Abstract
Penetrating foreign bodies of different origins in the head and neck are rare and potentially dangerous injuries, which might pose problems for their detection, primary care, and final treatment. Depending on the severity of the underlying trauma, some injuries present a higher risk for the presence of foreign bodies. Minor wounds, including common lacerations, are likely to be contaminated with loose gravel debris or dental fragments, and need to be distinguished from severe wounds caused by impalement, shootings, stabbings, and explosions. Blast injuries resulting from terror attacks are challenging recent therapeutic concepts. Even though these injury patterns are uncommon, they carry the risk of impacted objects with dramatic consequences. Despite improving medical imaging techniques, detection remains a challenge as it is dependent on the material of the foreign body, the affected anatomical site, and the injury severity. Therefore, a detailed history of the circumstances leading to trauma is essential when foreign objects are not visible during clinical examination. Precise detection of the foreign body, its anatomical position, and the affected surrounding structures are vital, especially for impalement injuries of the head and neck area. Therefore, an interdisciplinary planning approach is essential prior to removal of the foreign object. Finally, tension-free anatomical adaptation of the corresponding structures is crucial for maintaining and restoring aesthetic and function. Here, we give an overview of the diagnosis and treatment of cases of foreign body injuries encountered in our department.
Keywords: foreign body, impalement injury, Jael's syndrome, head and neck surgery, craniomaxillofacial surgery
Injuries associated with foreign bodies in the head and neck area can occur at all stages of life, and show a heterogeneous etiology. The severity and risk for foreign bodies differs between injuries, and is dependent on the underlying trauma. In addition to a detailed medical history, thorough clinical examination and radiological assessment are crucial for the successful detection of clinically unapparent foreign bodies. In some cases, the foreign body might be visible without further diagnostics; however, in many cases the foreign body is not clinically apparent. For this reason, even though it is not visible upon initial evaluation, the surgeon needs to be aware of the potential risk of the existence of foreign bodies.
Bagatelle traumas (e.g., abrasion wounds) that exhibit superficial dirt particles and gravel debris, which can lead to dirt tattoos if wound cleaning is insufficient, represent the majority of cases seen in the emergency unit, and are generally easy to manage. 1
However, more severe traumatic injuries, including occupational and domestic accidents, assaults, and suicide attempts, represent a major cause for the occurrence of penetrating foreign bodies. Less common injuries, such as impalement injuries and wounds associated with bombings and blasts, gun and rifle shots, and stabbings, bear the risk of impacted objects and are often life-threatening. 2 3 4 These injuries need to be distinguished from ordinary injuries related to foreign bodies due to the complexity of diagnostics and treatment. Even though these causes of penetrating foreign body injuries are unusual in central Europe, surgeons of the head and neck area, including otorhinolaryngologists, radiologists, neurosurgeons, and craniomaxillofacial surgeons, need to be aware of the management and care of these dramatic injuries due to their increasing incidence meanwhile. 5 The foreign body material of theses wounds is often difficult to access especially in cases of close anatomical location to vital structures, 6 which may have a limited or fatal prognosis. 7
The following case series provide an overview of the diagnostics and treatment of dramatic foreign bodies of the head and neck area.
Case Series
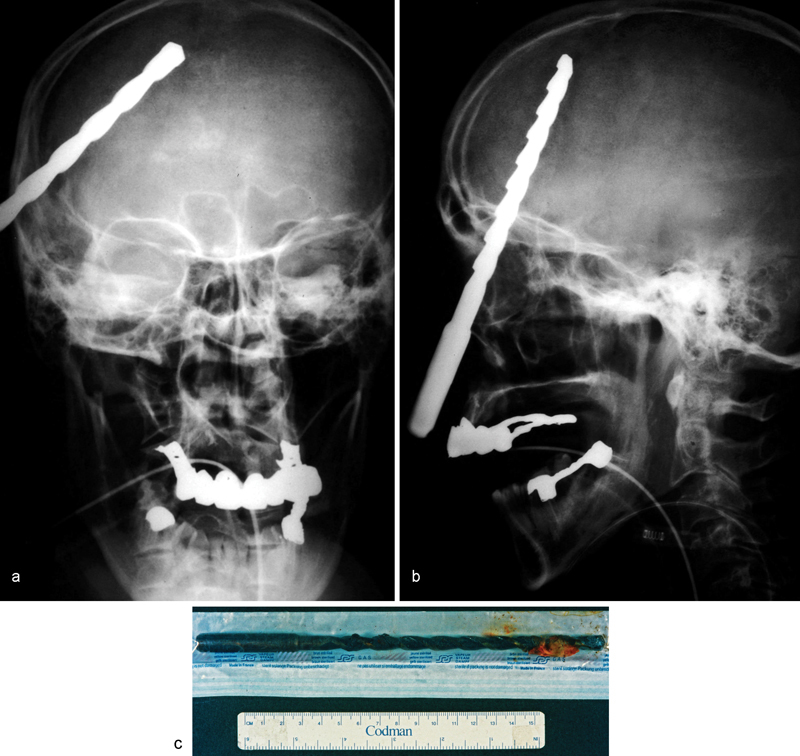
Case 1 : A 42-year-old patient was admitted to the emergency department after being hit by an Allen wrench at work. The impacted tool had penetrated the right orbit through the lower eyelid ( Fig. 1a ). Multidetector computed tomography (MDCT) imaging confirmed a close proximity of the foreign object to the ocular bulb and the skull base, although neither of these structures appeared to be affected ( Fig. 1b ). The patient was immediately taken into operating theater. Under general anesthesia, the penetration was extended by infraorbital incision to achieve a direct view of the orbit. In cooperation with ophthalmologists, the 8 × 1 cm tool was completely removed ( Fig. 1c ). The postoperative outcome was uneventful with no visual impairment or diplopia.
