Supplemental Digital Content is available in the text
Keywords: coronary artery disease, gender, percutaneous coronary intervention
Abstract
Background and objectives:
Previous researches have reported the controversial results regarding the gender difference in clinical outcomes of patients with coronary artery disease after percutaneous coronary intervention. Hence, this systematic review and meta-analysis was designed to investigate whether gender difference existed in patients with coronary artery disease after percutaneous coronary intervention.
Methods:
PubMed, Embase, and the Cochrane Library database were searched up to February 10, 2018. Studies comparing the gender-specific effect on clinical outcomes of patients with coronary artery disease after percutaneous coronary intervention were identified, to analyze mortality, major adverse cardiovascular events (MACE) and revascularization. Statistical software RevMan was utilized in this meta-analysis.
Results:
A total of 49 studies, involving 1,032,828 patients (774,115 males and 258,713 females) reporting gender-specific outcomes, were included in this study. The in-hospital mortality, 30-day mortality, 1-year mortality, and at least 2-years mortality in male patients with coronary artery disease after percutaneous coronary intervention were significantly lower than those of females (odds ratio [OR] 0.58 95% confidence interval [CI] 0.52–0.63, P < .001; OR 0.64, 95% CI 0.61–0.66, P = .04; OR 0.67, 95% CI 0.60–0.75, P < .001 and OR 0.71, 95% CI 0.63–0.79, P = .005, respectively). The MACE was significantly decreased in male subjects after initial percutaneous coronary intervention compared with females in <1-year or at least 1-year (OR 0.67, 95% CI 0.56–0.80, P < .001 and OR 0.84, 95% CI 0.76–0.93, P < .001). The male patients after percutaneous coronary intervention harbored higher rate of revascularization compared with females for at least 1-year (OR 1.17, 95% CI 1.00–1.36, P < .001), while the rate of revascularization in male patients for < 1-year was lower than that of females (OR 0.93, 95% CI 0.69–1.26, P < .001).
Conclusions:
The systematic review and meta-analysis suggests that the prognosis of male patients with coronary artery disease after percutaneous coronary intervention is better than that of females, except for long-term revascularization.
1. Introduction
Coronary artery disease is the most common cardiovascular disease caused by coronary stenosis, spasm or occlusion. It is estimated that up to 23.3 million people will die of cardiovascular disease by 2030.[1] To improve patient's viability, percutaneous coronary intervention (PCI) is the most commonly applied approach of reperfusion in many countries. However, multiple researches have pointed out that there were some prognostic differences between different genders.[2–44] Some studies have showed persistent gender difference in outcomes after adjusting multivariate factors,[2,5,7,9,10,13,15,18,20–25,28,30–33,35–39,41–43] while other studies also demonstrated that gender was not an independent factor for patient's outcome.[3,4,11,12,14,17,19,26,27,29,34,40,44] Although previous meta-analysis has demonstrated the effect of gender on response to PCI, which not involved major adverse cardiovascular events (MACE) and revascularization, and the follow-up period was also comparatively short.[45–48] Therefore, this meta-analysis was designed to determine the gender difference in patients with coronary artery disease after PCI, and provide evidence for the development of the guideline.
2. Materials and methods
2.1. Date source and search strategy
PubMed, Embase, and the Cochrane Library database were searched up to February 10, 2018. The following keywords and medical subject headings were utilized according to the “PICO” strategy: “coronary artery disease”, “percutaneous coronary intervention” or “PCI”, “gender”, or “sex”. Meanwhile, to prevent missing the related articles, the bibliography of the articles included in this study was retrieved manually. All analyses were based on previous published some studies, thus no ethical approval and patient consent are required.
2.2. Study selection and quality assessment
Three reviewers (YYG, FHY, and CLF) preliminarily and independently screened the articles that were eligible for study based on the title and summary. In the case of disagreements, the issues were solved through tripartite negotiation when checking the selected articles. The filtered article satisfied the following criteria: Coronary artery disease, including acute coronary syndrome, acute myocardial infarction, ST-segment elevation myocardial infarction, non-ST-segment elevation myocardial infraction, non-ST segment elevation acute coronary syndrome, unstable angina, and stable coronary artery disease; patients undergoing PCI; gender, sex, female, and male; gender-related different outcomes, including short and long-term mortality, MACE, revascularization. In this meta-analysis, all original articles were endeavored to collect, without considering case reports, summaries of the meeting or relevant comments of the original study. The Cochrane collaboration's tool[49] and Newcastle–Ottawa scale[50] were utilized to assess the quality of randomized controlled trials and observational studies.
2.3. Outcome definition
The outcomes of this pooled analysis included 3 primary endpoints, that was, mortality, MACE, and revascularization. The mortality was assessed mainly from in-hospital mortality, 30-day mortality, 1-year mortality, and at least 2-years mortality. The MACE and revascularization were divided by the cutoff of 1 year, including <1-year and at least 1-year MACE, revascularization for <1 year and at least 1 year.
2.4. Statistical analysis
Statistical software RevMan (version 5.3, Cochrane Collaboration Network) was utilized for data analysis in this meta-analysis. For all the outcomes, dichotomous data were pooled as Mantel–Haenszel odds ratio (OR) with the corresponding 95% confidence interval (CI). Statistical heterogeneity was evaluated by Chi-square test, which was showed by I2 statistic. Fixed effects models were employed in the case of no evidence of heterogeneity (I2≥50%), otherwise random effects model was used. Subgroup analysis was performed to figure out sources of heterogeneity in the case of large heterogeneity. Sensitivity analysis was performed to determine whether any single study was primarily responsible for the final results. All statistical tests were two-tailed, and a P value < 0.05 was considered as statistical significance.
