Abstract
BACKGROUND AND OBJECTIVES
Studies about stroke in Saudi Arabia are limited. This retrospective study aims to determine the clinical characteristics of Saudi patients with heart failure (HF) with and without subsequent stroke, and also to find out whether gender differences exist in the presentation of HF patients who had stroke.
DESIGN AND SETTINGS
Retrospective study done at King Abdulaziz Medical City (KAMC), Riyadh, Saudi Arabia, from 2002–2008.
PATIENTS AND METHODS
A total of 293 patient (151 males, 142 females) charts from 2002–2008 were reviewed at KAMC. These charts were from Saudi patients who were diagnosed with HF, with and without subsequent stroke. Demographics, HF characteristics, stroke risk factors, and metabolic characteristics were noted and analyzed.
RESULTS
No difference was observed in HF characteristics and stroke risk factors among HF patients with and without subsequent stroke. In terms of metabolic profile, those who had stroke had significantly higher low-density lipoprotein (LDL)--cholesterol levels as compared to those without (P=.03). Stratification to gender and adjusting for age and risk factors revealed that significantly higher LDL-cholesterol and total cholesterol levels were observed in female stroke patients (P values .02, .028, respectively) and significantly higher blood urea nitrogen levels were observed in male stroke patients (P=.04) as compared to their counterparts who never had a stroke.
CONCLUSION
The gender differences in the metabolic presentation of Saudi HF patients with stroke warrant further clinical investigation. Atherogenic dyslipidemia and renal insufficiency are suggested to be early predictors for stroke and should be closely monitored in Saudi HF patients.
Annual stroke incidence documented in the MENA region ranged from 27.5 to 63 per 100 000 people, with ischemic stroke subtype being the commonest of all stroke incidences.1,2 It is acknowledged that there is scarcity of stroke data in this region, and further studies, both epidemiologic and intervention in nature, are needed to understand if the course of stroke in this specific region is the same or different from its counterparts in the developed world. In the GCC alone, there is evidence pointing to the severe lack of awareness about stroke in the general population, with the highest risk group having the poorest knowledge. 3 The lack of proper knowledge, coupled with an increasingly modernized but unhealthy lifestyle secondary to industrialization, can only exacerbate the already increasing prevalence of chronic, noncommunicable diseases among the Gulf Cooperation Council (GCC) nations and can potentially overwhelm the health sector in the near future if no intervention is done.4,5
In Saudi Arabia, the status of acute stroke care is way behind other developing nations, with only 1 active stroke center out of 7 centers in more than 350 hospitals across the kingdom.6 Furthermore, data on stroke are insufficient, which may probably explain why there is an equally lack of response from health policy makers. In this retrospective study performed in a tertiary hospital, we aim to describe the clinical profile of Saudi stroke patients who had congestive heart failure (CHF), also an under-studied population, to fill some missing gaps in the current management of stroke and also to add up in the evidence of emerging diseases in the kingdom.
PATIENTS AND METHODS
This is a retrospective chart review study conducted at King Abdullaziz Medical City (KAMC), Riyadh. Records of all Saudi patients admitted at KAMC from 2002–2008 who were diagnosed with heart failure (with or without stroke) based on echocardiogram and/or catheter and with available imaging evidence (CT scan, MRI) were included for review. The records of patients seen at the out-patient department of internal medicine from 2002–2008 were also reviewed for possible patient inclusion. Patients who had other comorbidities such as end-stage organ failure, risk factors for stroke (bleeding disorders, hypercoagulable states, and carotid stenosis) were excluded. All information, including demographics, HF characteristics (ejection fraction [EF], medications taken, etc.), stroke risk factors (presence of diabetes mellitus, hypertension, smoking history, and prior myocardial infarction), and metabolic parameters, such as hemoglobin, fasting glucose, lipid (triglycerides, HDL-, LDL-, and total cholesterol), and renal profile (including blood urea nitrogen [BUN] and creatinine), as well as electrolytes (Na and K), were recorded. Information also included functional classification of heart failure based on the recommendations of the New York Heart Association (NYHA).7 All in all, a total of 293 patients (151 males, 142 females) were deemed eligible for the study.