Case 2 : A 4-year-old girl was admitted to the emergency department after tripping while holding a key in her hands, ramming the foreign object into her cheek. Radiological examination confirmed perforation of the left maxillary sinus ( Fig. 2a ). Surgical removal of the key was performed under general anesthesia ( Fig. 2b ). The anterior wall of the maxillary sinus was flipped back without the need for osteosynthetic stabilization due to the young age of the patient. Wound healing showed no sequela.
Case 3 : A 64-year-old patient shot himself by accident while handling a self-made rat trap in Turkey. Four days later, the patient travelled back to Germany on his own and visited the emergency department. Aside from multiple skin lesions, mainly around the periorbital region, clinical examination including ophthalmological assessment was uneventful, with the patient reporting only slightly blurred vision. Conventional X-ray demonstrated the presence of multiple shotgun projectiles throughout the soft tissue of his face ( Fig. 3a , b ). In total, 46 projectiles were removed transcutaneously guided by intraoperative navigation and a C-arm X-ray, and assisted by ophthalmologists ( Fig. 3c ). One projectile, located close to the superior orbital fissure, was left in place to prevent further damage ( not shown ). Postoperatively, the patient's sight was undisturbed and healing proceeded normally. To our knowledge, no complications related to the remaining projectile have been noted.
Case 4 : Another case of a foreign body caused by a gunshot was presented by a 63-year-old patient. Clinically, a single entry wound was detectable in the forehead, but there was no bullet exit wound. An MDCT scan revealed a single bullet close to the occipital bone, which had entered the cranium through the forehead, crushing the frontal sinus and ethmoid cells ( Fig. 4a ). A bullet with a 2-cm diameter was removed by craniotomy in cooperation with colleagues from the neurosurgery department ( Fig. 4b ). Wound therapy included debridement with large exposure of the frontal sinus, reconstruction and fixation of the anterior wall, and dura repair under a perioperative antibacterial regime. Shortly after removal, the patient was transferred to begin neurological rehabilitation.
Case 5 : A dramatic case of a shooting was presented by a 50-year-old patient, who was found in his apartment with severe injuries to his midface. The patient had attempted to commit suicide by positioning a gun to his right temple. Due to excessive bleeding and insufficient respiration, the patient was intubated and transferred to the hospital. At the time of arrival, the patient presented unstable blood circulation with hypotension, which was treated by intensive blood transfer and transfusion management with the administration of catecholamines. A cranial MDCT scan confirmed the severe injuries of the patient, which included extensive destruction of the midface including the orbits and ocular bulb, in addition to the presence of multiple projectile fragments and dislocated intracranial bone fragments ( Fig. 5a , b ). Furthermore, intracranial bleeding, fracture of the skull base, and a pneumocephalus were also present. The condition of the patient subsequently deteriorated with a poor prognosis, and the patient died without any further intervention.
Case 6 : A 53-year-old patient suffered an impalement injury with a metallic drill, which had penetrated his neurocranium. The patient had tried to commit suicide, injuring himself in the thorax and head ( Fig. 6a , b ). MDCT imaging displayed the position of the impacted drill, which had entered the skull at the front temporal cortex, and there was also an injury of the lung parenchyma ( not shown ). Following immediate thoracotomy to stabilize the patient, the drilling device was completely removed by osteoclastic trepanation performed by our colleagues in the neurosurgery department ( Fig. 6c ). However, the patient subsequently died due to increased cerebral edema and severe damage to the brain parenchyma.
Case 7 : Another impalement injury, also known as a Jael's syndrome, 8 was presented by a 38-year-old psychiatric patient who had attempted to commit suicide by stabbing himself in the face with a knife. Clinical examination and radiological imaging of the patient displayed an intracranial penetrating stab injury, which had entered the neurocranium supraorbitally ( Fig. 7a , b ). The impacted knife was removed via craniotomy and dura repair in cooperation with the neurosurgery department. No injury to the greater intracranial vessels was detectable. Postoperative wound healing proceeded without any complains.
Case 8 : A 22-year-old patient was picked up by an ambulance complaining of facial pain in his right midface. Several months prior, the patient had suffered a blast injury, which caused the loss of his right eye during an armed conflict in Syria, where initial treatment had been performed. Clinically, the patient presented a large scar that extended from his lower right eye to his right nostril. Intranasal examination revealed a purulent foreign object in the nasopharynx. Conventional X-ray followed by an MDCT scan revealed a radiopaque mass in the central midface region, which did not affect the frontobasal region ( Fig. 8a , b ). A cerebral angiogram showed close proximity to the carotid arteries, but without any obvious injury ( Fig. 8c ). Antibiogram revealed multidrug-resistant gram-negative pathogens including Escherichia coli and Pseudomonas aeruginosa . A large piece of shrapnel measuring 8 × 3 × 3.5 cm ( Fig. 8d ) was removed under perioperative antibacterial treatment with endotracheal general anesthesia by performing an incision along the preexisting scar of the cheek and through the existing defect in the maxillary sinus. Following surgical removal, the postoperative outcome included no sequela, and rehabilitation was achieved with ocular prosthesis.
Case 9 : A critically injured 58-year-old patient with severe trauma resulting from a close explosion was transferred from a hospital in Egypt. Aside from a pneumothorax with respiratory insufficiency, the patient had also suffered multiple severe burn wounds on his hands and face. Clinically, the patient presented a complete mobile midface with an open wound on his right cheek and a pus-secreting open wound under his lower right eyelid that penetrated into his nasal cavity. The MDCT imaging revealed a complex panfacial fracture with a comminuted central midface and angulus fracture of his left mandible. Furthermore, a hyperdense foreign body was visible in his left cheek ( Fig. 9a , b ). After stabilization of the patient, surgical treatment, including thorough wound cleaning and insertion of drainage systems, temporary fracture reduction, and the removal of a metal object, was carried out ( Fig. 9c ). The foreign body had penetrated the patient's right cheek, exiting intraorally to also penetrate the left cheek and crush the left angulus. Due to the serious bacterial infection, as indicated by the detection of Klebsiella pneumoniae in the cerebrospinal fluid, extensive antibiotic regimes were initiated including intrathecal administration (as a treatment of last resort). However, the patient subsequently died due to multiple organ failure under progressive sepsis.
