Abstract
This study retrospectively evaluated the effectiveness and safety of traditional Chinese medicine Shenqilixin Formula (SQLXF) as an adjunctive intervention for treating patients with chronic heart failure (CHF).
This retrospective study included 135 patients with CHF. They were allocated to a treatment group or a control group according to the different treatments they received. Seventy five patients in the treatment group underwent SQLXF plus routine treatment, while 60 subjects in the control group received routine treatment only. The primary outcome was cardiac function. It was measured by the left ventricular end diastolic diameter (LVDD), left ventricular ejection fraction (LVEF), cardiac output (CO), every cardiac output (ECO), and cardiac index (CI). The secondary outcome included motor function. It was measured by the standard 6-MinuteWalk Test (6MWT). In addition, adverse events (AEs) were also recorded.
Compared to subjects in the control group, patients in the treatment group revealed greater effectiveness in cardiac function, measured by LVEF (P < .05), CO (P < .05), and ECO (P < .05), and motor function, measured by the 6MWT scale (P < .05). Moreover, no significant differences of AEs were found between the 2 groups.
SQLXF as an adjunctive therapy to routine treatment may help to improve both cardiac and motor function in patients with CHF.
Keywords: chronic heart failure, effectiveness, Shen Qi Li Xin formula
1. Introduction
Chronic heart failure (CHF) is a very common condition among the cardiology diseases.[1–3] It is often associated with high mortality rates, frequent hospitalizations, and also the poor quality of life in patients with CHF.[4,5] Its prevalence rate is reportedly 26 million worldwide,[5] and more frequent with increasing age, with 10% among patients more than 70 years.[5–7] It affects nearly 4.2 million people from China with 1.3% prevalence rates.[8,9] The incidence of CHF has been reported as 0.7 to 0.9 per 1000 in the Chinese population.[10,11] Additionally, its incidence continues increasing in China because of the rapidly aging population.[8]
Its treatment focuses on managing symptoms improvement with lifestyle changing, taking medications and surgery. However, in many patients, CHF cannot be controlled with a single type of intervention, and most patients still suffer from poorly controlled CHF symptoms and poor quality of life.[12,13] It has been reported that regular treatment can effectively control CHF. However, it still has limited effectiveness.[14]
Complementary medicine, especially traditional Chinese medicine is an effective alternative treatment for patients with CHF.[15–24] Of those, Shenqilixin Formula (SQLXF) has been used to treat patients with CHF in China with few adverse events (AEs).[19–24] However, there is still limit data of SQLXF for treating CHF. More clinical evidence is still needed to support its effectiveness and safety. Therefore, in this retrospective study, we evaluated the effectiveness and safety of SQLXF for treating Chinese patients with CHF.
2. Methods and materials
2.1. Ethic approval
This retrospective study was approved by the ethics committee of The First Affiliated Hospital of Heilongjiang University of Chinese Medicine. All patients provided written informed consent.
2.2. Study design
It was operated between January 2015 and November 2017 at The First Affiliated Hospital of Heilongjiang University of Chinese Medicine. Around 135 eligible patients with CHF were assigned to a treatment group (75 patients) or a control group (60 patients) according the different treatments they received. Patients in the treatment group received SQLXF as an adjunctive therapy to routine treatment, while subjects in the control group received routine treatment only.
2.3. Patients
All eligible patients with CHF and the symptoms of New York Heart Association (NYHA) functional class (II–IV) were included in this retrospective study.[25] All patients aged between 51 and 83 years. Patients were excluded if they had severe valve stenosis; cardiomyopathy (hypertrophy or restriction); pericarditis (constriction), myocarditis; acute myocardial infarction; cardiogenic shock; various malignancies, trauma, connective tissue disease, pregnancy and breastfeeding; severe liver, renal insufficiency. All outcomes were measured before and after 6 months treatment.
2.4. Intervention
All patients in both groups were administrated routine treatment according to clinical standard treatment of CHF, such as eating less salt, limiting fluid intake, and taking prescription medications. The prescription medications included trimetazidine hydrochloride for the improvement of myocardial energy metabolism; and aspirin and atorvastatin for the secondary prevention of coronary heart disease. Patients received these interventions based on the actual situation of patients with cardiac, diuretic and nitroprusside in order to improve heart failure. In addition, patients in the treatment group also received SQLXF (Ginseng 20 g, Astragalus 20 g, Cassia twig 10 g, Epimedium 15 g, Semen lepidii 20 g, Atractylodes 15 g, Motherwort 15 g, Poria 20 g, Atractylodes 15 g, Motherwort 15 g, Salvia 15 g, Agrimony 30 g, licorice 10 g),[19] once daily at every morning and evening time before meals, for a total of 6 months treatment.
