Abstract
BACKGROUND AND OBJECTIVE
Ochronic arthropathy of hip (Black Hip) is a rare clinical manifestation of congenital disorder of amino acid metabolism characterized by a classic triad: (1) degenerative arthritis, (2) ochronotic pigmentation, and (3) urine that turns black on long standing or alkalinization. We report a case of ochronic arthropathy of the left hip joint that was successfully treated by total hip arthroplasty.
DESIGN AND SETTINGS
This is a case study conducted at PES Medical College, Andhra Pradesh, India.
PATIENTS AND METHODS
A 60-year-old female patient came with a history of progressive pain in her left hip joint for the last 8 months. She was diagnosed to be suffering from ochronic arthritis of left hip.
RESULTS
After tissue confirmation she was operated with total hip replacement. At the end of 2 years, the patient was symptom free without any implant loosening.
CONCLUSION
Ochronotic arthropathy is a rare metabolic disorder that can be underdiagnosed many a times. Early management is only symptomatic, and advanced cases need surgical intervention. Vitamin preparations are given because of the influence of vitamin C on tyrosine and phenylalanine metabolism. In the cases of severe degenerative arthritis of hip, total hip replacement may be considered as a surgical option.
Alkaptonuria is a rare single-gene congenital amino acid metabolic disorder characterized by black pigmentation of cartilage and other connective tissues with an incidence ranging from 1 in 5 million to 1 in 20 million.1 Premature degenerative arthritis affects the large joints in many of these patients. It is an autosomal recessive disorder with congenital absence of the enzyme homogenstic acid oxidase, which is necessary for the metabolism of amino acids phenylalanine and tyrosine.2,3 This condition is characterized by deposition of blackish yellow pigment or ochre in the cartilage and other connective tissues. A total of 50% patients are asymptomatic; the remaining develop ochronotic arthropathy later in life.4 We are reporting a rare case of alkaptonuric arthropathy of left hip joint that was successfully treated with total hip replacement.
