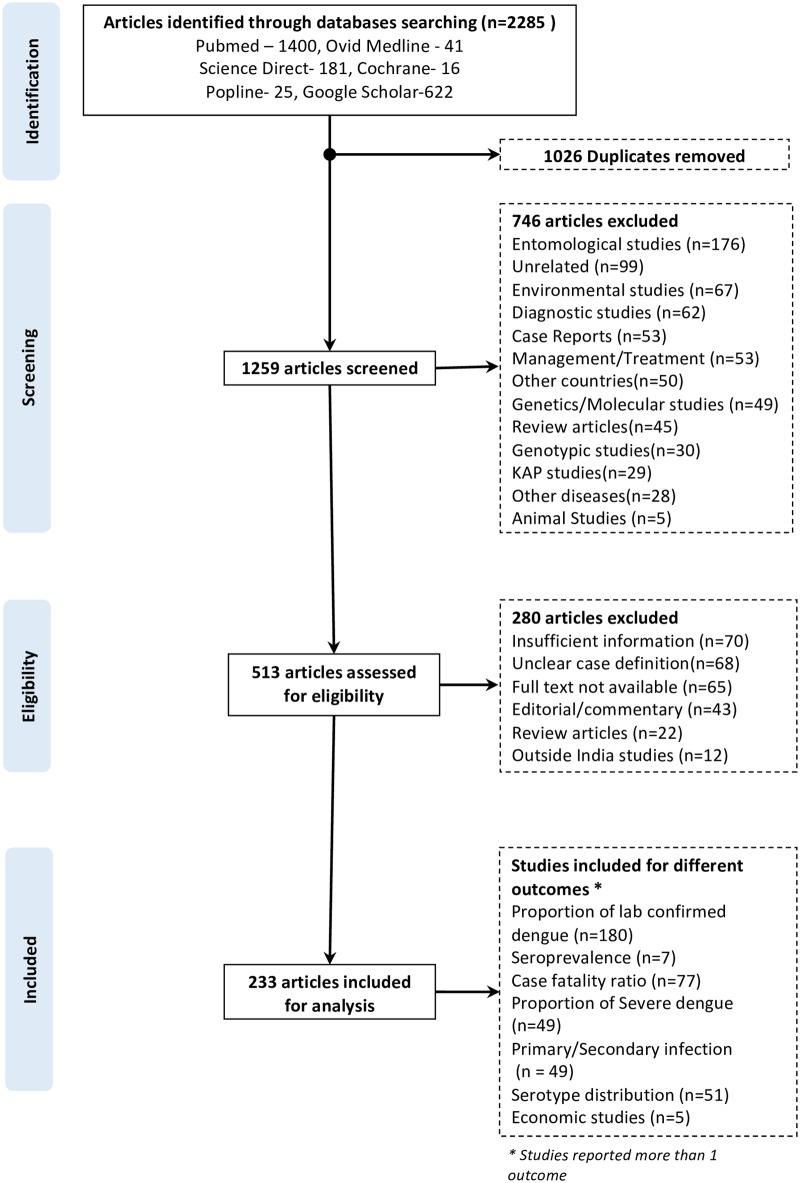
The search strategy initially identified 2,285 articles from different databases. After removal of duplicates, 1,259 articles were considered for title and abstract screening. Seven hundred and forty-six articles were excluded for reasons provided in Fig 1. Thus, 513 articles were found to be eligible for full-text review. After the review of full-text articles, 233 studies were included for the analysis [21–253]. The details of the studies included in the review are provided in the PRISMA flowchart (Fig 1). None of the studies reported incidence of dengue fever.
Fig 1. Flow diagram showing the article selection in the systematic review on dengue in India.
Primary outcomes
Prevalence (proportion) of laboratory confirmed dengue fever
Of the 233 studies included in the analysis, 180 provided information about proportion of laboratory confirmed dengue cases among clinically suspected patients [21–200]. This included 154 studies conducted in hospital or laboratory setting [21–174] and 26 studies reporting outbreak investigations [175–200]. Of the 154 studies conducted in hospital/ laboratory setting, 40 were conducted when an outbreak was ongoing in the area [135–74]. The diagnosis of acute dengue infection was based on a single assay in 86 studies (IgM antibodies = 68, RT-PCR = 11, HI antibodies = 4, virus isolation = 2, detection of NS1 antigen = 1) and more than one assay in 95 studies.
Case definitions used: Of the 154 studies conducted in hospital settings, WHO or NVBDCP case definitions were used by 39 and 2 studies respectively. The remaining studies used case definitions such as acute febrile illness/acute undifferentiated illness (n = 20), and clinically suspected dengue fever (n = 93). Similarly, of the 26 reported outbreaks, investigators used WHO or NVBDCP case definitions in 7 and 2 settings respectively, whereas acute febrile illness and clinically suspected dengue fever case definitions were used in 5 and 12 settings respectively.
Place and time distribution of studies: Of the 154 studies conducted in hospital setting, 75, 41, 27 and 7 were from north, south, east and western Indian states respectively, whereas 3 studies were from north-eastern states. One study reported data from VRDL network, covering multiple regions in India [65]. Of the 26 outbreaks, most (10, 38.5%) were reported from Southern states, followed by 9 (34.6%) in the north, 4 (15.4%) in the east, and 3 (11.5%) in the north-eastern Indian states. Most (65, 42.2%) studies conducted in hospital settings were between 2011–2017, while 48 (31.2%) were conducted between 2006–2010 and 41 (26.6%) were conducted before 2006. Eighteen (69.2%) of the 26 outbreaks were reported after 2000.
Of the 180 studies which reported proportion of dengue cases, 74 studies (30%) provided the details of laboratory confirmed cases by month with most (n = 60, 81%) reporting higher dengue positivity between August and November months.
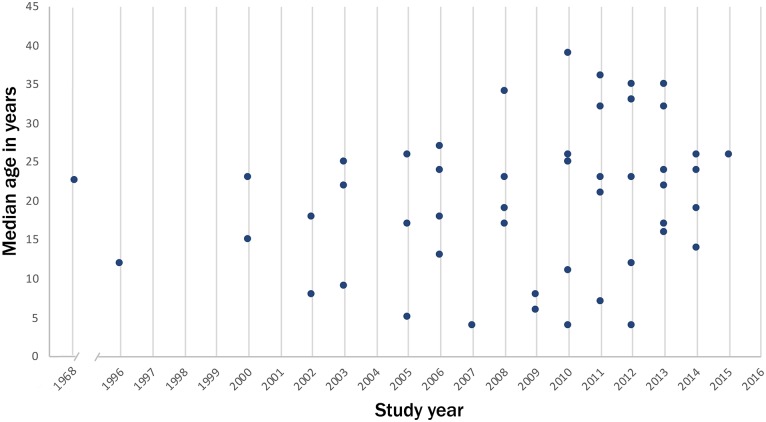
Age distribution of dengue cases: The age distribution of laboratory confirmed dengue patients was available from 52 out of 180 studies. The pooled median age of laboratory confirmed dengue cases in these studies was 22 years (Fig 2). Fifteen (28.8%) studies reported the median age of dengue cases below 15 years.
Fig 2. Distribution of median age of laboratory confirmed dengue cases by year of study, India.
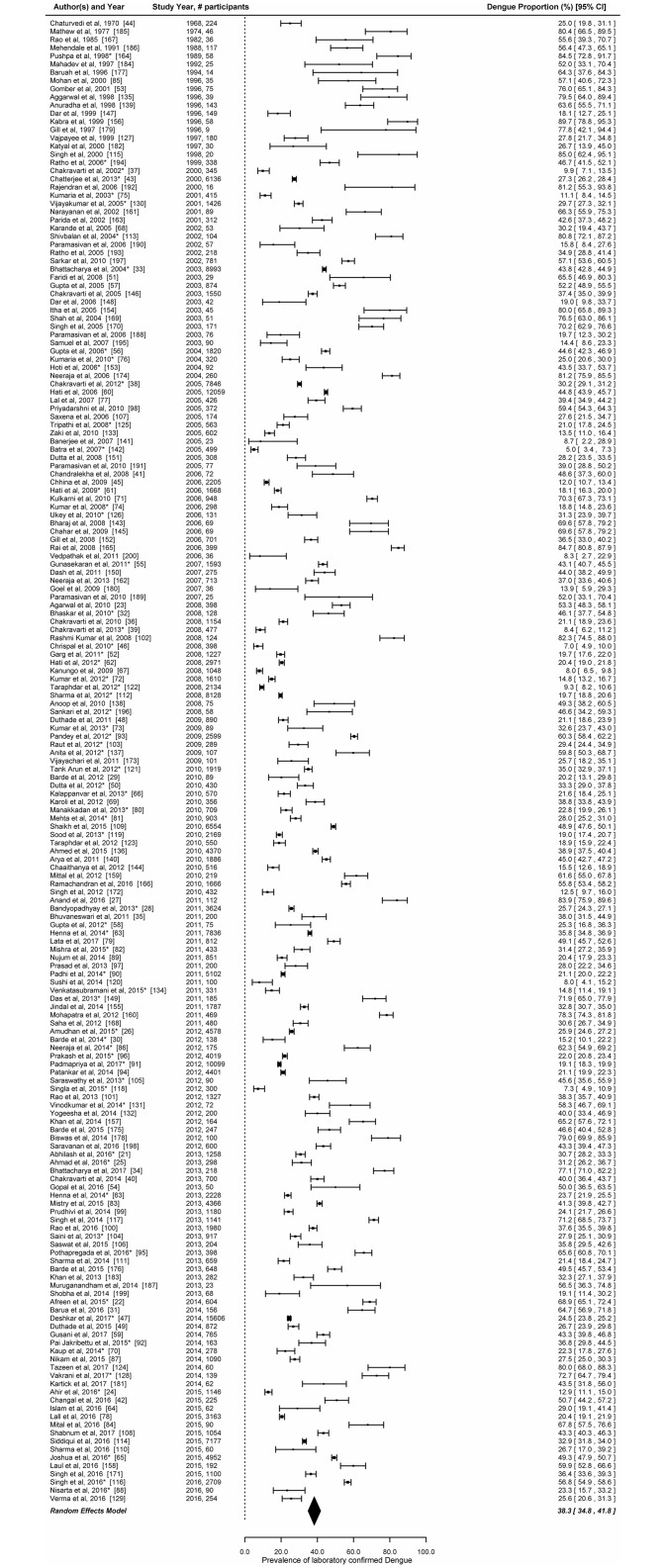
Estimates of prevalence (proportion): The overall estimate of the prevalence of laboratory confirmed dengue infection in the random effects model based on testing of 213,285 clinically suspected patients from 180 studies was 38.3% (95% CI: 34.8%–41.8%) (Fig 3). There was a significant heterogeneity in the prevalence reported by the 180 studies (LRT p<0.001). The prevalence of laboratory confirmed dengue infection was higher in studies reporting outbreaks or hospital-based surveillance studies during outbreaks (47.3%, 95% CI: 40.9–53.8) as compared to hospital-based surveillance studies (33.6%, 95% CI: 29.9–37.5) (S1A and S1B Fig). The attack rates of suspected dengue case patients were available in 8 out of the 26 outbreak investigations reports. The attack rates ranged between 1.9% and 19.5%.
Fig 3. Prevalence (proportion) of laboratory confirmed dengue among clinically suspected patients in India.
Error bars indicate 95% confidence intervals. Diamonds show the pooled estimates with 95% confidence intervals based on random effects (RE) model.
In the univariate mixed effect meta-regression model, odds of laboratory confirmation were higher in case of outbreaks or hospital-based studies conducted during outbreaks (OR = 1.8, 95% CI: 1.3–2.4). Studies which used WHO/ NVBDCP case definitions for enrolment of patients also had higher odds of detecting laboratory confirmed dengue compared to studies which used acute febrile illness/ clinically suspected dengue cases as case definitions. Compared to studies conducted before 2006–10, studies conducted between 2011 and 2017 had higher odds of identifying laboratory confirmed patients (OR = 1.33, 95% CI: 0.93–1.9). The odds of laboratory confirmation did not differ by region (Table 1). In the multivariate meta-regression model constructed by including all covariates, case definition (WHO/NVBDCP), type of study (hospital-based surveillance studies conducted during outbreaks or outbreaks) and period of study (prior to 2005 and 2011–2017) were associated with higher odds of dengue cases being laboratory confirmed.
Table 1. Meta-regression of variables associated with the proportion of laboratory confirmed dengue infections, based on a univariate and multivariate model.