SQLXF was provided by the Department of Medication Preparation of The First Affiliated Hospital of Heilongjiang University of Chinese Medicine with the Decoctable Packaging Machine (Donghua Decoction Machine: YF12/3+1, Beijing, China).[26] The prescribed herbal medication of SQLXF was put into the decoction machine. After decocting, each prescription was automatically divided into 2 bags, each bag 150 mL for one day consumption.
2.5. Outcome measurements
The primary outcome was cardiac function, measured by the left ventricular end diastolic diameter (LVDD),[27] left ventricular ejection fraction (LVEF),[28] cardiac output (CO),[29] every cardiac output (ECO),[30] and cardiac index (CI)[31] through the color Doppler echocardiography. The secondary outcomes included motor function, measured by the standard 6-MinuteWalk Test (6MWT),[32] and AEs related to the treatment of SQLXF. All the outcomes were measured before and after 6-month treatment.
2.6. Statistical analysis
Statistical Package for the Social Sciences (SPSS) software (version.17.0) was used to analyze all the characteristic values, and outcome data. The t-test or Mann–Whitney rank sum test was utilized to analyze continuous data; and Chi-square test test was used to analyze the categorical data. P < .05 was recommended as statistically significant.
3. Results
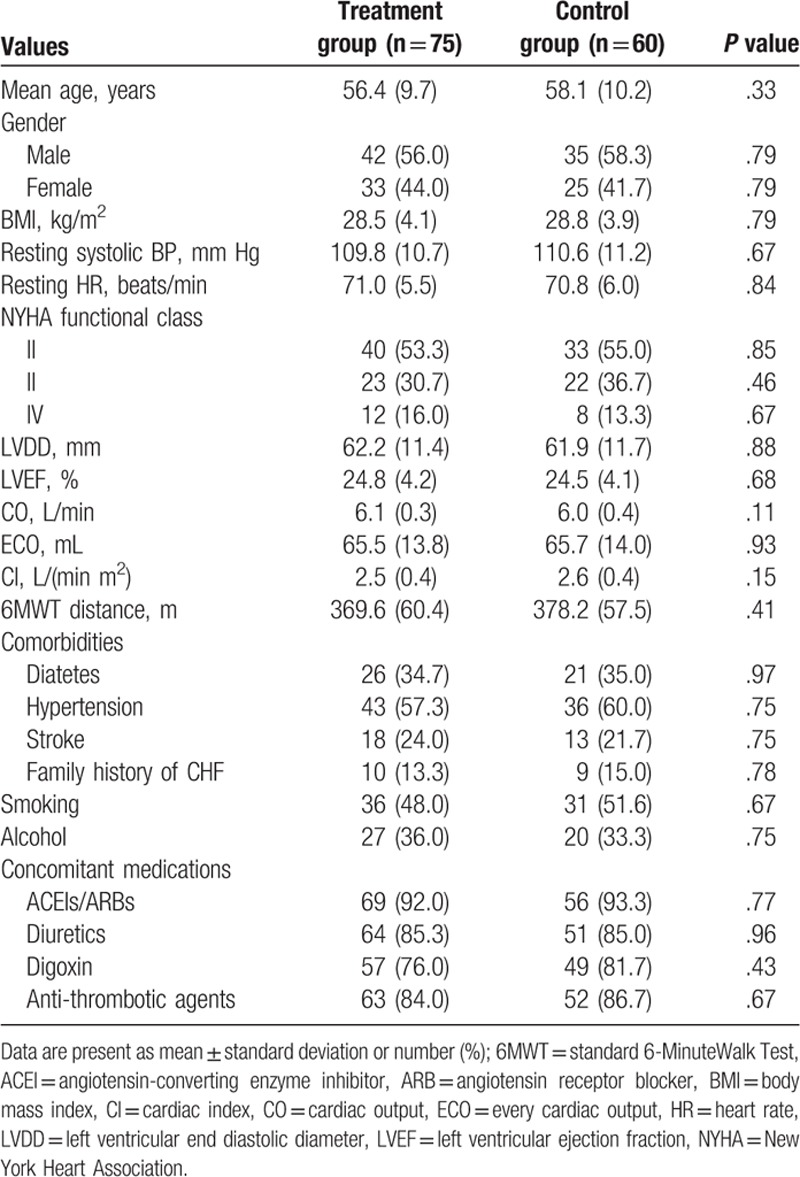
Around 135 patients were initially included in this retrospective study (Table 1). No significant differences of all characteristics were found before the treatment 2 groups (Table 1).