PATIENTS AND METHODS
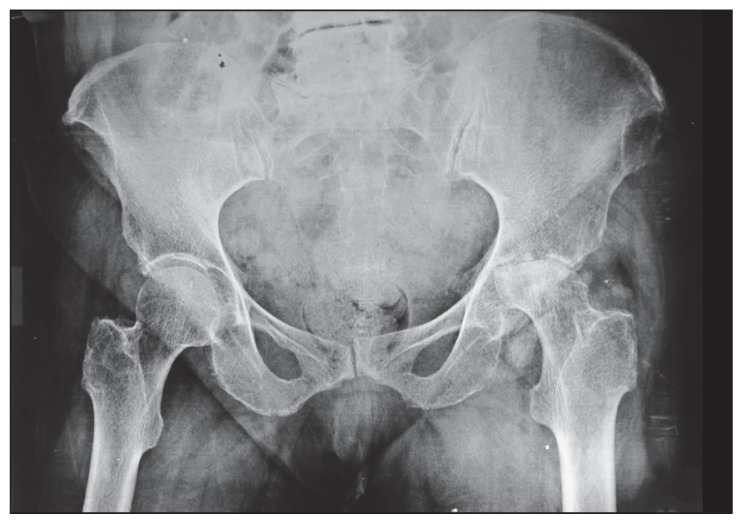
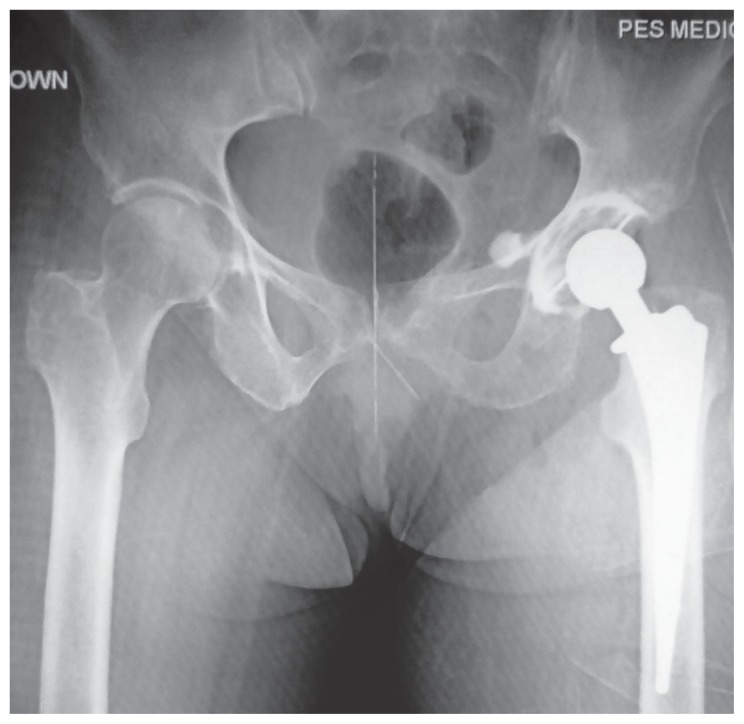
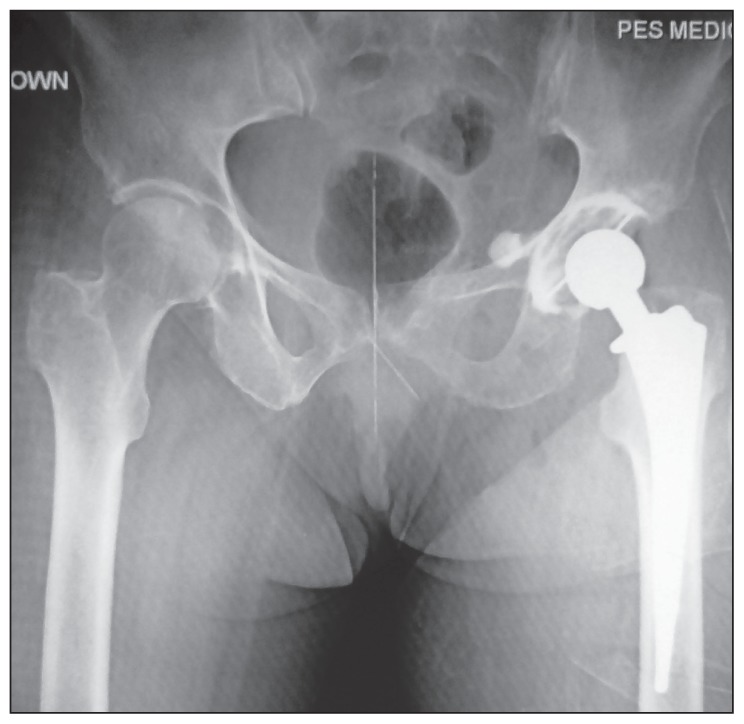
A 60-year-old female patient was referred to us with a history of progressive pain in her left hip joint for the last 8 months and low back ache from the last 10 years. She was diagnosed to have lumbar spondylosis and arthritis of left hip joint secondary to avascular necrosis of femoral head in the previous hospital. When we examined, the patient had painful gross restriction of left hip movements with 5 cm shortening. The opposite hip and knees were clinically normal. Spine movements were painful and restricted. Dark pigmentation was noted in the ear cartilage and conjunctiva (Figure 1). The serial x-rays of the pelvis, which were taken earlier, showed progressive destruction of the femoral head (Figures 2, 3, and 4). The x-ray of lumbosacral spine showed intervertebral disk calcification with narrowing of the disk spaces and gross osteoporosis with degenerative changes (Figure 5). The x-ray of chest showed calcification of the costal cartilages.
Figure 1.
Dark pigmentation in the ear cartilage and conjunctiva.
Figure 2.
X-ray of the pelvis showing destruction of the femoral head.
Figure 3.
Second x-ray of the pelvis showing more destruction of the femoral head.
Figure 4.
Subsequent x-ray of the pelvis showing further destruction of the femoral head.
Figure 5.
X-ray of lumbosacral spine showing intervertebral disk calcification.
On detailed questioning, the patient revealed that her urine turned dark on long standing and also gave history of staining of the clothes in the axilla. The patient’s urine sample was mixed with sodium hydroxide and kept for 4 hours, which turned dark. The examination of the urine confirmed the presence of homogenstic acid. Based on these clinicoradiological findings, the diagnosis of ochronosis was made.