3. Results
3.1. Search results
A total of 6636 articles were retrieved, of which 157 related articles were identified after screening the title and abstract. Studies with subjects <100, non-English literature and those failed to meet the inclusion criteria of the study were excluded by reading the full text. Final only 49 nonrandomized control studies are included, which 13 studies were from Asian countries, 25 studies from European countries, 11 studies from North American, and 2 studies from Australia. The duration of follow-up varied from hospital stay to 30-day, and lasting to 7 years. The NOS was utilized to evaluate all the enrolled studies in this pooled analysis. Of them the quality score was 7 and 8 in 16 and the remaining 33 studies on the 0 to 10 scoring system, respectively (see Table, Supplemental Content, which illustrates the specific scores for each study).
3.2. Baseline data characteristics
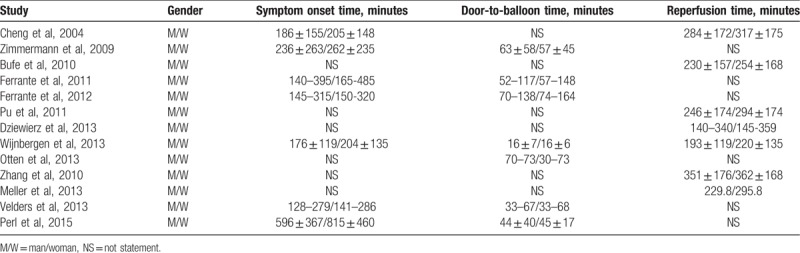
Age, a history of hypertension, hyperlipidemia or dyslipidemia, diabetes mellitus, and smoking are reviewed by carefully reading the full text and summarizing the baseline data of each study (Table 1). Meanwhile, the male patients with coronary artery disease after PCI were found to harbor lower incidence of hypertension (OR 0.58, 95% CI 0.47–0.71, P < .001), diabetes (OR 0.72, 95% CI 0.68–0.77, P < .001), hyperlipidemia or dyslipidemia (OR 0.98, 95% CI 0.94–1.02, P < .001), and cardiogenic shock (OR 0.78, 95% CI 0.65–0.92, P < .001) compared with females. Although the smoking rate of male subjects (OR 2.65, 95% CI 2.16–3.24, P < .001) was higher than that of females, but the symptom onset time, door-to-balloon time and reperfusion time for female patients with coronary artery disease after PCI were longer than those of males (Table 2). In addition, the age of male patients is younger compared with females (Table 1).
Table 1.
Characteristics of included studies.
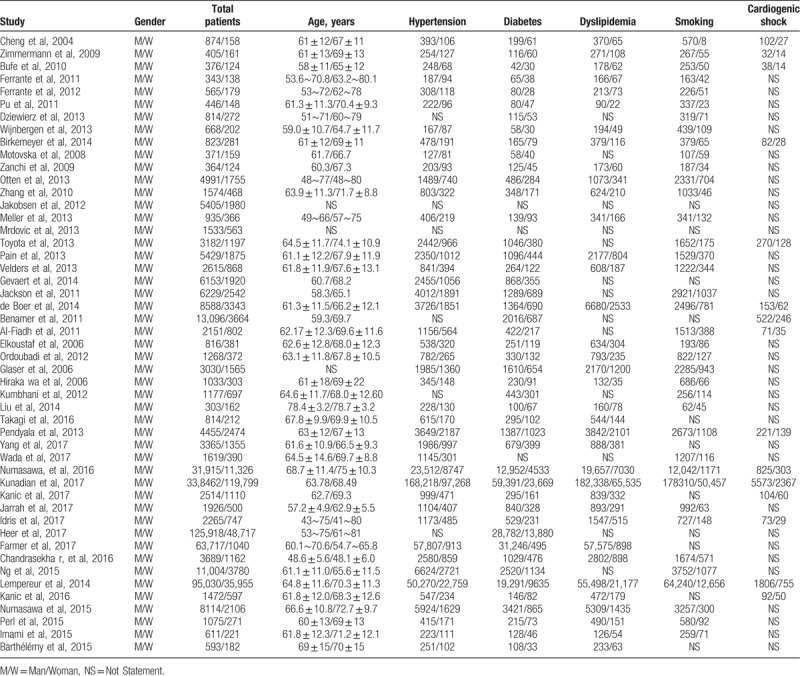
Table 2.
The ischemia-reperfusion time between different genders were mentioned in this study.
3.3. The mortality
The 24 studies (n = 430,914)[5,10,12,14,18,19,21,22,24–28,30,32,35,37,39,40,41,43,44,51,52] reported on PCI postoperative in-hospital mortality, which show that the in-hospital mortality of male patients was significantly lower than that of females (OR 0.58, 95% CI 0.52–0.63, P < .001, I2 = 66%) (Fig. 1). This gender differences also reflect in 30-day mortality [OR 0.64, 95% CI 0.61–0.66, P = .04, I2 = 40%; 19 studies (n = 523,304)],[2–4,7,8,13–17,23,25,26,33–36,42,53] 1-year mortality [OR 0.67, 95% CI 0.60–0.75, P < .001, I2 = 73%; 20 studies (n = 590,590)][8,10,13,15–17,20,25,26,28,30,33,35,36,38,43,44,53–55] and >2-years mortality [OR 0.71, 95% CI 0.63–0.79, P = .005, I2 = 57%; 14 studies (n = 43,096)][4–6,18,19,23,29,31,34,36,40,43,52,56] (Figs. 2–4). Due to the low heterogeneity (I2 < 50%) of the 30-day follow-up, the fixed effects models were used, without subgroup analysis. Other follow-up results showed that the I2 value was >50%. Subgroup analysis was carried out according to different prognostic factors. However, the source of heterogeneity could not be accurately identified, thus the random effects model was used. Sensitivity analysis indicated that the results of each group were relatively stable and reliable.
