Abstract
BACKGROUND AND OBJECTIVES
Injury to the head is the most common affected body part in pediatric trauma and could be associated with deleterious consequences. It presents a challenge for developing countries since many injuries are preventable and there are few epidemiological data to support injury prevention programs. The current study aimed to determine demographic characteristics, etiology and outcome of head injury in the pediatric population and compare findings to international figures.
DESIGN AND SETINGS
Retrospective review of consecutive cases registered in major trauma center database, Riyadh, from 2001 to 2009.
PATIENTS AND METHODS
The database registry was limited to hospitalized patients following injury. Any head injury in a patient ≤18 years was included.
RESULTS
Of 3796 patients identified, 1219 patients (32.1%) suffered head injury (mean age 8.6 years; males 78.4%). Children under 12 years comprised 66.3%. Motor vehicle crash (MVC) was the commonest cause (34.2%), followed by pedestrian injury (30.3%) and falls (28.4%). When stratified by age, falls (45.6%) were the most common etiology under 6 years while MVC was the leading cause in high school students (74.4%). The latter group had the lowest mean (SD) Glascow coma scale scores ( 8.58 [4.7]), highest mean injury severity scale scores (23.4 [21]), highest rate of craniotomy (7%) and highest mortality (20%).
CONCLUSION
One third of pediatric trauma requiring hospital admission suffered head injury. Preschoolers and elementary school students were mostly affected. The striking incidence of pedestrian and fall injuries call for organized national prevention programs. Additionally, more attention should be directed to reduce MVC among high school students given their comparative high rate of severe injuries and deaths following trauma.
Head injury is a major cause of mortality, morbidity and disability in children.1–4 In the US, severe head injury constituted around 7.4% of total injury of patients less than 14 years.5 Although infectious disease may predominate in many developing countries as a major cause of morbidity and mortality, injuries and deaths from motor vehicle crash (MVC)-related head injuries are becoming more frequent.6,7 Saudi Arabia is no exception, given the rapid economic growth of the country.8 The resultant morbidity and mortality create an enormous socioeconomic burden.9,10 Research towards injury etiology and risk factors remained the key factor leading to any successful prevention program.1 Globally, children constitute only 33.3% of the world population, but the great majority (88.7%) of these children live in developing countries.11,12 A unifying characteristic of developing countries is the immaturity of injury prevention programs.10,13,14 In addition, many essential trauma health care support services such as pre-hospital care, hospital-to-hospital transport services, and a clear designation of regional trauma centers are still developing in these countries.15 Given these critical differences in health services, we feel that data pertaining to injury prevalence and risk factors acquired from developed countries might not be the best source to inform decisions of policy makers. Moreover, outcomes data acquired from settings such as those in developing countries, with the aforementioned limitations, would be more relevant so long as in-hospital care is analogous to what is standard in developed nations.
In the current study, it was our primary goal to describe the demographics and causes of head injury in children of 18 years of age and younger in a major trauma referral hospital and academic center in Riyadh, Saudi Arabia. Our secondary objectives were to examine the severity of head injury, overall trauma severity, types of surgical interventions for involved cases, the influence of patient body weight on the injury status, and the pattern of outcome for those injuries. Such analysis would be valuable to shed light on this significant problem in this part of the developing world and could serve as a cornerstone for initiation of injury prevention programs in developing nations.
METHODS
This was a retrospective cohort study that included all trauma cases, from May 2001 to March 2009, who were included in the King Abdulaziz Medical City Trauma Registry (KAMC-TR), and were diagnosed with head injury. The KAMC-TR is a prospectively recorded database of all trauma patients admitted to the center. A full-time data registrar collects data and longitudinally follows patients from the time of admission until the final disposition. For quality assurance purposes, an annual audit of 5% of the data is undertaken through medical records. Furthermore, to assure complete capture of all cases, a daily report from medical records is generated of all discharged trauma patients and is cross checked against the abstracted charts. Data collected include variables pertaining to demographics, mechanism of injury, resuscitation variables, in-hospital treatment variables and final in-hospital outcomes. Post-discharge visits are not captured in the database nor are patients who receive their treatment in the emergency department and who do not require in-hospital admission. Institutional ethics board approval was obtained prior to the commencement of the study.