Data analysis
Data was analyzed using the SPSS, version 16.5 (Chicago, IL, USA). Frequencies were presented as percentage (%) and continuous variables were presented as mean (standard deviation). For group and subgroup comparisons, chi-square test was done for frequencies, independent t test for normally distributed continuous variables, and Mann-Whitney U test for variables with non-Gaussian distribution. Significance set at P<.05.
RESULTS
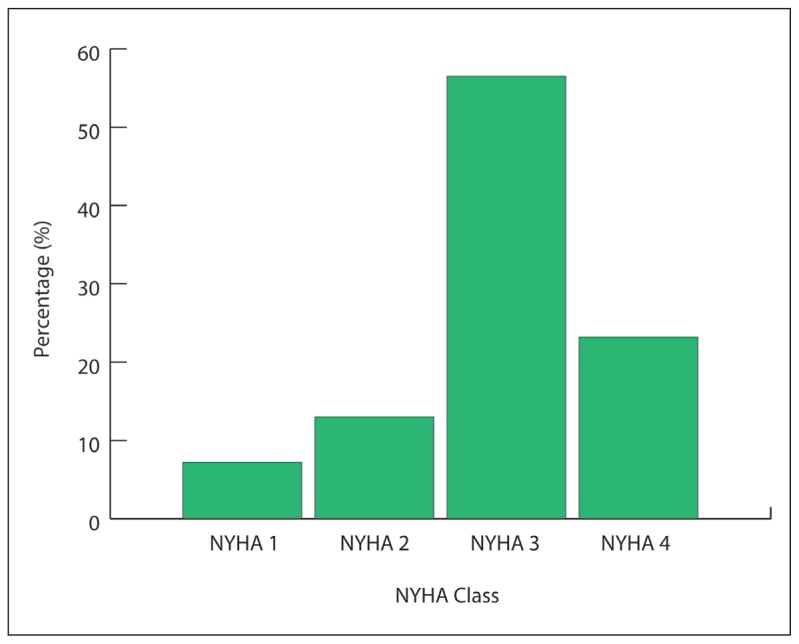
Based on the NYHA classification scheme, 25 patients (8.5%) were under class 1, 50 patients (17.1%) under class 2, 160 patients (54.6%) under class 3, and 58 patients (19.8 %) under class 4 (not shown in Table 1). Table 1 describes the general characteristics of the cohort. Out of the 293 eligible charts reviewed, 69 subjects (30.8%) had sub-sequent stroke. Those who had stroke were compared to those without, and found no significant differences in terms of demographics, heart failure characteristics, and stroke risk factors. However, when the 2 groups were compared in terms of metabolic parameters, it was found out that those who had subsequent stroke had borderline significance and higher circulating levels of total cholesterol (P=.05) and significantly higher levels of LDL-cholesterol (P=.03) as compared to those without. Table 2 shows the uniformity of findings done on stroke in Saudi Arabia from 1991 to the present study, in terms of major risk factors (hypertension and diabetes mellitus) and type of stroke (ischemic).
Table 1.
General characteristics and risk factors among HF patients with and without subsequent stroke.
