Abstract
Background:
Placement of closed suction drains after total knee arthroplasty is an age-old practice; however, benefits and disadvantages of this procedure remain disputable in various studies.
Methods:
We performed an electronic database search in Medline/PubMed, the Cochrane Library, and Embase to retrieve publications with respect to this issue and then screened reference lists of related articles manually to obtain any additional ones. Randomized controlled trials (RCTs) evaluating the use of closed suction drains after primary total knee arthroplasty were eligible for this study. Useful data were extracted to calculate the pooled risk ratios (RRs) or weighted mean differences (WMDs) as well as corresponding 95% confidence intervals (CIs) as summary estimates.
Results:
Nineteen RCTs were included in the quantitative analysis. Compared with patients in the nondrainage group, those in the drainage group were significantly correlated with a decreased need of dressing change (RR = 0.31, 95% CI 0.12 to 0.79, P = .015) but an increased risk of homologous transfusion (RR = 1.38, 95% CI: 1.04–1.83) and longer time to regain straight-leg raising (WMD = 0.97 d, 95% CI: 0.48–1.46). Two groups showed no significant difference in total blood loss, hemoglobin drop, superficial wound infection, prosthetic joint infection, formation of deep vein thrombosis, duration of hospital stay, and range of movement.
Conclusions:
Based on this analysis, the use of closed suction drains after total knee arthroplasty is probably not superior to no drains for most outcome measures and therefore surgeons may wish to reconsider the routine use of this empirical practice until there is further evidence.
Keywords: closed suction drains, meta-analysis, randomized controlled trial, total knee arthroplasty
1. Introduction
Hematoma formation is a matter of concern after total knee arthroplasty. On the one hand, it was thought to provide a good medium for the colonization of bacteria and act as a risk factor of superficial wound infection and periprosthetic joint infection; one the other hand, increased tissue tension caused by a large hematoma might affect blood perfusion and joint mobility.[1,2] In order to evacuate blood trapped in the joint cavity, prevent the formation of hematoma and therefore reduce the incidence of abovementioned complications, an intraarticular closed suction drain is often installed at the end of total knee arthroplasty.[1] However, this age-old practice was questioned as multiple articles failed to demonstrate that fewer infections occurred owing to the use of drains; contrarily, some authors reported retrograde infection caused by bacteria migration through drain lumen.[3] Although lots of orthopedists still follow this practice empirically, debate over the benefits of closed suction drains has never stopped.[4–7] We performed a systematic review and meta-analysis with respect to this topic in 2011[8]; however, at that time, pooled analyses of several valuable outcome parameters were unavailable due to limited number of trials. Some high-quality studies were published in recent years and for the purpose of better illustrating this issue, an updated meta-analysis is requisite.
2. Method
We conducted this research according to the checklist of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.[9] The database search, literature selection, methodological assessment, and data abstraction were performed by 2 investigators (QYZ and LL) independently and repeatedly. Disagreement was settled by consensus or arbitration of the third investigator (WS). Informed consent or ethics approval was not needed due to that data pooled in the quantitative analysis were extracted from published articles.
2.1. Database search and literature selection
We performed a computerized search for 3 electronic databases including PubMed/Medline, Embase, and the Cochrane Library using queries combined by following keywords: (“drain” OR “drainage”) AND (“arthroplasty” OR “joint replacement”). No language or time limitations were imposed, and the last database search was conducted on June 14, 2017. Bibliographies of relevant articles were then hand checked to retrieve other additional articles of interest. Studies eligible for our meta-analysis had to meet the criteria listed below: study design, randomized controlled trial (RCT); population, candidates that require total knee arthroplasty; closed suction drains were adopted in the experimental group; and sufficient data were provided in regard to infection, blood loss, hemoglobin drop, transfusion, ecchymosis, deep vein thrombosis (DVT), range of motion, length of hospital stay, or other outcome estimates. After obviously unqualified and redundant publications were excluded by reading titles and abstracts, full texts of remainders were acquired and reviewed to ascertain their eligibility.
2.2. Data extraction and methodology quality assessment
For eligible studies, following information was extracted and imported to a predesigned Excel table: authors, published year, inclusion period, study design, demographic data of participants, related disorders, time to remove drains, criteria for homologous transfusion, length of follow-up, and methodological information. Methodological quality was assessed by using the Consolidated Standards of Reporting Trials (CONSORT) checklist.[10] This tool contains 22 items and a higher score represents better quality.
