Abstract
Rationale:
We report a rare case of syphilitic meningomyelitis presenting with visceral crisis and possessing characteristic imaging findings.
Patient concerns:
The patient, a 50-year-old woman, complained of pain in the upper abdomen and back. She then developed numbness in both lower extremities and weakness in the left lower limb.
Diagnosis:
Magnetic resonance imaging (MRI) of the spinal cord revealed the candle guttering sign and irregular enhancement at the T6 level. Rapid plasma reagin test of the cerebrospinal fluid yielded a titer of 1:8. Thus, the patient was diagnosed with syphilitic meningomyelitis.
Interventions:
She was treated with ceftriaxone and dexamethasone after the failure of penicillin treatment.
Outcomes:
She could perform the activities of daily living, and her pain completely disappeared.
Lessons:
A patient with syphilitic meningomyelitis can present with visceral crisis caused by the involvement of the posterior nerve roots or the posterior horn, which usually occurs in patients with tabes dorsalis. Considering the non-specific symptoms and MRI features, we should be aware that abdominal pain may be a symptom of myelopathy, and syphilitic meningomyelitis ought to be taken into account in a patient with longitudinally extensive myelitis.
Keywords: syphilitic meningomyelitis, visceral crisis, abdominal pain, candle guttering sign
1. Introduction
Treponema pallidum subspecies pallidum is the causative agent of syphilis. This spirochete mainly spreads through sexual contact and blood transmission. Within a few days of infection, the organism can invade the central nervous system (CNS), and neurosyphilis can develop at any time during the course of the disease.[1] Therefore, when treating patients with syphilis, the clinician must rule out the involvement of other organs and especially of the CNS. Here, we present a rare case of syphilitic meningomyelitis that presented with visceral crisis. Neurologic symptoms appeared later on, and characteristic findings on magnetic resonance imaging (MRI) and serologic tests helped confirm the diagnosis. The Ethics Committee of the First Hospital of Jilin University approved the study. The patient has provided informed consent for publication of the case.
2. Case report
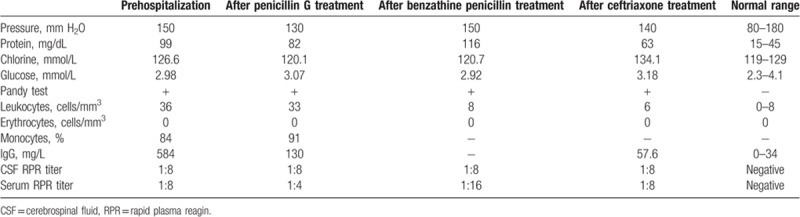
A 50-year-old woman was admitted to our hospital with 1-month history of stomachache. A gastroscopy examination performed at a local hospital before the appearance of the neurologic symptoms showed only mild erosive gastritis. The pain gradually extended to the upper abdomen and back. About 20 days after the onset of the gastric pain, she developed numbness in both lower extremities and weakness in the left lower limb. She reported having dysuria 7 days before her hospitalization but denied having any weakness or numbness in upper extremities. She had no history of upper respiratory tract infection, diarrhea, visual impairment, trauma, tumor, or weight loss. No relevant family history of neurologic disorders was present. A neurologic examination revealed that muscle strength in the left lower limb was 4/5. Her patellar tendon reflexes were exaggerated, and she had bilateral extensor plantar responses. A sensory examination revealed the loss of joint position sense in the left lower limb and a sensory level of approximately T1 on the right side. Higher mental functions, cranial nerve function, strength in the upper extremities and the right leg, muscle tension, and coordinate movements were normal. On the basis of the patient's symptoms and clinical findings, we localized the lesion to the thoracic cord. The clinical impression was Brown–Sequard syndrome caused by the lateral hemisection of the spinal cord. The MRI of the spinal cord was performed, and it showed swelling of the thoracic cord with diffuse high signal intensity on T2-weighted images (Fig. 1A). A lumbar puncture (LP) revealed the following: colorless cerebrospinal fluid (CSF); pressure, 150 mm H2O; protein, 99 mg/dL; glucose, 2.98 mmol/L; leukocyte count, 36 cells/mm3; monocytes, 84%; erythrocyte count, 0 cells/mm3; immunoglobulin G index, 0.80; negative cytology; oligoclonal bands, negative; and neuromyelitis optica antibody, negative. A serum