Abstract
Rationale:
Primary cardiac tumors are very rare, and angiosarcoma accounts for about 33% of all primary malignant cardiac tumors. Primary cardiac epithelioid angiosarcoma is a highly aggressive and difficult to diagnose tumor, with early systemic metastasis and poor prognosis.
Patient concerns:
A 35-year-old Han male experienced sudden severe palpitation and moderate dyspnea. The patient received a whole body F-18 fluoro-deoxyglucose positron emission tomography (18F-FDG PET)/computed tomography (CT) scan, the scan showed a large mass in the right atrium (RA) and numerous pulmonary nodules in both lungs.
Diagnoses:
The patient was diagnosed as right atrial epithelioid angiosarcoma with multiple pulmonary metastasis by pulmonary biopsy through CT-guided percutaneous transthoracic fine needle aspiration.
Interventions:
The patient received a cycle of chemotherapy with docetaxel and gemcitabine, followed by another cycle with epirubicin and ifosfamide.
Outcomes:
The chemotherapy was ineffective. After the two cycles, the bilateral pleural effusion steadily increased, the patient had severe dyspnea and palpitation, and died three weeks later, with an overall survival of 2.5 months.
Lessons:
Primary angiosarcoma of heart is a very rare and aggressive disease, and its diagnosis and treatment are difficult. Most patients may have systemic metastasis at diagnosis, and have a very short survival without surgical resection. Hence, early diagnosis and surgical resection is extremely important to treat this disease.
Keywords: atrial angiosarcoma, case report, imaging-guided biopsy, pulmonary metastasis
1. Introduction
Primary cardiac tumors are very rare, and detected in 0.002% to 0.33% of autopsy series.[1] Approximately 20% to 30% of all primary cardiac neoplasms are malignant, of which angiosarcoma is the most common. Primary cardiac angiosarcoma accounts for about 33% of all primary malignant cardiac tumors.[1,2] Angiosarcoma is typically localized in the right atrium, in about 74% of the patients.[3] It is a highly aggressive tumor with early systemic metastasis and poor prognosis. Diagnosis of this disease is difficult, and is often delayed due to lack of specific symptoms. Definitive diagnosis is based on the histopathological examination.[4] The therapy for cardiac epithelioid angiosarcoma remains controversial, with no standard treatment regimens.
In this study, we presented a rare case of right atrial mass and multiple pulmonary lesions, which was suspected to be malignant cardiac tumor with multiple lung metastasis. This case study highlights the difficulties in diagnosing and treating cardiac tumors.
2. Case report
A 35-year-old Han male experienced sudden severe palpitation and moderate dyspnea since November 2014. The symptoms lasted for approximately 1 to 5 minutes and were relieved by rest. The patient smoked for >10 years, but had no history of drinking, circulatory or respiratory diseases. In December 2014, the patient visited hospital nearby, a transthoracic echocardiogram (TTE) was performed, which showed severe pericardial effusion. After drainage, the patient's pericardial effusion was controlled, palpitation and dyspnea improved, but severe cough and occasional hemoptysis occurred. For evaluation of the disease, whole body F-18 fluoro-deoxyglucose positron emission tomography (18F-FDG PET)/computed tomography (CT) was performed, which confirmed a large mass (6 cm × 6.7 cm × 6.3 cm) in the right atrium (RA) with intense FDG uptake (SUVmax:22) and numerous pulmonary nodules in both lungs with FDG avid (SUVmax:7.2). The enlarged mediastinal and bilateral hilar nodes also had elevated FDG activity (SUVmax:4.5) (Fig. 1). For further diagnosis and treatment, the patient visited our Wuhan Union Hospital one week later, and cardiac magnetic resonance imaging (MRI) showed a heterogeneously enhanced hypodense mass in the inner wall of RA, which was suspected to be malignant cardiac tumor (Fig. 2). To confirm the diagnosis, we performed a chest CT scan (Fig. 3), and CT-guided percutaneous transthoracic fine needle aspiration biopsy of the pulmonary nodule. The pulmonary nodule was confirmed to be an epithelioid angiosarcoma probably originating from the heart (Fig. 4). The immunohistochemistry results were as follows: VIM(+), TTF-1(−), NapsinA(−), CK7(−), Ki67(LI:60%), PCK(−), Syn(−), cgA(−), CD56(−), LCA(−), CK8/18(−), Hepatocyte(−), Gly-3(−), CD34(+), CD31(+), SMA(−), ERG(+), Des(−), MyoD1(−), MyoGenin(−), and Calretinin(−).