| Without stroke | With stroke | P value | |
|---|---|---|---|
|
| |||
| Demographics | |||
| N | 224 | 69 | |
| Gender (M/F) | 119/105 | 32/37 | |
| Age (y) | 67.6 (12.7) | 70.8 (11.9) | .07 |
| HF characteristics | |||
| Systolic dysfunction (EF < 55%) | 167 (74.6) | 49 (71) | .64 |
| Diastolic dysfunction (EF ≥55%) | 57 (25.4) | 20 (29) | .75 |
| Documented CAD | 156 (69.6) | 53 (76.8) | .29 |
| Aspirin | 142 (63.4) | 38 (55.1) | .26 |
| Warfarin | 41 (18.3) | 8 (11.6) | .27 |
| β-blocker | 140 (62.5) | 44 (63.8) | .89 |
| ACE Inhibitor | 112 (50.0) | 40 (58.0) | .27 |
| Stroke risk factors | |||
| Diabetes mellitus | 107 (47.8) | 41 (59.4) | .10 |
| AF | 46 (20.5) | 20 (29.0) | .19 |
| Prior MI | 54 (24.1) | 10 (14.5) | .098 |
| Hypertension | 188 (83.9) | 61 (88.4) | .44 |
| Smoking | 36 (16.1) | 10 (14.5) | .85 |
| Metabolic parameters | |||
| Glucose (mmol/L) | 10.2 (5.5) | 10.8 (5.6) | .39 |
| Triglycerides (mmol/L) | 1.6 ( 0.7) | 1.7 ( 0.8) | .91 |
| Total cholesterol (mmol/L) | 3.6 (1.1) | 3.9 (1.3) | .05 |
| HDL-cholesterol (mmol/L) | 0.94 ( 0.3) | 0.98 ( 0.3) | .29 |
| LDL-cholesterol (mmol/L)a | 2.3 ( 0.9) | 2.6 ( 0.9) | .03 |
| BUN (g/dL) | 12.8 (9.5) | 14.1 (8.6) | .31 |
| Creatinine (mg/dL) | 148.9 (123.6) | 152.6 (129.7) | .83 |
| K (mmol/L) | 4.3 ( 0.7) | 4.3 ( 0.6) | .51 |
| Na (mmol/L) | 135.9(11.2) | 136.4 (7.3) | .76 |
| Hb (g/L) | 117.4 (23.1) | 111.7 25.5) | .08 |
BUN: Blood urea nitrogen, K: potassium, Na: sodium, Hb: hemoglobin, LDL: low-density lipoprotein, HDL: high-density lipoprotein, HF: heart failure, AF: atrial fibrillation, CAD: coronary artery disease, ACE: angiotensin-converting enzyme, MI: myocardial infarction, EF: Ejection fraction. Note: Data presented as frequency (%).
Continuous variable, presented as mean (SD); significant P<.05.
Table 2.
Stroke observational studies in Saudi Arabia (1991–2012).
| Study | N | Age | Major risk factor | Type |
|---|---|---|---|---|
|
| ||||
| Al-Rajeh et al, 1991 | 372 | ---- | Hypertension | Ischemic |
| Al-Rajeh et al, 1993 | 500 | 63 (17.0) | Hypertension | Ischemic |
| El Sayed et al, 1999 | 329 | 62.8 (11.1) | Hypertension + DM | Ischemic |
| Qari, 2000 | 71 | 63.0 | Hypertension | Ischemic |
| Present study, 2012 | 293 | 70.8 ( 11.9) | Hypertension + DM | Ischemic |
DM: Diabetes mellitus.
To further dissect these findings, the cohort was sub-divided into males and females, and repeated metabolic comparisons were made while adjusting for age (Table 3). The elevated circulating levels of LDL- and total cholesterol were found in female HF patients (P values .02 and .028, respectively), and this significance was absent in the male group. In the males on the other hand, BUN was significantly higher in the stroke group as compared to those without stroke (P<.04). The rest of the parameters in both genders, including glucose, other lipid parameters, renal profile markers, and electrolytes, were comparable. Furthermore, there were no apparent gender differences in terms of HF characteristics and stroke risk factors (not shown in Table 3).
Table 3.
