Abstract
Interventional radiology's role in the management of portal hypertension in the pediatric population differs from the management of adult portal hypertension. In the pediatric population, portal hypertension is frequently secondary to thrombosis and cavernous transformation of the extrahepatic portion of the portal vein. Transjugular intrahepatic portosystemic shunt can be utilized to manage portal hypertension in children with intrinsic liver disease that results in cirrhosis and portal hypertension, and is often used as a bridge to transplant. While technically feasible in extrahepatic portal vein occlusion, the sequelae of portosystemic shunting are less desirable in a child. The Meso-Rex bypass procedure, which represents the mainstay of management for pediatric portal hypertension, provides surgical relief of extrahepatic portal vein obstruction and restores mesenteric venous blood flow to the liver. This article aims to review management of portal hypertension in children as it pertains to the interventional radiologist, including preoperative assessment, postoperative evaluation, and the management of complications of the Meso-Rex bypass.
Keywords: Meso-Rex bypass, Rex shunt, cavernous transformation, portal hypertension, extrahepatic portal vein obstruction
Objectives: Upon completion of this article, the reader will be able to (1) provide an overview of significant ways that management of portal hypertension in the pediatric population differs from management of the adult population; (2) explain the role of interventional radiology procedures in the management of pediatric portal hypertension, and describe the interventional techniques used.
Accreditation: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit ™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Portal hypertension, or elevated portal pressure due to resistance to portal flow, is defined as an absolute portal venous pressure of >10 mm Hg or a pressure gradient between portal and systemic veins of >5 mm Hg. 1 2 3 Portal hypertension can be classified into three main categories based on the anatomic location ( Table 1 ). 3 4 5
Table 1. Three main categories of portal hypertension based on anatomic location.
| Location | Subclassification | Examples |
|---|---|---|
| Prehepatic | Portal vein thrombus | |
| SMV thrombus | ||
| Intrahepatic | Presinusoidal | Hepatic fibrosis |
| Schistosomiasis | ||
| Sinusoidal | Cirrhosis Biliary atresia Posthepatitis |
|
| Postsinusoidal | Veno-occlusive disease | |
| Posthepatic | Budd–Chiari | |
| Hepatic vein occlusion | ||
| Right heart failure |
Abbreviation: SMV, superior mesenteric vein.
Extrahepatic (prehepatic) portal vein thrombosis (PVT) is the most common cause of portal hypertension in the pediatric population, accounting for ∼70% of cases, 6 and it is the most common cause of an upper gastrointestinal (GI) bleed in this population. In extrahepatic PVT, normal hepatopetal flow from the superior mesenteric vein and splenic vein is impeded by obstruction of the main portal vein. 7 8 This can result in cavernous transformation of the portal vein 9 10 within 6 to 20 days of acute portal vein thrombus. Development of cavernous transformation can be associated with severe portal hypertension, biliary disease, liver dysfunction, and coagulopathy. Patients may present with ascites, splenomegaly, or encephalopathy.
Although this sequence of events can occasionally be secondary to iatrogenic injury related to neonatal catheterization of the umbilical vein, and even more infrequently secondary to tumor or infection, no cause is found in up to 50% of cases (idiopathic prehepatic portal hypertension) ( Table 2 ). 11 12 13 Unlike in adults, coagulopathies are not a frequent cause of PVT in children. 13 14
Table 2. Causes of extrahepatic portal vein obstruction leading to portal hypertension.
| Etiology | Example |
|---|---|
| Iatrogenic | Neonatal catheterization (umbilical vein catheter) |
| SMV thrombus | |
| Regional trauma | Surgery |
| Liver transplant | |
| Infection | Neonatal omphalitis Intra-abdominal infection |
| Tumor | |
| Idiopathic | Unknown |
Abbreviation: SMV, superior mesenteric vein.