Figure 1.
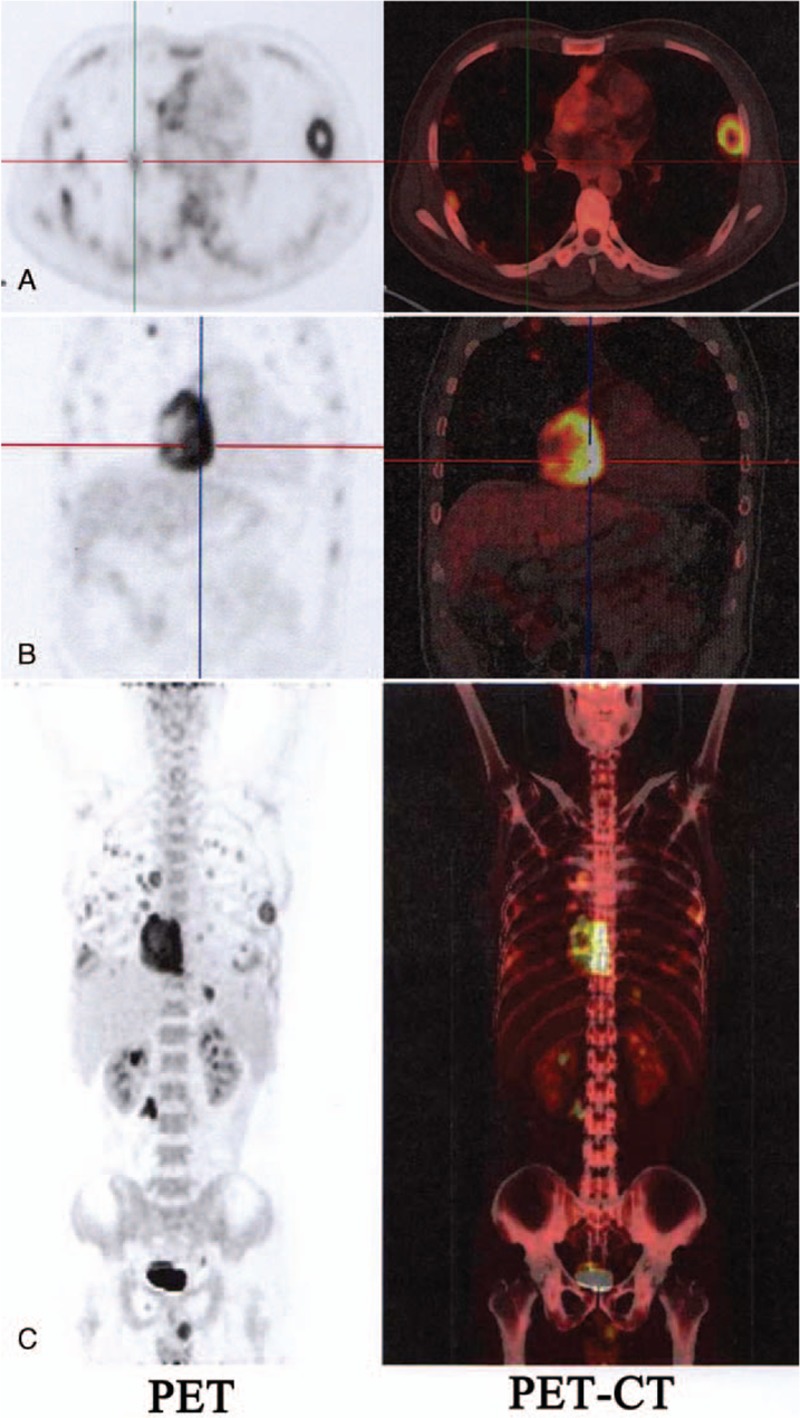
18-F-fluoro-deoxyglucose (FDG) contrast enhanced positron emission tomography/computed tomography (PET-CT) images. (A) Pulmonary nodules in both lungs and hilar nodes with elevated FDG activity. (B) A large mass (6 cm × 6.7 cm × 6.3 cm) in the right atrium (RA) with intense FDG uptake (SUVmax:22). (C) Whole body projection images showed intense FDG uptake in cardiac mass with multiple FDG avid metastases. 18F-FDG = F-18 fluoro-deoxyglucose, CT = computed tomography, PET = positron emission tomography, RA = right atrium.