Metabolic characteristics of male and female HF patients with and without subsequent stroke.
| Males | Females | |||
|---|---|---|---|---|
| Without stroke | With stroke | Without stroke | With stroke | |
|
| ||||
| N | 119 | 32 | 105 | 37 |
| Age (y) | 65.6 (12.9) | 71.7 (12.8) | 69.8 (12.0) | 69.9 (11.3) |
| Glucose (mmol/L) | 9.8 ( 5.5) | 10.8 ( 5.5) | 10.6 (5.5) | 10.9 (5.7) |
| Triglycerides (mmol/L) | 1.6 ( 0.7) | 1.4 ( 0.6) | 1.6 (0.7) | 1.8 (0.8) |
| Total cholesterol (mmol/L) | 3.4 ( 0.9) | 3.4 (1.1) | 3.8 (1.2) | 4.3 (1.3) * |
| HDL-cholesterol (mmol/L) | 0.9 ( 0.3) | ( 0.2) | 0.98 (0.3) | (0.3) |
| LDL-cholesterol (mmol/L) | 2.2 ( 0.8) | 2.3 ( 0.9) | 2.4 (1.0) | 2.8 (0.9) * |
| BUN (g/dL) | 12.2 ( 9.1) | 15.5 ( 8.7)a | 13.4 (9.9) | 12.9 (8.6) |
| Creatinine (mg/dL) | 158.3 (139.0) | 169.7 (120.0) | 138.1 (102.8) | 137.8 (137.4) |
| K (mmol/L) | 4.4 ( 0.7) | 4.3 ( 0.6) | 4.3 (0.8) | 4.3 (0.7) |
| Na (mmol/L) | 135.7 (6.8) | 136.8 (7.4) | 136.1 (14.7) | 136.0 (7.3) |
| Hb (g/L) | 123.2 (24.8) | 114.9 (28.6) | 111.0 (19.3) | 108.9 (22.4) |
BUN: Blood urea nitrogen, K: potassium, Na: sodium, Hb: hemoglobin, LDL: low-density lipoprotein, HDL: high-density lipoprotein, HF: heart failure, AF: atrial fibrillation.
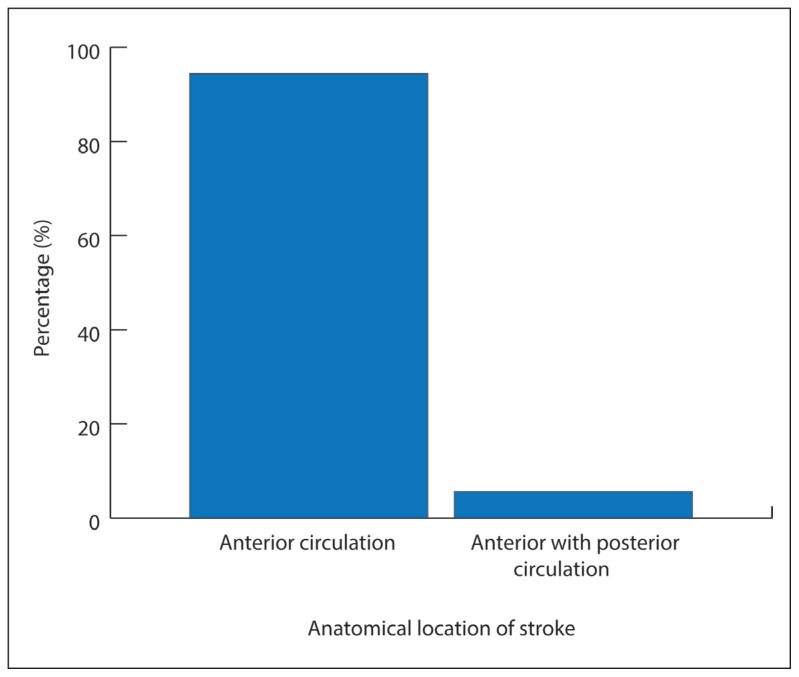
Figure 1 shows that more than half of the patients who had stroke were classified under NYHA class 3 (56.5%), with NYHA class 1 being the least (7.2%). Figure 2 shows that all patients who had stroke occurred in the anterior circulation, with only 5.6% patients having stroke both in the anterior and posterior circulation.
Figure 1.
Stroke versus NYHA functional class.
Figure 2.
Prevalence of the anatomical location of stroke.