(n = 180).
| Variable | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | P* | Odds Ratio (95% CI) | P* | |
| Region | ||||
| East | Ref | Ref | ||
| North | 1.41 (0.93,2.15) | 0.11 | 1.30 (0.89,1.98) | 0.17 |
| North-East | 2.39 (0.97,5.88) | 0.06 | 1.94 (0.81,4.65) | 0.14 |
| South | 1.34 (0.85,2.11) | 0.20 | 1.23 (0.79,1.90) | 0.36 |
| West | 0.82 (0.36,1.88) | 0.65 | 0.93 (0.42,2.06) | 0.85 |
| Study Type | ||||
| Hospital based surveillance (HBS) | Ref | Ref | ||
| Outbreak/HBS during outbreak | 1.78 (1.32,2.41) | 0.00 | 1.65 (1.20,2.27) | 0.00 |
| Case Definition | ||||
| AFI /Clinically suspected | Ref | Ref | ||
| WHO/NVBDCP | 1.52 (1.09,2.12) | 0.01 | 1.38 (1.01,1.91) | 0.05 |
| Year of study (midpoint) | 0.97 (0.95,0.99) | |||
| Year of study (midpoint) | ||||
| 1982–2005 | 1.67 (1.14–2.47) | 0.00 | 1.46 (1.01–2.14) | 0.05 |
| 2006–2010 | Ref | Ref | ||
| 2011–2017 | 1.33 (0.93–1.9) | 0.12 | 1.45 (1.02–2.05) | 0.04 |
Ref—Reference category; CI—Confidence interval; P*–P value.
Seroprevalence of dengue among healthy individuals
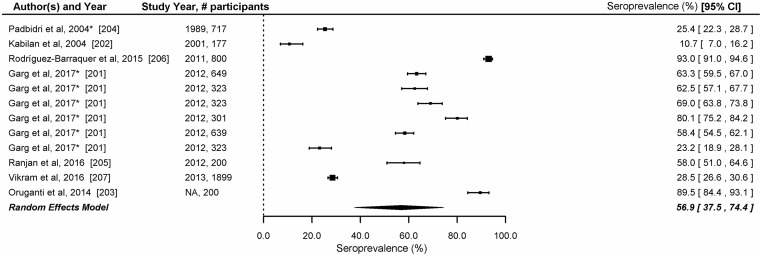
We included 7 studies reporting seroprevalence of dengue based on detection of IgG (n = 5), neutralizing antibodies (n = 1) or HI antibodies (n = 1) against dengue in the analysis [201–207]. These studies, conducted in 12 Indian states [Andaman and Nicobar islands (n = 1), Andhra Pradesh (n = 2), Tamil Nadu (n = 3), Delhi (n = 4), West Bengal (n = 1), and Maharashtra (n = 1)], surveyed 6,551 individuals. The study population surveyed in these studies included healthy children (n = 2), general population (n = 3), blood donors (n = 1) and neighbourhood contacts of dengue confirmed cases (n = 1). The overall seroprevalence of dengue fever based on these studies was 56.9% (95% CI: 37.5–74.4) (Fig 4). The age-specific prevalence of IgG antibodies was available in three studies [201, 204, 206]. There was a significant heterogeneity in the seroprevalence reported by the seven studies (LRT p<0.001). In the 3 studies which provided age specific seroprevalence, by the age of 9 years, 47.6% -73.4% children were reported to have developed IgG or neutralizing antibodies against dengue (Table 2).
Fig 4. Seroprevalence of dengue in India.
Error bars indicate 95% confidence intervals. Diamonds show the pooled estimates with 95% confidence intervals based on random effects (RE) model.
Table 2. Dengue seroprevalence by age, reported in 3 studies from India.
| Garg et al (n = 2558) [201] | Rodríguez-Barraquer et al (n = 800) [206] | Padbidri et al (n = 717) [204] | |||
|---|---|---|---|---|---|
| Age (y) | Seroprevalence (%) | Age (y) | Seroprevalence (%) | Age (y) | Sero-prevalence (%) |
| 5 | 40.7% | 5–9 | 77.1 | 0–9 | 47.6 |
| 6 | 50.9% | 10–14 | 90.3 | 10–19 | 24.0 |
| 7 | 58.6% | 15–19 | 91.7 | 20–29 | 26.8 |
| 8 | 67.4% | 20–29 | 96.3 | 30–39 | 25.0 |
| 9 | 70.8% | 30–40 | 98.8 | > = 40 | 23.3 |
| 10 | 73.4% | ||||
| Overall | 59.6 (95% CI: 57·7–61·5) | 93 (95% CI: 91.1–94.6) | 25.4 (95%CI: 22.3–28.7) | ||
Figure in square bracket indicate reference
Case fatality ratios (CFR)
Seventy-seven studies provided information about case fatality ratios; most of them (n = 72, 93.5%) were conducted after 2000. The reported CFRs in these studies ranged from 0% to 25%. There was a significant heterogeneity in the CFRs reported by the 74 studies (LRT p<0.001). Twenty (25.9%) studies reported CFR of 2% or more. Three studies [30, 239, 195] which affected overall meta-estimates due to small denominator and hence were excluded from analysis. The pooled estimate of CFR was 2.6% (95% CI: 2.0–3.4) (Fig 5).
Fig 5. Studies reporting case fatality ratio among laboratory confirmed dengue cases in India.
Error bars indicate 95% confidence intervals. Diamonds show the pooled estimates with 95% confidence intervals based on random effects (RE) model.
Secondary outcomes
Primary and secondary dengue infection
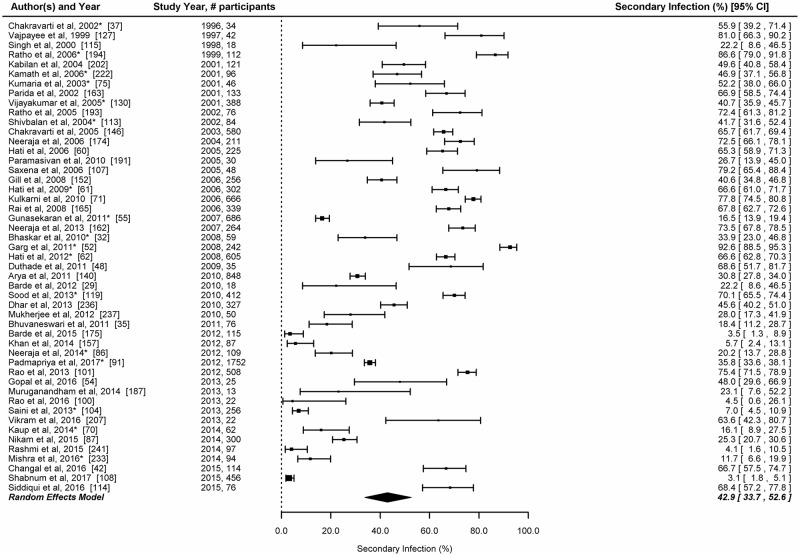
A total of 49 studies provided data which enabled classification of laboratory confirmed dengue into primary and secondary dengue infections. The number of patients with acute dengue infections in these studies ranged between 13 and 1752. Only two studies estimated the proportion of secondary infection based on IgG to IgM ratio [174, 237]. The prevalence of secondary dengue infection was <10% in 6 studies, 10–25% in 9 studies, 26–50% in 12 studies, 51–75% in 17 studies and >75% in 5 studies. The overall proportion of secondary dengue infection among laboratory confirmed patients was 42.9% (95%CI: 33.7–52.6) (Fig 6).
Fig 6. Proportion of secondary infection among laboratory confirmed dengue cases in India.
Error bars indicate 95% confidence intervals. Diamonds show the pooled estimates with 95% confidence intervals based on random effects (RE) model.
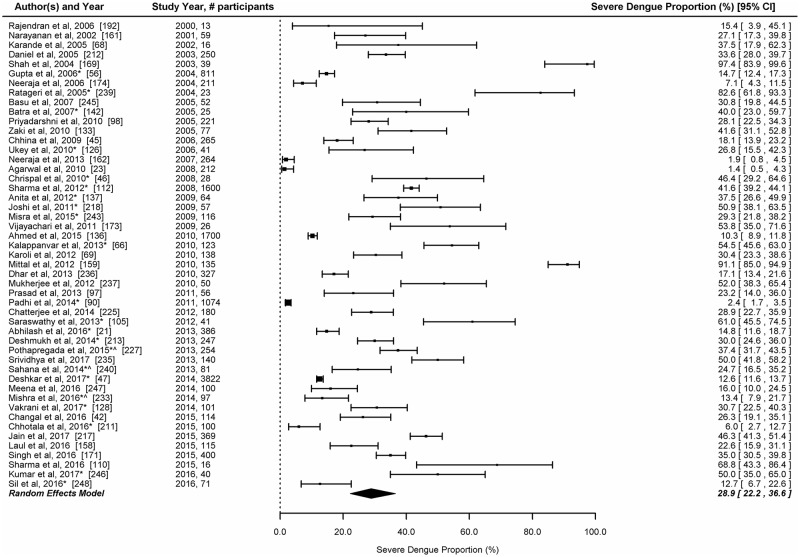
Proportion of severe cases
Information about severity of dengue was available in 49 studies. Most studies (n = 46, 93.9%) used the WHO 1997 classification while 3 studies used the WHO 2009 classification for dengue severity. The reported proportion of severe dengue cases among laboratory confirmed patients ranged between 1.4% and 97.4%. The overall proportion of severe dengue among laboratory confirmed studies in the random effects model was 28.9% (95% CI: 22.2–36.6) (Fig 7).
Fig 7. Proportion of severe dengue infections among laboratory confirmed dengue cases in India.
Serotypes of dengue virus
Information about dengue serotypes was available in 51 studies. These studies were conducted in 19 Indian states; with a regional distribution of north (n = 28), south (n = 13), east (n = 4), northeast (n = 4), and west (n = 2). Thirty-eight (75%) of the 51 studies reported circulation of more than one serotype. The predominant serotypes reported in these studies were DEN-2 and DEN-1 in the northern region, DEN-2 and DEN-3 in the southern region, and DEN-1 and DEN-2 in the eastern and the western regions. In the four studies reported from the north-eastern region, the predominant serotypes was DEN-3 followed by DEN-1 and DEN-2 serotypes (Table 3).
Table 3. Circulating dengue virus serotypes by state and region, India, 1982–2015.
| 2000 and earlier | 2001 to 2005 | 2006 to 2010 | 2011 and above | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| State by region | 1982 | 1988 | 1996 | 1997 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| East | |||||||||||||||||||
| Odisha [149] | 2,3 | ||||||||||||||||||
| Odisha [90] | 2,1 | ||||||||||||||||||
| West Bengal [123] | 1,2 | ||||||||||||||||||
| West Bengal [67] | 1,4,3,2 | ||||||||||||||||||
| North | |||||||||||||||||||
| Chandigarh [193] | 2 | ||||||||||||||||||
| Delhi [167] | 1,2 | ||||||||||||||||||
| Delhi [147] | 2,1 | ||||||||||||||||||
| Delhi [127] | 1 | ||||||||||||||||||
| Delhi [148] | 3,1,2,4 | ||||||||||||||||||
| Delhi [107] | 2,3 | ||||||||||||||||||
| Delhi[143] | 3,1,2,4 | ||||||||||||||||||
| Delhi [36] | 1,2,3 | ||||||||||||||||||
| Delhi [172] | 1 | ||||||||||||||||||
| Delhi [42] | 1,2,4 | ||||||||||||||||||
| Delhi [64] | 2,1,3,4 | ||||||||||||||||||
| Delhi [217] | 2,4 | ||||||||||||||||||
| Delhi [22] | 2,1,3 | 2,1,3 | |||||||||||||||||
| Delhi [76] | 2,3,4,1 | ||||||||||||||||||
| Delhi [38] | 3,2,1,4 | ||||||||||||||||||
| Delhi [56] | 3,1,2,4 | ||||||||||||||||||
| Delhi [39] | 1,2,3,4 | ||||||||||||||||||
| Delhi [242] | 1,2,3,4 | ||||||||||||||||||
| Delhi [137] | 2,4 | ||||||||||||||||||
| Delhi [58] | 1 | ||||||||||||||||||
| Madhya Pradesh [163] | 2 | ||||||||||||||||||
| Madhya Pradesh [29] | 4 | ||||||||||||||||||
| Madhya Pradesh [176] | 2 | ||||||||||||||||||
| Madhya Pradesh [30] | 4,1 | ||||||||||||||||||
| Uttar Pradesh [243] | 2,3,1,4 | ||||||||||||||||||
| Uttar Pradesh [93] | 2,3,1 | ||||||||||||||||||
| Uttar Pradesh [82] | 2,3,1 | ||||||||||||||||||
| Uttar Pradesh [96] | 1,3,2 | ||||||||||||||||||
| North-east | |||||||||||||||||||
| Arunachal Pradesh [157] | 3, 1,2 | ||||||||||||||||||
| Assam, Nagaland, Meghalaya, Manipur [50] | 1,2,3,4 | ||||||||||||||||||
| Manipur [183] | 3,1,2,4 | ||||||||||||||||||
| Manipur [196] | 2 | ||||||||||||||||||
| South | |||||||||||||||||||
| Andaman & Nicobar [181] | 3 | ||||||||||||||||||
| Andaman & Nicobar [144] | 1,2 | ||||||||||||||||||
| Andhra Pradesh [150] | 4, 3 | ||||||||||||||||||
| Karnataka [131] | 2,3,4,1 | ||||||||||||||||||
| Kerala [138] | 2 | ||||||||||||||||||
| Kerala [244] | 1,3,2 | ||||||||||||||||||
| Kerala [73] | 2,3,1,4 | ||||||||||||||||||
| Kerala [80] | 1,3,2 | ||||||||||||||||||
| Puducherry [27] | 3 | ||||||||||||||||||
| Puducherry [153] | 3 | ||||||||||||||||||
| Tamil Nadu [189] | 3 | ||||||||||||||||||
| Telangana [162] | 4,3 | ||||||||||||||||||
| Telangana [86] | 2,3,4,1 | ||||||||||||||||||
| West | |||||||||||||||||||
| Maharashtra [186] | 2,1 | ||||||||||||||||||
| Maharashtra [98] | 1,2,3 | ||||||||||||||||||
Key for coloured cell: Blue—One circulating serotype, Yellow—two co-circulating serotypes, Green—three co- circulating serotypes, Orange—four co- circulating serotypes. Numbers mentioned in the cell indicate predominant serotypes, in descending order.