Figure 2.
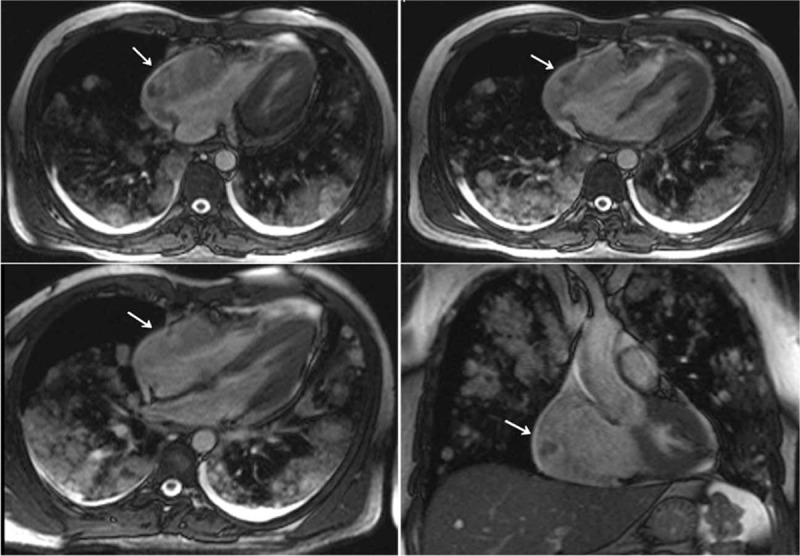
Cardiac magnetic resonance imaging (MRI) showed a mass in the inner wall of the right atrium. MRI = magnetic resonance imaging.
Figure 3.
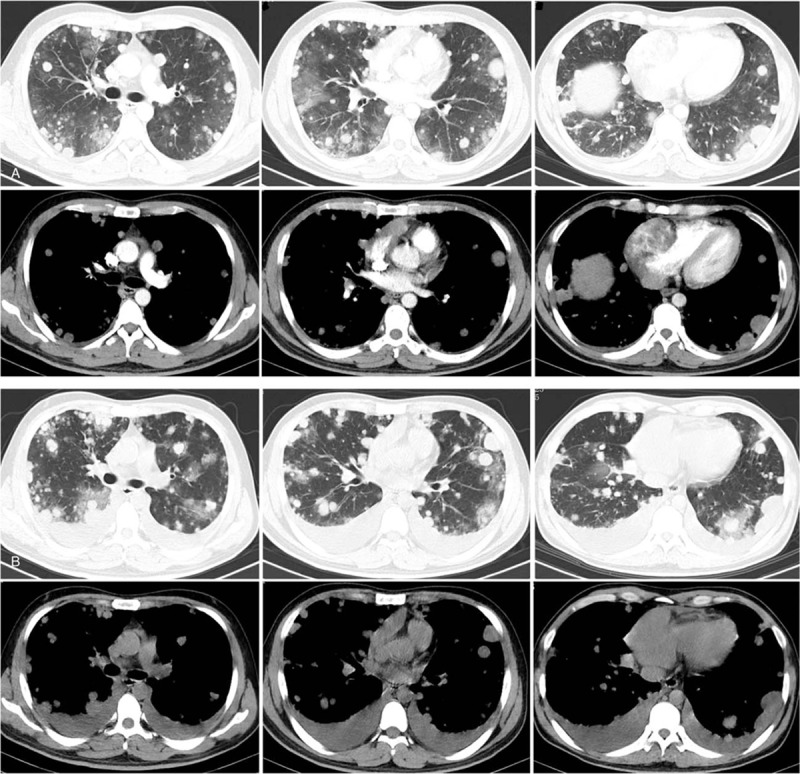
Chest computed tomography (CT) scan. (A) a large mass (6 cm × 6.7 cm × 6.3 cm) in the right atrium (RA) and numerous pulmonary nodules in both lungs were seen by CT scan before therapy. (B) Some pulmonary nodules were enlarged and the bilateral pleural effusion increased after one cycle of chemotherapy. CT = computed tomography, RA = right atrium.