Initial treatment for pediatric portal hypertension focuses on preventing and controlling variceal formation and upper GI bleeding by utilizing medical therapy (e.g., nonselective β-blockers), sclerotherapy, and band ligation of varices. A hepatic venous pressure gradient (HVPG)10 mm Hg is predictive of the formation of varices and decompensation of cirrhosis in adults, but its role is less well defined in the pediatric population. 15
Surgical treatment is typically reserved for those patients who have failed medical and endoscopic measures, or who have significant sequela of portal venous hypertension, including significant splenomegaly. Historically, surgical techniques included splenectomy along with the creation of a portosystemic shunt. The Meso-Rex bypass procedure, first described in 1992, provided a physiological and anatomic bypass that could correct portal hypertension in the setting of portal vein occlusion. Most commonly, the Meso-Rex bypass or “Rex shunt” consists of a conduit, typically autologous right internal jugular vein, connecting the intrahepatic left portal vein (LPV) to the infrapancreatic superior mesenteric vein. This conduit reestablishes first-pass portal perfusion. It is important for the interventional radiologist to be familiar with the preoperative assessment and postoperative management of these shunts.
Finally, in the small percentage of patients with chronic liver disease or failed shunt surgery, transjugular intrahepatic portosystemic shunt (TIPS) is a treatment consideration, which is often used as a bridge to transplant.
Role of HVPG Measurement
While published data on HVPG measurement in children are limited, there may be similar pressure thresholds for the development of complications in the pediatric population. 15 HVPG measurements are feasible in pediatric patients, but there remains no general recommendation regarding the use of these measurements in clinical practice. 15 In children with chronic liver disease who require a transjugular liver biopsy, HVPG can be performed simultaneously to provide important supportive diagnostic and prognostic information about the underlying liver process.
Shunt Surgery
There are multiple types of surgical shunt procedures, including mesocaval, coronariocaval, inferior mesenteric vein/left renal vein, proximal splenorenal, distal splenorenal (“Warren shunt”), and mesenterico-LPV (Rex) shunt procedures. While portosystemic shunts can provide relief of extrahepatic portal vein obstruction, systemic shunting and its known sequelae are less desirable in children. In contrast, the mesenterico-portal Rex shunt bypasses the extrahepatic portal obstruction but maintains physiological intrahepatic portal vein perfusion, thereby avoiding the effects of systemic shunting. For the Rex shunt, the LPV is surgically exposed at the Rex recess and a conduit (typically autologous internal jugular vein) is anastomosed at that site. Next, this conduit is taken over the pancreas, posterior to the stomach, through the mesocolon, and then anastomosed to the infrapancreatic SMV ( Fig. 1a , b ).
Fig. 1.
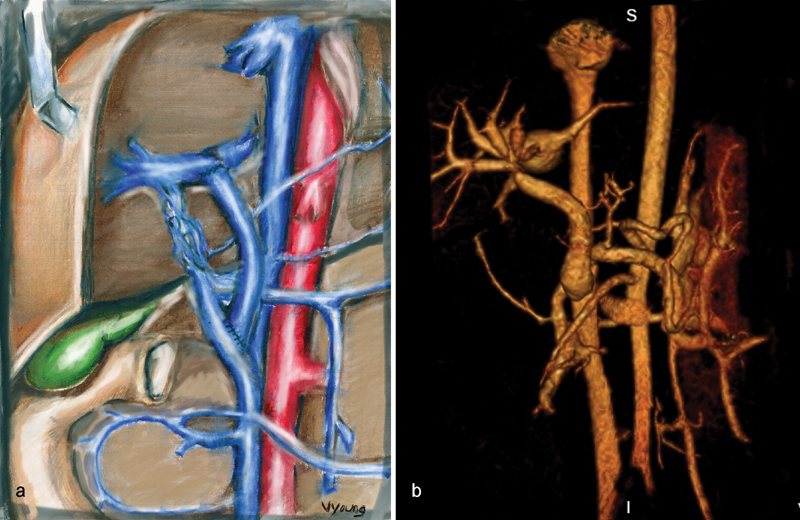
Meso-Rex bypass schematic (a) and volume-rendered magnetic resonance angiography after Meso-Rex bypass (b) .