2.3. Statistical analysis
Heterogeneity across studies was quantitatively assessed by using I2 statistic and an I2 of <50% indicated a statistically nonsignificant heterogeneity. By using a random effect model, we calculated the pooled risk ratio (RR) and corresponding 95% confidence intervals (CIs) for dichotomous data; meanwhile, weighted mean difference (WMD) as well as associated 95% CIs was applied to compare continuous data. All statistical processes were performed by using STATA, Version 12.0 (StataCorp, College Station, TX).
3. Results
The database search and study selection processes are depicted in Fig. 1. Characteristics of included trials and enrolled subjects are presented in Tables 1 and 2.
Figure 1.
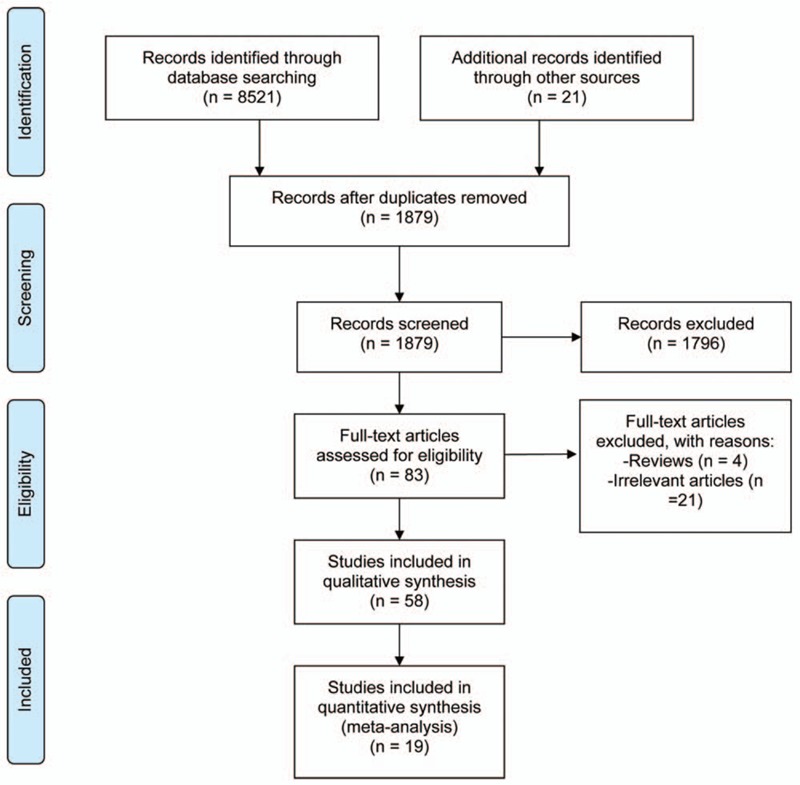
A flow chart summarizing the selection process of included RCTs for this meta-analysis.
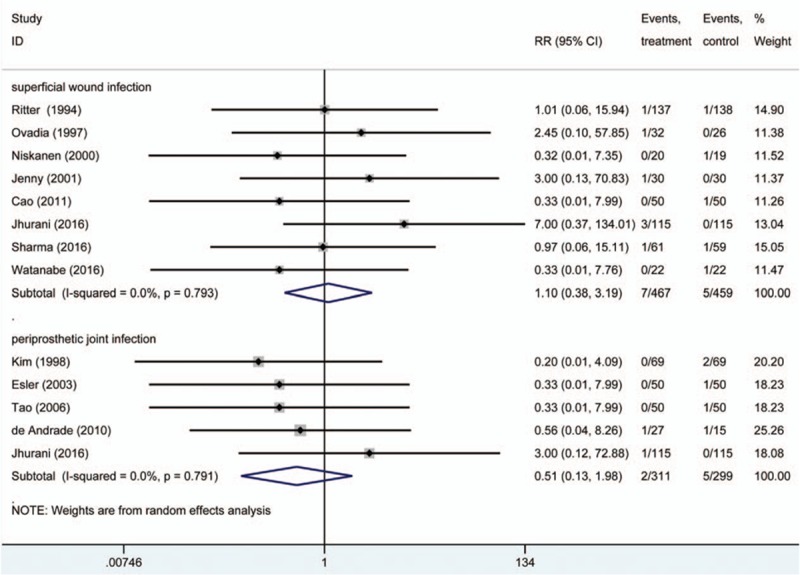
Table 1.
Characteristics of included studies.