Figure 4.
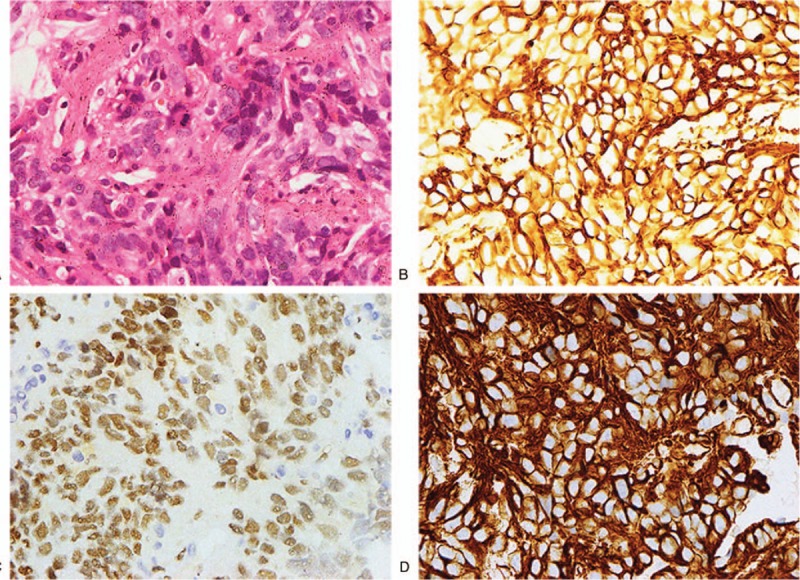
Epithelioid angiosarcoma was identified by H&E and immunohistochemical staining. (A) H&E staining (×400). (B) High expression of CD 31 by immunohistochemical staining (×400). (C) High expression of ERG by immunohistochemical staining (×400). (D) High expression of VIM by immunohistochemical staining (×400).
The final diagnosis of this patient was right atrial epithelioid angiosarcoma with multiple pulmonary metastasis (stage IV), based on the imaging and biopsy results. The patient had no family history of this disease. Three days later, the patient started chemotherapy with docetaxel (75 mg/m2) and gemcitabine (900 mg/m2). After a cycle of this chemotherapy, the patient had grade 3 leucopenia, grade 2 thrombocytopenia, and slight nausea, the adverse reactions gradually decreased after corresponding supportive care. Three weeks after the first cycle of chemotherapy, the patient had severe cough, hemoptysis, aggravated dyspnea, and palpitation. Chest CT scan was repeated (Fig. 3) to evaluate the effectiveness of chemotherapy. The disease had progressed indicating that the chemotherapy had failed. Some pulmonary nodules were enlarged and the bilateral pleural effusion had increased. Then, we used epirubicin (30 mg/m2, d1–3) and ifosfamide (1500 mg/m2, d1–4) in the second cycle of chemotherapy. The patient had grade 4 leucopenia, grade 2 thrombocytopenia, severe anemia, and nausea after therapy, and this cycle of chemotherapy was also ineffective. The bilateral pleural effusion rapidly increased, the patient had severe dyspnea and palpitation, and died 3 weeks after the second cycle of chemotherapy, with an overall survival of 2.5 months.
3. Discussion
Primary cardiac tumors are very rare, and fewer than one-third are malignant. The malignant tumors include angiosarcoma, lymphoma, fibrosarcoma, myosarcoma, and myxosarcoma, of which angiosarcoma is the most common with an extremely rare incidence of 0.0001%.[5] It typically occurs in middle-aged men, in the right atrium and pericardium.[6] Our patient was a 35-year-old male with a tumor in the right atrium.
The diagnosis of cardiac angiosarcoma is difficult because the symptoms associated with the disease are not specific. Common symptoms include palpitation, heart failure, chest pain, dyspnea, hemoptysis and congestive heart failure, or acute right heart failure secondary to pericardial tamponade.[7] Occasionally, an abrupt event may occur as the first clinical sign. Systemic symptoms occur in few cases and include night sweats, fever and weight loss.[8] Our patient presented with sudden severe palpitation and moderate dyspnea. Since the symptoms were nonspecific, he was initially misdiagnosed as coronary heart disease. Our patient had no systemic symptoms, which was in accordance with previous reports.