Economic burden
Direct and Indirect cost analysis: An estimate of direct and indirect costs was reported in three studies. The average direct cost per case of dengue ranged between USD 23.5 and USD 161 and the indirect cost was around USD 25 whereas the average cost of hospitalization ranged between USD 186 and USD 432.2 [range 249-252]. The cost of dengue treatment in the private health sector was two to four times higher than that in the public sector hospitals [249, 253].
Economic impact of dengue on National Economy: Three macro-level studies addressed the economic impact of dengue faced by India [250, 251, 253]. It was estimated that the average total economic burden due to dengue in India was USD 27.4 million [251]. Another study estimated that the total direct medical cost of dengue in 2012 was USD 548 million [253]. The overall economic burden of dengue would be even higher if the cost borne by individual patients is combined with the society level cost of dengue prevention, vector control, disease control and its management, dengue surveillance as well as the cost of research and development [250, 251, 253].
Publication bias and sensitivity analysis
Funnel plots and Egger’s test revealed no publication bias in the estimates of dengue prevalence in hospital-based surveillance studies, hospital-based surveillance studies during outbreaks and outbreak investigations. CFR estimates, however, showed a significant publication bias, and studies with high prevalence were more likely to be published. In the sensitivity analysis, the estimated pooled proportions were found to be consistent for all study outcomes. (S3 Appendix)
Discussion
The present study has estimated the burden of dengue fever based on published literature from India spanning over five decades. Most of the published literature included in the analysis were hospital/ laboratory-based surveillance studies or reports of dengue outbreak investigations. Additionally the published data from VRDL network has been included in the analysis [65, 96]. The data from the other two nationally representative surveillance platforms could not be used for the analysis because surveillance data from NVBDCP only reports the number of laboratory confirmed dengue cases, while the IDSP data is not available in the public domain.
There was no community-based epidemiological study reporting the incidence of dengue fever. Our analysis revealed that among the clinically suspected dengue fever patients, the estimated prevalence of laboratory-confirmed dengue infection was 38%. The burden of dengue was also variable in studies conducted in different settings. Our findings indicated that most of the laboratory confirmed dengue cases in India occurred in young adults. Dengue positivity was higher between the months of August and November, corresponding to monsoon and post-monsoon season in most states in India.
In the meta-regression, studies that had used WHO/NVBDCP case definitions and the hospital based studies conducted during outbreaks or studies reporting outbreaks were more likely to have laboratory confirmation of dengue. The odds of laboratory confirmation were also higher among studies conducted during the period of 2011 to 2017, as compared to studies conducted prior to the year 2000.
Information about seroprevalence of dengue in the general population is a useful indicator for measuring endemicity of dengue fever. The dengue vaccine (CYD-TDV) manufactured by Sanofi Pasteur has been introduced in two sub-national programs in Philippines and Brazil [254] and it has been suggested that vaccine acts by boosting the naturally acquired immunity [255]. WHO SAGE conditionally recommends the use of this vaccine for areas in which dengue is highly endemic as defined by seroprevalence in the population targeted for vaccination [12, 256]. The results of the two vaccine trials and mathematical modelling suggest that optimal benefits of vaccination if seroprevalence in the age group targeted for vaccination was in the range of ≥70% [255, 256]. In 2018, WHO revised the recommendation from population sero-prevalence criteria to pre-vaccination screening strategy [257]. The pooled estimate based on the seven studies conducted in India indicated a dengue seroprevalence of 57%. However, this estimated seroprevalence is not representative of the country, as these studies were conducted only in 12 Indian states, and some had used a convenience sampling method [201].
The computed pooled estimate of case fatality due to dengue in India was 2.6% with a high variability in the reported CFRs. The CFR estimated in our study was higher than the estimate of 1.14% (95% CI: 0.82–1.58) reported in the meta-analysis of 77 studies conducted globally; in the 69 studies which adopted WHO 1997 dengue case classification, the pooled CFR was 1.1% (0.8–1.6) while the pooled CFR for 8 studies which used the WHO 2009 case definition, the pooled CFR was 1.6% (95% CI: 0.64–4.0) [258]. Higher CFR observed in our analysis could be due to smaller sample sizes as 14 of the 35 studies that reported CFR of 2.6 or higher had a sample size of 100 or less, while in the remaining 21 studies the denominator ranging between 101 and 400. Also, we only considered laboratory confirmed dengue cases in the denominator for the calculation of CFR. As per the NVBDCP surveillance data, a total of 683,545 dengue cases and 2,576 deaths were reported in India during 2009–2017 giving a CFR of 0.38% [6]. The lower CFR estimates from NVBDCP data could probably be on account of under-reporting of deaths due to dengue, or inclusion of higher number of mild cases in the denominator [259]. As per the NVBDCP surveillance data, an average of 28,227 dengue cases and 154 deaths were reported annually during 2009–2012. The number of dengue cases reported increased thereafter, with an average of 100,690 cases per year during 2013–2017. However, the reported number of deaths did not increase proportionately. The information about severity of dengue cases is not available from NVBDCP surveillance data.
The published studies from India indicated circulation of all the four-dengue serotypes, with DEN-2 and DEN-3 being the more commonly reported serotypes. Two third of the studies reported circulation of more than one serotype. Co-circulation of multiple serotypes was particularly evident from the published studies in Delhi. More than two third (16/19) studies from Delhi reported circulation of more than one serotype; and most of the studies conducted in the last 10 years identified co-circulation of more than one serotype [Table 3]. Our review also revealed that more than two-fifth of the laboratory confirmed infections were secondary dengue infections and nearly one-fourth of the cases were severe in nature. Circulation of numerous dengue serotypes is known to increase the probability of secondary infection, leading to a higher risk of severe dengue disease [260].
Our systematic review has certain limitations. First, our study included only peer-reviewed literature from selected databases and we excluded grey literature which may have provided additional data. Second, most of the studies on disease burden were hospital-based, with no community-based studies estimating incidence. Hospital-based studies do not provide any information about the community level transmission as hospitalization is a function of health-seeking behaviour of the population. In absence of the information about health seeking behaviour provided in these studies, we estimated the prevalence of dengue using number of patients tested in the hospitals as the denominator. Third, the hospital-based studies used varying case definitions and laboratory tests to confirm dengue infection. Fourth, information about the type of health facility (public or private), or residential status of patients (urban or rural), and age was not uniformly reported and hence we did not estimate the dengue prevalence by these variables.
In conclusion, the findings of our systematic review indicate that dengue continues to be an important public health problem in India, as evidenced by the high proportion of dengue positivity, severity and case fatality as well as co-circulation of multiple dengue virus serotypes. Our review also identified certain research gaps in the understanding on dengue epidemiology in the country. There is a need to initiate well planned community-based cohort studies representing different geographic regions of the country in order to generate reliable estimates of age-specific incidence of dengue fever in India. As such studies are cost intensive, a national level survey to estimate age-stratified dengue seroprevalence rates could be an alternative. Such estimates could be used to derive the relative proportions of primary and secondary infections using mathematical models [261]. Well planned studies in different geographic settings are also needed to generate reliable data about economic burden from India. Although the existing dengue surveillance platforms of NVBDCP, IDSP and VRDL are generating data about dengue disease burden, these systems could be strengthened to also generate data about dengue serotypes, severity, and primary and secondary infection from India.
Supporting information
(PDF)
(PDF)
(PDF)
(XLSX)
(PDF)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was funded by the Department of Bio-technology, Govt of India. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Geneva, Switzerland: WHO; 2009. Dengue: guidelines for diagnosis, treatment, prevention and control. [PubMed] [Google Scholar]
- 2.World Health Organization. Dengue hemorrhagic fever: diagnosis, treatment and control. 1997. [Google Scholar]
- 3.Barniol J, Gaczkowski R, Barbato EV, da Cunha RV, Salgado D, Martínez E, et al. Usefulness and applicability of the revised dengue case classification by disease: multi-centre study in 18 countries. BMC Infect Dis. 2011;11:106 10.1186/1471-2334-11-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kakkar M. Dengue fever is massively under-reported in India, hampering our response. BMJ. 2012. December 19;345:e8574–e8574. 10.1136/bmj.e8574 [DOI] [PubMed] [Google Scholar]
- 5.Chakravarti A., Arora R. & Luxemburger C. Fifty years of dengue in India. Trans R Soc Trop Med Hyg 2012; 106, 273–282. 10.1016/j.trstmh.2011.12.007 [DOI] [PubMed] [Google Scholar]
- 6.National Vectorborne Disease Control Program, Directorate General of Health Services. http://nvbdcp.gov.in/DENGU1.html
- 7.National Centre for Disease Control, Directorate General of Health Services. Integrated Disease Surveillance Program: Diseases under surveillance. http://www.idsp.nic.in/showfile.php?lid=3923
- 8.Department of Health Research, Govt of India. Establishment of a network of Laboratories for managing epidemics and Natural Calamities (VRDL) http://dhr.gov.in/schemes/establishment-network-laboratories-managing-epidemics-and-natural-calamities
- 9.Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013; 496:504–7. 10.1038/nature12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hadinegoro SR, Arredondo-García JL, Capeding MR, Deseda C, Chotpitayasunondh T, Dietze R, et al. Efficacy and Long-Term Safety of a Dengue Vaccine in Regions of Endemic Disease. N Engl J Med. 2015;373:1195–206. 10.1056/NEJMoa1506223 [DOI] [PubMed] [Google Scholar]
- 11.Villar L, Dayan GH, Arredondo-Garcia JL, Rivera DM, Cunha R, Deseda C, et al. Efficacy of a tetravalent dengue vaccine in children in Latin America. N Engl J Med. 2015;372:113–23. 10.1056/NEJMoa1411037 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Dengue vaccine: WHO position paper, July 2016—recommendations. Vaccine. 2017;35:1200–1201. 10.1016/j.vaccine.2016.10.070 [DOI] [PubMed] [Google Scholar]
- 13.Nisalak A. Laboratory diagnosis of dengue virus infections. Southeast Asian J Trop Med Public Health. 2015;46 Suppl 1:55–76. [PubMed] [Google Scholar]