Figure 1.
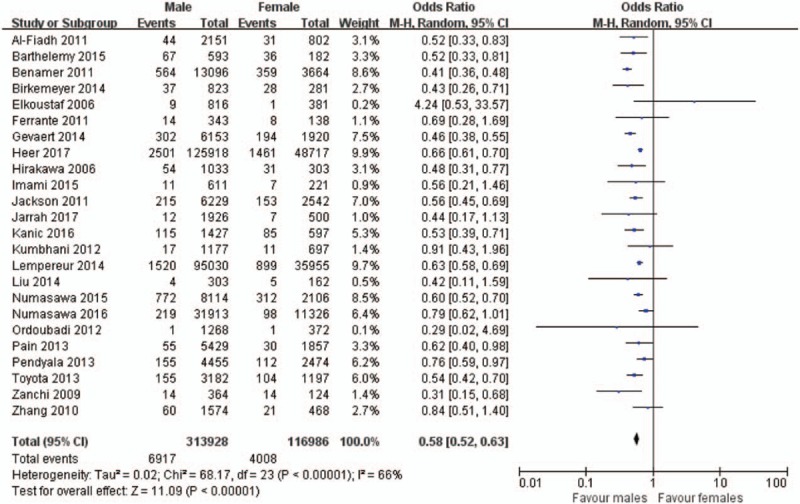
Forest plot of in-hospital mortality in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
Figure 2.
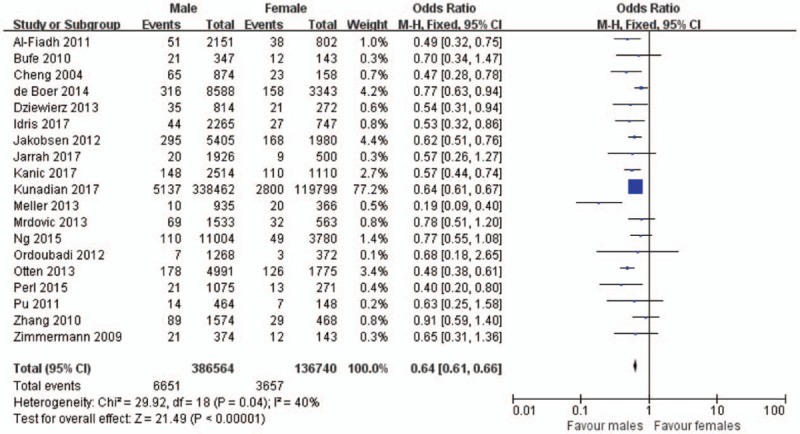
Forest plot of 30-day mortality in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
Figure 4.
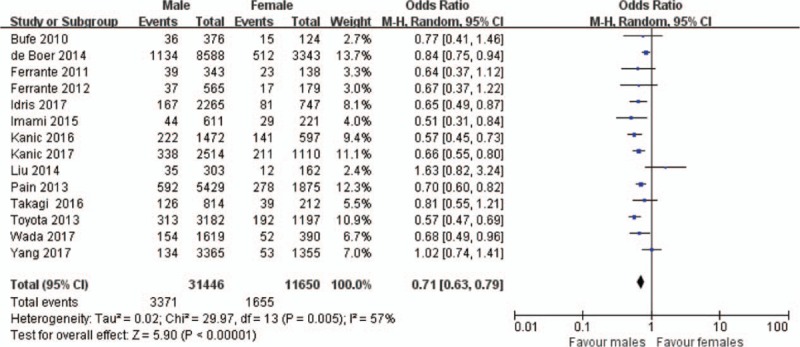
Forest plot of at least 2-years mortality in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
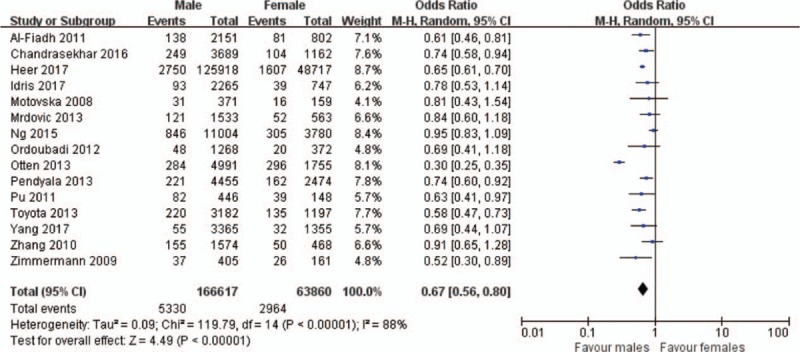
Figure 3.