Due to the location of the tumor and nonspecific symptoms, diagnosis is often delayed with an average time interval from presentation to the correct diagnosis of 3 years,[9] and >50% of these tumors have systemic metastases at the time of diagnosis. Most common metastasis sites include lung, liver, brain and bone, although metastasis to lymph nodes, pancreas, spleen, skin, mandible, adrenal glands and kidneys have also been reported.[9–11] Angiosarcoma has extensive infiltration and high degree of malignancy, and infiltration or direct extension into myocardium and pericardium is common. Our patient also had pericardial effusion and multiple pulmonary metastasis at the time of diagnosis, which were the most frequent sites of metastasis.
Given the specific properties of cardiac angiosarcoma, imaging examinations are critical in diagnosing this disease. Echocardiography is usually the first imaging modality for the diagnosis. The sensitivity and specificity of transthoracic and transesophageal for detection of cardiac masses are 93% and 97%, respectively.[12] Cardiac MRI has high specificity to identify pseudotumors, thrombi and lipomas, but cannot differentiate residual disease.[9,13] Whole body PET/CT also provides metabolic information of tumors and is particularly helpful to delineate the extent of tumor infiltration and assess the metastasis.[14] In some cases, the typical location of mass with infiltration is suggestive of angiosarcoma.[6,9] Cardiac MRI and PET/CT were performed in our patient, which showed a heterogeneously enhanced hypodense mass in the inner wall of right atrium with high grade FDG uptake and numerous pulmonary nodules with serious FDG avid, suggestive of malignant cardiac tumor with pulmonary metastasis.
Although imaging examinations are important, the definitive diagnosis of cardiac angiosarcoma is based on histopathology.[15] Previously, the diagnosis of cardiac angiosarcoma was made by surgery or postmortem.[15] In addition, hemorrhagic pericardial fluid and cytologic examination of fluid were helpful for diagnosis.[16] However, histopathology based on tissue specimens is critical for clarifying the nature of a cardiac mass. In preceding decades, various methods were used to obtain tissue specimens in addition to thoracotomy. Transthoracic echocardiography or CT-guided biopsy and transesophageal echocardiography-guided transvenous endomyocardial biopsy of cardiac mass are less invasive as compared to thoracotomy, and are frequently used for diagnosis. However, transthoracic biopsy of a right atrial mass has a potential risk of cardiac rupture because the right atrial wall is thin.[8] Hence, patients may refuse the biopsy at the original site. In some rare cases, biopsy of metastatic nodules outside the heart was also performed for pathological evidence. Qiu and Zhang[17] diagnosed a case of primary cardiac angiosarcoma by multimodality imaging-guided liver biopsy. In our case, after careful consideration of the advantages and disadvantages of all available techniques, and the patient's refusal of biopsy or surgical treatment of the right atrial mass, we performed a biopsy of pulmonary nodule through CT-guided percutaneous transthoracic fine needle aspiration, which supported the diagnosis of primary cardiac epithelioid angiosarcoma with pulmonary metastasis. To the best of our knowledge, this is the first report on primary cardiac epithelioid angiosarcoma confirmed by pulmonary biopsy through CT-guided percutaneous transthoracic fine needle aspiration.
Cardiac angiosarcoma has a dismal prognosis because of highly aggressive malignancy with local invasion and a high incidence of systemic metastasis with a median survival ranging from 6 to 11 months.[18] Treatment of cardiac angiosarcoma is controversial due to the poor prognosis.[19] Surgical resection remains the first-line treatment of choice when no evidence of metastases exists and myocardial resection is reparative.[20] If the tumor is resectable, adjuvant therapies, including chemotherapy, radiotherapy and targeted therapy, can improve the chances of survival because of the high probability of metastasis.[21–24] Among the surgical therapeutic methods, heart transplantation has also been suggested, although many moral and social dilemmas exist.[25] The survival after surgery ranges from 2 to 55 months, with a median survival of 14 months.[18] In patients with incomplete surgical resection, chemotherapy and radiotherapy can also be selected. High doses of radiation could improve control of local tumor, but increases severe adverse events.[26]
However, most patients have systemic metastasis at diagnosis, for which multi-modality treatment is favored. Thus, various combinations of surgery, chemotherapy, radiotherapy, and/or transplantation have been utilized, with varying results. The patients with systemic metastasis have a mean survival of 3.8 ± 2.5 months without surgical resection.[27] In our patient, the tumor involved the right atrium along with multiple pulmonary metastasis and pericardium infusion, so surgical resection was inappropriate, and hence we selected chemotherapy.