Preoperative Evaluation
Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are all frequently employed as part of the preoperative evaluation. The main objectives of preoperative imaging prior to Meso-Rex bypass is to confirm the presence of extrahepatic portal vein occlusion, evaluate the extent of cavernous transformation ( Fig. 2a , b ), evaluate the patency and size of the intrahepatic portal venous system and superior mesenteric vein, evaluate for large collaterals that may alternatively be used for a bypass, and assess for additional vascular and solid organ abnormalities. While CT angiography (CTA) and MR angiography (MRA) are highly sensitive and accurate in predicting patency of the superior mesenteric vein, cross-sectional imaging does not adequately delineate the intrahepatic portal venous anatomy. Often the intrahepatic portal venous system is diminutive, which is why cross-sectional imaging is limited; however, it is well delineated with wedged hepatic venous portography, which is highly sensitive and accurate in predicting patency of the LPV. 16 This is performed via a transjugular approach ( Fig. 3 ). At our center, the right internal jugular vein is punctured under ultrasound guidance using a 21-G needle standard micropuncture set system. A 9F vascular sheath is placed, which allows us to perform transjugular liver biopsies to exclude underlying liver disease. Subsequently, the hepatic veins are catheterized with a 5F catheter and wedged venograms are performed. Generally, the left hepatic vein and the middle hepatic vein wedge venograms allow the best opacification of the portal vein at the Rex recess. Direct percutaneous portography is less frequently used as the portal branches are often diminutive and access can be challenging. Furthermore, direct access to the left portal venous system risks injuring the possible anastomosis site. Alternative shunts may be employed at the time of surgery if there is inadequate anatomy for a Meso-Rex bypass (e.g., no useable portal vein at time of surgical exploration of the Rex recessus). 17
Fig. 2.
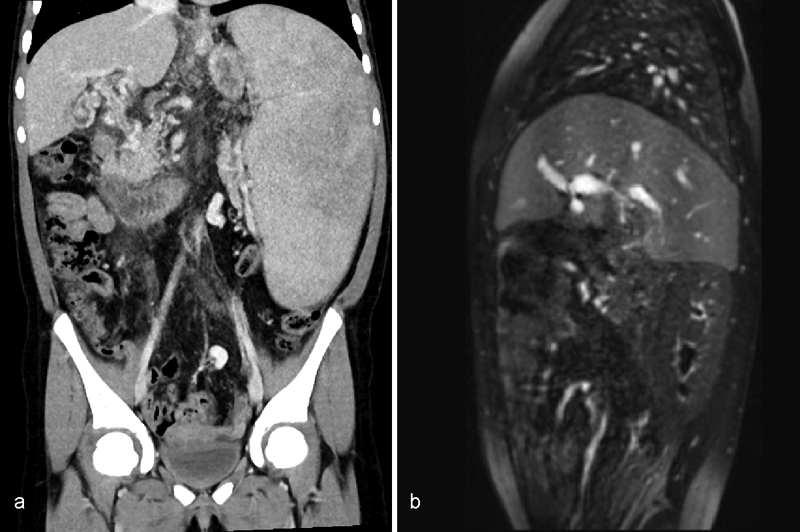
Computed tomography angiography ( a ) demonstrating cavernous transformation. Magnetic resonance angiography ( b ) demonstrating the same patient, post Meso-Rex bypass, with narrowing at the portal anastomosis.
Fig. 3.

Wedged hepatic venous portography via the transjugular approach to evaluate patency of the left portal vein and Rex recessus prior to Meso-Rex bypass.
Evaluation of Postoperative Complications
Color and Doppler ultrasound is most frequently employed to assess shunt patency at follow-up. Some centers also perform CTA or MRA at specific time intervals. Immediate complications of Meso-Rex shunt frequently include the presence of fluid collections (seroma, hematoma, abscess). Patients with graft stenosis or occlusion may present with the sequelae of recurrent portal hypertension, including GI bleed, ascites, splenomegaly, and thrombocytopenia. Graft stenosis often occurs at the portal anastomosis and can be confirmed with elevated velocities and aliasing on ultrasound or narrowing noted on CTA/MRA.
Meso-Rex Complications and Interventions
Interventional radiology is often the first line of treatment for graft-related stenosis or occlusion via angioplasty/stenting or thrombectomy, respectively. The approach utilized at our center is a percutaneous transhepatic access under ultrasound-guided access into the portal vein. Utilizing a 5F marker tip sheath, the stenosis is often easily traversed with a glidewire/glide catheter and the stenosis is delineated and pressures across the narrowing are obtained ( Fig. 4a ). Balloon angioplasty is employed at sites of stenosis ( Fig. 4b , c ), and repeat pressure gradients across the narrowing are obtained to confirm normalization of the gradient. Generally, stents are not utilized in children, as sizing can be problematic in a growing child; however, in the setting of recalcitrant stenosis not responsive to angioplasty or a graft requiring multiple interventions, stents may be utilized.