From a public health perspective, we conducted this study in the city of Riyadh, which is home to 5.8 million residents comprising 24.1% of the country’s population. 11 The median age of the Saudi population is 21 years and children under the age of 19 comprise 41.7% of the total population.11 Major traumas get transferred to a trauma center based on their location. King Abdulaziz Medical city (KAMC), where the study was conducted, is one the trauma referrals centers in Riyadh.
All consecutive patients at 18 years and younger who were identified through the KAMC-TR with a diagnosis of head injury were included. Descriptive data including age, gender, location and mechanism of injury were abstracted. Patients were stratified according to their age at the time of head injury into four groups: patients under 6, those in elementary school (6 to <12 years), those in intermediate school (12 to <16 years) and high school children (16 to 18 years). We also abstracted data pertaining to in-hospital outcomes of the head injuries such as death, severe disability, need for craniotomy, need for critical care, length of stay in the critical care unit and the overall length of stay in the hospital.
The overall injury severity was assessed using the injury severity score (ISS). Several studies have confirmed the validity of the ISS as a predictor of mortality and length of hospital stay.13 Glasgow Coma Scale (GCS) was used as a measure of the severity of head injury. Both GCS and ISS were considered at the time of presentation to the emergency department. Both measures have been shown to provide a valid assessment of the outcome of multiple trauma patients with head injuries.14
Descriptive statistics in the form of mean and standard deviation were provided. Categorical variables were analyzed using the chi-square test. ANOVA was calculated for multiple groups with continuous variables. The level of significance was set at P value <.05. Data were analyzed using SPSS software (release 17.0; SPSS, IBM, Armonk, NY).
RESULTS
During the 8 years study period, 8941 patients were identified from our trauma database; 3796 (42.5%) were 18 years and younger, of whom, 1219 (32.1%) patients were diagnosed with head injury. The mean age of patients was 8.6 years (range 1 month to 18 years). Children under 12 years comprised 66.3% of the cohort (Table 1). Males were more affected than females (78.4% vs. 21.6%, ratio 3.6:1). The weight of the patients was available for individuals younger than 12 year of age. The mean overall patient weight was 8.8 kg (range 2.5–77 kg). The mean patient weight of children younger than 6 years was 13.2 (5.2) kg while it was 27.0 (9.6) kg for those between 6 to <12 years. The overall weight of the patients was negatively correlated with GCS (r=−0.128, P<.001), and positively correlated with both ISS (r=0.138, P<.001) and length of stay (LOS, r=0.128, P<.001). When stratified by age groups, the mean weight of those less than 6 years was negatively correlated with GCS (r=−0.158, P=.001) and only approached a statistically significant correlation with ISS (r=0.082, P=.059) and LOS (r=0.08, P=.064). Considering the group between 6 to <12 years, the mean weight of the patients was only statistically correlated with LOS (r=0.097, P=.049).