Fig. 1.
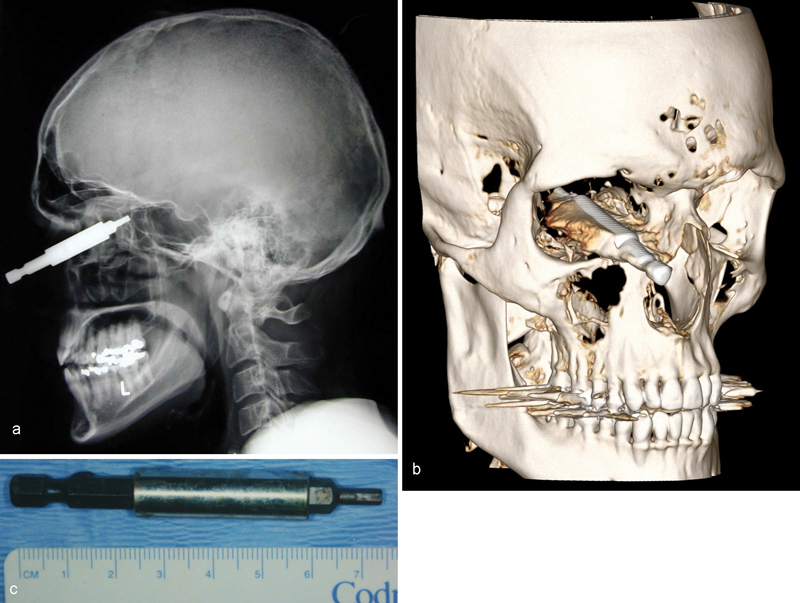
( a ) Lateral skull radiograph showing a radiopaque foreign object penetrating the orbital funnel close to the skull base. ( b ) Three-dimensional reconstruction of a multidetector computed tomography scan demonstrating the position of the Allen wrench inside the orbital funnel. ( c ) Postoperative image of the removed Allen wrench.
Fig. 2.

( a ) Lateral skull radiograph showing the radiopaque object penetrating the maxillary sinus. ( b ) Postoperative image of the removed key.
Fig. 3.
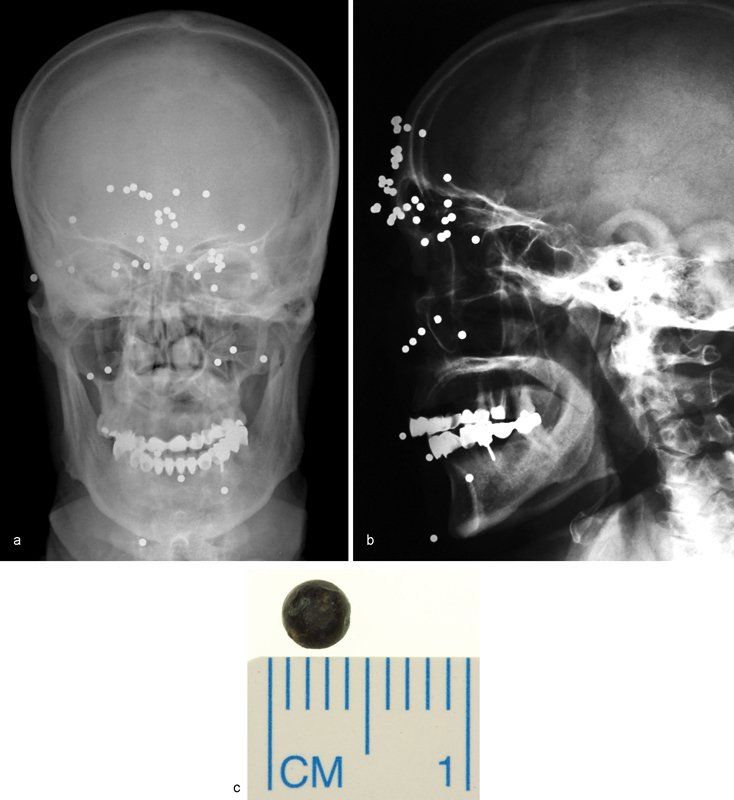
( a and b ) Frontal and lateral skull radiographs showing multiple radiopaque round foreign bodies spread over the face entering the orbital funnel. ( c ) Postoperative picture of a single shotgun pellet.
Fig. 4.
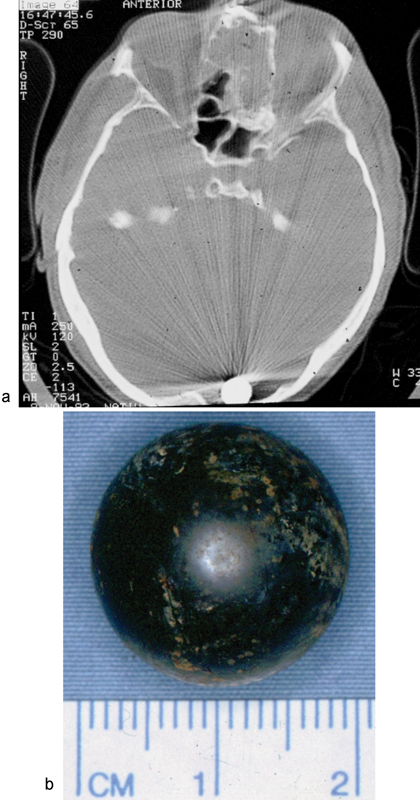
( a ) Intraoperative C-arm radiograph showing destruction of the ethmoidal bone with opacity, as well as a radiopaque intracranial foreign object close to the occipital bone. ( b ) Postoperative image of the removed bullet.