DISCUSSION
In the present study, there was a high prevalence of associated comorbidities among the cohort, which include hypertension, diabetes mellitus, and dyslipidemia. While these diseases are age-related, it is worthy to note that these chronic noncommunicable diseases are very high in the Kingdom,4 and dyslipidemia alone is extremely high in the general Saudi population, including both children and adults.8,9 The highlights of the present study reveal gender differences in the metabolic profile of stroke among Saudi patients with heart failure, atherogenic dyslipidemia being more prominent in females and renal insufficiency more prominent in males, a finding not established in other studies of the same ethnicity. Gender differences in stroke presentation have nevertheless been demonstrated in the Caucasian populations of European and American descent and to a small extent in the Chinese population. 10–14 The evidence reveal that chronic atherogenic dyslipidemia increases the predisposition of developing early recurrent stroke in patients who already had a transient ischemic attack,15 and major adverse cardiovascular events among patients already known to harbor coronary artery disease.16 The female gender has a better metabolic profile during adolescent and premenopausal stages compared to males,17 but in the absence of menstruation (menopause), women tend to catch up men in acquiring cardiovascular risk factors, and have an even higher mortality as compared to men in the presence of diabetes mellitus.18 In the present study, women outnumbered men in encountering stroke (37 versus 32), and while both genders had an abnormal lipid profile, women had worse levels of both LDL- and total cholesterol.
Another gender difference elicited in the present study was the higher circulating levels of BUN among men who had subsequent stroke, a finding not observed among females. It is already known that BUN is a potentially powerful predictor of mortality in patients with acutely decompensated HF.11,19 The underlying renal insufficiency can also explain why patients having normal ventricular EFs with diastolic dysfunction develop CHF.20 On the relationship between renal function and stroke, it has been observed that BUN/creatinine ratio above 15 is an independent predictor of an acute ischemic stroke.21 The estimated glomerular filtration rate, however, is also a strong predictor for acute stroke, but it is more common and presents a poorer outcome in patients with hemorrhagic, rather than ischemic stroke.22 The gender difference elicited in this study needs further examination.
Other results in the present study were in accordance with other findings.23–27 There was no significant gender difference in HF medications given to patients, similar to the EuroHeart Failure Survey II 28, and while in the previous study they found a higher proportion of women having diabetes mellitus, this was not the case in the present study, probably secondary to the unequal distribution of subjects. Results from previous local studies also confirm present findings, as shown in (Table 3), with ischemic stroke being the most common type and hypertension and diabetes mellitus the most common risk factors. Worthy to note is the higher mean age of stroke presentation in the present study as compared to other studies, which could either mean improved health care over the past years, or by chance. This needs further confirmation.
The authors acknowledge several study limitations. The findings cannot be generalized for the entire population as it is a single-center study. A larger epidemiologic study is needed to confirm the findings. Furthermore, the retrospective data was limited as it did not include potential confounders such as diet and physical activity. Nevertheless, the strength of the study is its relative large sample size, and that the findings are unique, and the first to demonstrate gender differences in the presentation of Saudi HF patients with subsequent stroke.
In conclusion, the results of the present study suggest gender differences in the metabolic characteristics of Saudi HF patients with subsequent stroke on equal HF medications and stroke risk factors. While standard care is to be routinely given, a more customized approach is recommended in the overall management of these patients, paying closer attention to rehydration status and atherogenic dyslipidemic profile as early warning signs to a possible stroke in males and females, respectively.