Table 1.
Patient characteristics by age groups.
| Age group (years) | Number (%) | Craniotomy (%) | Average length of hospital stay (days) |
|---|---|---|---|
|
| |||
| <6 | 444 (36.4) | 2.7 | 16.6 |
| 6–11.9 | 364 (29.9) | 3.8 | 21.9 |
| 12–15.9 | 184 (15.1) | 4.9 | 27.7 |
| 16–18 | 227 (18.6) | 7 | 39.2 |
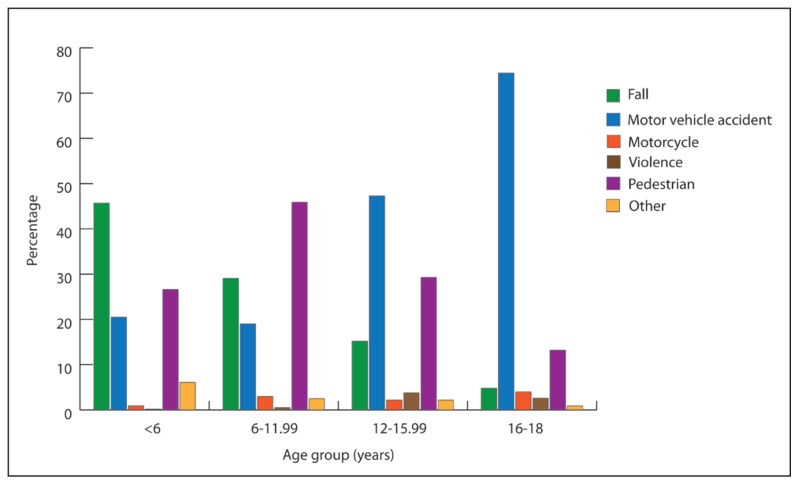
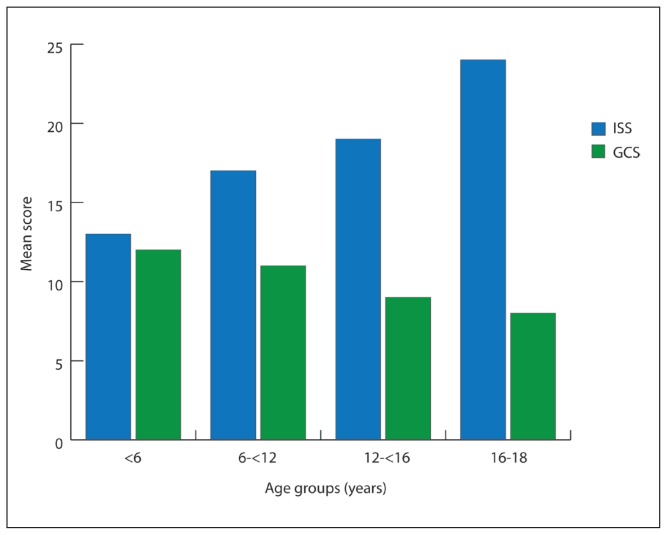
Overall, motor vehicle crash (MVC) was the leading cause of head injury (34.2%), followed by pedestrian injuries (30.3%), falls (28.4%), motorcycle crash (2.3%), violence (1.4%), and others (3.4%). The mechanism of injury was different according to the age group. While falls was the leading cause of head injury in patients less than 6 years (45.9%), pedestrian-related injuries were the most common (45.9%) between 6 to 12 years, and MVC was the leading mechanism of head injuries in the age groups of 12–16 and 16–18 (47.2% and 74.4% respectively) (Figure 1). The mean ISS for our cohort was 16.6 (range 1 to 75) and the median GCS was 11 (range 3 to 15). Across the four age strata there was a trend towards increasing severity of injury with increasing age, which was accompanied by an inverse drop in GCS (P<.0001) (Figure 2).
Figure 1.
Mechanism of injury stratified by age groups.
Figure 2.
Mean Injury Severity Score (ISS) and Glasgow Coma Score (GCS) at presentation to the emergency department stratified by different age groups.
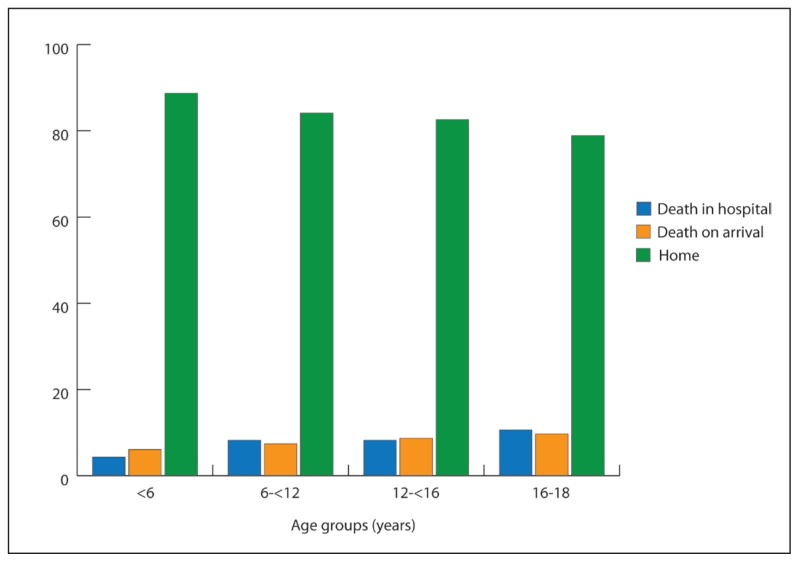
Following assessment and resuscitation in the emergency department, 7.5% died, 33.6% were admitted to the critical care unit, and a smaller number (6.3%) went to the operating room for various procedures. Only 4.2% of the total population underwent a craniotomy procedure. Craniotomies were most common in the high school age group 16–18 years (7%) compared to other age groups. This difference approached statistical significance (P=.059). There was no gender difference in number of craniotomies (4.2% each). The overall mean LOS was 24.2 days (range 1–1681 days). Expectedly, older children—who on average sustained more severe injuries—stayed longer in the hospital as compared to younger children (Table 1). The majority of patients (84.6%) were discharged home. The overall mortality rate was 14.7%; half died on arrival. Only 0.3% was transferred to other hospitals. When stratified by age, 1 in every 5 patients within the age group 16–18 years died (Figure 3).