Table 1.
Characteristics of all eligible included patients.
All outcome evaluations are shown in Table 2. When compared to the patients in the control group, patients in the treatment group showed better effect in LVEF, CO, ECO, and 6MWT distance, respectively (P < .05), although the negative results of LVDD (P = 0.23) and CI (P = 0.31) were detected.
Table 2.
Primary and secondary outcomes after 6 months treatment.

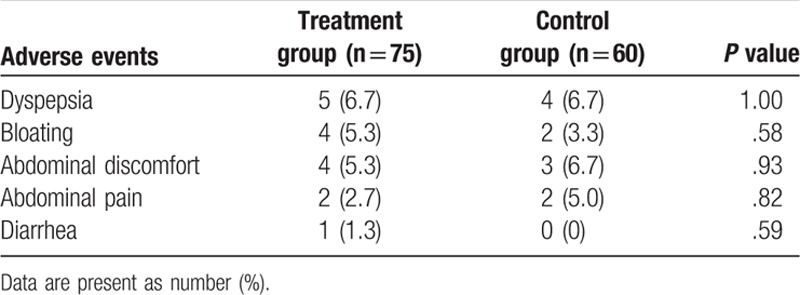
All AEs recorded in both groups are listed in Table 3. No significant differences in all AEs were found between the 2 groups. The most frequent AEs were dyspepsia, bloating, and abdominal discomfort. No death related to the treatment occurred.
Table 3.
Adverse events.
4. Discussion
Many factors can result in CHF, such as coronary heart disease, myocardial ischemia, myocardial infarction, cardiomyopathy, cardiac overload, and so on.[1,4,5] Initially, they may cause myocardial injury, then lead to ventricular filling and (or) ejection, and eventually develop to the CHF. Patients with such condition often involve in poor heart and motor function, and even the poor quality of life.[10]
SQLXF has been reported to treat CHF by several previous animal experimental and clinical studies.[19–24,33–38] Animal experimental studies found that SQLXF can effectively enhance cardiac function in CHF rats by regulating the energy metabolism of impaired cardiomyocytes, and the expression of mitochondrial uncoupling protein 2; improving myocardial tissue morphology, inhibiting ventricular remodeling, adenosine triphosphate, creatine phosphate and insulin resistance; reducing death rates of CHF rats, decreasing the expression of Caspase-3 and Caspase-9 in myocardium, the content of free fatty acids, and fasting blood glucose.[33–38] The results of clinical studies showed that SQLXF can improve the serum levels of Galectin-3, B-Brain natriuretic peptide, soluble intercellular adhesionmolecule-1 in patients with CHF. Moreover, it can also improve clinical symptoms, cardiac and motor function, as well as the quality of life in patients with such condition.[19–24]
The results of this study found that SQLXF with routine treatment was superior to routine treatment alone for treating CHF at the end of 6-month treatment. Our results are partly consistent with the previous studies,[19,20] which indicate that SQLXF may help to improve either the cardiac function, or the motor function in patients with CHF.
Our study also has 3 limitations. First, the achieved effectiveness was the results of the synergistic effectiveness of SQLXF with routine treatment, and not of SQLXF alone, although the baseline medications were similar between both groups. Second, it was difficult to discern whether the AEs were caused by SQLXF or routine treatment, because all patients in the treatment group underwent both medications. Third, the present study did not include the evaluation of the quality of life in patients with CHF. Further studies should avoid these limitations.
5. Conclusion
The results of the present study demonstrate that SQLXF as an adjunctive therapy to routine treatment may help to enhance both cardiac function and motor function in patients with CHF.
Author contributions
Conceptualization: Xiao-wei Deng, Yan-bo Sui, Qi-yuan Tian, Yi-qing Zhang.
Data curation: Xiao-wei Deng, Yan-bo Sui, Yi-qing Zhang, Ze-guang Li.
Investigation: Li Liu, Ze-guang Li.
Methodology: Li Liu.
Project administration: Yan-bo Sui, Yi-qing Zhang.
Resources: Yan-bo Sui, Yi-qing Zhang.
Software: Li Liu, Ze-guang Li.
Supervision: Xiao-wei Deng.
Validation: Xiao-wei Deng, Qi-yuan Tian, Yi-qing Zhang, Ze-guang Li.
Visualization: Xiao-wei Deng, Yan-bo Sui, Qi-yuan Tian, Yi-qing Zhang.
Writing – original draft: Xiao-wei Deng, Yan-bo Sui, Li Liu, Qi-yuan Tian, Yi-qing Zhang, Ze-guang Li.