Fig. 4.
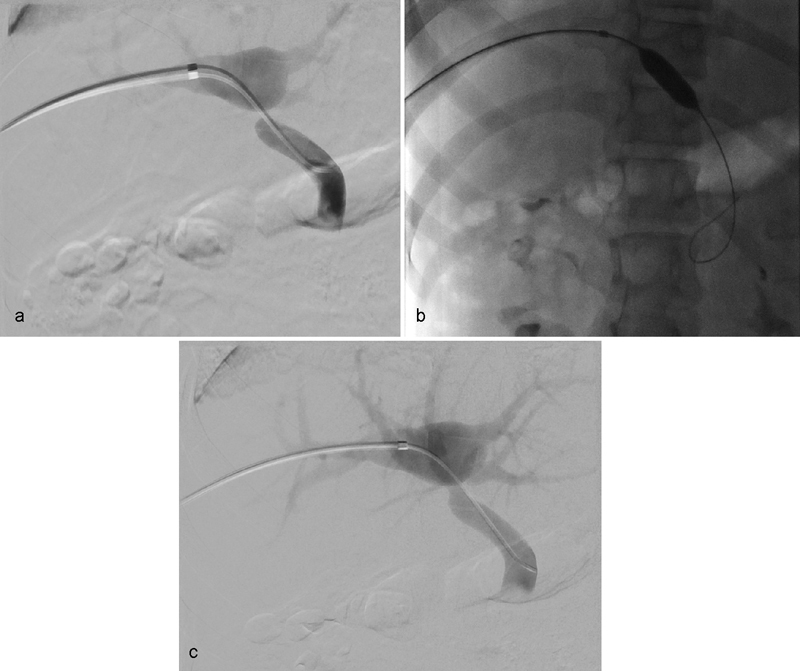
Rex intervention, balloon angioplasty of stenosis (a, b) ; gradient 15 to 3 (c) .
There have been several successful cases of shunt thrombolysis at our center utilizing thrombolytic therapy (such as tissue plasminogen activator) and mechanical/suction thrombectomy. Once the intervention is performed, the catheter is removed, and the tract is embolized. At our center, we opt to use Gelfoam plugs to mitigate the presence of streak artifact on future cross-sectional imaging.
TIPS as an Intervention
While technically feasible, TIPS is rarely indicated in extrahepatic portal vein occlusion given the proven efficacy of Meso-Rex shunts. In addition, the Rex shunt is preferred as it avoids the sequelae of portosystemic shunting. For children with primary liver disease that results in cirrhosis and end-stage liver failure, liver transplantation is the primary therapy in children. While TIPS are frequently considered as a bridge to transplant in adults with cirrhosis, this practice is much less common in the pediatric population. 15 If transplantation or surgical portosystemic shunting is not feasible, a TIPS may be considered to palliate variceal bleeding that persists despite combined pharmacological and endoscopic therapy.
Other Interventions
Additional treatments may be indicated depending on the etiology of portal hypertension in the pediatric patient. For instance, there may be a role for angioplasty and stenting in the setting of Budd–Chiari. In patients with arterioportal fistulas and associated portal hypertension, embolization can be easily performed. Posttransplant portal anastomotic strictures or thrombosis can be managed utilizing similar techniques to the adult population.
Conclusion
The management of portal hypertension in children differs from the management of adult portal hypertension. Extrahepatic (prehepatic) PVT is the most common cause of portal hypertension in the pediatric population, with the surgical Meso-Rex bypass providing definitive management by reestablishing first-pass portal perfusion. It is important that the interventional radiologist be familiar with the Meso-Rex procedure, including preoperative evaluation and postoperative management. TIPS is not typically indicated for the management of pediatric extrahepatic PVT but can be utilized in the management of portal hypertension in children with inherent liver disease that results in cirrhosis and portal hypertension. The interventional radiologist should be familiar with the limited scenarios when TIPS is the appropriate course of treatment in the pediatric patient with portal hypertension.