Forest plot of 1-year mortality in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
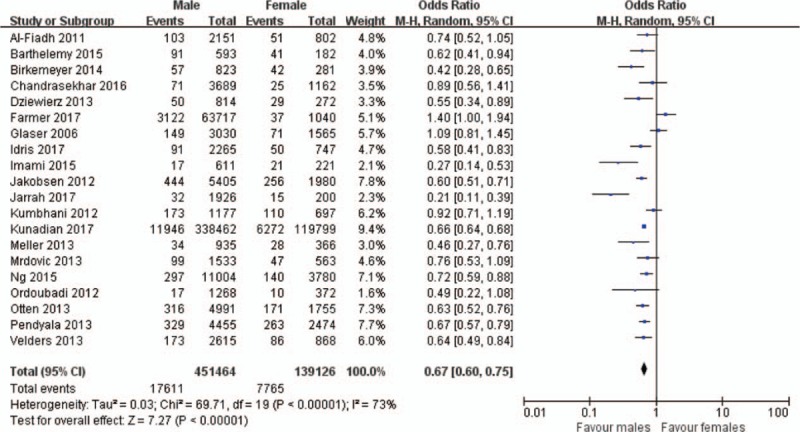
3.4. MACE
Pooled analysis of 15 studies (n = 230,477) shows that the incidence of MACE was lower in male patients with coronary artery disease after PCI compared with females in follow-up period of < 1-year (OR 0.67, 95% CI 0.56–0.80, P < .001, I2 = 88%)[3,7,11,13,14,17,18,25,26,30,36,37,38,53,56] (Fig. 5). The male patients also experienced lower rate of MACE than females when the follow-up period was extended to at least 1-year [OR 0.84, 95% CI 0.76–0.93, P < .001, I2 = 74%; 17 studies (n = 111,903)][4–6,13,17,18,25,26,29,30,31,36,38,52,54–56] (Fig. 6). The results of both groups displayed that the I2 value was >50%, but the appropriate factors for the high heterogeneity after adopted the subgroup analysis cannot be identified. Therefore, the meta-analysis of MACE was performed by random effects model. Sensitivity analysis showed that no single study was responsible for the overall effect size, and the results were stable and credible.
Figure 5.
Forest plot of <1-year MACE in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
Figure 6.
Forest plot of the least 1-year MACE in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
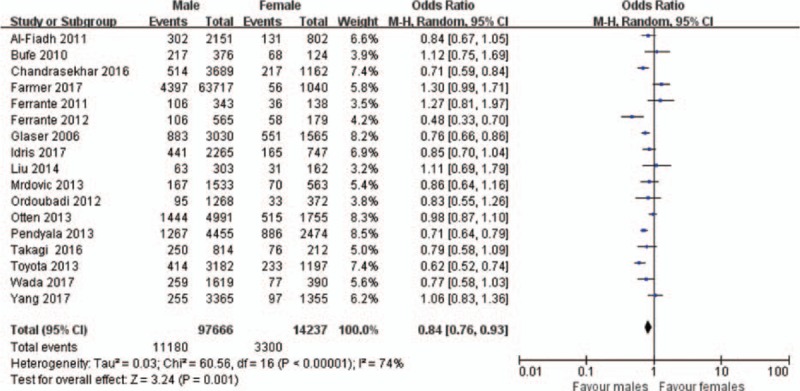
3.5. The revascularization
The pooled data show that the revascularization rate in male patients with coronary artery disease after PCI was lower than that of females during a follow-up period of <1-year [OR 0.93, 95% CI 0.69–1.26, P < .001, I2 = 64%; 9 studies (n = 39,375)][2,13,14,25,26,35,36,53,56] (Fig. 7), which was on opposite to the outcomes between male and female patients for at least 1-year [OR 1.17, 95% CI 1.00–1.36, P < .001, I2 = 71%; 16 studies (n = 37,770)[4–6,9,10,13,18,25,26,29,30,35,36,44,52,56] (Fig. 8). The result showed that the I2 values of both groups were >50%. Random effects model was utilized, because the heterogeneity cannot be explained according to subgroup analysis. Sensitivity analysis indicated that the result was stable and relatively robust.
Figure 7.
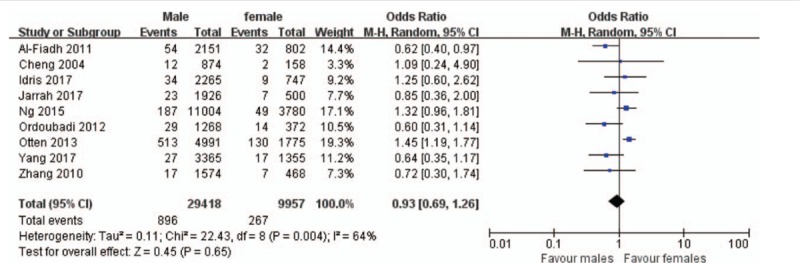
Forest plot of <1-year revascularization rate in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
Figure 8.
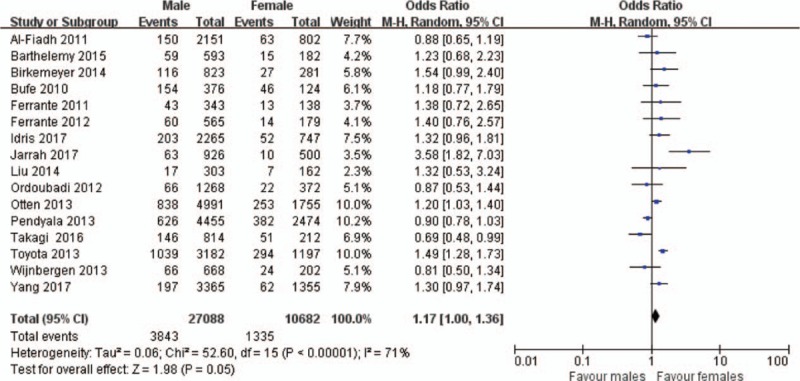
Forest plot of the least 1-year revascularization rate in male vs female patients with coronary artery disease after PCI. PCI = percutaneous coronary intervention.