Figure 3.
Hospital disposition stratified by age groups. DOA: Death on Arrival. ISS: injury severity score. GCS: Glasgow coma scale.
DISCUSSION
Head injury is the most affected body region in pediatric trauma.3,16–20 It was the commonest injury (65%) among children with ISS>11 following trauma in a report from eastern Ontario, Canada.16 Additionally, earlier reports by Ivan et al showed a head injury rate of 8.8% among pediatric emergency admissions in a Canadian trauma center.17 The estimated population incidence of traumatic brain injury in the US was 73.5/100 000.18 However, it is variable and may go up to 300/100 000 depending on the study methodology and the area of reporting.18 In Norway, Brudvik reported that head injuries were commonest among the youngest children (51%) while upper extremity injury was commonest in school children.19 Comparable data from the developing world are few. Head injury constituted 4.75% of all cases in the emergency department in a hospital based study in Malaysia.20 In the report by Adesunkanmi et al from Nigeria, including road traffic crashes involving children, head injury was found to be the commonest mode of injury.7 The current report is the largest from the developing world and it demonstrates that one-third of pediatric admissions following trauma suffered head injury. This has direct implications for decision-making in developing countries where public health issues are similar to Saudi Arabia, particularly due to the paucity of well-organized injury prevention programs.
Predictors associated with sustaining a head injury in our study were male gender, age under 12 years, and MVC. The mean age of patients who sustained head injury was 8.6 years. This correlates with other observational studies.8,10 The male dominance was also consistent with other reports from Saudi and worldwide.8,17,21 MVC was the major cause of injury (34.1%) in the current study as well as in previous reports from Saudi Arabia and the developing world.9,10,16,22,23 Additionally, the variability in the mechanism of injury with age (Figure 1) is consistent with previously published reports. While falls tends to predominate in the younger age group, vehicle crashes tend to affect older children and teenagers. This could be attributed to underage driving, inappropriate driver licensing and tendency for high speed and reckless driving in this age group.10
Falls accounted for a large percentage of pediatric traumas in our study and in others.24 Such predilection could be partly explained by the immature cognitive, perceptual and judgmental abilities of the younger age group.25 Furthermore, this underscores the importance of safe environments for playing outdoors for instance. Municipalities should pay more attention to providing safe parks where children can play, which are found more in the developed world.
Pedestrian injuries represent a challenge to the developing world. The current study demonstrated that pedestrian injuries were only slightly preceded by MVC (30% vs. 34% respectively). It was the commonest in the age group between 6 and those younger than 12 years of age. A similar finding was previously published from different parts of the developing world.7,20 Some of these could be attributed to the lack of direct adult supervision. 20 Additionally, studies have shown that children have behavioral and cognitive limitations and they lack essential knowledge about safety.26 Hence the need for more effective educational injury prevention programs like “think first” and “safe kids” in the developing world that takes in consideration the epidemiology of injuries in these regions.
Obesity was shown to be associated with worse injury, more pulmonary complications, prolonged ICU stay, and higher mortality in several reports.27–30 In the study by Pomerantz et al, obese individuals had worse lower extremity injury while fewer face and head injuries. 30 This finding was similar to other studies.27–29 Our data correspond to previous reports in showing an increased association of obesity with worse injury severity and prolonged length of hospital stay. Additionally, obesity was associated with worse head injuries, which could be attributed to the high incidence of MVC in the current study.