- 14.Shu PY, Huang JH. Current advance in dengue diagnosis. Clin Diagn Lab Immunol. 2004;11:642–50. 10.1128/CDLI.11.4.642-650.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.JBC_Form_CritAp_Prev.pdf [Internet]. [cited 2017 Oct 4]. http://joannabriggs.org/assets/docs/jbc/operations/criticalAppraisalForms/JBC_Form_CritAp_Prev.pdf
- 16.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Medicine 2007;4: e297 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 18.Newcombe RG. Logit Confidence Intervals and the Inverse Sinh Transformation. The American Statistician 2001; 55: 200–202. [Google Scholar]
- 19.R Development Core Team (2014) R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- 20.Wolfgang V. Conducting meta-analyses in R with metafor package. Journal of Statistical Software 2010; 36: 1–48. [Google Scholar]
- 21.Abhilash KPP, Jeevan JA, Mitra S, Paul N, Murugan TP, Rangaraj A, et al. Acute Undifferentiated Febrile Illness in Patients Presenting to a Tertiary Care Hospital in South India: Clinical Spectrum and Outcome. J Glob Infect Dis. 2016;8(4):147–54. 10.4103/0974-777X.192966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Afreen N, Deeba F, Khan WH, Haider SH, Kazim SN, Ishrat R, et al. Molecular characterization of dengue and chikungunya virus strains circulating in New Delhi, India. Microbiol Immunol. 2014;58(12):688–96. 10.1111/1348-0421.12209 [DOI] [PubMed] [Google Scholar]
- 23.Agarwal J, Kapoor G, Srivastava S, Singh KP, Kumar R, Jain A. Unusual clinical profile of Dengue Infection in patients attending a tertiary care teaching hospital in north India. Int J Infect Dis. 2010;14:174–5. [Google Scholar]
- 24.Ahir HR, Vaghela HG. Seroprevalence of Dengue Viral Infection in Patients attending Tertiary Care Hospital, South Gujarat, India. Int J Curr Microbiol Appl Sci. 2016;5(11):96–96. [Google Scholar]
- 25.Ahmad S, Dhar M, Mittal G, Bhat NK, Shirazi N, Kalra V, et al. A comparative hospital-based observational study of mono- and co-infections of malaria, dengue virus and scrub typhus causing acute undifferentiated fever. Eur J Clin Microbiol Infect Dis. 2016;35(4):705–11. 10.1007/s10096-016-2590-3 [DOI] [PubMed] [Google Scholar]
- 26.Amudhan M, Sekar R, Sivashankar M, Raja GA, Ganesan S, Mythreyee M. Higher incidence of dengue in Theni district, South India. Indian J Med Microbiol. 2015;33(3):458–9. 10.4103/0255-0857.158605 [DOI] [PubMed] [Google Scholar]
- 27.Anand AM, Sistla S, Dhodapkar R, Hamide A, Biswal N, Srinivasan B. Evaluation of NS1 Antigen Detection for Early Diagnosis of Dengue in a Tertiary Hospital in Southern India. J Clin Diagn Res. 2016;10(4):DC01–04. 10.7860/JCDR/2016/15758.7562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.28 Bandyopadhyay B, Bhattacharyya I, Adhikary S, Konar J, Dawar N, Sarkar J, et al. A comprehensive study on the 2012 dengue fever outbreak in Kolkata, India. ISRN Virol 2013;2013:5 [Google Scholar]
- 29.Barde PV, Godbole S, Bharti PK, Chand G, Agarwal M, Singh N. Detection of dengue virus 4 from central India. Indian J Med Res. 2012;136(3):491 [PMC free article] [PubMed] [Google Scholar]
- 30.Barde PV, Shukla MK, Bharti PK, Kori BK, Jatav JK, Singh N. Co-circulation of dengue virus serotypes with chikungunya virus in Madhya Pradesh, central India. WHO South-East Asia Journal of Public Health. 2014;3(1):36 10.4103/2224-3151.206881 [DOI] [PubMed] [Google Scholar]
- 31.Barua A, Gill N. A comparative study of concurrent dengue and malaria infection with their monoinfection in a teaching hospital in Mumbai. J Assoc Physicians India. 2016;64(8):49–52. [PubMed] [Google Scholar]
- 32.Bhaskar ME, Moorthy S, Kumar NS, Arthur P. Dengue haemorrhagic fever among adults-An observational study in Chennai, south India. The Indian Journal of Medical Research. 2010;132(6):738. [PMC free article] [PubMed] [Google Scholar]
- 33.Bhattacharya D, Mittal V, Bhardwaj M, Chhabra M, Ichhpujani RL, Lal S. SeroSurveillance in Delhi, India- and early warning signal for timely detection of dengue outbreaks. Dengue Bull. 2004; 28: 207–209 [Google Scholar]
- 34.Bhattacharya PK, Gautom D, Nath N, Sarma A, Saikia H. Clinical profile of dengue in a hitherto non-endemic region-A hospital based study from northeast India. Indian Journal of Medical Specialities. 2017;8(3):124–130. [Google Scholar]
- 35.Bhuvaneswari C, Raja R, Arunagiri K, Mohana S, Sathiyamurthy K, Krishnasamy K, et al. Dengue epidemiology in Thanjavur and Trichy district, Tamilnadu-Jan 2011-dec 2011.Indian J Med Sci. 2011;65(6):260 [PubMed] [Google Scholar]
- 36.Chakravarti A, Kumar A, Matlani M. Displacement of dengue virus type 3 and type 2 by dengue virus type 1 in Delhi during 2008. Indian J Med Microbiol. 2010;28(4):412. [DOI] [PubMed] [Google Scholar]
- 37.Chakravarti A, Kumaria R, Berry N, Sharma VK. Serodiagnosis of Dengue Infection by Rapid Immunochromatography Test in a Hospital Setting in Delhi, India, 1999–2001. 2002; 26: 107–112 [Google Scholar]
- 38.Chakravarti A, Matlani M, Kashyap B, Kumar A. Awareness of changing trends in epidemiology of dengue fever is essential for epidemiological surveillance. Indian J Med Microbiol. 2012;30(2):222 10.4103/0255-0857.96699 [DOI] [PubMed] [Google Scholar]
- 39.Chakravarti A, Chauhan MS, Kumar S, Ashraf A. Genotypic characterization of dengue virus strains circulating during 2007–2009 in New Delhi. Arch Virol. 2013;158(3):571–81. 10.1007/s00705-012-1522-5 [DOI] [PubMed] [Google Scholar]
- 40.Chakravarti A, Roy P. Comments on 'Current emerging situation of dengue in India': with regard to the clinical and laboratory characteristics of paediatric dengue in India. Trop Doct. 2014;44(4):246–7. 10.1177/0049475514543942 [DOI] [PubMed] [Google Scholar]
- 41.Chandralekha, Gupta P, Trikha A. The north Indian dengue outbreak 2006: a retrospective analysis of intensive care unit admissions in a tertiary care hospital. Trans R Soc Trop Med Hyg. 2008;102(2):143–7. 10.1016/j.trstmh.2007.11.002 [DOI] [PubMed] [Google Scholar]
- 42.Changal KH, Raina A, Raina M, Bashir R, Latief M, Mir T, et al. Differentiating secondary from primary dengue using IgG to IgM ratio in early dengue: an observational hospital based clinico-serological study from North India. BMC infectious diseases. 2016;16(1):715 10.1186/s12879-016-2053-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chatterjee S, Khatun T, Sarkar A, Taraphdar D. An overview of dengue infections during 2000–2010 in Kolkata, India. Dengue Bull. 2013;37:77. [Google Scholar]
- 44.Chaturvedi UC, Kapoor AK, Mathur A, Chandra D, Khan AM, Mehrotra RML. A clinical and epidemiological study of an epidemic of febrile illness with haemorrhagic manifestations which occurred at Kanpur, India, in 1968. Bull World Health Organ. 1970;43(2):281 [PMC free article] [PubMed] [Google Scholar]
- 45.Chhina DK, Goyal O, Goyal P, Kumar R, Puri S, Chhina RS. Haemorrhagic manifestations of dengue fever & their management in a tertiary care hospital in north India. Indian J Med Res. 2009;129(6):718–721. [PubMed] [Google Scholar]
- 46.Chrispal A, Boorugu H, Gopinath KG, Chandy S, Prakash JAJ, Thomas EM, et al. Acute undifferentiated febrile illness in adult hospitalized patients: the disease spectrum and diagnostic predictors-an experience from a tertiary care hospital in South India. Trop doct. 2010;40(4):230–234. 10.1258/td.2010.100132 [DOI] [PubMed] [Google Scholar]
- 47.Deshkar ST, Raut SS, Khadse RK. Dengue infection in central India: a 5 years study at a tertiary care hospital. Int J Res Med Sci. 2017;5(6):2483–2489. [Google Scholar]
- 48.Duthade MM, Bhakare JK, Damle AS. Clinical profile of dengue haemorrhagic fever from Jan 2009 to Dec 2009 in and around Aurangabad. J Commun Dis. 2011;43(2):131–4. [PubMed] [Google Scholar]
- 49.Duthade MM, Damle AS, Bhakre JB, Gaikwad AA, Iravane JA, Jadhav A, et al. The Study of Detection of Dengue NS1 Antigen and IgM Antibody by ELISA in and around Aurangabad, India. Int J Curr Microbiol App Sci. 2015;4(10):416–422. [Google Scholar]
- 50.Dutta P, Khan SA, Borah J, Mahanta J. Demographic and clinical features of patients with Dengue in Northeastern Region of India: a retrospective cross-sectional study during 2009–2011. J Virol Microbiol. 2012;2012. [Google Scholar]
- 51.Faridi MMA, Aggarwal A, Kumar M, Sarafrazul A. Clinical and biochemical profile of dengue haemorrhagic fever in children in Delhi. Trop doct. 2008;38(1):28–30. 10.1258/td.2007.006158 [DOI] [PubMed] [Google Scholar]
- 52.Garg A, Garg J, Rao YK, Upadhyay GC, Sakhuja S. Prevalence of dengue among clinically suspected febrile episodes at a teaching hospital in North India. Journal of Infectious Diseases and Immunity. 2011;3(5):85–89. [Google Scholar]
- 53.Gomber S, Ramachandran VG, Kumar S, Agarwal KN, Gupta P, Dewan DK. Hematological observations as diagnostic markers in dengue hemorrhagic fever-a reappraisal. Indian pediatrics. 2001;38(5):477–481. [PubMed] [Google Scholar]
- 54.Gopal KA, Kalaivani V, Anandan H. Prevalence of Dengue Fever and Comparative Analysis of IgM and IgG Antibodies in Dengue Fever in Thoothukudi-Southern Coastal City, Tamil Nadu. Annals of International Medical and Dental Research, 2016;2(6):4–7 [Google Scholar]
- 55.Gunasekaran P, Kaveri K, Mohana S, Arunagiri K, Babu BS, Priya PP, et al. Dengue disease status in Chennai (2006–2008): A retrospective analysis. Indian J Med Res.2011;133(3):322. [PMC free article] [PubMed] [Google Scholar]
- 56.Gupta E, Dar L, Kapoor G, Broor S. The changing epidemiology of dengue in Delhi, India. Virol J. 2006;3:92 10.1186/1743-422X-3-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gupta E, Dar L, Narang P, Srivastava VK, Broor S. Serodiagnosis of dengue during an outbreak at a tertiary care hospital in Delhi. Indian J Med Res. 2005;121(1):36 [PubMed] [Google Scholar]
- 58.Gupta E, Mohan S, Bajpai M, Choudhary A, Singh G. Circulation of Dengue virus-1 (DENV-1) serotype in Delhi, during 2010–11 after Dengue virus-3 (DENV-3) predominance: A single centre hospital-based study. Vector Borne Zoonotic Dis. 2012;49(2):82. [PubMed] [Google Scholar]
- 59.Gusani JK, Assudani HJ, Kothari K, Ghosh AN. Serological and Epidemiological Picture of Dengue during the Year 2014: An Exclusive Study of Kutch District, Gujarat, India. Int J Curr Microbiol App Sci. 2017;6(5):2100–2106. [Google Scholar]
- 60.Hati AK. Studies on dengue and dengue haemorrhagic fever (DHF) in West Bengal State, India. J Commun Dis. 2006;38(2):124–9. [PubMed] [Google Scholar]
- 61.Hati AK. Dengue serosurveillance in Kolkata, facing an epidemic in West Bengal, India. J Vector Borne Dis. 2009;46(3):197–204. [PubMed] [Google Scholar]
- 62.Hati AK, Bhattacharjee I, Mukherjee H, Bandyopadhayay B, Bandyopadhyay D, De R, et al. Concurrent dengue and malaria in an area in Kolkata. Asian Pac J Trop Med. 2012;5(4):315–7. 10.1016/S1995-7645(12)60046-7 [DOI] [PubMed] [Google Scholar]
- 63.As Henna, Ijas Ahmed K, Harilal Sl, Saritha N, Ramani BaiJ T, Nujuma ZT. Trends in dengue during the periods 2002–2004 and 2010–2012 in a tertiary care setting in Trivandrum, Kerala, India. Dengue Bulletin;2014;38:43. [Google Scholar]
- 64.Islam A, Abdullah M, Tazeen A, Afreen N, Deeba F, Naqvi IH, et al. Detection of all the four serotypes of dengue virus in New Delhi, India during post monsoon season of 2015. Indian J Health Sci Care. 2016;3(3):24–29. [Google Scholar]
- 65.Joshua V, Murhekar MV, Ashok M, Kanagasabai K, Ravi M, Sabarinathan R, et al. Mapping dengue cases through a national network of laboratories, 2014–2015. Indian J Med Res. 2016;144(6):938 10.4103/ijmr.IJMR_673_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kalappanvar NK, Vinodkumar CS, Basavarajappa KG, Chandrasekhar G, Sanjay D. Outbreak of dengue infection in rural Davangere, Karnataka. Asian Pac J Trop Med. 2013;6(6):502 10.1016/S1995-7645(13)60084-X [DOI] [PubMed] [Google Scholar]
- 67.Kanungo S, Amarasinghe A. Dipika Sur, et al. Surveillance for dengue fever in eastern Kolkata, West Bengal, India: preliminary results. In: International meeting on emerging diseases and surveillance, Abstract presented at IMED Vienna, Austria. 2009.