Chemotherapy for cardiac angiosarcoma is controversial, and there is no randomized trial of metastatic sarcomas with or without chemotherapy. For the majority of sarcomas, the most eligible agents are doxorubicin and ifosfamide cyclophosphamide, taxanes, vincristine, dactinomycin, etc.[25] Combination therapy with doxorubicin and ifosfamide was effective for the treatment of metastatic soft-tissue sarcoma, including angiosarcoma, regardless of origin.[28,29] Recent studies showed that docetaxel has similar efficacy for metastatic angiosarcomas.[26,30,31] Gemcitabine was also effective for treating advanced angiosarcoma.[29,32] Moreover, the successful administration of molecular targeted therapy in some tumors indicated that it may have possible therapeutic benefit in angiosarcoma as well.[33] The efficacy of antiangiogenic drugs, such as sorafenib, bevacizumab, and imatinib, have been demonstrated in some phase II trials for the treatment of advanced or metastatic angiosarcoma. Sorafenib had a better progression-free survival with 3.8 months, and the overall survival was 14.9 months, but the response rate was lower than standard cytotoxic agents.[34] Bevacizumab was also effective for sarcoma with 57% response rate,[33] but imatinib was ineffective.[35] Since our patient had hemoptysis, and given the adverse effects of anti-angiogenic drugs, we used chemotherapy without anti-angiogenic drugs. However, the first cycle of chemotherapy with docetaxel and gemcitabine, and the second cycle of chemotherapy with epirubicin and ifosfamide were both ineffective. After 2 cycles of chemotherapy, the bilateral pleural effusion rapidly increased, the patient had severe dyspnea and palpitation, and died 3 weeks later, with an overall survival of 2.5 months.
4. Conclusion
Primary angiosarcoma of the heart is a very rare and aggressive disease, and its diagnosis and treatment are difficult. Most patients may have systemic metastasis at diagnosis, and have a very short survival without surgical resection. This is the first report on diagnosis of primary cardiac epithelioid angiosarcoma by pulmonary biopsy through CT-guided percutaneous transthoracic fine needle aspiration, but the prognosis of our patient was very poor. Hence, we need to improve the methods of diagnosis and therapy of this disease.
Acknowledgments
The authors thank the family of this patient for providing the medical information.
Author contributions
Conceptualization: Cuiwei Liu, Yanxia Zhao, Ting Hu, Jinghua Ren, Linka Xie, Jie Xiong, Hongge Wu, Xiaofang Dai, Shihong Fei.
Data curation: Cuiwei Liu, Zhongyuan Yin, Jinghua Ren, Jielin Wei, Shihong Fei.
Formal analysis: Yanxia Zhao, Zhongyuan Yin, Jielin Wei, Jie Xiong, Shihong Fei.
Investigation: Cuiwei Liu, Yanxia Zhao, Ting Hu, Jielin Wei, Linka Xie, Jie Xiong, Xiaofang Dai.
Methodology: Cuiwei Liu, Yanxia Zhao, Zhongyuan Yin, Ting Hu, Jinghua Ren, Jielin Wei, Linka Xie, Jie Xiong, Xiaofang Dai.
Project administration: Cuiwei Liu, Linka Xie, Hongge Wu.
Resources: Hongge Wu.
Software: Zhongyuan Yin, Hongge Wu.
Supervision: Yanxia Zhao.
Validation: Zhongyuan Yin, Ting Hu, Jinghua Ren, Linka Xie, Hongge Wu, Xiaofang Dai.
Visualization: Ting Hu, Hongge Wu.