Fig. 5.
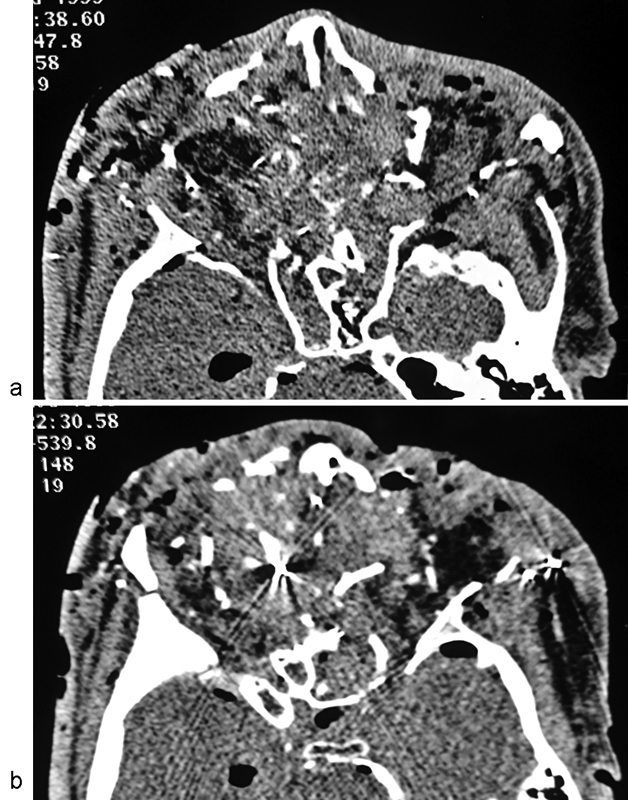
( a and b ) Axial multidetector computed tomography scan revealing massive destruction with comminuted fracture of the orbital region, in addition to hyperdense foreign bodies and artifacts.
Fig. 6.
( a and b ) Frontal and lateral skull radiographs showing a radiopaque foreign body penetrating intracranially. ( c ) Postoperative image of the metallic drill.
Fig. 7.
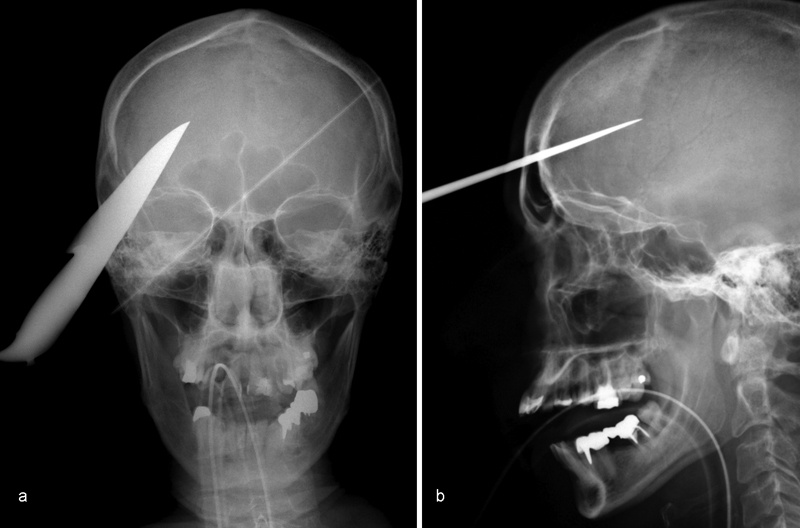
( a and b ) Lateral and frontal skull radiographs showing a radiopaque foreign body penetrating into the neurocranium.
Fig. 8.
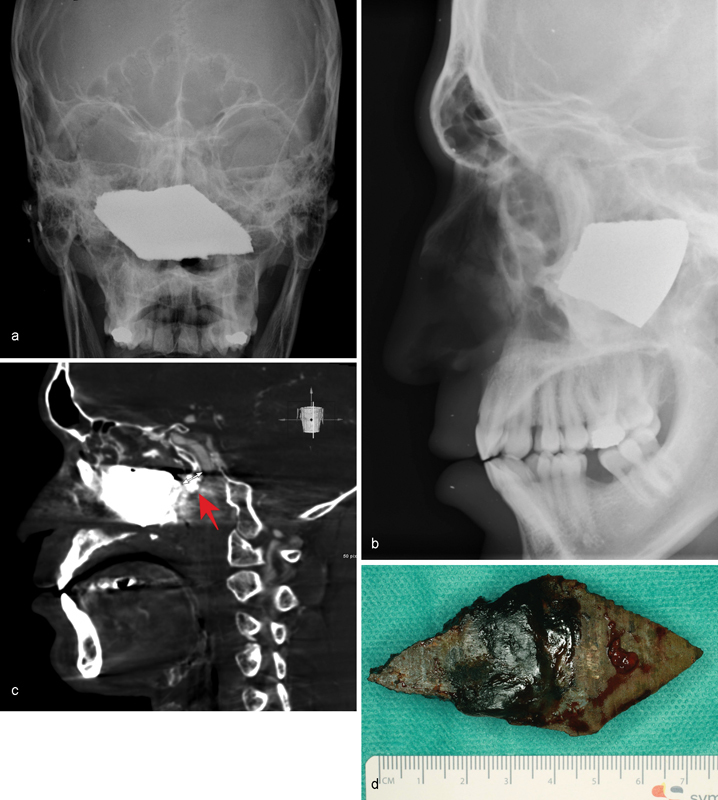
( a and b ) Frontal and lateral skull radiographs illustrating a large radiopaque mass in the center of the bony midface. ( c ) Angiogram showing the close proximity of the foreign body to the internal carotid artery. ( d ) Postoperative image of the shrapnel.