REFERENCES
- 1.Tran J, Mirzaei M, Anderson L, Leeder SR. The epidemiology of stroke in the Middle East and North Africa. J Neurol Sci. 2010;295(1–2):38–40. doi: 10.1016/j.jns.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 2.Benamer HT, Grosset D. Stroke in Arab countries: a systemic literature review. J Neurol Sci. 2009;284(1–2):18–23. doi: 10.1016/j.jns.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Kamran S, Bener AB, Deleu D, Khoja W, Jumma M, Al Shubaili A, Inshashi J, Sharouqi I, Al Khabouri J. The level of awareness of stroke risk factors and symptoms in the Gulf Cooperation Council countries: Gulf Cooperation Council Stroke awareness study. Neuroepidemiology. 2007;29(3–4):235–42. doi: 10.1159/000112856. [DOI] [PubMed] [Google Scholar]
- 4.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yousef M, Sabico SL, Chrousos GP. Diabetes Mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (Riyadh cohort 2): a decade of an epidemic. BMC Med. 2011;9:76. doi: 10.1186/1741-7015-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alhyas L, McKay A, Balasanthiran A, Majeed A. Prevalences of overweight, obesity, hyperglycemia, hypertension and dyslipidemia in the Gulf: systematic review. JRSM Short Rep. 2011;2(7):55. doi: 10.1258/shorts.2011.011019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al Khathaami AM, Alqahtani H, Alwabel A, Alosherey N, Kojan S, Aljumah M. The status of acute stroke care in Saudi Arabia: an urgent call for action! Int J Stroke. 2011;6(1):75–6. doi: 10.1111/j.1747-4949.2010.00542.x. [DOI] [PubMed] [Google Scholar]
- 7.The Criteria Committee of the New York Heart Association. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Blood Vessels. Boston: Little Brown; 1964. [Google Scholar]
- 8.Al-Daghri NM. Extremely high prevalence of metabolic syndrome manifestations among Arab youth: a call for early intervention. Eur J Clin Invest. 2010;40(12):1063–6. doi: 10.1111/j.1365-2362.2010.02341.x. [DOI] [PubMed] [Google Scholar]
- 9.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Sabico SL, Chrousos GP. Decreasing prevalence of metabolic syndrome but a persistently high prevalence of dyslipidemia among Adult Arabs. PLoS One. 2010;5(8):e12159. doi: 10.1371/journal.pone.0012159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yesilot NF, Koyuncu BA, Coban O, Tuncay R, Bahar SZ. Gender differences in acute stroke: Istanbul medical school stroke registry. Neurol India. 2011;59(2):174–9. doi: 10.4103/0028-3886.79130. [DOI] [PubMed] [Google Scholar]
- 11.Kazory A. Emergence of blood urea nitrogen as a biomarker of neurohormonoal activation in heart failure. Am J Cardiol. 2010;106(5):694–700. doi: 10.1016/j.amjcard.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 12.Leslie-Mazwi TM, Brott TG, Brown RD, Jr, Worrall BB, Silliman SL, Case LD, Frankel MR, Rich SS, Meschia JF. Sex differences in stroke evaluations in the Ischemic Stroke Genetics Study. J Stroke Cerebrovasc Dis. 2007;16(5):187–93. doi: 10.1016/j.jstrokecerebrovasdis.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith MA, Lisabeth LD, Brown DL, Morgenstern LB. Gender somparisons of diagnostic evaluation for ischemic stroke patients. Neurology. 2005;65(6):855–8. doi: 10.1212/01.wnl.0000176054.72325.0f. [DOI] [PubMed] [Google Scholar]
- 14.Huang Y, Wang JG, Wei JW, Headley AP, Wong LK, Heeley EL, Arima H, Sun J, Li Q, Liu M, Li Z, Wu L, Cheng Y, Huang Q, Zhang S, Xu E, Yang Q, Lu C, Anderson CS CH inaQUEST Investigators. Age and gender variations in the management of ischaemic stroke in China. Int J Stroke. 2010;5(5):351–9. doi: 10.1111/j.1747-4949.2010.00460.x. [DOI] [PubMed] [Google Scholar]