Writing - original draft: Cuiwei Liu, Yanxia Zhao, Zhongyuan Yin, Ting Hu, Jinghua Ren, Jielin Wei, Linka Xie, Jie Xiong, Hongge Wu, Xiaofang Dai.
Writing - review & editing: Cuiwei Liu, Yanxia Zhao, Zhongyuan Yin, Ting Hu, Jinghua Ren, Jielin Wei, Linka Xie, Jie Xiong, Hongge Wu, Xiaofang Dai, Shihong Fei.
Footnotes
Abbreviations: 18F-FDG PET = F-18 fluoro-deoxyglucose positron emission tomography, CT = computed tomography, MRI = magnetic resonance imaging, RA = right atrium, TTE = transthoracic echocardiogram.
This study was supported by a grant from the National Natural Science Foundation of China (No. 81602189). The Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology gave an approval for this study. The patient was dead, his family had agreed for publication of the case, and his wife had provided informed consent.
The authors have no conflicts of interest to disclose.
References
- [1].Silverman NA. Primary cardiac tumors. Ann Surg 1980;191:127–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Janigan DT, Husain A, Robinson NA. Cardiac angiosarcomas. A review and a case report. Cancer 1986;57:852–9. [DOI] [PubMed] [Google Scholar]
- [3].Herrmann MA, Shankerman RA, Edwards WD, et al. Primary cardiac angiosarcoma: a clinicopathologic study of six cases. J Thorac Cardiovasc Surg 1992;103:655–64. [PubMed] [Google Scholar]
- [4].Mahajan A, Rekhi B, Laskar S, et al. Primary pulmonary artery sarcoma masquerading as pulmonary thromboembolism: a rare diagnosis unveiled. Clin Sarcoma Res 2017;7:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kodali D, Seetharaman K. Primary cardiac angiosarcoma. Sarcoma 2006;2006:39130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Dhull VS, Sharma P, Mukherjee A, et al. 18F-FDG PET-CT for evaluation of cardiac angiosarcoma: a case report and review of literature. Mol Imaging Radionucl Ther 2015;24:32–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chalhoub E, Mattar BI, Shaheen W, et al. Cardiac angiosarcoma presenting with tamponade. Intern Med 2012;51:2905–7. [DOI] [PubMed] [Google Scholar]
- [8].Bruce CJ. Cardiac tumours: diagnosis and management. Heart 2011;97:151–60. [DOI] [PubMed] [Google Scholar]
- [9].Jain A, Simon S, Elangovan I. (18)F-fluoro-deoxyglucose positron emission tomography-computed tomography in initial assessment and diagnosis of right atrial angiosarcoma with widespread visceral metastases: A rare case report and review of the literature. Indian J Nucl Med 2015;30:51–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Waness A, Batoon AA, Mirza I, et al. Elusive cardiac angiosarcoma in a young pregnant female: rare presentation with fatal outcome. Cardiol Res 2015;6:292–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ramadhan A, Willén H, Thor A. Angiosarcoma of the mandible: metastasis from a primary tumor of the right atrium of the heart. Case Rep Clin Med 2013;02:53–7. [Google Scholar]
- [12].Chen YC. Localization of angiosarcoma by peri-operative transesophageal echocardiography. Int J Cardiovasc Imaging 2017;33:1749–51. [DOI] [PubMed] [Google Scholar]
- [13].Lindsey J, Stacey RB. Cardiac magnetic resonance in cardiac angiosarcoma. Echocardiography 2017;34:1077–81. [DOI] [PubMed] [Google Scholar]
- [14].Taywade SK, Damle NA, Tripathi M, et al. Unusual presentation of rare cardiac tumor: the role of F-18-fluorodeoxyglucose positron emission tomographyc/computed tomography. Indian J Nucl Med 2017;32:157–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Leduc C, Jenkins SM, Sukov WR, et al. Cardiac angiosarcoma: histopathologic, immunohistochemical, and cytogenetic analysis of 10 cases. Hum Pathol 2017;60:199–207. [DOI] [PubMed] [Google Scholar]