Our study has several limitations. First, the retrospective nature of this review renders it susceptible to multiple biases such as information biases. Although the mechanism of data collection, data cleaning, and quality control of our trauma database are on par with similar databases, biases associated with retrospective analyses cannot be ignored. Secondly, this is a hospital-based study and as such referral bias could be important. To best inform policy maker’s decisions, population-based data are needed. However, this study documents at least a diluted account of the head injury reality in our city. Thirdly, since the database included patients who were admitted to the hospital or who died in the emergency department, “milder” head injuries that did not require admission could be missed.
Head injuries comprise approximately one-third of hospital pediatric trauma admission to the trauma center. The factors that correlated with head injuries in children include male sex, age less than 12 years, and motor vehicle crashes. Nationwide measures toward injury prevention are required to enhance the use of seat belts and helmets and provide education against dangerous driving practices. Further population-based data are needed in our country and similar emerging economies to help inform policy makers and influence change.
REFERENCES
- 1.MacKenzie EJ. Epidemiology of injuries: current trends and future challenges. Epidemiol Rev. 2000;22(1):112–9. doi: 10.1093/oxfordjournals.epirev.a018006. [DOI] [PubMed] [Google Scholar]
- 2.Ciastko AR. Head injuries in childhood. Can Med Assoc J. 1983 Sep 15;129(6):532. [PMC free article] [PubMed] [Google Scholar]
- 3.Lam WH, MacKersie A. Paediatric head injury: incidence, aetiology and management. Paediatr Anaesth. 1999;9(5):377–85. doi: 10.1046/j.1460-9592.1999.00431.x. [DOI] [PubMed] [Google Scholar]
- 4.Gofin R, Adler B, Hass T. Incidence and impact of childhood and adolescent injuries: a population-based study. J Trauma. 1999 Jul;47(1):15–21. doi: 10.1097/00005373-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Demetriades D, Murray J, Martin M, Velmahos G, Salim A, Alo K, et al. Pedestrians injured by automobiles: relationship of age to injury type and severity. J Am Coll Surg. 2004 Sep;199(3):382–7. doi: 10.1016/j.jamcollsurg.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 6.Abantanga FA, Mock CN. Childhood injuries in an urban area of Ghana a hospital-based study of 677 cases. Pediatr Surg Int. 1998 Sep;13(7):515–8. doi: 10.1007/s003830050387. [DOI] [PubMed] [Google Scholar]
- 7.Adesunkanmi AR, Oginni LM, Oyelami OA, Badru OS. Road traffic accidents to african children: assessment of severity using the injury severity score (ISS) Injury. 2000 May;31(4):225–8. doi: 10.1016/s0020-1383(99)00236-3. [DOI] [PubMed] [Google Scholar]
- 8.Crankson SJ. Motor vehicle injuries in childhood: a hospital-based study in Saudi Arabia. Pediatr Surg Int. 2006 Aug;22(8):641–5. doi: 10.1007/s00383-006-1715-7. [DOI] [PubMed] [Google Scholar]
- 9.Tamimi TMDM, Bhatty MA, et al. Causes and types of road injuries in Asir Province, Saudi Arabia, 1975–1977: Preliminary study. Saudi Med J. 7 [Google Scholar]
- 10.Kapp C. WHO acts on road safety to reverse accident trends. Traffic accidents kill 1.26 million people each year; 2nd leading cause of death among those aged 15–29. Lancet. 2003 Oct 4;362(9390):1125. doi: 10.1016/s0140-6736(03)14501-1. [DOI] [PubMed] [Google Scholar]
- 11.Central Department for Statistics and Information. Annual Statistical Books. 2007. [cited 2009 31 July]; Available from: http://www.cdsi.gov.sa/showsection.aspx?lid=26&id=318.
- 12.UNICEF. Statistics and monitoring. [cited 200930 July]; Available from: http://www.unicef.org/statistics/index_step1.php.
- 13.Parker SZB, Augustyn M. Developmental and behavioral pediatrics: a handbook for primary care. Second ed. Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 14.Central Department for Statistics and Information. Annual Statistical Books. 2007. Available from: http://www.cdsi.gov.sa/showsection.aspx?lid=26&id=318.