- 68.Karande S, Gandhi D, Kulkarni M, Bharadwaj R, Pol S, Thakare J, et al. Concurrent outbreak of leptospirosis and dengue in Mumbai, India, 2002. J Trop Pediatr. 2005;51(3):174–81. 10.1093/tropej/fmh100 [DOI] [PubMed] [Google Scholar]
- 69.Karoli R, Fatima J, Siddiqi Z, Kazmi KI, Sultania AR. Clinical profile of dengue infection at a teaching hospital in North India. J Infect Dev Ctries. 2012;6(7):551–4. [DOI] [PubMed] [Google Scholar]
- 70.Kaup S, Sankarankutty J. Seroprevalence and seasonal trend of dengue virus infection at a teaching hospital in Tumkur, India. Scholars Journal of Applied Medical Sciences. 2014;2:922–926. [Google Scholar]
- 71.Kulkarni MJ, Sarathi V, Bhalla V, Shivpuri D, Acharya U. Clinico-epidemiological profile of children hospitalized with dengue. Indian J Pediatr. 2010;77(10):1103–1107. 10.1007/s12098-010-0202-2 [DOI] [PubMed] [Google Scholar]
- 72.Kumar A, Balachandran V, Dominic A, Dinesh KR, Karim S, Rao G. Serological evidence of leptospirosis and dengue coinfection in an endemic region in South India. Annals of Tropical medicine and public health. 2012;5(4):286. [Google Scholar]
- 73.Kumar NP, Jayakumar PR, George K, Kamaraj T, Krishnamoorthy K, Sabesan S, et al. Genetic characterization of dengue viruses prevalent in Kerala State, India. J Med Microbiol. 2013;62(4):545–552. [DOI] [PubMed] [Google Scholar]
- 74.Kumar R, Tripathi P, Tripathi S, Kanodia A, Pant S, Venkatesh V. Prevalence and clinical differentiation of dengue fever in children in northern India. Infection. 2008;36(5):444–9. 10.1007/s15010-008-7172-6 [DOI] [PubMed] [Google Scholar]
- 75.Kumaria R, Chakravarti A, Verma V. Sero-diagnosis of dengue infections in a hospital setting in Delhi, India, 1999–2002. In: J Clin Virol; 2003; 28:p. S63–S63. [Google Scholar]
- 76.Kumaria R. Correlation of disease spectrum among four Dengue serotypes: a five years hospital based study from India. Braz J Infect Dis. 2010;14(2):141–6. [PubMed] [Google Scholar]
- 77.Lal M, Aggarwal A, Oberoi A. Dengue fever—an emerging viral fever in Ludhiana, North India. Indian J Public Health. 2007;51(3):198–9. [PubMed] [Google Scholar]
- 78.Lall H, Gupta P, Debbarma M, Sharma P, Ansari SK, Jais M, et al. Sero-Prevalance of Dengue in Tertiary Care Hospital in Delhi. Int J Curr Microbiol Appl Sci. 2016;5(6):439–445. [Google Scholar]
- 79.Lata S, Singh G, Dubey S. An Epidemiological Investigation of Dengue Outbreak in Shri Muktsar Sahib District, Punjab, India 2012. 2017;3(1):152–158. [Google Scholar]
- 80.Manakkadan A, Joseph I, Prasanna RR, Kailas L, Sreekumar E. Lineage shift in Indian strains of Dengue virus serotype-3 (Genotype III), evidenced by detection of lineage IV strains in clinical cases from Kerala. Virol J. 2013;10(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mehta KD, Gelotar PS, Vachhani SC, Makwana N, Sinha M. Profile of dengue infection in Jamnagar city and district, west India. WHO South East Asia J Public Health. 2014;3(1):72–4. 10.4103/2224-3151.206888 [DOI] [PubMed] [Google Scholar]
- 82.Mishra G, Jain A, Prakash O, Prakash S, Kumar R, Garg RK, et al. Molecular characterization of dengue viruses circulating during 2009–2012 in Uttar Pradesh, India. J Med Virol. 2015;87(1):68–75. 10.1002/jmv.23981 [DOI] [PubMed] [Google Scholar]
- 83.Mistry M, Goswami Y, Chudasama RK, Thakkar D. Epidemiological and demographic characteristics of dengue disease at a tertiary care centre in Saurashtra region during the year 2013. J Vector Borne Dis. 2015;52(4):299–303. [PubMed] [Google Scholar]
- 84.Mital R, Agarwal V, Agarwal A. To Assess the relative incidence of and to compare the hemocytological changes in malaria, dengue and typhoid fever or their combination, in children admitted in a tertiary care centre in western UP, India. Internat J Contemp Medic Res. 2016;3(3):718–23. [Google Scholar]
- 85.Mohan B, Patwari AK, Anand VK. Hepatic dysfunction in childhood dengue infection. J Trop Pediatr. 2000;46(1):40–3. 10.1093/tropej/46.1.40 [DOI] [PubMed] [Google Scholar]
- 86.Neeraja M, Iakshmi V, Teja VD, Lavanya V, Priyanka EN, Subhada K, et al. Unusual and rare manifestations of dengue during a dengue outbreak in a tertiary care hospital in South India. Arch Virol. 2014;159(7):1567–73. 10.1007/s00705-014-2010-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nikam AP, Bhise PR, Deshmukh MM. Seroprevalence of Dengue infection in clinically suspected cases of dengue at tertiary care hospital in central India. Int J Med Res Rev 2015;3(6):593–596. [Google Scholar]
- 88.Nisarta A, Ahir H. Study of Seroprevalence of Dengue Virus Infection in a Tertiary Care Hospital in Patan, Gujarat, India. Int J Curr Microbiol App Sci. 2016;5(10):819–824. [Google Scholar]
- 89.Nujum ZT, Thomas A, Vijayakumar K, Nair RR, Pillai MR, Indu PS, et al. Comparative performance of the probable case definitions of dengue by WHO (2009) and the WHO-SEAR expert group (2011). Pathog Glob Health. 2014;108(2):103–110. 10.1179/2047773214Y.0000000131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Padhi S, Dash M, Panda P, Parida B, Mohanty I, Sahu S, et al. A three year retrospective study on the increasing trend in seroprevalence of dengue infection from southern Odisha, India. Indian J Med Res. 2014;140(5):660–4. [PMC free article] [PubMed] [Google Scholar]
- 91.Padmapriya P, Kumar VS, Raja RS, Sheriff AK, Uma TS, Mohana S, et al. Dengue scenario: Chennai perspective-a six-year study (2009–2014). Arch Virol. 2017;162(1):273–279. 10.1007/s00705-016-3040-3 [DOI] [PubMed] [Google Scholar]
- 92.Pai Jakribettu R, Boloor R, Thaliath A, Yesudasan George S, George T, Ponadka Rai M, et al. Correlation of Clinicohaematological Parameters in Paediatric Dengue: A Retrospective Study. J Trop Med. 2015;2015(1–2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pandey N, Nagar R, Gupta S. Trend of dengue virus infection at Lucknow, north India (2008–2010): a hospital based study. Indian J Med Res. 2012;136(5):862 [PMC free article] [PubMed] [Google Scholar]
- 94.Patankar M, Patel B, Gandhi V, Shah P, Vegad M. Seroprevalence of Dengue in Gujarat, Western India: A study at a tertiary care hospital. Int J Med Sci Public Health. 2014;3:16–8 [Google Scholar]
- 95.Pothapregada S, Kamalakannan B, Thulasingham M. Risk factors for shock in children with dengue fever. Indian J Crit Care Med. 2015;19(11):661–4. 10.4103/0972-5229.169340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Prakash O, Singh DD, Mishra G, Prakash S, Singh A, Gupta S, et al. Observation on dengue cases from a virus diagnostic laboratory of a tertiary care hospital in North India. Indian J Med Res. 2015;142 Suppl:S7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Prasad D, Kumar C, Jain A, Kumar R. Accuracy and applicability of the revised WHO classification (2009) of dengue in children seen at a tertiary healthcare facility in northern India. Infection. 2013;41(4):775–82. 10.1007/s15010-013-0405-3 [DOI] [PubMed] [Google Scholar]
- 98.Priyadarshini D, Gadia RR, Tripathy A, Gurukumar KR, Bhagat A, Patwardhan S, et al. Clinical findings and pro-inflammatory cytokines in dengue patients in Western India: a facility-based study. PLoS ONE. 2010. 14;5(1):e8709 10.1371/journal.pone.0008709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Prudhivi S, Yenigalla BM, Myneni RB. Incidence of dengue in a rural hospital, Chinakakani, Andhra Pradesh, South India and comparison of two commercially available enzyme linked immunosorbent assays with immunochromatographic rapid test. Int J Res Med Sci. 2014;4:1534–40. [Google Scholar]
- 100.Rao MRK, Padhy RN, Das MK. Prevalence of dengue viral and malaria parasitic co-infections in an epidemic district, Angul of Odisha, India: An eco-epidemiological and cross-sectional study for the prospective aspects of public health. J Infect Public Health.2016;9(4):421–428. 10.1016/j.jiph.2015.10.019 [DOI] [PubMed] [Google Scholar]
- 101.Rao MS, Pavani K, Dass M, Kareem MA, Vinayaraj EV. Seroprevalence of dengue virus in a tertiary care hospital, Andhra Pradesh, South India. Int J Res Med Sci. 2013;1(4):448–50. [Google Scholar]
- 102.Rashmi Kumar C, Jyotsana Agarwal G, Nagar R, Jain A. Changing clinical manifestations of dengue infection in north India. Dengue Bull. 2008; 32: 118–25. [Google Scholar]
- 103.Raut S, Patil A. Dengue in and around Nagpur- Central India. Journal of Evolution of Medical and Dental Sciences. 2012;1:853–6. [Google Scholar]
- 104.Saini S, Kinikar AG, Deorukhkar S, Bhalerao D, Roushani SB. Epidemiology and seropositivity of dengue fever cases in a rural tertiary care hospital of western Maharashtra, India. Int J Bio Med Res. 2013;4(7):473–7. [Google Scholar]
- 105.Saraswathy MP, Sankari K, Sakthi G, Sripriya D, Lakshmi P. Incidence of dengue hemorrhagic fever in children: a report from Melmaruvathur Tamilnadu, India. J Pharm Sci Innov. 2013;2(1):34–36. [Google Scholar]
- 106.Saswat T, Kumar A, Kumar S, Mamidi P, Muduli S, Debata NK, et al. High rates of co-infection of Dengue and Chikungunya virus in Odisha and Maharashtra, India during 2013. Infection, Genetics and Evolution. 2015;35:134–141. 10.1016/j.meegid.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 107.Saxena P, Parida MM, Dash PK, Santhosh SR, Srivastava A, Tripathi NK, et al. Co-Circulation of Dengue Virus Serotypes in Delhi, India, 2005: Implication for Increased DH. Dengue Bull. 2006; 30: 283–287. [Google Scholar]
- 108.Shabnum M, Reddy PS, Devi PV. Screening of Dengue Fever in Clinically Suspected Cases in a Tertiary Care Hospital, Nellore, Andhra Pradesh, South India. J. Pathol. Microbiol.2017; 2(1):10–12. [Google Scholar]
- 109.Shaikh N, Raut CG, Manjunatha M. Co-infections with chikungunya and dengue viruses: A serological study in Karnataka State, India. Indian J Med Microbiol. 2015;33(3):459 10.4103/0255-0857.158607 [DOI] [PubMed] [Google Scholar]
- 110.Sharma S, Jain S, Rajaram S. Spectrum of maternofetal outcomes during dengue infection in pregnancy: an insight. Infect Dis Obstet Gynecol. 2016;2016(11):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sharma Y, Arya V, Jain S, Kumar M, Deka L, Mathur A. Dengue and Typhoid Co-infection- Study from a Government Hospital in North Delhi. J Clin Diagn Res. 2014;8(12):DC09–11. 10.7860/JCDR/2014/9936.5270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sharma Y, Kaur M, Singh S, Pant L, Kudesia M, Jain S. Seroprevalence and trend of dengue cases admitted to a government hospital, delhi—5-year study (2006–2010): a look into the age shift. Int J Prev Med. 2012;3(8):537–43. [PMC free article] [PubMed] [Google Scholar]
- 113.Shivbalan S, Anandnathan K, Balasubramanian S, Datta M, Amalraj E. Predictors of spontaneous bleeding in Dengue. Indian J Pediatr. 2004;71(1):33–6. [DOI] [PubMed] [Google Scholar]