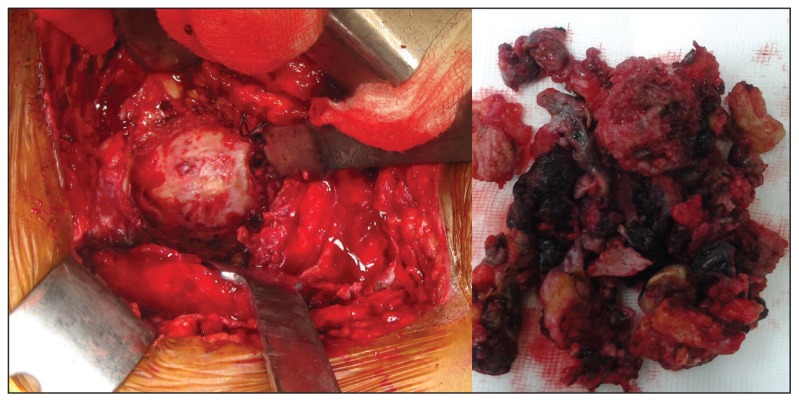
The patient was planned for elective total hip replacement under epidural anesthesia. The hip joint was opened with Moore’s approach. During the exposure, the tissues around the joint were found to be dark in color with gross involvement of the joint capsule and the synovium (Figure 6). It was decided to abandon the procedure to have a tissue diagnosis keeping in mind the rare possibility of chronic fungal infection. The joint was debrided and the tissue was sent for histopathological examination. The histological sections of removed bone and soft tissue demonstrated the classic findings of ochronosis, including pigmented areas, reactive giant cells, and thickened synovium. Once the histopathology report confirmed the diagnosis of ochronosis, the patient was operated with reverse hybrid total hip replacement after 1 week (INDUS cemented cup and uncemented stem; Figure 7). The patient was followed up with regular intervals at 6 weeks, 3 months, 6 months, and yearly afterward. At the end of 2 years, the patient was symptom free without any loosening of the implants and was satisfied with the outcome. The opposite hip and knees were found to be normal.
Figure 6.
Opening of the hip joint with Moore’s approach.
Figure 7.
Reverse hybrid total hip replacement technique.
DISCUSSION
Ochronosis or alkaptonuria is an autosomal recessive disorder due to the deficiency of homogenstic acid axidase, which is an important enzyme in the metabolism of amino acids phenylalanine and tyrosine.5 Normally, this enzyme breaks down homogenstic acid to fumaric acid and acetoacetic acid. In the absence of this enzyme, homogenstic acid gets polymerized and deposited in the connective tissues. Some part of homogenstic acid gets excreted through urine and sweat. Such urine turns dark color after long standing or mixing with alkaline agent like sodium hydroxide.4,6 Confirmatory tests for diagnosis are chromatographic, enzymatic, or spectrophotometric determinations of homogentisic acid (HGA).
Patients with alkaptonuria may be asymptomatic throughout their life, but severe cases will be manifested early in the infancy like staining of the nappies on expose to air.5,7 Maximum number of cases is diagnosed in the fourth to fifth decades. These patients are presented with staining of clothes in the axillae and appearance of pigmented nodules in pinnae, sclera, or skin.1,8,9 Ochronosis affects the entire body and can involve cardiovascular, genitourinary, ocular, cutaneous, and musculoskeletal system.10,11
Ochronotic arthropathy usually manifests in adult life with the progression of symptoms with age. In severe cases, arthropathy occurs much earlier.9 Cartilage has got special affinity for homogentisic acid pigment, and when sufficient amount is this pigment is deposited within the articular plates, it leads to the death of chondrocytes and calcification of cartilage.12,13
Spine is the first region to get affected, with patients complaining of stiffness and low back pain followed by weight-bearing joints like hip and knee.1,10,11
Smaller joints do not develop arthritis, but the cartilage within these joints shows pigmentation. The deposited HGA polymer in the cartilage leads to brittleness and fragmentation, which in turn leads to degenerative arthritis.11 The involvement of intervertebral disks leads to pigmentation and ossification of the nucleus pulposus, leading to degenerative changes.10 Pigmentation may involve tendons and ligaments because of their collagen content, which leads to tendon inflammation, calcification, and rupture.15
Primary treatment for ochronotic arthritis is mainly symptomatic.14–16 Physiotherapy and NSAIDS are beneficial but do not slow down the progression of the disease.16 Vitamin C preparations are given because of its influence on tyrosine and phenylalanine metabolism. 1 Dietary restrictions of food containing phenylalanine and tyrosine have proved to be successful in decreasing the symptoms. In the cases of severe ochronotic arthritis, total joint replacement may be considered for symptomatic pain relief.17
CONCLUSION
Ochronotic arthropathy is a rare disorder of metabolism that can be underdiagnosed many times. Sometimes it may present as a surprise to the surgeon on the operating table. Early management is only symptomatic and advanced cases need surgical intervention. As we reported, in the cases of severe degenerative arthritis of hip, total hip replacement surgery may be considered with preoperative counseling and explanation of outcomes of surgery compared to nonochronic patients.