4. Discussion
The main results of this meta-analysis are as follows: the mortality in male patients with coronary artery disease after PCI was lower than that of females; the male patients with coronary artery disease after PCI harbored a lower incidence of MACE, no matter whether the follow-up period was <1 year or at least 1 year; the male patients with coronary artery disease after PCI overwhelmed females in long-term revascularization.
The mortality in male patients with coronary artery disease after PCI was lower than that of females in this study both in short-term and long-term follow-up, which was consistent with previous systematic reviews.[45–48] Because female subjects had much more hypertension, diabetes, dyslipidemia this meta-analysis, especially longer times of reperfusion ischemia,[1–8,12,13,15,19,41] the latter may be caused by chest pain symptoms, which had not been fully explained in female patients with coronary artery disease, leading to delay prehospital visits. Therefore, the high mortality in female patients with coronary artery disease after PCI had been largely attributed to more adverse cardiovascular risk profiles compared with males. This meta-analysis has confirmed that the female patients with coronary artery disease were older than males, which may also attribute to the high mortality of female patients, and consistent with National Cardiovascular Data Registry ACTION Registry of America.[57] Meanwhile, in this study, it had also been verified that the female subjects were more prone to suffer from cardiogenic shock, which was considered as another important indicator for higher mortality in female patients with coronary artery disease after PCI. The same consequences were obtained by meta-analysis by Kano et al.[47] In short, it is an indisputable fact that the mortality in female patients with coronary artery disease after PCI was high.
Similar to the above results, the male patients with coronary artery disease after PCI also had a lower incidence of MACE for <1 year or at least 1-year in this meta-analysis, which is a supplement and summary to previous systematic reviews and observational studies.[7,25,29,38,54,56] The reasons for the above differences should first be attributed to the fact that the mortality in female patients with coronary artery disease after PCI is higher than that of males. Moreover, possessing more adverse cardiovascular risk profile was also an important factor for high incidence of MACE in female patients with coronary artery disease, the baseline data of this study had witnessed this proposition. The study of Jakobsen et al[15] also showed female patients with coronary artery disease were burdened with more complications and worse hemodynamic status compared with males. The gender difference of MACE was still largely attributed to the higher incidence of heart failure in female patients with STEMI in some cohort.[3,6,13,20] In summary, the above pathological factors had led to the high incidence of MACE in female patients with coronary artery disease after PCI. It is noteworthy that females had a worse clinical outcome, which reminds physicians should pay more attention to female patients in clinical practice.
This systematic review and meta-analysis also showed that male patients with coronary artery disease after PCI had the advantages of revascularization compared with females in the long-term follow-up, which was consistent with the parts of previous observational studies,[4–6,10,13,18,35,36,44,52,56] and supplied the main outcome of previous systematic reviews.[45–48] This may be associated with more smoking in males from the baseline data of this study. On the contrary, the low incidence of revascularization in female subjects also included lower follow-up rates, atypical symptoms, difficult identification of myocardial ischemia, unwillingness of receiving invasive examinations, as well as the prejudices of doctor that female subjects might harbor lower rate of coronary arteriography during follow-up.[17] In addition, female subjects with coronary artery disease after PCI had higher mortality during short and long-term follow-up, which might reduce the chance of next revascularization. Moreover, a research had indicated that the application of drug-eluting stents could decrease probability of coronary artery revascularization in female patients with PCI.[58] Furthermore, the coronary artery of male patient with coronary artery disease is prone to harbor complicated lesions, including left main disease, chronic total occlusion and diffuse lesion.[56] Meanwhile, male subjects suffering from more platelet-rich thrombus, atherosclerotic plaque rupture as well as micro-embolization were also demonstrated in some studies.[59] The above-described pathophysiological difference would result in elevated risks of revascularization in male subjects. However, the female had a high incidence of <1-year revascularization, which was an integral part to <1-year MACE. Overall, the incidence of revascularization in female patients with coronary artery disease after PCI was higher than that of males in short-term follow-up, which was opposite in long-term follow-up showed the opposite result.
4.1. Limitations
Firstly, the main limitations of this study were that all articles included in this study were nonrandomized control studies. Therefore, many subjective factors were inevitable during the follow-up. Secondly, of the 1,032,828 patients included in the meta-analysis, the female patients accounted for only 1/4 of the total sample size. Thus, unequal distribution of gender may lead to a bias. Thirdly, there are large discrepancy in sample size and follow-up spans among different studies, which may lead to heterogeneity. Because most studies had larger heterogeneity, the random effects model was adopted; the results may weaken the large sample information with better quality. Fourthly, due to the lack of patient-level data, subgroup analysis was not conducted according to the type of subjects, and the specific prognosis of patients with different types of coronary artery disease undergoing PCI could not be assessed. Final, the language included in the study was limited to English, and there was a lack of researches in South America and Africa countries. Therefore, language and regional bias may be unavoidable.
5. Conclusions
In conclusion, the prognosis of male patients with coronary artery disease after PCI is better than that of females, except for long-term revascularization.
Acknowledgments
We would like to thank Professor Jinhui Tian of Evidence Based Medicine Center of Lanzhou University for guidance in the systematic search and statistical support.
Author contributions
Conceptualization: Yaya Guo, Zhilu Wang.