- 15.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974 Mar;14(3):187–96. [PubMed] [Google Scholar]
- 16.Osmond MH, Brennan-Barnes M, Shephard AL. A 4-year review of severe pediatric trauma in eastern Ontario: a descriptive analysis. J Trauma. 2002 Jan;52(1):8–12. doi: 10.1097/00005373-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Ivan LP, Choo SH, Ventureyra EC. Head injuries in childhood: a 2-year survey. Can Med Assoc J. 1983 Feb 1;128(3):281–4. [PMC free article] [PubMed] [Google Scholar]
- 18.Reid SR, Roesler JS, Gaichas AM, Tsai AK. The epidemiology of pediatric traumatic brain injury in Minnesota. Arch Pediatr Adolesc Med. 2001 Jul;155(7):784–9. doi: 10.1001/archpedi.155.7.784. [DOI] [PubMed] [Google Scholar]
- 19.Brudvik C. Child injuries in Bergen, Norway. Injury. 2000 Dec;31(10):761–7. doi: 10.1016/s0020-1383(00)00093-0. [DOI] [PubMed] [Google Scholar]
- 20.Rohana J, Ong LC, Abu Hassan A. Epidemiology of head injury in Malaysian children: a hospital-based study. Med J Malaysia. 1998 Sep;53(3):217–22. [PubMed] [Google Scholar]
- 21.Rickels E, von Wild K, Wenzlaff P. Head injury in Germany: A population-based prospective study on epidemiology, causes, treatment and outcome of all degrees of head-injury severity in two distinct areas. Brain Inj. 2010;24(12):1491–504. doi: 10.3109/02699052.2010.498006. [DOI] [PubMed] [Google Scholar]
- 22.Feickert HJ, Drommer S, Heyer R. Severe head injury in children: impact of risk factors on outcome. J Trauma. 1999 Jul;47(1):33–8. doi: 10.1097/00005373-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Emejulu JK, Shokunbi MT. Aetiological patterns and management outcome of paediatric head trauma: one-year prospective study. Niger J Clin Pract. 2010 Sep;13(3):276–9. [PubMed] [Google Scholar]
- 24.Mazurek AJ. Epidemiology of paediatric injury. J Accid Emerg Med. 1994 Mar;11(1):9–16. doi: 10.1136/emj.11.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tabish A, Lone NA, Afzal WM, Salam A. The incidence and severity of injury in children hospitalised for traumatic brain injury in Kashmir. Injury. 2006 May;37(5):410–5. doi: 10.1016/j.injury.2006.01.039. [DOI] [PubMed] [Google Scholar]
- 26.Gresham LS, Zirkle DL, Tolchin S, Jones C, Maroufi A, Miranda J. Partnering for injury prevention: evaluation of a curriculum-based intervention program among elementary school children. J Pediatr Nurs. 2001 Apr;16(2):79–87. doi: 10.1053/jpdn.2001.23148. [DOI] [PubMed] [Google Scholar]
- 27.Brown CV, Neville AL, Rhee P, Salim A, Velmahos GC, Demetriades D. The impact of obesity on the outcomes of 1,153 critically injured blunt trauma patients. J Trauma. 2005 Nov;59(5):1048–51. doi: 10.1097/01.ta.0000189047.65630.c5. discussion 51. [DOI] [PubMed] [Google Scholar]
- 28.Brown CV, Neville AL, Salim A, Rhee P, Cologne K, Demetriades D. The impact of obesity on severely injured children and adolescents. J Pediatr Surg. 2006 Jan;41(1):88–91. doi: 10.1016/j.jpedsurg.2005.10.012. discussion 88–91. [DOI] [PubMed] [Google Scholar]
- 29.Boulanger BR, Milzman D, Mitchell K, Rodriguez A. Body habitus as a predictor of injury pattern after blunt trauma. J Trauma. 1992 Aug;33(2):228–32. doi: 10.1097/00005373-199208000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Pomerantz WJ, Timm NL, Gittelman MA. Injury patterns in obese versus nonobese children presenting to a pediatric emergency department. Pediatrics. 2010 Apr;125(4):681–5. doi: 10.1542/peds.2009-2367. [DOI] [PubMed] [Google Scholar]