Abstract
Despite the possibility that the methodological difference of this salivagram may influence the results for detection rate, there has been no study on the effect of the solution volume on detection rate. Moreover, to date, since the introduction of the nucleotide salivagram, there has been a tendency that a constant solution volume and nucleotide dose is not used in studies. Therefore, the aim of this study is to investigate the effect of solution volume on the detection rate of a salivagram in patients with brain lesion, and to determine the optimal solution volume of salivagram. We retrospectively reviewed clinical data and solution volume of radionuclide used in the salivagram of 77 patients with dysphagia, and the patients were divided into 2 groups according to the solution volume of the radionuclide (Group A-0.1 mL vs Group B-0.5 mL). Although, there was no significant difference between 2 groups in clinical data, there was a statistically significant difference in the detection rate of salivary aspiration between the 2 groups (3.3% vs 19.1%). Even a small difference of the solution volume of radionuclide in salivagram can affect the detection rate of salivary aspiration in patients with brain lesion. Further study with various solution volumes of radionuclide is warranted to determine the optimal solution volume of the radionuclide salivagram.
Keywords: aspiration, deglutition, drooling, dysphagia, salivary glands
1. Introduction
Previous studies have reported that pneumonia is one of the major complications, which can be a cause of death especially in patients with oropharyngeal dysphagia owing to brain lesions, such as stroke and traumatic brain injury (TBI).[1–4] For diagnosing and evaluating dysphagia, VFSS is the gold standard in clinical practice.[5–7] However, a radionuclide salivagram is known to be a more useful tool for detecting salivary aspiration, which is another important cause of aspiration pneumonia, compared with the videofluoroscopic swallowing study (VFSS).[8–10]
The radionuclide salivagram involves placing a small volume of radionuclide in the patient's mouth, and then a series of images record radioactivity in the bronchial tree, thereby showing salivary aspiration.[8–12] However, in previous studies using a salivagram, there have been several conflicting results in the detection rate of salivary aspiration for patients with brain lesions. Baikie et al[13] reported that positive findings of aspiration of salivary aspiration occurred with 55.6% (35/63) of bedridden spastic quadriparetic cerebral palsy patients. However, Wu and Zhao[14] reported that the positive response of saliva aspiration by radionuclide salivagram was 21.9% (7/32) in bedridden patients with brain lesion. Although the patients included in these studies were different, these conflicting results may be due to differences in the methods of implementing salivagrams as well as differences in the patient population involved.
In Baikie's study, they performed the salivagram in the supine position and then 99mTc-sulfur solution (0.5–1 mCi in a 20 mL of normal saline) was instilled into the patient's mouth over 1 hour using a feeding tube.[13] In contrast, in Kang's study, they used a different volume of solution (1 mCi in only a drop of saline) which was instilled into the mouth while the patient was in the supine position during the salivagram.[14] Despite the possibility that the methodological difference of this salivagram may influence the results for detection rate, there has been no study on the effect of the solution volume on detection rate. Moreover, to date, since the introduction of the nucleotide salivagram by Heyman et al[9,10] in 1989, there has been a tendency that a constant solution volume and nucleotide dose is not used in studies.
Therefore, to evaluate the effect of solution volume on the detection rate of a salivagram in patients with brain lesion and to determine the optimal solution volume of the radionuclide salivagram, we compared the detection rate of radionuclide salivagrams with varying solution volumes.
2. Materials and methods
2.1. Subjects
We retrospectively reviewed the medical records of 123 patients with dysphagia who underwent both radionuclide salivagrams and VFSS between March 2013 and January 2017. Among them, those with brain lesion, such as stroke, TBI, and hypoxic ischemic encephalopathy, were included. The following patients were excluded: those with neuromuscular disorders, spinal cord injury, and non-brain tumors. Patients were also excluded when the interval between the VFSS and the salivagram was >3 days. In addition, patients with insufficient medical records were also excluded. This study received Institutional Review Board approval of Daegu Fatima Hospital.
2.2. Clinical parameters
Sex, age, mini mental state examination (MMSE), Global Deterioration Scale (GDS), total score of Modified Barthel Index (MBI), and each subscore of MBI were reviewed.
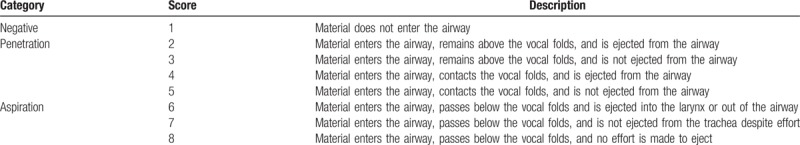
2.3. VFSS
The VFSS were performed using sequential swallowing of the following materials mixed with barium: thin fluids, thick fluids, pureed rice, and solids. Patients were evaluated in an upright seated position and were not instructed about any compensation techniques. The dynamic fluoroscopic images were obtained at the lateral and anterior–posterior positions, stored at 30 frames per second. The dynamic fluoroscopic images were reviewed by experienced 2 physicians. The degree of aspiration during VFSS was described using penetration-aspiration scale (PAS). (Table 1).