Fig. 9.
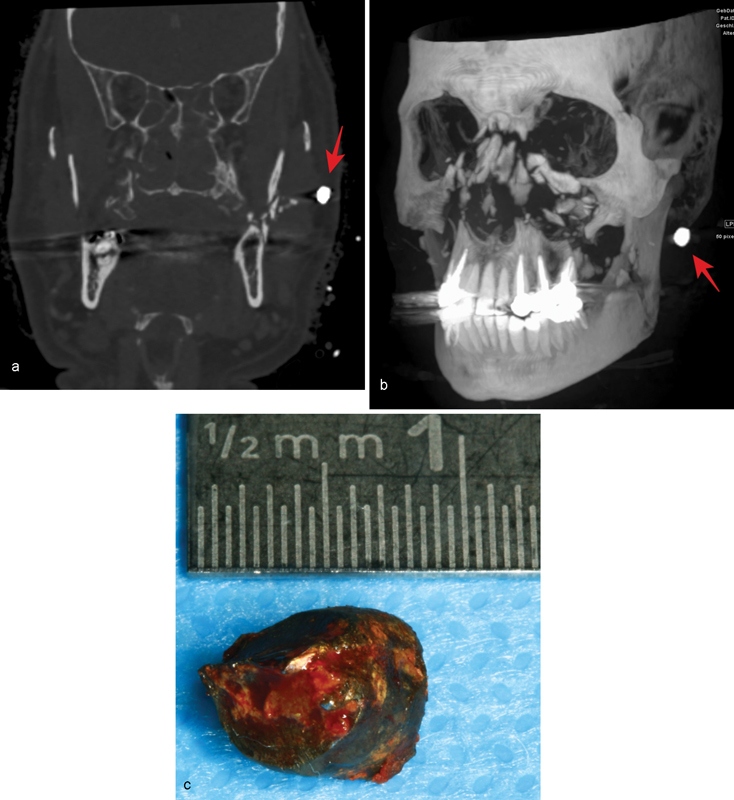
( a ) Axial multidetector computed tomography scan showing a fractured ascending left ramus with a hyperdense structure. ( b ) Three-dimensional reconstruction of a multidetector computed tomography scan revealing a central comminuted midfacial fracture with a hyperdense foreign object. ( c ) Postoperative image of the foreign object.
Discussion
Craniomaxillofacial surgeons are frequently confronted with foreign body injuries caused by a diversity of different trauma. In our patient population, the main causes included occupational ( case 1 ), domestic ( cases 2 and 3 ), and suicide attempts ( cases 4, 5, 6, and 7 ). Moreover, as mentioned in cases 8 and 9 , due to the rising number of refugees and the transfer of seriously injured patients from combat zones, as well as the increase in global terroristic attacks, special attention should be paid to injuries caused by destructive weapons and explosives. 9 In most cases, foreign bodies were associated with minor trauma, including small lacerations or open wounds, although foreign body injuries may also be severe, as demonstrated in some of our cases.
In general, injuries of the head and neck are potentially life-threatening depending on the location and extent of penetration of the foreign body. 10 11 12 Penetration injuries with or without impalement of the foreign object into the oral cavity, paranasal sinus, neurocranium, or neck risk injury to large vessels, airways, and crucial neurological structures, which present severe consequences for the patient. 13 Based on a biblical narrative about the murder of Sisera, an impalement injury of the craniofacial region is often referred to as Jael's syndrome. 8 As illustrated in cases 6 and 7 , these injuries are potentially life-threatening as they penetrate into the neurocranium. Furthermore, deep impaction of the foreign object and damage to vital structures also pose complications for its removal. 2
Acute Care
The acute treatment regime is dependent on the initial overall condition of the patient. Patients with life-threatening injuries are stabilized with advanced life support by securing the airways and managing blood loss/bleeding to maintain a sufficient blood supply. 14 15 There are differences in the injury patterns of pediatric patients and, therefore, possible variations in the therapeutic regime should be considered. 16
In primary care (first aid response), it is important that foreign bodies be left in place until diagnostics with radiological assessment is available, as the foreign bodies might act as a tamponade preventing severe bleeding. 15 17 Hasty removal without precise knowledge of the exact anatomical location and impaired surrounding structures might have disastrous consequences.
The diagnosis of foreign materials is challenging, especially in cases where the object is not fully visible. Besides a detailed medical history (if possible), clinical examination is crucial for the successful detection of foreign bodies. This is particularly important for small foreign bodies, for which soft tissue examination is essential for the detection and removal of the object. 18 19 In infants and children, full examination should be performed under general anesthesia, 20 as noncompliance might lead to incomplete assessment.
Radiological Assessment
Radiological assessment (conventional X-ray, ultrasound, MDCT, or magnetic resonance imaging [MRI]) should be adapted to the expected material of the foreign body (wood, glass, metal, tooth, debris, etc.) to minimize the risk of false-negative findings. 21 To address this, several studies have evaluated the efficiency of detecting foreign bodies by different radiological methods. 22 23 In general, MDCT imaging is most successful for detecting the majority of foreign bodies; however, it struggles with wooden objects. 24 Moreover, preoperative radiological assessment including the implementation of contrast agents should be chosen to visualize possible damage to the surrounding vascular structures. 25 To rule out arterial dissection, an arterial phase scan can be performed when an MRI cannot be conducted due to ferromagnetic foreign bodies. Excessive bleeding requires further detection of the affected vessels, which should include a noncontrast, arterial contrast phase and venous contrast phase scan.