Writing – review & editing: Xiao-wei Deng, Yan-bo Sui, Li Liu, Qi-yuan Tian, Yi-qing Zhang, Ze-guang Li.
Footnotes
Abbreviations: 6MWT = 6-MinuteWalk Test, AEs = adverse events, CHF = chronic heart failure, CI = cardiac, CO = cardiac output, ECO = every cardiac output, LVDD = left ventricular end diastolic diameter, LVEF = left ventricular ejection fraction, NYHA = New York Heart Association, SQLXF = Shenqilixin Formula.
Y-bS and Q-yT contribute equally to this study.
The authors have no conflicts of interest to disclose.
References
- [1].Hopper I, Easton K. Chronic heart failure. Aust Prescr 2017;40:128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Wang K, Wu J, Duan X, et al. Huangqi injection in the treatment of chronic heart failure: A systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e8167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Gu Q, Wu SJ, Zheng Y, et al. Tai Chi exercise for patients with chronic heart failure: A meta-analysis of randomized controlled trials. Am J Phys Med Rehabil 2017;96:706–16. [DOI] [PubMed] [Google Scholar]
- [4].Sun W, Zhang H, Guo J, et al. Comparison of the efficacy and safety of different ACE inhibitors in patients with chronic heart failure: a PRISMA-Compliant Network Meta-Analysis. Medicine (Baltimore) 2016;95:e2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail 2014;1:4–25. [DOI] [PubMed] [Google Scholar]
- [6].Kalter-Leibovici O, Freimark D, Freedman LS, et al. Disease management in the treatment of patients with chronic heart failure who have universal access to health care: a randomized controlled trial. BMC Med 2017;15:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Feola M, Testa M, Leto L, et al. Role of galectin-3 and plasma B type-natriuretic peptide in predicting prognosis in discharged chronic heart failure patients. Medicine (Baltimore) 2016;95:e4014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hung YT, Cheung NT, Ip S, et al. Epidemiology of heart failure in Hong Kong, 1997. Hong Kong Med J 2000;6:159–62. [PubMed] [Google Scholar]
- [9].Ademi Z, Pasupathi K, Liew D. Cost-effectiveness of eplerenone compared to usual care in patients with chronic heart failure and NYHA class II symptoms, an Australian perspective. Medicine (Baltimore) 2016;95:e3531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yang YN, Ma YT, Liu F, et al. Incidence and distributing feature of chronic heart failure in adult population of Xinjiang. Zhonghua Xin Xue Guan Bing Za Zhi 2010;38:460–4. [PubMed] [Google Scholar]
- [11].Tseng CH. Clinical features of heart failure hospitalization in younger and elderly patients in Taiwan. Eur J Clin Invest 2011;41:597–604. [DOI] [PubMed] [Google Scholar]
- [12].Wang Q, Dong L, Jian Z, et al. Effectiveness of a PRECEDE-based education intervention on quality of life in elderly patients with chronic heart failure. BMC Cardiovasc Disord 2017;17:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hua CY, Huang Y, Su YH, et al. Collaborative care model improves self-care ability, quality of life and cardiac function of patients with chronic heart failure. Braz J Med Biol Res 2017;50:e6355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wang SH, Mao JY, Hou YZ, et al. Routine western medicine treatment plus qishen yiqi dripping pill for treating patients with chronic heart failure: a systematic review of randomized control trials. Zhongguo Zhong Xi Yi Jie He Za Zhi 2013;33:1468–75. [PubMed] [Google Scholar]
- [15].Wang L, He Y, Zhang Y, et al. Effects of active components of Fuzi and Gancao compatibility on Bax, Bcl-2, and Caspase-3 in chronic heart failure rats. Evid Based Complement Alternat Med 2016;2016:7686045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Luo L, Chen J, Guo S, et al. Chinese herbal medicine in the treatment of chronic heart failure: three-stage study protocol for a randomized controlled trial. Evid Based Complement Alternat Med 2015;2015:927160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cui X, Zhang J, Li Y, et al. Effects of Qili Qiangxin capsule on AQP2, V2R, and AT1R in rats with chronic heart failure. Evid Based Complement Alternat Med 2015;2015:639450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Zick SM, Blume A, Aaronson KD. The prevalence and pattern of complementary and alternative supplement use in individuals with chronic heart failure. J Card Fail 2005;11:586–9. [DOI] [PubMed] [Google Scholar]