Table 1.
The penetration-aspiration scale (PAS).
2.4. Radionuclide salivagram
In radionuclide salivagram, patients were evaluated in a supine position under the gamma camera. All salivagram conducted in the department of nuclear medicine at our hospital. Tc-99m diethylenetriamine pentaacetic acid (DTPA) (3 mCi) was mixed with a different volume of normal saline (0.1 and 0.5 mL) and solution was administered into the mouth using a syringe. Sequential supine posterior images were obtained for 2 hours routinely; at 1, 5, 10, 20, 30, and 60 minutes after the instillation, images were taken by the gamma camera. Visual interpretation of the images was performed by an experienced nuclear medicine physician. Aspiration was reported to be present when radiopharmaceutical activity was detected in tracheobronchial fields (Fig. 1).
Figure 1.

Sequential images of radionuclide salivagram throughout 1 hour after oral administered of technetium 99m sulfur colloid solution. (A) The presence of radiotracer in trachea and bilateral bronchi demonstrates positive for salivary aspiration (arrows). (B) Uptake of radiotracer noted only in oropharynx, esophagus and stomach demonstrate negative for salivary aspiration.
2.5. Reliability of VFSS and radionuclide salivagram
To assess the inter-rater reliability of VFSS, the PAS of VFSS was analyzed by 2 experienced physiatrists. In addition, radionuclide salivagram was re-analyzed by a physiatrist who blinded to results of salivagram, and the results were compared with salivagram analysis of a nuclear medicine physician to assess the inter-rater reliability of the radionuclide salivagram. The inter-rater reliability (Crombach α value) of PAS was measured as 0.987, and that of the radionuclide salivagram was measured as 0.998.
3. Results and analysis
3.1. Statistical analysis
The comparison between the 2 groups was performed with either an independent sample t test or a Wilcoxon sum test, depending on the distribution of the continuous variables. A Chi-squared test was used to assess the independence of the categorical variables. Statistical analyses were performed using SPSS software, version 22.0 (SPSS, Chicago IL).
3.2. Patient characteristics
In total, 77 patients with brain lesion were enrolled in the study, with an average age of 70.36 ± 12.07 years. Of these, 47 (61.0%) were men and 30 (39.0%) were women (Table 2). Of 77 patients with brain lesion, there were 67 patients with stroke (87.0%), 4 patients with TBI (5.20%), 1 patient with a brain tumor (1.30%), and 2 patients with hypoxic ischemic encephalopathy (HIE) (2.60%).
Table 2.
Patient characteristics and comparison of the patients in the 2 groups.
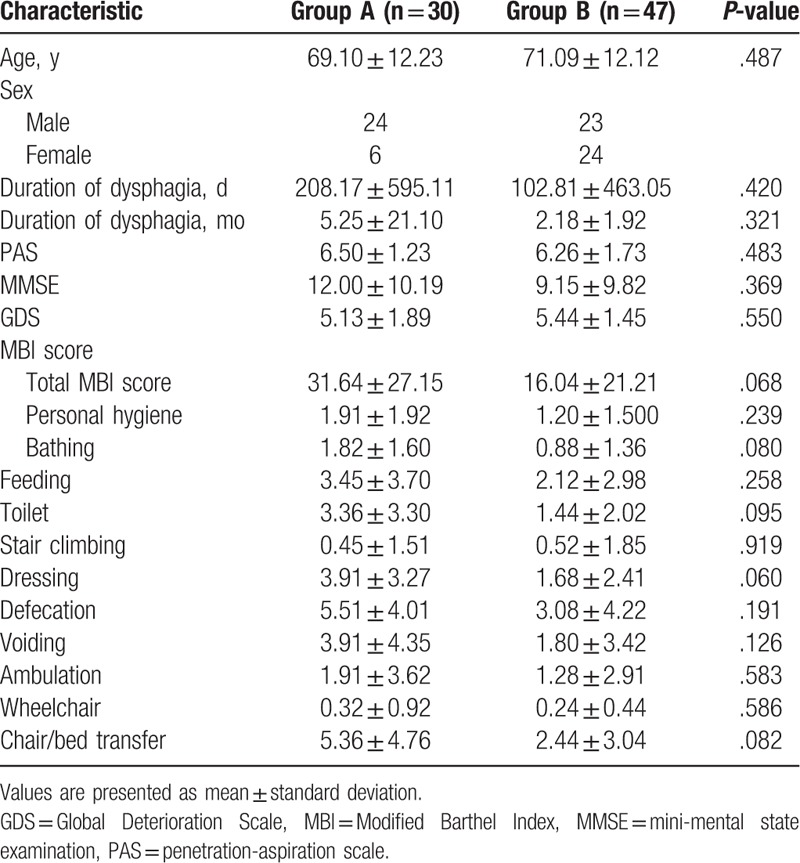
In group A (n = 47), there were 40 patients with stroke (85.1%), 2 patients with TBI (4.26%), 1 patient with a brain tumor (2.13%), 2 patients with HIE (4.26%), and 2 patients with Parkinson disease (4.26%). In group B (n = 30), there were 27 patients with stroke (90.0%), 2 patients with TBI (6.67%), and 1 patient with Parkinson disease (3.33%).