In cases where the object is not directly visible by imaging, attention should be paid to indirect signs including air bubbles, excessive soft tissue swelling, or abscess formation. In addition to the preoperative evaluation, intraoperative navigation and X-ray by C-arm provides excellent additional support for localization, as well as for the removal of debris particles from the soft tissue, including shotgun projectiles ( case 3 ). 26
Foreign Body Removal
In general, foreign bodies should be removed to avoid acute or chronic infection, as well as an immune response. 27 Other indications include neurological impairment, mechanical and functional impairment, and compromised aesthetics. However, when considering the surgical removal of a foreign body, the risk of collateral damage and possible benefits should be considered. 28 Even though the existence of foreign bodies might be uneventful in some cases, and wounds with persisting foreign bodies may heal uneventfully in the first place, 29 sequela may occur, even many years later. 30 31 32
In many cases, small, subdermal objects can be removed under local anesthesia. However, in cases of deeply embedded, large objects, we believe general anesthesia should be chosen due to the risk of excessive bleeding after removal, edema, and complications by the movements of the patient. 33
Large abrasion wounds contaminated with loose gravel debris require diligent brushing in the emergency setting to avoid unaesthetic dirt tattoos. Besides thorough wound cleaning, these wounds require the use of drainage systems to allow drainage of wound fluid. Nonhealing wounds with chronic infections often indicate persisting remnants. In these cases, a second-look surgery is essential for undisturbed healing. 34 35 In cases of intracranial perforating foreign bodies, osteoclastic trepanation, craniotomy, and craniectomy offer different advantages for removing the foreign body. 36 37 Overall, optimal planning of foreign body removal is crucial for preservation and restoration of the surrounding anatomical structures. Precise reconstruction of soft tissue injuries will help achieve the best possible outcome in regard to form, function, and aesthetics, ensuring optimal rehabilitation.
Systemic Therapy
In addition to a sufficient tetanus prophylaxis, perioperative antibacterial therapy is crucial for preventing infections caused by contaminated foreign bodies and should be started as soon as possible. Petersen and Waterman published a comprehensive overview of prophylaxis and treatment of infections associated with various penetrating traumatic injuries of the head and neck. An intravenous therapy with cefazolin (2 g every 8 hours) or a combination of ampicillin and sulbactam (2 g every 6 hours) should be administered for 10 to 14 days in cases of maxillofacial infection. 38
Exceptional Cases: Gunshot and Blast Injuries
Special attention should be paid to the treatment of self-inflicted gunshot or rifle injuries, as these wounds might exhibit severe powder burns and a large degree of destruction due to the high velocity of the bullet and close proximity of the gun. Therefore, these injuries, in particular, require diligent cleaning and reconstructive treatment ( cases 3, 4, and 5 ). 3 39 40
Another injury pattern is presented by victims of blast injuries, caused by a variety of improvised explosive devices (IEDs) in the context of terror attacks or acts of war ( cases 8 and 9 ). While the majority of these injuries primarily occur during war-related conflicts, the incidence of terror attacks that utilize IEDs has increased. These IEDs cause severe trauma with a higher frequency of penetrating injuries, as well as mortality rate, in the less protected civilian population. 15 41 42 Craniomaxillofacial surgeons, head and neck surgeons, neurosurgeons, and radiologists need to be aware of this type of injury as global terrorism becomes a greater concern.
Similar to gunshots wounds, these injuries often exhibit large destruction of soft tissue as well as comminuted bone fractures, with a high risk of wound contamination, severe burns, and penetrating injuries. 5 14 Suicide bombers try to maximize the number of casualties by adding extra metal particles (screws, nails, steel balls, etc.) into the IEDs, which pose a great risk for penetrating into the victims' bodies. Penetrating injuries are considered so-called secondary blast injuries caused by blast-energized fragments including IED particles, shrapnel, explosive debris components, and environmental debris. 5 43 44 These traumas carry the risk of severe bleeding from damage to the large vessels of the head and neck, thereby compromising the patient's airways. 15 Therefore, aggressive bleeding control and maintaining and restoring airways with early tracheotomy or coniotomy are often necessary. 15 After stabilizing vital signs, the patient should be transferred to a major trauma department with neurosurgery, head and neck surgeons, and ophthalmologists. Radiological assessment is critical in the following diagnostic approaches as inconspicuous wounds might cover up large pieces of shrapnel. 41 45
The treatment of these injuries requires a diligent approach, initially focusing on precise wound cleaning and soft tissue management, including the reconstruction of vulnerable nerve structures and blood vessels and removal of foreign body material. However, it is important to keep in mind that every case is unique, requiring individual steps and diligent consideration in regard to the best therapeutic regime.
Due to the high chance of bacterial contamination of these wounds, antibacterial treatment is critical, as illustrated in cases 8 and 9 . 46 Fracture stabilization and fixation represents the basis for restoring form and function. Aesthetic correction might take place after primary wound healing depending on the overall outcome of the patient. 14
In summary, depending on the location and injury pattern of penetrating injuries of the head and neck, interdisciplinary collaboration with colleagues from different specialties including ophthalmology, otolaryngology, and neurosurgery is required. Besides impalement injuries, even wounds that appear inconspicuous bear the risk of foreign body material; therefore, diligent clinical assessment and radiological diagnosis is important for a successful outcome. Overall, this study provides a comprehensive overview for the diagnostic and therapy of various penetrating injuries of the head and neck.
Acknowledgments
The article was language edited by Proof-Reading-Service.com (Letchworth Garden City, Hertfordshire, United Kingdom).
Conflict of Interest None declared.
Ethical Approval
Full ethical approval was granted by the ethical review committee of the Charité –Universitätsmedizin Berlin (EA2/084/17).