References
- 1.Vargas H E, Gerber D, Abu-Elmagd K. Management of portal hypertension-related bleeding. Surg Clin North Am. 1999;79(01):1–22. doi: 10.1016/s0039-6109(05)70004-9. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Groszmann R J, Fisher R L, Conn H O, Atterbury C E, Glickman M. Portal pressure, presence of gastroesophageal varices and variceal bleeding. Hepatology. 1985;5(03):419–424. doi: 10.1002/hep.1840050313. [DOI] [PubMed] [Google Scholar]
- 3.Mileti E, Rosenthal P. Management of portal hypertension in children. Curr Gastroenterol Rep. 2011;13(01):10–16. doi: 10.1007/s11894-010-0151-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grammatikopoulos T, McKiernan P J, Dhawan A. Portal hypertension and its management in children. Arch Dis Child. 2018;103(02):186–191. doi: 10.1136/archdischild-2015-310022. [DOI] [PubMed] [Google Scholar]
- 5.de Ville de Goyet J, D'Ambrosio G, Grimaldi C. Surgical management of portal hypertension in children. Semin Pediatr Surg. 2012;21(03):219–232. doi: 10.1053/j.sempedsurg.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Sarin S K, Sollano J D, Chawla Y K et al. Consensus on extra-hepatic portal vein obstruction. Liver Int. 2006;26(05):512–519. doi: 10.1111/j.1478-3231.2006.01269.x. [DOI] [PubMed] [Google Scholar]
- 7.Weiss B, Shteyer E, Vivante A et al. Etiology and long-term outcome of extrahepatic portal vein obstruction in children. World J Gastroenterol. 2010;16(39):4968–4972. doi: 10.3748/wjg.v16.i39.4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Webb L J, Sherlock S. The aetiology, presentation and natural history of extra-hepatic portal venous obstruction. Q J Med. 1979;48(192):627–639. [PubMed] [Google Scholar]
- 9.De Gaetano A M, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K. Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography. AJR Am J Roentgenol. 1995;165(05):1151–1155. doi: 10.2214/ajr.165.5.7572494. [DOI] [PubMed] [Google Scholar]
- 10.Bayraktar Y, Balkanci F, Kayhan B et al. Congenital hepatic fibrosis associated with cavernous transformation of the portal vein. Hepatogastroenterology. 1997;44(18):1588–1594. [PubMed] [Google Scholar]
- 11.Guimarães H, Castelo L, Guimarães J et al. Does umbilical vein catheterization to exchange transfusion lead to portal vein thrombosis? Eur J Pediatr. 1998;157(06):461–463. doi: 10.1007/s004310050853. [DOI] [PubMed] [Google Scholar]
- 12.Pacifico L, Panero A, Colarizi P, Matrunola M, Simonetti A F, Chiesa C. Neonatal Candida albicans septic thrombosis of the portal vein followed by cavernous transformation of the vessel. J Clin Microbiol. 2004;42(09):4379–4382. doi: 10.1128/JCM.42.9.4379-4382.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robson S C, Kahn D, Kruskal J, Bird A R, Kirsch R E. Disordered hemostasis in extrahepatic portal hypertension. Hepatology. 1993;18(04):853–857. doi: 10.1002/hep.1840180416. [DOI] [PubMed] [Google Scholar]
- 14.Fisher N C, Wilde J T, Roper J, Elias E. Deficiency of natural anticoagulant proteins C, S, and antithrombin in portal vein thrombosis: a secondary phenomenon? Gut. 2000;46(04):534–539. doi: 10.1136/gut.46.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shneider B L, Bosch J, de Franchis R et al. Portal hypertension in children: expert pediatric opinion on the report of the Baveno v Consensus Workshop on Methodology of Diagnosis and Therapy in Portal Hypertension. Pediatr Transplant. 2012;16(05):426–437. doi: 10.1111/j.1399-3046.2012.01652.x. [DOI] [PubMed] [Google Scholar]
- 16.Chaves I J, Rigsby C K, Schoeneman S E, Kim S T, Superina R A, Ben-Ami T.Pre- and postoperative imaging and interventions for the meso-Rex bypass in children and young adults Pediatr Radiol 20124202220–232., quiz 271–272 [DOI] [PubMed] [Google Scholar]
- 17.Superina R, Bambini D A, Lokar J, Rigsby C, Whitington P F. Correction of extrahepatic portal vein thrombosis by the mesenteric to left portal vein bypass. Ann Surg. 2006;243(04):515–521. doi: 10.1097/01.sla.0000205827.73706.97. [DOI] [PMC free article] [PubMed] [Google Scholar]