The duration of dysphagia onset was 5.25 ± 21.10 months in group A, and 2.18 ± 1.92 month in group B. However, there was no significant difference between groups A and B (P < .05)
3.3. Comparison of results of VFSS
In group A, there were 3 patients with penetration in VFSS (10.0%), and 27 patients with aspiration on VFSS (90.0%). In group B, there were 8 patients with penetration in VFSS (17.0%), and 39 patients with aspiration on VFSS (83.0%). The PAS of group A was 6.50 ± 1.23, and the PAS of group B was 6.26 ± 1.73 (Table 2). However, there was no significant difference between the 2 groups in PAS (P > .05).
3.4. Comparison of clinical variables between 2 groups based on solution volume
There was no significant difference between the 2 groups in areas such as age, MMSE, GDS, MBI, and history of aspiration pneumonia, except for the sex ratio (P > .05). However, there was a statistically significant difference in detection rate of salivary aspiration between group A (3.3%, 1/30) and group B (19.1%, 9/47) in the Chi-squared test (P < .05).
4. Discussion
To the best of our knowledge, there is no research investigating the difference in detection rate in salivary aspiration by radionuclide solution volume in radionuclide salivagrams. Salivary aspiration refers to saliva that is spilled over the tongue through the faucial isthmus.[8] It can lead to substantial respiratory morbidity, including unexplained lung diseases and recurrent pneumonia.[8] Although VFSS is a very important tool for evaluating aspiration of food and liquids, it may not detect salivary aspiration. Therefore, the radionuclide salivagram may have an important role in assessing the cause of aspiration pneumonia, such as salivary aspiration, compared with VFSS.
Presently, however, there are no definite guidelines for solution volume in radionuclide salivagram. The previous studies about radionuclide salivagrams have not shown consistency, especially in solution volumes of radionuclide.[8–10,13] Therefore, despite the usefulness of the salivagram, it was not uncommon to find different conflicting results in the detection rate of salivary aspiration in previous studies. Interestingly, in the results of our study, the detection rate of the high solution volume group (0.5 mL) was significantly higher than that of the low solution volume group (0.1 mL). These results are probably due to the fact that an excessive volume of radionuclide tends to produce the same effect as swallowing thin water, rather than pure salivary aspiration.
In normal subjects, saliva secretion increases from 0.3 mL/min during un-stimulation to 1 to 2 mL/min during stimulation.[15,16] Considering the amount of saliva secretion, it is believed that a large solution volume can induce a swallowing reaction and have a significant effect on the outcome of radionuclide salivarigram. Although additional research may be necessary to find an appropriate solution volume of nucleoclide in salivagrams, it seems necessary to minimize the solution volume in order to distinguish false positive salivary aspiration by the swallowing reaction due to a large amount of solution volume.
Our study has a few limitations. First, we could not compare solution volumes of various capacities: instead, only 2 solution volumes (0.1 mL vs 0.5 mL) were studied. So further prospective studies with more patients and various capacities of solution volume will be necessary to certify the results of our study. Second, this was a retrospective study with various diseases. Therefore, the effects of disease on the outcome of the salivagram could not be completely ruled out, although there were no significant differences in clinical variables, such as age, MMSE, GDS, total MBI score, PAS, and history of aspiration pneumonia between the 2 groups. However, it is obviously the first study which showed that solution volume may affect the results of a salivagram, so it seems to be sufficient as a preliminary study. Nevertheless, additional prospective research is considered to be necessary for patients with the same disease to completely eliminate the influence of diseases on salivagram results. In conclusion, even a small difference of the solution volume of radionuclide (0.1 mL vs 0.5 mL) in salivagram can affect the detection rate of salivary aspiration in patients with brain lesion. Therefore, it seems necessary to minimize the solution volume in order to distinguish false positive salivary aspiration caused by the swallowing reaction due to excessive solution volume. Further study with various solution volumes of radionuclide is warranted to establish the optimal solution volume of radionuclide salivagram.
