Abstract
Acute methanol intoxication is not an unusual poisoning. It can have serious neurological sequelae. We emphasize how neuroimaging can help in distinguishing methanol poisoning from other causes of acute unconsciousness in alcoholic patients such as hypoglycemic brain damage and carbon monoxide poisoning or head injury, which are frequently observed in alcoholic patients and are also responsible for altered sensorium. The most important findings in MR brain imaging in methanol poisoning have been bilateral putaminal hemorrhagic necrosis. Other less common findings are subcortical and deep white matter lesions, cerebral and cerebellar cortical lesions, and midbrain lesions, cerebral and intraventricular hemorrhage, and even enhancement of necrotic lesions, we found almost the entire spectrum of MRI findings in this patient with methanol poisoning. Neurological sequelae can entail the course and prognosis in methanol poisoning. The patient died because of ventilator-associated pneumonia that developed in the course of prolonged hospitalization.
Acute methanol intoxication, which can occur as accidental or suicidal ingestion, is not an unusual poisoning. However, in developing countries adulteration of ethanol is a most common cause of methanol intoxication. Patients generally present with acute neurological, visual, and gastrointestinal symptoms. 1 Brain MRI findings have been characteristic in methanol poisoning; bilateral putaminal hemorrhage is the most common finding. Brain MRI is seldom done in methanol poisoning; its significance lies when the patient remains in a state of altered sensorium even after the correction of metabolic parameters or when the patient’s condition deteriorates after having a period of improvement. MRI may be helpful in differentiating acute methanol intoxication from other conditions like hypoglycemic brain damage and head injury that can coexist or confound methanol intoxication and also lead to altered sensorium.
CASE
A 30-year-old alcoholic man was brought in with altered sensorium. He had a history of acute alcohol intake 6 hours prior to the presentation. On examination, his breathing pattern was of the Kussmaul type, and other findings were found normal on chest and cardiovascular system examination. On neurological examination, the Glasgow Coma Scale was 11, and no focal deficit was revealed. An arterial blood gas analysis that showed a high anion gap metabolic acidosis. The provisional diagnosis of acute methanol intoxication was suspected and a blood sample was sent for measuring the methanol level, which was high (27 mg/dL). Ethanol was given through a Ryle’s tube at 0.8 to 1 mL/kg of 95% as a loading dose and 0.21 mL/kg of 95% as a maintenance dose. Leucovorin and folic acid were also given: (leucovorin 1 mg/kg intravenously followed by folic acid 1 mg/kg every 4 hours for 6 doses). Ventilatory support was given to the patient to maintain respiration. The patient was weaned off from ventilatory support on day 5, but his sensorium did not improve. An MRI was done on the sixth day, which revealed subacute hemorrhage involving periventricular white matter, putamen, external capsule, and a superior cerebellar peduncle on both sides with a surrounding edema leading to compression over the lateral ventricles (Figure 1). The patient developed ventilator-associated pneumonia and died on the 30th day after admission.
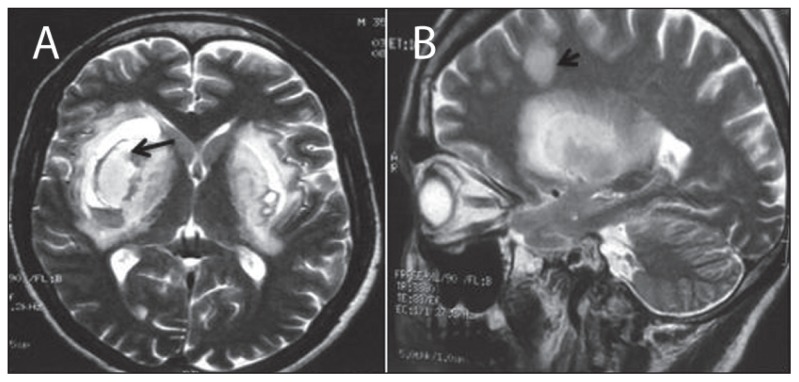
Figure 1.
A) Axial T2W gradient recalled echo image showing bilateral putaminal hemorrhage as hypointense areas due to susceptibility artefacts (arrow), B) left parasaggital T2W image shows ovoid subcortical and deep white matter lesion along with putaminal necrosis (arrow).