Treponema pallidum particle assay (TPPA) test was positive, and a serum rapid plasma reagin (RPR) test yielded a titer of 1:8. The CSF RPR titer was also 1:8. Contrast-enhanced imaging with gadolinium-DTPA revealed enhancement of the spinal parenchyma and pia mater at the T6 level, and “a candle guttering appearance” on sagittal images (Fig. 1B–D). The abnormal parenchymal enhancement was relatively reduced on T2-weighted images, which showed the characteristic “flip-flop sign” (Fig. 1A, B). The erythrocyte-sedimentation rate and tests for HIV, SS-A, SS-B, rheumatoid factor, tumor marker, vitamin B12, and folate were normal. Thus, the patient was finally diagnosed with syphilitic meningomyelitis. We treated her with penicillin G, 6.4 million units intravenously (IV) every 6 hours for 14 days (dexamethasone 5 mg was used for 3 days to prevent a Jarisch–Herxheimer reaction), but the symptoms of pain and weakness were not improved. Moreover, a review LP showed little improvement (Table 1). A single intramuscular (IM) injection of 2.4 million units benzathine penicillin was then administered once a week for a month. However, the limb weakness and numbness worsened, and a repeat MRI performed 45 days after the onset showed that the lesion was enlarging; however, the LP results improved (Table 1). We therefore stopped benzathine penicillin and treated the patient with ceftriaxone 1 g IV twice a day and dexamethasone 15 mg once a day for 15 days. After this treatment, the lesion in the thoracic cord decreased in size (Fig. 1E), and the symptoms of pain and weakness were alleviated. Over one and a half years of follow-up, the patient has been able to care for herself and perform the activities of daily living; her pain has disappeared completely.
Figure 1.
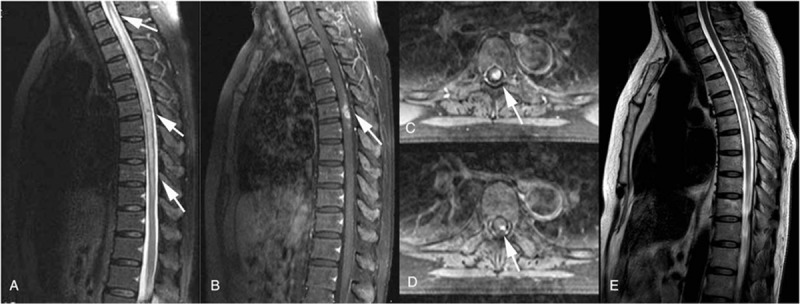
(A) A sagittal T2-weighted image of the thoracic spinal cord shows a long segment of diffuse high-signal intensity in the central portion of the spinal cord from T1 to T10. (B) A sagittal contrast-enhanced T1-weighted image shows enhancement of the pia mater at the T6 level. The superficial parts of T6 also strongly enhanced with gadolinium and showed a candle guttering appearance. The abnormal parenchymal enhancement was relatively reduced on T2-weighted images, which showed the characteristic “flip-flop sign.” (C, D) Axial T1-weighted images with contrast enhancement at the T6 level. (E) After treatment with ceftriaxone, the thoracic lesion has diminished, and might represent meningeal inflammation and spinal cord ischemia or edema.
Table 1.
Changes in the results of lumbar puncture.
3. Discussion
In this patient, the onset of syphilis was heralded by noncharacteristic symptoms, with chronic gastralgia being the chief complaint. This phenomenon is known as gastric crisis, which is a type of visceral crisis. It is caused by the involvement of the posterior nerve roots or the posterior horn and usually occurs in patients with tabes dorsalis.[2] The spinal ganglia contains numerous pseudounipolar neurons, whose axons split into 2 branches, one extending to the spinal posterior horn and the other to the peripheral sensory receptors in the trunk, limbs, visceral organs, and other parts of the body. Thus, the syphilitic involvement of the posterior nerve roots and the posterior horn leads to pain in both the visceral organs and the trunk. While there have been several case reports of syphilitic meningomyelitis, this is the first case in which this condition presented with visceral crisis.[3–13]
Neurosyphilis can be classified into several types based on the lesion in the spinal cord: syphilitic meningomyelitis, syphilitic spinal pachymeningitis, spinal vascular syphilis, syphilitic poliomyelitis, and tabes dorsalis.[14] Syphilitic meningomyelitis is a rare form of neurosyphilis that is pathologically characterized by meningeal inflammation and spinal cord ischemia or edema. These inflammatory and ischemic changes are partially reversible, and treatment with penicillin and corticosteroids can diminish the lesions to some extent.[3,4,6,7,9] The outcome of the present case supports this notion; after treatment with ceftriaxone and dexamethasone, our patient's neurologic symptoms and signs improved dramatically.