- 15.Sirimarco G, Deplanque D, Lavallee PC, Labreuche J, Mesequer E, Cabrejo L, Guidoux C, Olivot JM, Abboud H, Laperque B, Klein IF, Maziqhi M, Touboul PJ, Bruckert E, Amarenco P. Atherogenic dyslipidemia in patients with transient ischemic attack. Stroke. 2011;42(8):2131–7. doi: 10.1161/STROKEAHA.110.609727. [DOI] [PubMed] [Google Scholar]
- 16.Arca M, Montali A, Valiante S, Campagna F, Pigna G, Paoletti V, Antonini R, Barilla F, Tanzilli G, Vestri A, Gaudio C. Usefulness of atherogenic dyslipidemia for predicting cardiovascular risk in patients with angiographically defined coronary artery disease. Am J Cardiol. 2007;100(10):1511–6. doi: 10.1016/j.amjcard.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 17.Barrett-Connor E. Sex differences in coronary heart disease. Why are women so superior? The 1995 Ancel Keys Lecture. Circulation. 1997;95(1):252–64. doi: 10.1161/01.cir.95.1.252. [DOI] [PubMed] [Google Scholar]
- 18.Mercuro G, Deidda M, Piras A, Dessalvi CC, Maffei S, Rosano GM. Gender determinants of cardiovascular risk factors and diseases. J Cardiovasc Med (Hagerstoen) 2010;11(3):207–20. doi: 10.2459/JCM.0b013e32833178ed. [DOI] [PubMed] [Google Scholar]
- 19.Cauthen CA, Lipinski MJ, Abbate A, Appleton D, Nusca A, Varma A, Goudreau E, Cowley MJ, Vetrovec GW. Relation of blood urea nitrogen to long-term mortality in patients with heart failure. Am J Cardiol. 2008;101(11):1643–7. doi: 10.1016/j.amjcard.2008.01.047. [DOI] [PubMed] [Google Scholar]
- 20.Victor BM, Barron JT. Diastolic heart failure versus diastolic dysfunction: difference in renal function. Clin Cardiol. 2010;33(12):770–4. doi: 10.1002/clc.20824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin LC, Yang JT, Weng HH, Hsiao CT, Lai SL, Fann WC. Predictors of early clinical deterioration after acute ischemic stroke. Am J Emerg Med. 2011;29(6):577–81. doi: 10.1016/j.ajem.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 22.Hao Z, Wu B, Lin S, Kong FY, Tao WD, Wang DR, Liu M. Association between renal function and clinical outcome in patients with acute stroke. Eur Neurol. 2010;63(4):237–42. doi: 10.1159/000285165. [DOI] [PubMed] [Google Scholar]
- 23.Al-Rajeh S, Awada A, Niazi G, Larbi E. Stroke in a Saudi Arabian National Guard community. Analysis of 500 consecutive cases from a population-based hospital. Stroke. 1993;24(11):1635–9. doi: 10.1161/01.str.24.11.1635. [DOI] [PubMed] [Google Scholar]
- 24.Al-Rajeh S, Larbi E, Bademosi O, Awada A, Ismail H, Al-Freihi H, Al-Ghassab G. Stroke in a tertiary hospital in Saudi Arabia: a study of 372 cases. Eur Neurol. 1991;31(4):251–6. doi: 10.1159/000116685. [DOI] [PubMed] [Google Scholar]
- 25.El Sayed MM, Adeuja AO, El-Nahrawy E, Olaish MA. Characteristics of stroke in Hofuf, Saudi Arabia. Ann Saudi Med. 1999;19(1):27–31. doi: 10.5144/0256-4947.1999.27. [DOI] [PubMed] [Google Scholar]
- 26.Qari F. Profile of stroke in a teaching university hospital in the western region. Saudi Med J. 2000;21(11):1030–3. [PubMed] [Google Scholar]
- 27.Caso V, Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, Micheli S, Bertolani L, Venti M, Palmerini F, Billeci AM, Corni G, Previdi P, Silvestrelli G. Gender differences in patients with acute ischemic stroke. Women’s Health (Lond Engl) 2010;6(1):51–7. doi: 10.2217/whe.09.82. [DOI] [PubMed] [Google Scholar]
- 28.Nieminen MS, Harjola VP, Hochadel M, Drexier H, Komajada M, Brutsaert D, Dickstein K, Ponikowski P, Tavazzi L, Foliath F, Lopez-Sendon JL. Gender related differences in patients presenting with acute heart failure. Results from Euroheart Failure Survey II. Eur Heart J. 2008;10(2):140–8. doi: 10.1016/j.ejheart.2007.12.012. [DOI] [PubMed] [Google Scholar]