Data curation: Yaya Guo.
Formal analysis: Yaya Guo, Fahui Yin, Chunlei Fan.
Investigation: Yaya Guo, Fahui Yin, Chunlei Fan.
Methodology: Yaya Guo, Fahui Yin, Chunlei Fan.
Project administration: Zhilu Wang.
Resources: Yaya Guo.
Software: Yaya Guo.
Supervision: Zhilu Wang.
Validation: Zhilu Wang.
Writing – original draft: Yaya Guo.
Writing – review & editing: Fahui Yin, Chunlei Fan.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, MACE = major adverse cardiovascular events, OR = odds ratio, PCI = percutaneous coronary intervention.
Funding and conflict of interest: All authors have declared that no support, financial, or otherwise, has been received from any organization that may have an interest in the submitted work and there are no other relationships or activities that could appear to have influenced the submitted work.
YG, FY, and CF contributed equally to this work.
Supplemental Digital Content is available for this article.
References
- [1].World Health Organization. The top 10 causes of death, Fact Sheet No.310. Updated January 2017. Accessed date: Jan 16 2018. Available at: www.who.int/mediacentre/factsheets/fs310/en/. [Google Scholar]
- [2].Cheng CI, Yeh KH, Chang HW, et al. Comparison of baseline characteristics, clinical features, angiographic results, and early outcomes in male vs female with acute myocardial infarction undergoing primary coronary intervention. Chest 2004;126:47–53. [DOI] [PubMed] [Google Scholar]
- [3].Zimmermann S, Ruthrof S, Nowak K, et al. Short-term prognosis of contemporary interventional therapy of ST-elevation myocardial infarction: does gender matter? Clin Res Cardiol 2009;98:709–15. [DOI] [PubMed] [Google Scholar]
- [4].Bufe A, Wolfertz J, Dinh W, et al. Gender-based differences in long-term outcome after ST-elevation myocardial infarction in patients treated with percutaneous coronary intervention. J Females Health 2010;19:471–5. [DOI] [PubMed] [Google Scholar]
- [5].Ferrante G, Corrada E, Belli G, et al. Impact of female sex on long-term outcomes in patients with ST-elevation myocardial infarction treated by primary percutaneous coronary intervention. Can J Cardiol 2011;27:749–55. [DOI] [PubMed] [Google Scholar]
- [6].Ferrante G, Presbitero P, Corrada E, et al. Sex-specific benefits of sirolimus-eluting stent on long-term outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention: insights from the Multicenter Evaluation of Single High-Dose Bolus Tirofiban versus abciximab with sirolimus-eluting stent or bare-metal stent in acute myocardial infarction study trial. Am Heart J 2012;163:104–11. [DOI] [PubMed] [Google Scholar]
- [7].Pu J, Shan P, Ding S, et al. Gender differences in epicardial and tissue-level reperfusion in patients undergoing primary angioplasty for acute myocardial infarction. Atherosclerosis 2011;215:203–8. [DOI] [PubMed] [Google Scholar]
- [8].Dziewierz A, Siudak Z, Rakowski T, et al. Early administration of abciximab reduces mortality in female patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention (from the EUROTRANSFER Registry). J Thromb Thrombolysis 2013;36:240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wijnbergen I, Tijssen J, van’t Veer M, et al. Gender differences in long-term outcome after primary percutaneous intervention for ST-segment elevation myocardial infarction. Catheter Cardiovasc Interv 2013;82:379–84. [DOI] [PubMed] [Google Scholar]
- [10].Birkemeyer R, Schneider H, Rillig A, et al. Do gender differences in primary PCI mortality represent a different adherence to guideline recommended therapy? a multicenter observation. BMC Cardiovasc Disord 2014;14:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Motovska Z, Widimsky P, Aschermann M. The impact of gender on outcomes of patients with ST elevation myocardial infarction transported for percutaneous coronary intervention: analysis of the PRAGUE-1 and 2 studies. Heart 2008;94:e5. [DOI] [PubMed] [Google Scholar]
- [12].Zanchi J, Miric D, Giunio L, et al. Gender differences in in-hospital mortality and angiographic findings of patients with acute ST-segment elevation myocardial infarction (STEMI) undergoing percutaneous coronary intervention (PCI). Coll Antropol 2009;33:1359–62. [PubMed] [Google Scholar]
- [13].Otten AM, Maas AH, Ottervanger JP, et al. Is the difference in outcome between male and female treated by primary percutaneous coronary intervention age dependent? Gender difference in STEMI stratified on age. Eur Heart J Acute Cardiovasc Care 2013;2:334–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhang Q, Qiu JP, Zhang RY, et al. Absence of gender disparity in short-term clinical outcomes in patients with acute ST-segment elevation myocardial infarction undergoing irolimus-eluting stent based primary coronary intervention: a report from Shanghai Acute Coronary Event (SACE) Registry. Chin Med J 2010;123:782–8. [PubMed] [Google Scholar]
- [15].Jakobsen L, Niemann T, Thorsgaard N, et al. Sex- and age-related differences in clinical outcome after primary percutaneous coronary intervention. Eurointervention 2012;8:904–11. [DOI] [PubMed] [Google Scholar]
- [16].Meller SM, Lansky AJ, Costa RA, et al. Implications of myocardial reperfusion on survival in female versus male with acute myocardial infarction undergoing primary coronary intervention. Am J Cardiol 2013;112:1087–92. [DOI] [PubMed] [Google Scholar]