References
- 1.Antunes A A, Santos T S, Carvalho de Melo A U, Ribiero C F, Goncalves S R, de Mello Rode S. Tooth embedded in lower lip following dentoalveolar trauma: case report and literature review. Gen Dent. 2012;60(06):544–547. [PubMed] [Google Scholar]
- 2.Santos TdeS, Melo A R, de Moraes H H et al. Impacted foreign bodies in the maxillofacial region-diagnosis and treatment. J Craniofac Surg. 2011;22(04):1404–1408. doi: 10.1097/SCS.0b013e31821cc53e. [DOI] [PubMed] [Google Scholar]
- 3.Shvyrkov M B. Facial gunshot wound debridement: debridement of facial soft tissue gunshot wounds. J Craniomaxillofac Surg. 2013;41(01):e8–e16. doi: 10.1016/j.jcms.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Thach A B, Ward T P, Dick J S, II et al. Intraocular foreign body injuries during Operation Iraqi Freedom. Ophthalmology. 2005;112(10):1829–1833. doi: 10.1016/j.ophtha.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Wolf S J, Bebarta V S, Bonnett C J, Pons P T, Cantrill S V.Blast injuries Lancet 2009374(9687):405–415. [DOI] [PubMed] [Google Scholar]
- 6.Raska G M, Cordova S W, Lema R, Goldwasser M S. Management of penetrating trauma to the soft palate: a case report. J Oral Maxillofac Surg. 2007;65(07):1279–1285. doi: 10.1016/j.joms.2006.10.056. [DOI] [PubMed] [Google Scholar]
- 7.Olasoji H O, Tahir A A, Ahidjo A, Madziga A. Penetrating arrow injuries of the maxillofacial region. Br J Oral Maxillofac Surg. 2005;43(04):329–332. doi: 10.1016/j.bjoms.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 8.McKechnie J. A severe craniofacial impalement injury (Jael's syndrome) Br J Oral Maxillofac Surg. 1986;24(04):258–264. doi: 10.1016/0266-4356(86)90090-2. [DOI] [PubMed] [Google Scholar]
- 9.Brunner J, Singh A K, Rocha T, Havens J, Goralnick E, Sodickson A. Terrorist bombings: foreign bodies from the Boston Marathon bombing. Semin Ultrasound CT MR. 2015;36(01):68–72. doi: 10.1053/j.sult.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Powitzky R, Cordero J, Robinson M, Helmer R, Halldorsson A. Spectacular impalement through the face and neck: a case report and literature review. J Trauma. 2008;65(06):E53–E57. doi: 10.1097/01.ta.0000200857.68815.00. [DOI] [PubMed] [Google Scholar]
- 11.Khadivi E, Bakhshaee M, Khazaeni K. A rare penetrating neck trauma to zone III. Emerg Med J. 2007;24(12):840. doi: 10.1136/emj.2006.044586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borkar S A, Garg K, Garg M, Sharma B S. Transorbital penetrating cerebral injury caused by a wooden stick: surgical nuances for removal of a foreign body lodged in cavernous sinus. Childs Nerv Syst. 2014;30(08):1441–1444. doi: 10.1007/s00381-014-2364-0. [DOI] [PubMed] [Google Scholar]
- 13.Mohan S, Varghese G, Kumar S, Subramanian D P. Penetrating facial injury by a wooden log. Natl J Maxillofac Surg. 2014;5(02):228–231. doi: 10.4103/0975-5950.154844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maier H, Tisch M, Lorenz K J, Danz B, Schramm A. Penetrating injuries in the face and neck region. Diagnosis and treatment [in German] HNO. 2011;59(08):765–782. doi: 10.1007/s00106-011-2349-1. [DOI] [PubMed] [Google Scholar]
- 15.Shuker S T. The immediate lifesaving management of maxillofacial, life-threatening haemorrhages due to IED and/or shrapnel injuries: “when hazard is in hesitation, not in the action.”. J Craniomaxillofac Surg. 2012;40(06):534–540. doi: 10.1016/j.jcms.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Martin W S, Gussack G S. Pediatric penetrating head and neck trauma. Laryngoscope. 1990;100(12):1288–1291. doi: 10.1288/00005537-199012000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Ursic C, Curtis K. Thoracic and neck trauma. Part four. Int Emerg Nurs. 2010;18(04):177–180. doi: 10.1016/j.ienj.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Al-Jundi S H. The importance of soft tissue examination in traumatic dental injuries: a case report. Dent Traumatol. 2010;26(06):509–511. doi: 10.1111/j.1600-9657.2010.00925.x. [DOI] [PubMed] [Google Scholar]
- 19.Altundasar E, Demiralp B. The importance of soft tissue examination in post-traumatic decision-making: a case report. Aust Endod J. 2013;39(01):35–38. doi: 10.1111/j.1747-4477.2009.00216.x. [DOI] [PubMed] [Google Scholar]
- 20.Tandon P N, Gupta D S, Jurel S K, Srivastava S, Sharma S. Penetrating injury of face by a large machine bolt-a rare case report. J Maxillofac Oral Surg. 2015;14 01:100–102. doi: 10.1007/s12663-012-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faguy K.Imaging foreign bodies Radiol Technol 20148506655–678., quiz 679–682 [PubMed] [Google Scholar]
- 22.Ingraham C R, Mannelli L, Robinson J D, Linnau K F. Radiology of foreign bodies: how do we image them? Emerg Radiol. 2015;22(04):425–430. doi: 10.1007/s10140-015-1294-9. [DOI] [PubMed] [Google Scholar]
- 23.Javadrashid R, Fouladi D F, Golamian M et al. Visibility of different foreign bodies in the maxillofacial region using plain radiography, CT, MRI and ultrasonography: an in vitro study. Dentomaxillofac Radiol. 2015;44(04):2.0140229E7. doi: 10.1259/dmfr.20140229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krimmel M, Cornelius C P, Stojadinovic S, Hoffmann J, Reinert S. Wooden foreign bodies in facial injury: a radiological pitfall. Int J Oral Maxillofac Surg. 2001;30(05):445–447. doi: 10.1054/ijom.2001.0109. [DOI] [PubMed] [Google Scholar]