Author contributions
Conceptualization: Jong Min Kim, Zeeihn Lee, Donghwi Park.
Data curation: Donghwi Park.
Writing – original draft: Dae Hee Lee, Donghwi Park.
Writing – review and editing: Donghwi Park.
Footnotes
Abbreviations: DTPA = diethylenetriamine pentaacetic acid, GDS = Global Deterioration Scale, MBI = Modified Barthel Index, MMSE = mini mental state examination, PAS = penetration-aspiration scale, TBI = traumatic brain injury, VFSS = videofluoroscopic swallowing study.
Disclosure: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT, and Future Planning (NRF-2017R1D1A1B03033127).
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
The authors have no conflicts of interest to disclose.
References
- [1].Katzan IL, Cebul RD, Husak SH, et al. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 2003;60:620–5. [DOI] [PubMed] [Google Scholar]
- [2].Vermeij FH, Scholte op Reimer WJ, de Man P, et al. Stroke-associated infection is an independent risk factor for poor outcome after acute ischemic stroke: data from the Netherlands Stroke Survey. Cerebrovasc Dis 2009;27:465–71. [DOI] [PubMed] [Google Scholar]
- [3].Lee WK, Yeom J, Lee WH, et al. Characteristics of dysphagia in severe traumatic brain injury patients: a comparison with stroke patients. Ann Rehabil Med 2016;40:432–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Terre R, Mearin F. Prospective evaluation of oro-pharyngeal dysphagia after severe traumatic brain injury. Brain Inj 2007;21:1411–7. [DOI] [PubMed] [Google Scholar]
- [5].Kim DH, Choi KH, Kim HM, et al. Inter-rater reliability of videofluoroscopic dysphagia scale. Ann Rehabil Med 2012;36:791–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Park D, Oh Y, Ryu JS. Findings of abnormal videofluoroscopic swallowing study identified by high-resolution manometry parameters. Arch Phys Med Rehabil 2016;97:421–8. [DOI] [PubMed] [Google Scholar]
- [7].Park D, Shin CM, Ryu JS. Effect of different viscosities on pharyngeal pressure during swallowing: a study using high-resolution manometry. Arch Phys Med Rehabil 2017;98:487–94. [DOI] [PubMed] [Google Scholar]
- [8].Lee ZI, Yu KJ, Lee DH, et al. The effect of nebulized glycopyrrolate on posterior drooling in patients with brain injury: two cases of different brain lesions. Am J Phys Med Rehabil 2017;96:e155–8. [DOI] [PubMed] [Google Scholar]
- [9].Heyman S, Respondek M. Detection of pulmonary aspiration in children by radionuclide “salivagram”. J Nucl Med 1989;30:697–9. [PubMed] [Google Scholar]
- [10].Heyman S. The radionuclide salivagram for detecting the pulmonary aspiration of saliva in an infant. Pediatr Radiol 1989;19:208–9. [DOI] [PubMed] [Google Scholar]
- [11].Park HW, Lee WY, Park GY, et al. Salivagram after gland injection of botulinum neurotoxin A in patients with cerebral infarction and cerebral palsy. PM R 2012;4:312–6. [DOI] [PubMed] [Google Scholar]
- [12].Yang J, Codreanu I, Servaes S, et al. Radionuclide salivagram and gastroesophageal reflux scintigraphy in pediatric patients: targeting different types of pulmonary aspiration. Clin Nucl Med 2015;40:559–63. [DOI] [PubMed] [Google Scholar]
- [13].Baikie G, South MJ, Reddihough DS, et al. Agreement of aspiration tests using barium videofluoroscopy, salivagram, and milk scan in children with cerebral palsy. Dev Med Child Neurol 2005;47:86–93. [DOI] [PubMed] [Google Scholar]
- [14].Wu H, Zhao R. Image characteristics and classification of salivagram in the diagnosis of pulmonary aspiration in children. Nucl Med Commun 2017;38:617–22. [DOI] [PubMed] [Google Scholar]
- [15].Navazesh M, Christensen C, Brightman V. Clinical criteria for the diagnosis of salivary gland hypofunction. J Dent Res 1992;71:1363–9. [DOI] [PubMed] [Google Scholar]
- [16].Sreebny LM, Valdini A. Xerostomia. Part I: relationship to other oral symptoms and salivary gland hypofunction. Oral Surg Oral Med Oral Pathol 1988;66:451–8. [DOI] [PubMed] [Google Scholar]