- [17].Mrdovic I, Savic L, Asanin M, et al. Sex-related analysis of short- and long-term clinical outcomes and bleeding among patients treated with primary percutaneous coronary intervention: an evaluation of the RISK-PCI data. Can J Cardiol 2013;29:1097–103. [DOI] [PubMed] [Google Scholar]
- [18].Toyota T, Furukawa Y, Ehara N, et al. Sex-based differences in clinical practice and outcomes for Japanese patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J 2013;77:1508–17. [DOI] [PubMed] [Google Scholar]
- [19].Pain TE, Jones DA, Rathod KS, et al. Influence of female sex on long-term mortality after acute coronary syndromes treated by percutaneous coronary intervention: a cohort study of 7304 patients. Coron Artery Dis 2013;24:183–90. [DOI] [PubMed] [Google Scholar]
- [20].Velders MA, Boden H, van Boven AJ, et al. Influence of gender on ischemic times and outcomes after ST-elevation myocardial infarction. Am J Cardiol 2013;111:312–8. [DOI] [PubMed] [Google Scholar]
- [21].Gevaert SA, De BD, Evrard P, et al. Gender, TIMI risk score and in-hospital mortality in STEMI patients undergoing primary PCI: results from the Belgian STEMI registry. Eurointervention 2014;9:1095–101. [DOI] [PubMed] [Google Scholar]
- [22].Jackson EA, Moscucci M, Smith DE, et al. The association of sex with outcomes among patients undergoing primary percutaneous coronary intervention for ST elevation myocardial infarction in the contemporary era: Insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). Am Heart J 2011;161:106–12. [DOI] [PubMed] [Google Scholar]
- [23].de Boer SP, Roos-Hesselink JW, van Leeuwen MA, et al. Excess mortality in female compared to male after PCI in STEMI: an analysis of 11, 931 patients during 2000-2009. Int J Cardiol 2014;176:456–63. [DOI] [PubMed] [Google Scholar]
- [24].Benamer H, Tafflet M, Bataille S, et al. Female gender is an independent predictor of in-hospital mortality after STEMI in the era of primary PCI: insights from the greater Paris area PCI Registry. Eurointervention 2011;6:1073–9. [DOI] [PubMed] [Google Scholar]
- [25].Al-Fiadh AH, Andrianopoulos N, Farouque O, et al. Contemporary outcomes in female undergoing percutaneous coronary intervention for acute coronary syndromes. Int J Cardiol 2011;151:195–9. [DOI] [PubMed] [Google Scholar]
- [26].Fath-Ordoubadi F, Barac Y, Abergel E, et al. Gender impact on prognosis of acute coronary syndrome patients treated with drug-eluting stents. Am J Cardiol 2012;110:636–42. [DOI] [PubMed] [Google Scholar]
- [27].Hirakawa Y, Masuda Y, Uemura K, et al. Differences in in-hospital mortality between male and female with acute myocardial infarction undergoing percutaneous coronary intervention in Japan: Tokai Acute Myocardial Infarction Study (TAMIS). Am Heart J 2006;151:1271–5. [DOI] [PubMed] [Google Scholar]
- [28].Kumbhani DJ, Shishehbor MH, Karim S, et al. Influence of gender on long-term mortality in patients presenting with non-ST-elevation acute coronary syndromes undergoing percutaneous coronary intervention. Am J Cardiol 2012;109:1087–91. [DOI] [PubMed] [Google Scholar]
- [29].Takagi K, Chieffo A, Shannon J, et al. Impact of gender on long-term mortality in patients with unprotected left main disease: The Milan and New-Tokyo (MITO) Registry. Int J Cardiol 2014;177:1131–3. [DOI] [PubMed] [Google Scholar]
- [30].Pendyala LK, Torguson R, Loh JP, et al. Comparison of adverse outcomes after contemporary percutaneous coronary intervention in female versus male with acute coronary syndrome. Am J Cardiol 2013;111:1092–8. [DOI] [PubMed] [Google Scholar]
- [31].Wada H, Ogita M, Miyauchi K, et al. Impact of gender difference on long-term outcomes of percutaneous coronary intervention for coronary artery disease in patients under statin treatment. Heart Vessels 2017;32:16–21. [DOI] [PubMed] [Google Scholar]
- [32].Numasawa Y, Inohara T, Ishii H, et al. Comparison of outcomes of female versus male with non-ST-elevation acute coronary syndromes undergoing percutaneous coronary intervention (from the Japanese Nationwide Registry). Am J Cardiol 2017;119:826–31. [DOI] [PubMed] [Google Scholar]
- [33].Kunadian V, Qiu W, Lagerqvist B, et al. Gender differences in outcomes and predictors of all-cause mortality after percutaneous coronary intervention (data from United Kingdom and Sweden). Am J Cardiol 2017;119:210–6. [DOI] [PubMed] [Google Scholar]
- [34].Kanic V, Vollrath M, Tapajner A, et al. Sex-Related 30-Day and long-term mortality in acute myocardial infarction patients treated with percutaneous coronary intervention. J Females Health 2017;26:374–9. [DOI] [PubMed] [Google Scholar]
- [35].Jarrah MI, Hammoudeh AJ, Alnatour DB, et al. Gender differences in risk profile and outcome of Middle Eastern patients undergoing percutaneous coronary intervention. Saudi Med J 2017;38:149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Idris H, French JK, Shugman IM, et al. Influence of age and gender on clinical outcomes following percutaneous coronary intervention for acute coronary syndromes. Heart Lung Circ 2017;26:554–65. [DOI] [PubMed] [Google Scholar]
- [37].Heer T, Hochadel M, Schmidt K, et al. Sex differences in percutaneous coronary intervention—insights from the coronary angiography and PCI registry of the German society of cardiology. J Am Heart Assoc 2017;6:e004972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Chandrasekhar J, Usman Baber MD, Sartori S, et al. Sex-related differences in outcomes among male and female under 55 years of age with acute coronary syndrome undergoing percutaneous coronary intervention: Results from the PROMETHEUS Study. Catheter Cardiovasc Interv 2016;89:629–37. [DOI] [PubMed] [Google Scholar]