DISCUSSION
Acute methanol intoxication may be life threatening or can cause a permanent neurological deficit. The interval between the ingestion and the appearance of symptoms are correlated with the volume of methanol ingested and the amount of ethanol concomitantly ingested; a competitive inhibition exists between the two.2 Methanol itself causes an initial intoxication, whereas the permanent neurological sequelae are caused by its metabolites, mainly formic acid. Formic acid also causes a serious metabolic acidosis after a period of 12 to 24 hours.3–5 Central nervous system symptoms in the acute phase are common and include vomiting, nausea, dizziness, headache, and visual disturbances.4 Neuroimaging helps in distinguishing methanol poisoning from other causes of acute unconsciousness in alcoholic patients such as hypoglycemic brain damage and carbon monoxide poisoning or head injury. MRI findings in methanol poisoning are characteristic and include hemorrhagic putaminal necrosis (most common), subcortical and deep white matter lesions, cerebral and cerebellar cortical lesions, and midbrain lesions, cerebral and intraventricular hemorrhage, and even enhancement of necrotic lesions.1,4–7 Basal ganglia involvement is likely because of the direct effect of methanol metabolites and the selective vulnerability of the basal ganglia to acidosis, as compared to the rest of the brain. Selective basal ganglia and white matter lesions are not specific to methanol intoxication and can be seen in hepatolenticular degeneration, carbon monoxide poisoning, hypoxic-ischemic insult, and Leigh disease.6 The mechanism by which the methanol causes toxicity to the visual system is not well understood. Formic acid, the toxic metabolite, is responsible for ocular toxicity in animal models. Therefore, the myelinoclastic effect of formic acid is presumed to be responsible for optic nerve lesions or axonal loss in humans. 4 Our case showed almost the entire spectrum of MRI findings seen in methanol poisoning. The patient was in an unconscious state when he presented and only the history of being intoxicated with alcohol was forth-coming. Ethyl alcohol-intoxicated patients have a presentation similar to methanol ingestion; they can only be differentiated by measuring the level of methanol in the blood. MRI is another means by virtue of its characteristic findings in methanol poisoning, which can narrow down the possibilities that are usually encountered dealing with patients with alcohol intoxication such as hypoglycemic brain damage and head injury. In methanol intoxication, putaminal necrosis is usually permanent; however, in some series, significant regression of the neurological findings and disappearance of extrapyramidal symptoms are reported.8 The prognosis correlates with the amount of methanol consumed and the subsequent degree of metabolic acidosis. This is further dependent on the amount of formic acid that has accumulated in the blood.
REFERENCES
- 1.Halavaara J, Valanne L, Setala K. Neuroimaging supports the clinical diagnosis of methanol poisoning. Neuroradiology. 2002;44:924–8. doi: 10.1007/s00234-002-0855-2. [DOI] [PubMed] [Google Scholar]
- 2.Rathi M, Sakhuja V, Jha V. Visual blurring and metabolic acidosis after ingestion of bootlegged alcohol. Hemodial Int. 2006 Jan;10(1):8–14. doi: 10.1111/j.1542-4758.2006.01169.x. [DOI] [PubMed] [Google Scholar]
- 3.Kuteifan K, Oesterle H, Tajahmay T, Gutbub AM, Lapatte G. Necrosis and heamorrhage of the putamen in methanol poisoning shown on MRI. Neuroradiology. 1998;40:158–160. doi: 10.1007/s002340050558. [DOI] [PubMed] [Google Scholar]
- 4.Hsu HH, Chen CY, Chen FH, Lee CC, Chou TY, Zimmerman RA. Optic atrophy and cerebral infarcts caused by methanol intoxication: MRI. Neuroradiology. 1997;39:192–194. doi: 10.1007/s002340050391. [DOI] [PubMed] [Google Scholar]
- 5.Rubinstein D, Escott E, Kelly JP. Methanol intoxication with putaminal and white matter necrosis: MR and CT findings. AJNR. 1995;16:1492–1494. [PMC free article] [PubMed] [Google Scholar]
- 6.Sefidbakht S, Rasekhi AR, Kamali K, Borhani Haghighi A, Salooti A, Meshksar A, et al. Methanol poisoning: Acute MR and CT findings in nine patients. Neuroradiology. 2007;49:427–35. doi: 10.1007/s00234-007-0210-8. [DOI] [PubMed] [Google Scholar]
- 7.Blanco M, Casado R, Vazquez F, Pumar JM. CT and MR imaging findings in methanol intoxication. AJNR Am J Neuroradiol. 2006 Feb;27(2):452–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Hantson P, Duprez T, Mahieu P. Neurotoxicity to the basal ganglia shown by magnetic resonance image (MRI) following poisoning by methanol and other substances. J Toxicol Clin Toxicol. 1997;35:151–61. doi: 10.3109/15563659709001186. [DOI] [PubMed] [Google Scholar]