Kikuchi et al described the characteristic MRI features of syphilitic meningomyelitis as a “candle guttering appearance” and the flip-flop sign.[6] A long segment of the thoracic cord is usually involved in syphilitic meningomyelitis. This suggests that T pallidum might invade the spinal cord via the vessels and meninges, leading to parenchymatous inflammation and breakdown of the blood–spinal cord barrier.[6,8] The gadolinium enhancement seen on MRI might represent meningeal inflammation and spinal cord ischemia or edema secondary to meningovascular syphilis.[3–6,8,9] However, the flame sign, which is similar to the candle guttering appearance may help differentiate non-CNS intramedullary metastases from primary spinal cord tumors.[15] These MRI features can also be observed in spinal cord sarcoidosis.[16]
Owing to the nonspecific MRI features, the diagnosis of neurosyphilis must rely on serum and CSF tests such as nonspecific lipoidal tests (eg, RPR) and treponemal-specific tests (eg, TPPA). Once the diagnosis of neurosyphilis is established, treatment is initiated with high-dose IV penicillin for 14 days or 3 weekly doses of IM benzathine penicillin G. Ceftriaxone, 2 g/d IV, is an acceptable alternative. Before anti-treponemal treatment, prednisolone 20 to 60 mg daily for 3 days is recommended.[17] In our patient, dexamethasone was used for a longer time to restrict the expansion of edema that might result from meningeal inflammation or spinal cord ischemia and prevent Jarisch–Herxheimer reactions.[3,4,11]
The initial CSF examination in patients with syphilitic meningomyelitis demonstrates pleocytosis. However, pleocytosis does not parallel disease severity, as demonstrated in our patient. Although the CSF findings of lymphocytosis and elevated protein are often unhelpful in narrowing down the differential, they can help to guide treatment. The success of therapy is determined by a 4-fold drop or reversion to nonreactive in the titer of CSF-RPR.[1] Thus, follow-up CSF examination is necessary. CSF analysis should be repeated every 6 months until the cell count is normal.[18] Marra thought that if CSF abnormalities persist at 3 months after treatment (excluding elevated protein concentration), CSF should be reexamined at 6 months after therapy and again at 12 months if pleocytosis and CSF-RPR reactivity persist at 6 months.
In clinical practice, it is difficult to obtain precise information on patients’ sexual behaviors. In the HIV era, many neurosyphilis cases have been published, particularly, of early neurosyphilis.[19,20] Early treatment could prevent asymptomatic neurosyphilis from progressing to symptomatic neurosyphilis. To avoid delays in diagnosis and treatment, the clinician should take syphilitic meningomyelitis into account when he/she encounters a patient with longitudinally extensive myelitis in clinical practice.
4. Conclusion
Syphilitic meningomyelitis can present with visceral crisis and characteristic imaging findings. It is critical to diagnose this condition early and treat it with penicillin G or ceftriaxone in a timely manner. Abdominal pain may be a symptom of myelopathy, and syphilitic meningomyelitis ought to be considered in the differential diagnosis of a patient with longitudinally extensive myelitis.
Author contributions
Data curation: Nannan Zheng.
Writing – original draft: Li Sun, Nannan Zheng.
Writing – review & editing: Yu Yang, Haining Zhang.