- 114.Siddiqui O, Chakravarti A, Abhishek KS. Dengue: Lessons of an Outbreak. J Clin Diagn Res. 2016;10(6):DC01–04. 10.7860/JCDR/2016/19238.7927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Singh J, Balakrishnan N, Bhardwaj M, Amuthadevi P, George EG, Subramani K, et al. Silent spread of dengue and dengue haemorrhagic fever to Coimbatore and Erode districts in Tamil Nadu, India, 1998: need for effective surveillance to monitor and control the disease. Epidemiol Infect. 2000;125(1):195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Singh K, Sidhu SK, Devi P, Kaur M, Kaur M, Singh N. Seroprevalence of Common Viral Diseases: A Hospital Based Study from Amritsar, India. J Clin Diagn Res. 2016;10(12):DC15–DC19. 10.7860/JCDR/2016/22514.9019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Singh R, Singh SP, Ahmad N. A Study of Etiological Pattern in an Epidemic of Acute Febrile Illness during Monsoon in a Tertiary Health Care Institute of Uttarakhand, India. J Clin Diagn Res.2014;8(6):MC01–03. 10.7860/JCDR/2014/8965.4435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Singla N, Arora S, Goel P, Chander J, Huria A. Dengue in pregnancy: an under-reported illness, with special reference to other existing co-infections. Asian Pac J Trop Med. 2015;8(3):206–8. 10.1016/S1995-7645(14)60316-3 [DOI] [PubMed] [Google Scholar]
- 119.Sood S. A hospital based serosurveillance study of dengue infection in jaipur (rajasthan), India. J Clin Diagn Res.2013;7(9):1917–20. 10.7860/JCDR/2013/5562.3357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sushi KM, Sivasangeetha K, Kumar AS, Shastri P, Ganesan A, Anitha D, et al. Seroprevalence of Leptospirosis, Enteric fever and Dengue in patients with acute febrile illness in Tamil Nadu, India. Indian J Basic Applied Med Res 2014;3:615–23. [Google Scholar]
- 121.Tank Arun G, Jain Mannu R. Trend of dengue in a tertiary care hospital of Surat city, Western India. Nat J of Comm Med. 2012;3(2):302–04. [Google Scholar]
- 122.Taraphdar D, Sarkar A, Mukhopadhyay BB, Chatterjee S. A comparative study of clinical features between monotypic and dual infection cases with Chikungunya virus and dengue virus in West Bengal, India. Am J Trop Med Hyg. 2012;86(4):720–723. 10.4269/ajtmh.2012.11-0704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Taraphdar D, Sarkar A, Mukhopadhyay BB, Chakrabarti S, Chatterjee S. Rapid spread of chikungunya virus following its resurgence during 2006 in West Bengal, India. Trans. Royal Soc Trop Med Hyg. 2012;106(3):160–166. [DOI] [PubMed] [Google Scholar]
- 124.Tazeen A, Afreen N, Abdullah M, Deeba F, Haider SH, Kazim SN, et al. Occurrence of co-infection with dengue viruses during 2014 in New Delhi, India. Epidemiol Infect. 2017;145(1):67–77. 10.1017/S0950268816001990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tripathi P, Kumar R, Tripathi S, Tambe JJ, Venkatesh V. Descriptive epidemiology of dengue transmission in Uttar Pradesh. Indian Pediatr. 2008;45(4):315–8. [PubMed] [Google Scholar]
- 126.Ukey P, Bondade S, Paunipagar P, Powar R, Akulwar S. Study of seroprevalence of dengue Fever in central India. Indian J Community Med. 2010;35(4):517–9. 10.4103/0970-0218.74366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Vajpayee M, Mohankumar K, Wali JP, Dar L, Seth P, Broor S. Dengue virus infection during post-epidemic period in Delhi, India. Southeast Asian J Trop Med Public Health. 1999;30(3):507–10. [PubMed] [Google Scholar]
- 128.Vakrani GP, Subramanyam NT. Acute Renal Failure in Dengue Infection. J Clin Diagn Res. 2017;11(1):OC10–OC13. 10.7860/JCDR/2017/22800.9289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Verma RK, Singh DP, Kumari S, Siddique ME. Evaluation Of Ns1 Antigen-Capture Elisa And Igm Antibody Capture Elisa In Acute Cases Of Dengue In Rural Population In A Tertiary Care Teaching Hospital In Western Uttar Pradesh India. Int J Pharm Sci Res. 2016;7(4):1780. [Google Scholar]
- 130.Vijayakumar TS, Chandy S, Sathish N, Abraham M, Abraham P, Sridharan G. Is dengue emerging as a major public health problem? Indian J Med Res. 2005;121(2):100–7. [PubMed] [Google Scholar]
- 131.Vinodkumar CS, Kalapannavar NK, Basavarajappa KG, Sanjay D, Gowli C, Nadig NG, et al. Episode of coexisting infections with multiple dengue virus serotypes in central Karnataka, India. J Infect Public Health. 2013;6(4):302–6. 10.1016/j.jiph.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 132.Yogeesha K, Sreejith M, Sannegowda RB, Manjunath J, Arunachalam R. Clinical and Laboratory Parameters Differentiating Dengue from Other Causes of Acute Febrile Illnesses in A Tertiary Care Centre in South India. International Journal of Recent Trends in Science and Technology. 2014;10(2):373–7. [Google Scholar]
- 133.Zaki SA, Shanbag P. Clinical manifestations of dengue and leptospirosis in children in Mumbai: an observational study. Infection. 2010;38(4):285–91. 10.1007/s15010-010-0030-3 [DOI] [PubMed] [Google Scholar]
- 134.Venkatasubramani K, Paramasivan R, Thenmozhi V, Dhananjeyan K, Balaji T, Leo SVJ. Diagnosis of Chikungunya dominated co-infection with dengue during an outbreak in south India (2010 and 2012). Trop Doct. 2015;45(3):197–9. 10.1177/0049475515585476 [DOI] [PubMed] [Google Scholar]
- 135.Aggarwal A, Chandra J, Aneja S, Patwari AK, Dutta AK. An epidemic of dengue hemorrhagic fever and dengue shock syndrome in children in Delhi. Indian Pediatr. 1998;35(8):727–32. [PubMed] [Google Scholar]
- 136.Ahmed S, Ahmed N. Dengue Fever Outbreak in Delhi, North India: A Clinico-Epidemiological Study. Indian J Community Med. 2015;40(2):135 10.4103/0970-0218.153884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Anita C, Suresh K, Neha S, Sonia M. Dengue outbreak in Delhi in 2009: study of laboratory and clinical parameters. J Commun Dis. 2012;44(3):163–168. [PubMed] [Google Scholar]
- 138.Anoop M, Issac A, Mathew T, Philip S, Kareem NA, Unnikrishnan R, et al. Genetic characterization of dengue virus serotypes causing concurrent infection in an outbreak in Ernakulam, Kerala, South India. Indian J Exp Biol. 2010;48: 849–857. [PubMed] [Google Scholar]
- 139.Anuradha S, Singh N, Rizvi SNA, Agarwal S, Gur R, Mathur MD. The 1996 outbreak of dengue hemorrhagic fever in Delhi, India. Southeast Asian J Trop Med Public Health. 1998;29:503–6. [PubMed] [Google Scholar]
- 140.Arya SC, Agarwal N. Thrombocytopenia progression in dengue cases during the 2010 outbreak in Indian capital metropolis. Platelets. 2011;22(6):476–7. 10.3109/09537104.2011.556276 [DOI] [PubMed] [Google Scholar]
- 141.Banerjee G, Singh R. Sero-prevalence of Dengue infection in Lucknow. J Infect Dis.2007;39:69–70. [PubMed] [Google Scholar]
- 142.Batra P, Saha A, Chaturvedi P, Vilhekar KY, Mendiratta DK. Outbreak of dengue infection in rural Maharashtra. Indian J Pediatr. 2007;74:794–5. [PubMed] [Google Scholar]
- 143.Bharaj P, Chahar HS, Pandey A, Diddi K, Dar L, Guleria R, et al. Concurrent infections by all four dengue virus serotypes during an outbreak of dengue in 2006 in Delhi, India. Virol. J. 2008;5(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chaaithanya IK, Bhattacharya D, Muruganandam N, Thamizhmani R, Babu BVS, Sundaram SG, et al. Dengue: a newly emerging viral infection in Andaman and Nicobar Islands, India. Epidemiol Infect. 2012;140(10):1920–4. 10.1017/S0950268811002500 [DOI] [PubMed] [Google Scholar]
- 145.Chahar HS, Bharaj P, Dar L, Guleria R, Kabra SK, Broor S. Co-infections with Chikungunya Virus and Dengue Virus in Delhi, India. Emerg Infect Dis. 2009;15(7):1077–80. 10.3201/eid1507.080638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chakravarti A, Kumaria R. Eco-epidemiological analysis of dengue infection during an outbreak of dengue fever, India. Virol J.2005;2(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dar L, Broor S, Sengupta S, Xess I, Seth P. The first major outbreak of dengue hemorrhagic fever in Delhi, India. Emerg Infect Dis. 1999;5(4):589 10.3201/eid0504.990427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dar L, Gupta E, Narang P, Broor S. Cocirculation of dengue serotypes, Delhi, India, 2003. Emerging Infect Dis. 2006;12(2):352–3. 10.3201/eid1202.050767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Das B, Das M, Dwibedi B, Kar SK, Hazra RK. Molecular investigations of dengue virus during outbreaks in Orissa state, Eastern India from 2010 to 2011. Infect Genet Evol. 2013;16:401–10. 10.1016/j.meegid.2013.03.016 [DOI] [PubMed] [Google Scholar]
- 150.Dash PK, Sharma S, Srivastava A, Santhosh SR, Parida MM, Neeraja M, et al. Emergence of dengue virus type 4 (genotype I) in India. Epidemiol Infect. 2011;139(06):857–61. [DOI] [PubMed] [Google Scholar]
- 151.Dutta S, Deen JL, Sur D, Manna B, Kanungo S, Bhaduri B, et al. Increased utilization of treatment centre facilities during a dengue fever outbreak in Kolkata, India. Dengue Bull. 2008; 32: 162–66. [Google Scholar]
- 152.Gill PS, Deep A, Chaudhary U, Gill M, Singh H. An outbreak of dengue fever at a tertiary care centre, Haryana, India: a triggered catastrophe in 2006. Trop Med Health. 2008;36(4):143–7. [Google Scholar]
- 153.Hoti SL, Soundravally R, Rajendran G, Das LK, Ravi R, Das PK. Dengue and Dengue Haemorrhagic Fever Outbreak in Pondicherry, South India, during 2003–2004: Emergence of DENV-3. 2006; Dengue Bull. 2006; 30: 42–50. [Google Scholar]
- 154.Itha S, Kashyap R, Krishnani N, Saraswat VA, Choudhuri G, Aggarwal R. Profile of liver involvement in dengue virus infection. Natl Med J India. 2005;18(3):127 [PubMed] [Google Scholar]
- 155.Jindal N, Bansal R, Dhuria N. The 2011 outbreak of dengue virus infection in Malwa region of Punjab, India-an evaluation of various diagnostic tests. Asian Pac J Trop Med. 2014;4(5):363–6. [Google Scholar]
- 156.Kabra SK, Jain Y, Pandey RM, Singhal T, Tripathi P, Broor S, et al. Dengue haemorrhagic fever in children in the 1996 Delhi epidemic. Trans Royal Soc Trop Med Hyg. 1999;93(3):294–298. [DOI] [PubMed] [Google Scholar]
- 157.Khan SA, Dutta P, Topno R, Soni M, Mahanta J. Dengue Outbreak in a Hilly State of Arunachal Pradesh in Northeast India. Sci World J. 2014;2014:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Laul A, Laul P, Merugumala V, Pathak R, Miglani U, Saxena P. Clinical Profiles of Dengue Infection during an Outbreak in Northern India. Asian Pac J Trop Med. 2016;2016:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mittal H, Faridi MMA, Arora SK, Patil R. Clinicohematological Profile and Platelet Trends in Children with Dengue During 2010 Epidemic in North India. Indian J Pediatr. 2012;79(4):467–71. 10.1007/s12098-011-0586-7 [DOI] [PubMed] [Google Scholar]
- 160.Mohapatra MK, Patra P, Agrawala R. Manifestation and outcome of concurrent malaria and dengue infection. Journal of vector borne diseases. 2012;49(4):262 [PubMed] [Google Scholar]
- 161.Narayanan M, Aravind MA, Thilothammal N, Prema R, Sargunam CR, Ramamurty N. Dengue fever epidemic in Chennai-a study of clinical profile and outcome. Indian Pediatr. 2002;39(11):1027–1033. [PubMed] [Google Scholar]
- 162.Neeraja M, Lakshmi V, Dash PK, Parida MM, Rao PVL. The clinical, serological and molecular diagnosis of emerging dengue infection at a tertiary care institute in southern, India. J Clin Diagn Res. 2013;7(3):457–61. 10.7860/JCDR/2013/4786.2798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Parida MM, Dash PK, Upadhyay C, Saxena P, Jana AM. Serological & virological investigation of an outbreak of dengue fever in Gwalior, India. Indian J Med Res. 2002;116:248–54. [PubMed] [Google Scholar]