- [16].Randall MB, Geisinger KR. Angiosarcoma of the heart: pericardial fluid cytology. Diagn Cytopathol 1990;6:58–62. [DOI] [PubMed] [Google Scholar]
- [17].Qiu ZX, Zhang Q. Primary cardiac angiosarcoma confirmed by multimodality imaging guided liver biopsy. Int J Clin Exp Pathol 2014;7:1188–92. [PMC free article] [PubMed] [Google Scholar]
- [18].Antonuzzo L, Rotella V, Mazzoni F, et al. Primary cardiac angiosarcoma: a fatal disease. Case Rep Med 2009;2009:591512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Shanmugam G. Primary cardiac sarcoma. Eur J Cardio-thoracic Surg 2006;29:925–32. [DOI] [PubMed] [Google Scholar]
- [20].Fukunaga NM, Kitai TMDP, Imai YMDP, et al. Three-year survival in primary cardiac angiosarcoma. J Med Invest 2017;64:181–3. [DOI] [PubMed] [Google Scholar]
- [21].Wang M, Fu G, Jiang H, et al. Multimodality treatment for cardiac angiosarcoma. Int Med 2014;53:1949–53. [DOI] [PubMed] [Google Scholar]
- [22].Bellitti R, Buonocore M, De Rosa N, et al. Primary cardiac angiosarcoma in a 25-year-old man: excision, adjuvant chemotherapy, and multikinase inhibitor therapy. Tex Heart Inst J 2013;40:186–8. [PMC free article] [PubMed] [Google Scholar]
- [23].Abu Saleh WK, Ramlawi B, Shapira OM, et al. Improved outcomes with the evolution of a neoadjuvant chemotherapy approach to right heart sarcoma. Ann Thorac Surg 2017;104:90–6. [DOI] [PubMed] [Google Scholar]
- [24].Schur S, Hamacher R, Brodowicz T. Pazopanib in primary cardiac angiosarcoma of the right atrium: a case report. Case Rep Oncol 2016;9:363–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Batzios S, Michalopoulos A, Kaklamanis L, et al. Angiosarcoma of the heart: case report and review of the literature. Anticancer Res 2006;26:4837–42. [PubMed] [Google Scholar]
- [26].Jang Y, Kim J, Shim JW, et al. Primary cardiac angiosarcoma: a prolonged response to surgical resection followed by concurrent chemoradiotherapy with docetaxel. SpringerPlus 2016;5:648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Patel SD, Peterson A, Bartczak A, et al. Primary cardiac angiosarcoma—a review. Med Sci Monit 2014;20:103–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Serrano C, García Á, Brana I, et al. Angiosarcoma of the ovary: is it always a lethal disease? J Clin Oncol 2010;28:675–7. [DOI] [PubMed] [Google Scholar]
- [29].Yonezawa I, Waki M, Tamura Y, et al. Gemcitabine-based regimen for primary ovarian angiosarcoma with MYC amplification. Curr Oncol 2014;21:e782–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Penel N, Italiano A, Raycoquard I, et al. Metastatic angiosarcomas: doxorubicin-based regimens, weekly paclitaxel and metastasectomy significantly improve the outcome. Ann Oncol 2012;23:517. [DOI] [PubMed] [Google Scholar]
- [31].Minichillo S, Pantaleo MA, Nannini M, et al. Efficacy of weekly docetaxel in locally advanced cardiac angiosarcoma. BMC Res Notes 2015;8:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Stacchiotti S, Palassini E, Sanfilippo R, et al. Gemcitabine in advanced angiosarcoma: a retrospective case series analysis from the Italian Rare Cancer Network. Ann Oncol 2012;23:501–8. [DOI] [PubMed] [Google Scholar]
- [33].Agulnik M, Yarber JL, Okuno SH, et al. An open-label, multicenter, phase II study of bevacizumab for the treatment of angiosarcoma and epithelioid hemangioendotheliomas. Ann Oncol 2013;24:257–63. [DOI] [PubMed] [Google Scholar]
- [34].Maki RG, D’Adamo DR, Keohan ML, et al. Phase II study of sorafenib in patients with metastatic or recurrent sarcomas. J Clin Oncol 2009;7:3133–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].RC, JK W, RG M, et al. Phase II multicenter trial of imatinib in 10 histologic subtypes of sarcoma using a bayesian hierarchical statistical model. J Clin Oncol 2009;7:3148–53. [DOI] [PubMed] [Google Scholar]