Footnotes
Abbreviations: CNS = central nervous system, CSF = cerebrospinal fluid, IM = intramuscular, IV = intravenous, LP = lumbar puncture, MRI = magnetic resonance imaging, RPR = rapid plasma reagin, TPPA = Treponema pallidum particle assay.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Marra CM. Neurosyphilis. Continuum (Minneap Minn) 2015;21:1714–28. [DOI] [PubMed] [Google Scholar]
- [2].Oshita K, Saeki N, Niinai H, et al. Successful treatment of tabetic lightning pain and visceral crisis with gabapentin. J Anesth 2011;25:952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Nabatame H, Nakamura K, Matuda M, et al. MRI of syphilitic myelitis. Neuroradiology 1992;34:105–6. [DOI] [PubMed] [Google Scholar]
- [4].Tashiro K, Moriwaka F, Sudo K, et al. Syphilitic myelitis with its magnetic resonance imaging (MRI) verification and successful treatment. Jpn J Psychiatry Neurol 1987;41:269–71. [DOI] [PubMed] [Google Scholar]
- [5].Tsui EYK, Ng SH, Chow L, et al. Syphilitic myelitis with diffuse spinal cord abnormality on MR imaging. Eur Radiol 2002;12:2973–6. [DOI] [PubMed] [Google Scholar]
- [6].Kikuchi S, Shinpo K, Niino M, et al. Subacute syphilitic meningomyelitis with characteristic spinal MRI findings. J Neurol 2003;250:106–7. [DOI] [PubMed] [Google Scholar]
- [7].Chilver-Stainer L, Fischer U, Hauf M, et al. Syphilitic myelitis rare, nonspecific, but treatable. Neurology 2009;72:673–5. [DOI] [PubMed] [Google Scholar]
- [8].Dongmei He, Jiang B. Syphilitic myelitis: magnetic resonance imaging features. Neurol India 2014;62:89–91. [DOI] [PubMed] [Google Scholar]
- [9].Tohge R, Shinoto Y, Takahashi M. Longitudinally extensive transverse myelitis and optic neuropathy associated with syphilitic meningomyelitis and human immunodeficiency virus infection: a case report and review of the literature. Intern Med 2017;56:2067–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ted Strom, Schneck SA. Syphilitic meningomyelitis. Neurology 1991;41:325–6. [DOI] [PubMed] [Google Scholar]
- [11].Srivastava T, Thussu A. MRI in syphilitic meningomyelitis. Neurol India 2000;48:196–7. [PubMed] [Google Scholar]
- [12].Jacquemin GL, Proulx P, Gilbert DA, et al. Functional recovery from paraplegia caused by syphilitic meningomyelitis. J Spinal Cord Med 2002;25:133–7. [DOI] [PubMed] [Google Scholar]
- [13].Matijošaitis V, Vaitkus A, Pauza V, et al. Neurosyphilis manifesting as spinal transverse myelitis. Medicina (Kaunas) 2006;42:401–5. [PubMed] [Google Scholar]
- [14].Berger JR. Neurosyphilis and the spinal cord. J Nerv Ment Dis 2011;199:912–3. [DOI] [PubMed] [Google Scholar]
- [15].Samartzis D, Gillis CC, Shih P, et al. Intramedullary spinal cord tumors: part I - epidemiology, pathophysiology, and diagnosis. Global Spine J 2015;5:425–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gary M, Nesbit, Gary M, et al. Spinal cord sarcoidosis: a new finding at MR imaging with Gd-DTPA enhancement. Radiology 1989;173:839–43. [DOI] [PubMed] [Google Scholar]
- [17].Berger JR, Dean D. Neurosyphilis. Handb Clin Neurol 2014;121:1461–72. [DOI] [PubMed] [Google Scholar]
- [18].Nazia Karsan, Robert Barker, O’Dwyer JP. Clinical reasoning: the “great imitator”. Neurology 2014;83:e188–96. [DOI] [PubMed] [Google Scholar]
- [19].Merins V, Hahn K. Syphilis and neurosyphilis: HIV-coinfection and value of diagnostic parameters in cerebrospinal fluid. Eur J Med Res 2015;20:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Centers for Disease Control and Prevention (CDC). Symptomatic early neurosyphilis among HIV-positive men who have sex with men - four cities, United States, January 2002–June 2004. MMWR Morb Mortal Wkly Rep 2007;56:625–8. [PMC free article] [PubMed] [Google Scholar]