- [19].Wu L, Su Y, Tian ZK, et al. Effect of Shenqi Lixin formula on serum galectin-3 and BNP expression in patients with chronic heart failure. Zhong Yi Yao Zhong Xue 2016;33:49–52. [Google Scholar]
- [20].Sun XP, Liu L, Zou GL, et al. Clinical observation on treatment of 60 cases of chronic heart failure with modified Shenqi Yixin Decoction. Zhong Yi Yao Si Jie 2013;30:87–9. [Google Scholar]
- [21].Li L, Gao Q, Dou JJ. Observation on the therapeutic effect of Lixin I in treating congestive heart failure—effect of serum sICAM-1 concentration and 6-minute walk test. J Liaoning Coll Trad Chin Med 2009;36:19–20. [Google Scholar]
- [22].Zou GL, Zhong WL, Sui YB, et al. Effects of blood circulation and hydrotherapy on cardiac function and serum NT-proBNP levels in patients with left ventricular ejection fraction with normal heart failure Chinese. J Integr Trad West Med 2014;34:146–8. [PubMed] [Google Scholar]
- [23].Jiang YP, Liu L, Zhao XX, et al. Clinical observation on treatment of chronic heart failure with deficiency of heart and kidney with modified shenqi yixin prescription. J Liaoning Coll Trad Chin Med 2017;19:171–4. [Google Scholar]
- [24].Liu L, Hu S, Sui Y, et al. Effect of Yiqi Yangyang and Huoxue-Li-Shui method on congestive heart failure and its effect on insulin resistance. Shaanxi Coll Trad Chin Med 2013;36:33–6. [Google Scholar]
- [25].Raphael C, Briscoe C, Davies J, et al. Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart 2007;93:476–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chen WX, Peng ZS, Ye SL, et al. Comparative study on the decocting rate of the decocting agent of the YF12/3+1 type decocting machine and the traditional method in our hospital. Med Theory Pract 2012;25:2175–6. [Google Scholar]
- [27].Belenkie I. Beat-to-beat variability of echocardiographic measurements of left ventricular end diastolic diameter and performance. J Clin Ultrasound 1979;7:263–8. [DOI] [PubMed] [Google Scholar]
- [28].Burstein B, Jayaraman D, Husa R. Early left ventricular ejection fraction as a predictor of survival after cardiac arrest. Acute Card Care 2016;18:35–9. [DOI] [PubMed] [Google Scholar]
- [29].Agostoni P, Cattadori G. Noninvasive cardiac output measurement: a new tool in heart failure. Cardiology 2009;114:244–6. [DOI] [PubMed] [Google Scholar]
- [30].Raissuni Z, Zores F, Henriet O, et al. Can we obtain a noninvasive and continuous estimation of cardiac output? Comparison between three noninvasive methods. Int Heart J 2013;54:395–400. [DOI] [PubMed] [Google Scholar]
- [31].Carlsson M, Andersson R, Bloch KM, et al. Cardiac output and cardiac index measured with cardiovascular magnetic resonance in healthy subjects, elite athletes and patients with congestive heart failure. J Cardiovasc Magn Reson 2012;14:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Morard MD, Bosquet L, Laroche D, et al. Are first ventilatory threshold and 6-minute walk test heart rate interchangeable? A pilot study in healthy elderlies and cardiac patients. Ann Phys Rehabil Med 2015;58:92–7. [DOI] [PubMed] [Google Scholar]
- [33].Hu MX, Liu L. Effect of Shenqi yin xin decoction on energy metabolism of H9C2 myocardial cells. Chin Med Pharmacol 2013;20:590–1. [Google Scholar]
- [34].Jin J, Cui L, Zou GL, et al. Effects of Shenqi Yixin recipe on myocardial structure and cytokines in rats with chronic congestive heart failure induced by adriamycin. Acta Metallurgica Sinica 2014;20:128–32. [Google Scholar]
- [35].Jin J, Ma LQ, Zou GL, et al. Effects of Shenqi Yixin recipe on the expression of caspase-3 and caspase-9 in myocardial tissue of chronic congestive heart failure. Zhong Guang Xi Yi Jie He Za Zhi 2014;9:151–5. [Google Scholar]
- [36].Zou GL, Li JZ, Dai XM, et al. Effect of Shenqi Yixin Recipe on mitochondrial uncoupling protein 2 in cardiomyocytes of rats with heart failure. J Trad Chin Med 2017;36:231–3. [Google Scholar]
- [37].Li W, Li L, Sui YB, et al. Effects of Shenqi Yixin decoction on myocardial metabolism and remodeling in CHF rats. Zhong Yi Yao Si 2014;31:102–4. [Google Scholar]
- [38].Liu L, Zhu L, Jia J, et al. Effect of Shenqi Yixin decoction on cardiac function and insulin resistance in rats with congestive heart failure. Jinlin Chin Med J 2013;33:497–8. [Google Scholar]