- [39].Lempereur M, Magne J, Cornelis K, et al. Impact of gender difference in hospital outcomes following percutaneous coronary intervention. Results of the Belgian Working Group on Interventional Cardiology (BWGIC) registry. Eurointervention 2014;12:e216–223. [DOI] [PubMed] [Google Scholar]
- [40].Kanic V, Vollrath M, Naji FH, et al. Gender related survival differences in ST-elevation myocardial infarction patients treated with primary PCI. Int J Med Sci 2016;13:440–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Numasawa Y, Kohsaka S, Miyata H, et al. Gender differences in in-hospital clinical outcomes after percutaneous coronary interventions: an insight from a Japanese multicenter registry. PLoS One 2015;10:e0116496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Michal Laufer-Perl MD, Yacov Shacham MD, Sivan Letourneau-Shesaf MD, et al. Gender-related mortality and in-hospital complications following ST-segment elevation myocardial infarction: data from a primary percutaneous coronary intervention cohort. Clin Cardiol 2015;38:145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Ghauharali-Imami S, Bax M, Haasdijk A, et al. The impact of gender on long-term mortality in patients with multivessel disease after primary percutaneous coronary intervention. Netherlands Heart J 2015;23:592–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Barthélémy O, Degrell P, Berman E, et al. Sex-related differences after contemporary primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Arch Cardiovasc Dis 2015;108:428–36. [DOI] [PubMed] [Google Scholar]
- [45].Bavishi C, Bangalore S, Patel D, et al. Short and long-term mortality in female and male undergoing primary angioplasty: a comprehensive meta-analysis. Int J Cardiol 2015;198:123–30. [DOI] [PubMed] [Google Scholar]
- [46].Mg VDM, Nathoe HM, Van d GY, et al. Worse outcome in female with STEMI: a systematic review of prognostic studies. Eur J Clin Invest 2015;45:226–35. [DOI] [PubMed] [Google Scholar]
- [47].Conrotto F, D’Ascenzo F, Humphries KH, et al. A meta-analysis of sex-related differences in outcomes after primary percutaneous intervention for ST-segment elevation myocardial infarction. J Interv Cardiol 2015;28:132–40. [DOI] [PubMed] [Google Scholar]
- [48].Jang JS, Park YA, Jin HY, et al. P4661Sex difference in mortality among patients with acute myocardial infarction treated by primary percutaneous coronary intervention: a meta-analysis. Eur Heart J 2017;38(suppl 1) [Google Scholar]
- [49].Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomized trials. Brit Med J 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of non-randomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [51].Elkoustaf RA, Mamkin I, Mather JF, et al. Comparison of results of percutaneous coronary intervention for non-ST-elevation acute myocardial infarction or unstable angina pectoris in male versus female. Am J Cardiol 2006;98:182–6. [DOI] [PubMed] [Google Scholar]
- [52].Liu Y, Hu X, Xue Q, et al. Influence of sex on outcomes after percutaneous coronary intervention in patients over 75 years of age with coronary heart disease. Clin Interv Aging 2014;9:1831–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Ng VG, Baumbach A, Grinfeld L, et al. Impact of bleeding and bivalirudin therapy on mortality risk in female undergoing percutaneous coronary intervention (from the REPLACE-2, ACUITY, and HORIZONS-AMI Trials). Am J Cardiol 2015;117:186–91. [DOI] [PubMed] [Google Scholar]
- [54].Farmer MM, Stanislawski MA, Plomondon ME, et al. Sex differences in 1-year outcomes after percutaneous coronary intervention in the Veterans Health Administration. J Females Health 2017;26:1062–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Glaser R, Selzer F, Jacobs AK, et al. Effect of gender on prognosis following percutaneous coronary intervention for stable angina pectoris and acute coronary syndromes. Am J Cardiol 2006;98:1446–50. [DOI] [PubMed] [Google Scholar]
- [56].Yang J, Zhang F, Qian J, et al. Sex-based influence on clinical outcomes after drug-eluting stent implantation in real-world patients: insight from the FOCUS registry. Ann Med 2017;49:185–95. [DOI] [PubMed] [Google Scholar]
- [57].Smilowitz NR, Mahajan AM, Roe MT, et al. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION Registry-GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With the Guidelines). Circ Cardiovasc Qual Outcomes 2017;10:e003443. [DOI] [PubMed] [Google Scholar]
- [58].Iyanoye A, Moreyra AE, Swerdel JN, et al. Gender disparity in the use of drug -eluting stents during percutaneous coronary intervention for acute myocardial infarction. Catheter Cardiovasc Interv 2015;86:221–8. [DOI] [PubMed] [Google Scholar]
- [59].Wiviott SD, Cannon CP, Morrow DA, et al. Differential expression of cardiac biomarkers by gender in patients with unstable angina/non-ST-elevation myocardial infarction: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy-Thrombolysis In Myocardial Infarction 18) substudy. Circulation 2004;109:580–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