- 25.Kieck C F, de Villiers J C. Vascular lesions due to transcranial stab wounds. J Neurosurg. 1984;60(01):42–46. doi: 10.3171/jns.1984.60.1.0042. [DOI] [PubMed] [Google Scholar]
- 26.Lorenz K J, Bockers A, Fassnacht U, Wilde F, Wegener M. Implementation of a miniaturised navigation system in head and neck surgery for the detection and removal of foreign bodies. Eur Arch Otorhinolaryngol. 2017;274(01):553–559. doi: 10.1007/s00405-016-4212-1. [DOI] [PubMed] [Google Scholar]
- 27.Yanay O, Vaughan D J, Diab M, Brownstein D, Brogan T V. Retained wooden foreign body in a child's thigh complicated by severe necrotizing fasciitis: a case report and discussion of imaging modalities for early diagnosis. Pediatr Emerg Care. 2001;17(05):354–355. doi: 10.1097/00006565-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Schulz M R, Glawe H, Siedschlag W D, Nisch G, Winkelmann H. Conservative or surgical treatment for foreign body injuries of the brain [in German] Zentralbl Neurochir. 1992;53(02):69–73. [PubMed] [Google Scholar]
- 29.Voss J O, Raguse J D, Hoffmeister B, Adolphs N. Magnetic resonance imaging induced acute midfacial pain - incidental finding of a dislocated dental bur. Eur J Oral Implantology. 2015;8(02):183–187. [PubMed] [Google Scholar]
- 30.Grevers G, Reiterer A. Traumatically-induced foreign bodies of the paranasal sinuses [in German] Laryngorhinootologie. 1990;69(03):155–157. doi: 10.1055/s-2007-998164. [DOI] [PubMed] [Google Scholar]
- 31.Rudagi B M, Halli R, Kini Y, Kharkhar V, Saluja H. Foreign bodies in facial trauma-report of 3 cases. J Maxillofac Oral Surg. 2013;12(02):210–213. doi: 10.1007/s12663-010-0072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vikram A, Mowar A, Kumar S. Wooden foreign body embedded in the zygomatic region for 2 years. J Maxillofac Oral Surg. 2012;11(01):96–100. doi: 10.1007/s12663-010-0161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Litvack Z N, Hunt M A, Weinstein J S, West G A. Self-inflicted nail-gun injury with 12 cranial penetrations and associated cerebral trauma. Case report and review of the literature. J Neurosurg. 2006;104(05):828–834. doi: 10.3171/jns.2006.104.5.828. [DOI] [PubMed] [Google Scholar]
- 34.Joyce S, Rao Sripathi B H, Mampilly M O, Firdoose Nyer C S. Foreign body granuloma. J Maxillofac Oral Surg. 2014;13(03):351–354. doi: 10.1007/s12663-010-0113-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bosman W M, Ritchie E D, da Costa S A. Cutaneous fistula due to remaining foreign bodies after penetrating neck injury. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-201278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carrillo-Ruiz J D, Juárez-Montemayor V, Méndez-Viveros A, Frade-García A, Bolaños-Jiménez R.Skull stab wound from a metal railroad nail perforating the right frontal lobe Brain Inj 201327(7–8):973–977. [DOI] [PubMed] [Google Scholar]
- 37.Luo W, Liu H, Hao S, Zhang Y, Li J, Liu B.Penetrating brain injury caused by nail guns: two case reports and a review of the literature Brain Inj 201226(13–14):1756–1762. [DOI] [PubMed] [Google Scholar]
- 38.Petersen K, Waterman P. Prophylaxis and treatment of infections associated with penetrating traumatic injury. Expert Rev Anti Infect Ther. 2011;9(01):81–96. doi: 10.1586/eri.10.155. [DOI] [PubMed] [Google Scholar]
- 39.Weisel G, Pillekamp H. Treatment of gunpowder tattoo and foreign bodies after blast injuries [in German] HNO. 2011;59(08):807–810. doi: 10.1007/s00106-011-2354-4. [DOI] [PubMed] [Google Scholar]
- 40.Yuksel F, Celikoz B, Ergun O, Peker F, Açikel C, Ebrinc S. Management of maxillofacial problems in self-inflicted rifle wounds. Ann Plast Surg. 2004;53(02):111–117. doi: 10.1097/01.sap.0000116304.70332.26. [DOI] [PubMed] [Google Scholar]
- 41.Mathews Z R, Koyfman A. Blast Injuries. J Emerg Med. 2015;49(04):573–587. doi: 10.1016/j.jemermed.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 42.Yeh D D, Schecter W P. Primary blast injuries--an updated concise review. World J Surg. 2012;36(05):966–972. doi: 10.1007/s00268-012-1500-9. [DOI] [PubMed] [Google Scholar]
- 43.Armstrong J H, Sullivent E E, Sasser S M. Blast injuries from bombings: what craniofacial and maxillofacial surgeons need to know. J Craniofac Surg. 2010;21(04):954–959. doi: 10.1097/SCS.0b013e3181e17b79. [DOI] [PubMed] [Google Scholar]
- 44.Singh A K, Buch K, Sung E et al. Head and neck injuries from the Boston Marathon bombing at four hospitals. Emerg Radiol. 2015;22(05):527–532. doi: 10.1007/s10140-015-1322-9. [DOI] [PubMed] [Google Scholar]
- 45.Singh A K, Ditkofsky N G, York J D et al. Blast Injuries: From Improvised Explosive Device Blasts to the Boston Marathon Bombing. Radiographics. 2016;36(01):295–307. doi: 10.1148/rg.2016150114. [DOI] [PubMed] [Google Scholar]
- 46.Hauer T, Huschitt N, Kulla M, Kneubuehl B, Willy C. Bullet and shrapnel injuries in the face and neck regions. Current aspects of wound ballistics [in German] HNO. 2011;59(08):752–764. doi: 10.1007/s00106-011-2365-1. [DOI] [PubMed] [Google Scholar]