- 164.Pushpa V, Venkatadesikalu M, Mohan S, Cherian T, John TJ, Ponnuraj EM. An epidemic of dengue haemorrhagic fever/dengue shock syndrome in tropical India. Ann Trop Paediatr. 1998;18(4):289–93. [DOI] [PubMed] [Google Scholar]
- 165.Rai S, Chakravarti A, Matlani M, Bhalla P, Aggarwal V, Singh N, et al. Clinico-laboratory findings of patients during dengue outbreak from a tertiary care hospital in Delhi. Trop Doc. 2008;38(3):175–7. [DOI] [PubMed] [Google Scholar]
- 166.Ramachandran VG, Das S, Roy P, Hada V, Mogha NS. Chikungunya: a reemerging infection spreading during 2010 dengue fever outbreak in National Capital Region of India. VirusDisease. 2016;27(2):183–6. 10.1007/s13337-016-0314-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Rao CV, Bagchi SK, Pinto BD, Ilkal MA, Bharadwaj M, Shaikh BH, et al. The 1982 epidemic of dengue fever in Delhi. Indian J Med Res. 1985;82:271–5 [PubMed] [Google Scholar]
- 168.Saha B, Bandyopadhyay B, Tripathi A, Mallik S, Ghosh M, Ray K. Prevalence of chikungunya and dengue in a recent outbreak of seasonal febrile illness: an observational study in a tertiary referral hospital at Kolkata, India. Int J Infect Dis. 2012;16:e108. [Google Scholar]
- 169.Shah I, Deshpande GC, Tardeja P. Outbreak of dengue in Mumbai and predictive markers for dengue shock syndrome. J Trop Pediatr. 2004;50(5):301–305. 10.1093/tropej/50.5.301 [DOI] [PubMed] [Google Scholar]
- 170.Singh NP, Jhamb R, Agarwal SK, Gaiha M. The 2003 outbreak of dengue fever in Delhi, India. Southeast Asian J Trop Med Public Health. 2005;36(5):1174 [PubMed] [Google Scholar]
- 171.Singh N, Singh J. Clinical presentation of dengue outbreak 2015, Haryana, India: a prospective observational study. Annals of Applied Bio-Sciences. 2016;3(2):A158–163 [Google Scholar]
- 172.Singh P, Mittal V, Rizvi MMA, Chhabra M, Sharma P, Rawat DS, et al. The first dominant co-circulation of both dengue and chikungunya viruses during the post-monsoon period of 2010 in Delhi, India. Epidemiol Infect. 2012;140(07):1337–42. [DOI] [PubMed] [Google Scholar]
- 173.Vijayachari P, Singh SS, Sugunan AP, Shriram AN, Manimunda SP, Bharadwaj AP, et al. Emergence of dengue in Andaman & Nicobar archipelago: Eco-epidemiological perspective. Indian J Med Res. 2011;134(2):235–7. [PMC free article] [PubMed] [Google Scholar]
- 174.Neeraja M, Lakshmi V, Teja VD, Umabala P, Subbalakshmi MV. Serodiagnosis of dengue virus infection in patients presenting to a tertiary care hospital. Indian J Med Microbiol. 2006;24(4):280 [DOI] [PubMed] [Google Scholar]
- 175.Barde PV, Kori BK, Shukla MK, Bharti PK, Chand G, Kumar G, et al. Maiden outbreaks of dengue virus 1 genotype III in rural central India. Epidemiol Infect.2015;143(02):412–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Barde PV, Shukla MK, Kori BK, Chand G, Jain L, Varun BM, et al. Emergence of dengue in tribal villages of Mandla district, Madhya Pradesh, India. Indian J Med Res. 2015;141(5):584–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Baruah H, Mohapatra P, Kire M, Pegu DK, Mahanta J. Haemorrhagic Manifestations Associated with Dengue Virus Infection in Nagaland. J Commun Dis. 1997;28:301–3. [PubMed] [Google Scholar]
- 178.Biswas DK, Bhunia R, Basu M. Dengue fever in a rural area of West Bengal, India, 2012: an outbreak investigation. WHO-SEAJPH. 2014;3(1):46 10.4103/2224-3151.206883 [DOI] [PubMed] [Google Scholar]
- 179.Gill KS, Bandyopadhyay S, Bhardwaj M, Katyal R, Kumar K. Dengue Outbreak in Ludhiana (Punjab), India, 1996. Dengue Bull. 1997;21:47–51. [Google Scholar]
- 180.Goel MK, Malik JS, Khanna P, Gaur DR, Behera BK, Yadav RK. Sero-epidemiological investigation of an outbreak of fever in rural area of Rohtak. J Commun Dis. 2009;41(3):215–7. [PubMed] [Google Scholar]
- 181.Kartick C, Bharathi GSJ, Surya P, Anwesh M, Arun S, Muruganandam N, et al. Outbreak investigation of fever mimicking dengue in Havelock Island, an important tourist destination in the Andaman & Nicobar Archipelago, 2014. Epidemiol Infect. 2017;145(07):1437–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Katyal R, Bhardwaj M, Harit AK, Sharma SK, Kumar K, Gill KS. Dengue, Japanese Encephalitis and West Nile Flaviviral Infections Detected during a Dengue Outbreak in Sonepat District, Haryana State, India.Dengue Bull.2000;24:24–28. [Google Scholar]
- 183.Khan SA, Dutta P, Borah J, Chowdhury P, Doloi PK, Mahanta J. Dengue outbreak in an Indo-Myanmar boarder area: epidemiological aspects and risk factors. Trop Biomed. 2013;30(3):451–8. [PubMed] [Google Scholar]
- 184.Mahadev PVM, Prasad SR, Ilkal M, Mavale MS, Bedekar SS, Banerjee K. Activity of dengue-2 virus and prevalance of Aedes aegypti in the Chirimiri colliery area, Madhya Pradesh, India. Southeast Asian J Trop Med Public Health. 1997;28:126–37. [PubMed] [Google Scholar]
- 185.Mathew T, Suri JC, Suri NK, Bhola SR, Arora RR, Lal P, et al. Investigation on an epidemic of dengue in Jammu, 1974. Indian J Med Res. 1977;65(5):613–22. [PubMed] [Google Scholar]
- 186.Mehendale S, Risbud A, Rao J, Banerjee K. Outbreak of dengue fever in rural areas of Parbhani district of Maharashtra (India). Indian J Med Res. 1991;93:6–11. [PubMed] [Google Scholar]
- 187.Muruganandam N, Chaaithanya IK, Mullaikodi S, Surya P, Rajesh R, Anwesh M, et al. Dengue virus serotype-3 (subtype-III) in Port Blair, India. J Vector Borne Dis.2014;51(1):58 [PubMed] [Google Scholar]
- 188.Paramasivan R, Thenmozhi V, Hiriyan J, Dhananjeyan KJ. Serological & entomological investigations of an outbreak of dengue fever in certain rural areas of Kanyakumari district, Tamil Nadu. Indian J Med Res. 2006;123(5):697 [PubMed] [Google Scholar]
- 189.Paramasivan R, Dhananjeyan KJ, Leo S, Muniaraj M, Thenmozhi V, Rajendran R, et al. Dengue fever caused by dengue virus serotype-3 (subtype-III) in a rural area of Madurai district, Tamil Nadu. Indian J Med Res 2010, 132: 339–342. [PubMed] [Google Scholar]
- 190.Paramasivan P, Thenmozhi V, Kabilan L, Tewari SC, Arunachalam N, Dhananjeyan KJ, et al. Seroepidemiology of a focal outbreak of dengue in Tamil Nadu. Indian J Med Res. 2006, 124 (6): 718–720. [PubMed] [Google Scholar]
- 191.Paramasivan R, Thenmozhi V, Thangaratham PS, Rajendran R, Tewari SC, Dhananjeyan KJ, et al. An outbreak of dengue fever in Tirupur, Coimbatore district, Tamil Nadu. Indian J Med Res. 2010;132:105–7. [PubMed] [Google Scholar]
- 192.Rajendran G, Amalraj D, Das LK, Ravi R, Das PK. Epidemiological and Entomological Investigation of Dengue Fever in Sulurpet, Andhra Pradesh, India. Dengue Bull.2006;30:93–8. [Google Scholar]
- 193.Ratho RK, Mishra B, Kaur J, Kakkar N, Sharma K. An outbreak of dengue fever in periurban slums of Chandigarh, India, with special reference to entomological and climatic factors. Indian J Med Sci. 2005;59(12):518–26. [PubMed] [Google Scholar]
- 194.Ratho RK, Mishra B, Kumar S, Varma S. Dengue Fever/Dengue Haemorrhagic Fever in Chandigarh (North India). Dengue Bull. 2006;30:278–280. [Google Scholar]
- 195.Samuel PP, Thenmozhi V, Tyagi BK. A focal outbreak of dengue fever in a rural area of Tamil Nadu. Indian J Med Res. 2007;125(2):179–81. [PubMed] [Google Scholar]
- 196.Sankari T, Hoti SL, Singh TB, Shanmugavel J. Outbreak of dengue virus serotype-2 (DENV-2) of Cambodian origin in Manipur, India-Association with meteorological factors. Indian J Med Res. 2012;136(4):649 [PMC free article] [PubMed] [Google Scholar]
- 197.Sarkar A, Taraphdar D, Chatterjee S. Investigations of Recurrent outbreaks of unknown fever, establish rural dengue activity in West Midnapore, a costal district in West Bengal, India. Archives of Clinical Microbiology. 2010;1(4). [Google Scholar]
- 198.Saravanan MSP, Fredrick T, Jayaraman Y, Ramamoorthy M, David Jk, Vaithianathan H. Burden of dengue fever and investigating challenges, Melur block, Tamilnadu, India. Stanley Medical Journal. 2017;3(4):44–49. [Google Scholar]
- 199.Shobha S, Lokanath H, Kumar J, Rao A. A retrospective assessment of dengue fever outbreak in Bangalore urban district, Southern India. Int J Med Sci Public Health; 2014; 3(7): 845–849. [Google Scholar]
- 200.Vedpathak VL, Soundale SG, Lakde RN, Deo DS, Khadilkar HA. Clinico-epidemiological profile of an outbreak of dengue fever in rural area of Ambajogai Mandai, District Beed. J Commun Dis. 2011;43(1):69–72 [PubMed] [Google Scholar]
- 201.Garg S, Chakravarti A, Singh R, Masthi NRR, Goyal RC, Jammy GR, et al. Dengue serotype-specific seroprevalence among 5- to 10-year-old children in India: a community-based cross-sectional study. Int J Infect Dis. 2017;54:25–30. 10.1016/j.ijid.2016.10.030 [DOI] [PubMed] [Google Scholar]
- 202.Kabilan L, Velayutham T, Sundaram B, Tewari SC, Natarajan A, Rathnasamy R, et al. Field- and laboratory-based active dengue surveillance in Chennai, Tamil Nadu, India: observations before and during the 2001 dengue epidemic. Am J Infect Control. 2004;32(7):391–6. [DOI] [PubMed] [Google Scholar]
- 203.Oruganti G, Dinaker M, Tez KSRS, Rajesh JG, Vijay YV, Reddy PS. High sero-prevalence of dengue IgG antibodies among healthy individuals in Andhra Pradesh, India. Indian Journal of Public Health Research & Development. 2014;5(1):131. [Google Scholar]
- 204.Padbidri VS, Wairagkar NS, Joshi GD, Umarani UB, Risbud AR, Gaikwad DL, et al. A serological survey of arboviral diseases among the human population of the Andaman and Nicobar Islands, India. Southeast Asian J Trop Med Public Health. 2002;33:794–800. [PubMed] [Google Scholar]
- 205.Ranjan P, Natarajan V, Bajpai M, Gupta E. High Seroprevalence of Dengue Virus Infection in Blood Donors From Delhi: A Single Centre Study. J Clin Diagn Res. 2016;10(10):DC08 10.7860/JCDR/2016/21262.8711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Rodríguez-Barraquer I, Solomon SS, Kuganantham P, Srikrishnan AK, Vasudevan CK, Iqbal SH, et al. The hidden burden of dengue and chikungunya in Chennai, India. PLOS Negl. Trop. Dis. 2015;9(7):e0003906 10.1371/journal.pntd.0003906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Vikram K, Nagpal BN, Pande V, Srivastava A, Saxena R, Anvikar A, et al. An epidemiological study of dengue in Delhi, India. Acta Trop.2016;153:21–27. 10.1016/j.actatropica.2015.09.025 [DOI] [PubMed] [Google Scholar]
- 208.Agarwal R, Kapoor S, Nagar R, Misra A, Tandon R, Mathur A, et al. A clinical study of the patients with dengue hemorrhagic fever during the epidemic of 1996 at Lucknow, India. 1999;30 (4):735–740 [PubMed] [Google Scholar]
- 209.Kumar A, Pandit VR, Shetty S, Pattanshetty S, Krish SN, Roy S. A profile of dengue cases admitted to a tertiary care hospital in Karnataka, southern India. Trop Doct. 2010;40(1):45–6. 10.1258/td.2009.080376 [DOI] [PubMed] [Google Scholar]
- 210.Bhalla A, Singhal M, Suri V, Kumar S. Clinical profile of dengue fever in a tertiary care centre in North Western India. Int J Infect Dis. 2014;21:324. [Google Scholar]