REFERENCES
- 1.Laskar FII, Sargison KD. Ochronotic arthropathy. J Bone and Joint surgery. 1970;52 B:653–664. [PubMed] [Google Scholar]
- 2.Cooper JA, Moran TJ. Alkaptonuria or Ochronosis. Arch Pathol. 1957;64:46–48. [PubMed] [Google Scholar]
- 3.Epalcin BS. Lea. 4th Ed. Philadelphia: Feb, 1976. The spine, a radiological text and atlas; p. 335. [Google Scholar]
- 4.Greenfield GB. Radiology of bone diseases J. 3rd Ed. B Lippincort; Philadelphia: 1975. p. 800. [Google Scholar]
- 5.La Du BN. Alkaptonuria. In: stanbury JB, Wyngaarden JB, Fredericson DS, editors. The metabolic basis of inherited disease. 4th edition. New York: McGraw-Hill; 1978. pp. 268–82. [Google Scholar]
- 6.Cervenonsky J, Sitaji S, Urbanek T. Alkaplonuria and ochronosis. J Bone Joint Surg. 1959;41 A:1169–1177. [PubMed] [Google Scholar]
- 7.O’Brien WM, La Du B, Burin JJ. Ochronotic arthropathy. Am J Med. 1963;34:813–817. [Google Scholar]
- 8.Sharma OP, Gupta SK, Mohan V, Kothari MS, Agarwal AK. Ochronosis with urinary tract involvement. Indian J Radiogy. 1981;35:199–201. [Google Scholar]
- 9.Gupta RP, Mohan V, Hantlra II, Bang RL. Ochronotic arthropathy. J Kuwait Med Assoc. 1987;21(4):339–341. [Google Scholar]
- 10.Albers SE, Brozena SJ, Glass LF, Fenske NA. Alkaptonuria and ochronosis: case report and review. J Am Acad Dermatol. 1992 Oct;27(4):609–14. doi: 10.1016/0190-9622(92)70230-d. [DOI] [PubMed] [Google Scholar]
- 11.Gaines JJ., Jr The pathology of alkaptonuric ochronosis. Hum Pathol. 1989 Jan;20(1):40–6. doi: 10.1016/0046-8177(89)90200-1. Erratum in Hum Pathol 1989 May;20(5):500. [DOI] [PubMed] [Google Scholar]
- 12.Aegerter E, Kirpatrick JA. Chapter 21 in Orthopaedic diseases: Physiology Pathology, Radiology. 4th edition. Philadelphia: W.B. Saunders; 1975. Arthritis; pp. 632–34. [Google Scholar]
- 13.Di-Franco M, Caori G, Bonucci E. A morphological study of bone and articular cartilage in ochronosis. Virchows Arch. 2000;436(1):74–81. doi: 10.1007/pl00008202. [DOI] [PubMed] [Google Scholar]
- 14.La Du BN., Jr Alcaptonuria and ochronotic arthritis. Mol Biol Med. 1991 Feb;8(1):31–8. [PubMed] [Google Scholar]
- 15.Mannoni A, Selvi E, Lorenzini S, et al. Alkaptonuria, ochronosis, and ochronotic arthropathy. Semin Arthritis Rheum. 2004 Feb;33(4):239–48. doi: 10.1053/s0049-0172(03)00080-5. [DOI] [PubMed] [Google Scholar]
- 16.Borman P, Bodur H, Ciliz Ciliz D. Ochronotic arthropathy. Rheumatol Int. 2002 Mar;21(5):205–9. doi: 10.1007/s00296-002-0175-1. [DOI] [PubMed] [Google Scholar]
- 17.Kerimoglu S, Onder C, Aynaci O, Malkoc CH. Hip arthroplasty for ochronosis. Saudi Med J. 2005 Nov;26(11):1812–4. [PubMed] [Google Scholar]