- 211.Chhotala YH, Suva CM. A study of clinical profile of dengue fever in a tertiary care hospital of Jamnagar, Gujarat, India Int J Infect Dis. 2016;4(10):4500–4504. [Google Scholar]
- 212.Daniel R, Philip AZ. A study of Clinical Profile of Dengue Fever in Kollam, Kerala, India. Dengue Bull. 2005;29:197–202. [Google Scholar]
- 213.Deshmukh JM, Mavadiya S. Clinical profile of dengue infection in pediatric age group in West India. Journal of Evolution of Medical and Dental Sciences. 2014;3(35):9179–9185. [Google Scholar]
- 214.Deshwal R, Qureshi MI, Singh R. Clinical and laboratory profile of dengue fever. J Assoc Physicians India. 2015;63(12):30–32. [PubMed] [Google Scholar]
- 215.Giri S, Sharma V, Easow B, Agarwal MP, Sharma A. Low mortality during 2008 outbreak of dengue in Delhi, India: a clinicobiochemical study. Rev Ciênc Méd Biol. 2010;9:10–12. [Google Scholar]
- 216.Gupta YK, Bhardwaj HS, Bhardwaj BL, Bhardwaj K, Lal K, Prashar N. Clinical profile of dengue fever in a tertiary care centre in North India. Headache.2012;15:10–94. [Google Scholar]
- 217.Jain S, Mittal A, Sharma SK, Upadhyay AD, Pandey RM, Sinha S, et al. Predictors of dengue-related mortality and disease severity in a tertiary care center in North India. In: Open Forum Infect Dis.2017; 4(2):ofx056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Joshi R, Bai V. Profile of dengue patients admitted to a tertiary care hospital in Mumbai. Turkish J Pediatr. 2011;53(6):626. [PubMed] [Google Scholar]
- 219.Juneja D, Nasa P, Singh O, Javeri Y, Uniyal B, Dang R. Clinical profile, intensive care unit course, and outcome of patients admitted in intensive care unit with dengue. J Crit Care. 2011;26(5):449–452. 10.1016/j.jcrc.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 220.Kabra SK, Verma IC, Arora NK, Jain Y, Kalra V. Dengue haemorrhagic fever in children in Delhi. Bull World Health Organ. 1992;70(1):105 [PMC free article] [PubMed] [Google Scholar]
- 221.Kale AV, Haseeb M, Sandeep C, Shoeb K, Akshay G, Khaled M. Clinical Profile and Outcome of Dengue Fever from a Tertiary Care Centre at Aurangabad Maharashtra India: An Observational Study. IOSR Journal of Dental and Medical Sciences. 2014;13(9):14–9. [Google Scholar]
- 222.Kamath SR, Ranjit S. Clinical features, complications and atypical manifestations of children with severe forms of dengue hemorrhagic fever in South India. Indian J Pediatr. 2006;73(10):889–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Krishnamoorthy S, Bhatt AN, Mathew CT, Ittyachen AM. Hepatitis and thrombocytopenia: markers of dengue mortality. Trop doc. 2017;47(2):136–141. [DOI] [PubMed] [Google Scholar]
- 224.Nagaram PP, Piduru P, Munagala VK, Matli VV. Clinical and laboratory profile and outcome of dengue cases among children attending a tertiary care hospital of South India. Int J Contemp Pediatr. 2017;4(3):1074–1080. [Google Scholar]
- 225.Chatterjee N, Mukhopadhyay M, Ghosh S, Mondol M, Das C, Patar K. An observational study of dengue fever in a tertiary care hospital of eastern India. J Assoc Physicians India. 2014;62(3):224–7. [PubMed] [Google Scholar]
- 226.Nimmagadda SS, Mahabala C, Boloor A, Raghuram PM, Nayak A. Atypical manifestations of dengue fever (DF)-where do we stand today? J Clin Diagn Res. 2014;8(1):71 10.7860/JCDR/2014/6885.3960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Pothapregada S, Kamalakannan B, Thulasingham M, Sampath S. Clinically Profiling Pediatric Patients with Dengue. J Glob Infect Dis. 2016;8(3):115–20 10.4103/0974-777X.188596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Sahu R, Verma R, Jain A, Garg RK, Singh MK, Malhotra HS, et al. Neurologic complications in dengue virus infection A prospective cohort study. Neurology. 2014;83(18):1601–1609. 10.1212/WNL.0000000000000935 [DOI] [PubMed] [Google Scholar]
- 229.Saroch A, Arya V, Sinha N, Taneja RS, Sahai P, Mahajan RK. Clinical and laboratory factors associated with mortality in dengue. Trop doc. 2017;47(2):141–145. [DOI] [PubMed] [Google Scholar]
- 230.Sharma NL, Balasubramanyam V, Kandati J, Ponugoti M. Clinical and laboratory profile of dengue fever in children during an outbreak-one year study at tertiary care hospital, Chennai, Tamilnadu, India. Int J Contemp Pediatr. 2016;4(1):110–115. [Google Scholar]
- 231.Sharma K, Yadav A. Association of mean platelet volume with severity, serology & treatment outcome in dengue fever: prognostic utility. J Clin Diagn Res.2015;9(11):EC01 10.7860/JCDR/2015/14285.6710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Sharma G, Bhatt D, Garg GK, Sharma D, Gulati RK. A prospective seroepidemiologic study on dengue in children in Southeastern Rajasthan, India. Pediatric Review: Int J Pediatr.2016. 3(10). [Google Scholar]
- 233.Mishra S, Ramanathan R, Agarwalla SK. Clinical Profile of Dengue Fever in Children: A Study from Southern Odisha, India. Scientifica.2016;2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Verma S, Sharma SK. Clinical profiles of dengue fever in a teaching hospital of North India. Journal Of Advance Researches In Medical Sciences (Formerly Journal of Advance Researches in Biological Sciences). 2014;6(2):159–162. [Google Scholar]
- 235.Srividya V, Kruthika N. Clinico-epidemiological profile of dengue cases in a Medical College Hospital, Bengaluru, Karnataka, India. Int J Community Med Public Health. 2017;4(4):928–932. [Google Scholar]
- 236.Dhar M, Shirazi N, Ahmad S, Srivastava S, Biswas D, Bhat NK. De novo experience of a single outbreak of dengue infection at a tertiary referral centre of Uttarakhand, North India. Journal, J Indian Acad Clin Med. 2013;14(3–4):225–9 [Google Scholar]
- 237.Mukherjee S, Mitra S, Samanta M, Roy P, Sarkar M, Chatterjee S. Changing clinical profile of Dengue infection: A newer perspective in the pediatric population. J Pediatric Infect Dis. 2012;7(1):1–7. [Google Scholar]
- 238.Nandi J, Sharma RS, Dutta PK, Dhillon GPS. Dengue in the National Capital Territory (NCT) of Delhi (India): Epidemiological and entomological profile for the period 2003 to 2008. Dengue Bull. 2008;32: 156–61. [Google Scholar]
- 239.Ratageri VH, Shepur TA, Wari PK, Chavan SC, Mujahid IB, Yergolkar PN. Clinical profile and outcome of dengue fever cases. Indian J Pediatr. 2005;72(8):705–706. [DOI] [PubMed] [Google Scholar]
- 240.Sahana KS, Sujatha R. Clinical profile of dengue among children according to revised WHO classification: analysis of a 2012 outbreak from Southern India. Indian J Pediatr. 2015;82(2):109–113. 10.1007/s12098-014-1523-3 [DOI] [PubMed] [Google Scholar]
- 241.Rashmi MV, Hamsaveena null. Haematological and biochemical markers as predictors of dengue infection. Malays J Pathol. 2015;37(3):247–51. [PubMed] [Google Scholar]
- 242.Matlani M, Chakravarti A. Changing trends of dengue disease: a brief report from a tertiary care hospital in New Delhi. Braz J Infect Dis. 2011;15(2):184–5. [PubMed] [Google Scholar]
- 243.Misra UK, Kalita J, Mani VE, Chauhan PS, Kumar P. Central nervous system and muscle involvement in dengue patients: A study from a tertiary care center. J Clin Virol. 2015;72:146–51. 10.1016/j.jcv.2015.08.021 [DOI] [PubMed] [Google Scholar]
- 244.Reddy MN, Dungdung R, Valliyott L, Pilankatta R. Occurrence of concurrent infections with multiple serotypes of dengue viruses during 2013–2015 in northern Kerala, India. PeerJ. 2017;5:e2970 10.7717/peerj.2970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Basu M, Dasgupta MK, Kundu TK, Sengupta B, De GK, Roy BN. Profile of pediatric dengue cases from a tertiary care hospital in Kolkata. Indian J Public Health. 2007;51(4):234–6. [PubMed] [Google Scholar]
- 246.Kumar CM, Vyas KSK, Krishna YS. Clinical profile of dengue fever with severe thrombocytopenia and its complications: a retrospective study at a tertiary care hospital in South India. Int J Res Med Sci. 2017;5(5):1751–5. [Google Scholar]
- 247.Meena KC, Jelia S, Meena S, Arif M, Ajmera D, Jatav VS. A study of hematological profile in dengue fever at tertiary care center, Kota Rajasthan, India. Int J Adv Med. 2016;3(3):621–4. [Google Scholar]
- 248.Sil A, Das A. A Study on Different Aspects of Severe Dengue Fever in Pediatric Age Group in A Tertiary Care Setting of Eastern India. GJRA. 2016;5(10):95–97 [Google Scholar]
- 249.Kumar D, Garg S. Economic burden of dengue fever on households in Hisar district of Haryana state, India. Int J Adv Med Health Res 2014; 1(2):99–103. [Google Scholar]
- 250.Garg P, Nagpal J, Khairnar P, Seneviratne SL. Economic burden of dengue infections in India. Trans R Soc Trop Med Hyg. 2008; 102(6):570–7. 10.1016/j.trstmh.2008.02.015 [DOI] [PubMed] [Google Scholar]
- 251.Murtola T, Vasan S, Puwar T, Govil D, Field R, Gong H, Bhavsar-Vyas A, Suaya J, Howard M, Shepard D, Kohli V, Prajapati P, Singh A, Mavalankar D. Preliminary estimate of immediate cost of chikungunya and dengue to Gujarat, India. Dengue Bull 2010; 34: 32–38. [Google Scholar]
- 252.Vinothkumar PS, Prasad KN, Ingalgeri Basavaraj M, Gnanamani G. Descriptive study on treatment cost for fever during outbreak of Dengue fever in Pondicherry. International Journal of Scientific and Research Publications 2013; 3(11):1–3. [Google Scholar]
- 253.Shepard DS, Halasa YA, Tyagi BK, Adhish SV, Nandan D, Karthiga KS, Chellaswamy V, Gaba M, Arora NK, INCLEN Study Group. Economic and disease burden of dengue illness in India. Am Soc Trop Med & Hygiene 2014; 91(6):1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.WHO. Updated Questions and Answers related to the dengue vaccine Dengvaxia and its use. 2017. http://www.who.int/immunization/diseases/dengue/q_and_a_dengue_vaccine_dengvaxia_use/en/
- 255.WHO. Background paper on dengue vaccines. Prepared by the SAGE working group on dengue vaccines and who secretariat. 2016. http://www.who.int/immunization/sage/meetings/2016/april/1_Background_Paper_Dengue_Vaccines_2016_03_17.pdf?ua=1
- 256.WHO. Dengue vaccine: WHO position paper–July 2016. Wkly Epidemiol Rec. 2016; 91:349–64. [PubMed] [Google Scholar]
- 257.WHO. Revised SAGE recommendation on use of dengue vaccine 2018. http://www.who.int/immunization/diseases/dengue/revised_SAGE_recommendations_dengue_vaccines_apr2018/en/
- 258.Low GK, Ogston SA, Yong MH, Gan SC, Chee HY. Global dengue death before and after the new World Health Organization 2009 case classification: A systematic review and meta-regression analysis. Acta Trop. 2018;182:237–245. 10.1016/j.actatropica.2018.03.014 [DOI] [PubMed] [Google Scholar]
- 259.Das S, Sarfraz A, Jaiswal N, Das P. Impediments of reporting dengue cases in India. J Infect Public Health. 2017; 10:494–498. 10.1016/j.jiph.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 260.Halstead SB. Dengue. Lancet 2007;370:1644–52 10.1016/S0140-6736(07)61687-0 [DOI] [PubMed] [Google Scholar]
- 261.Imai N, Dorigatti I, Cauchemez S, Ferguson NM. Estimating dengue transmission intensity from sero-prevalence surveys in multiple countries. PLoS Negl Trop Dis. 2015;9:e0003719 10.1371/journal.pntd.0003719 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(XLSX)
(PDF)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.