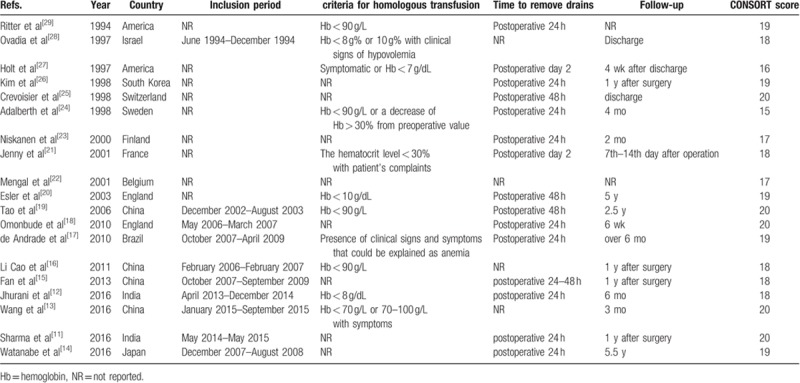
Table 2.
Demographic information of subjects.
Eventually, 19 RCTs[11–29] were considered eligible for this meta-analysis, 17[11–18,20,21,23–29] of which were published in English, 1[22] in French, and 1[19] in Chinese. Fourteen[11,13,17–22,24–29] trials reported the random method, of which 11[11,13,18–22,24–26,28] applied sealed envelope, 1[29] used randomization chart, 1[17] decided the grouping by tossing a coin, and 1[27] was a quasi-randomized trial. As to the inclusion criteria, 14[13,16–25,27–29] RCTs only enrolled patients receiving unilateral arthroplasty; 3[14,15,26] RCTs adopted self-control method, recruited patients receiving bilateral arthroplasty, and administrated one side with closed suction drain and another side without; 1[12] RCTs which did not apply self-control also enrolled only bilateral patients and 1[11] RCTs recruited bilateral and unilateral patients simultaneously. All studies investigated primary total knee arthroplasty (TKA) and adopted cemented endoprostheses.
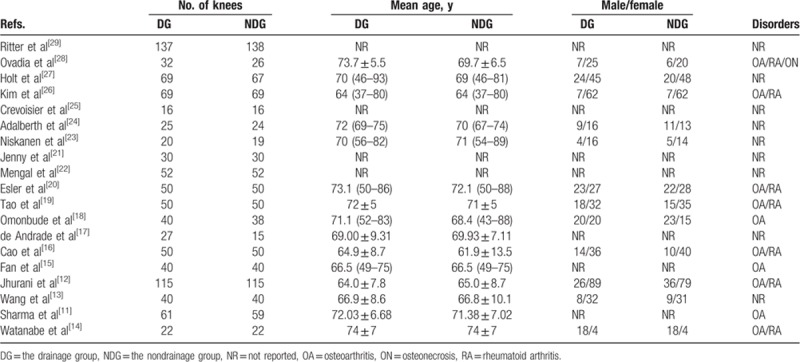
3.1. Infection
Eight[11,12,14,16,21,23,28,29] RCTs provided detailed data accessible to obtain RR and corresponding 95% CIs of superficial wound infection between 2 groups and 5[12,17,19,20,26] RCTs reported periprosthetic joint infection. There was no significant heterogeneity across included trials (I2 = 0 in both subgroup analyses). The pooled outcome estimates of these studies suggested that the use of closed suction drains did not significantly influence infection rate, either superficial wound infection (RR = 1.10, 95% CI: 0.38–3.19, P = .861) or periprosthetic joint infection (RR = 0.51, 95% CI: 0.13–1.98, P = .392) (Fig. 2).
Figure 2.
Incidence of postoperative infections between the drainage group and the nondrainage group.
3.2. Total blood loss, hemoglobin drop, and transfusion
Postoperative calculating blood loss contains 2 parts, namely, visible blood loss and hidden blood loss. Four[12,13,16,21] RCTs provided means and standard deviations of total blood loss in the drainage group and the nondrainage group, in which 3[12,13,16] trials assessed the exact blood loss by using Gross's formula and 1[21] did not depicted the method to calculate total blood loss. The pooled result indicated a trend toward more total blood loss in the drainage group compared with the nondrainage group but the difference was not statistically significant (WMD = 99.60 mL, 95% CI: −15.91 to 215.11, P = .091; P for heterogeneity <.01, I2 = 87.4%) (Fig. 3).
Figure 3.
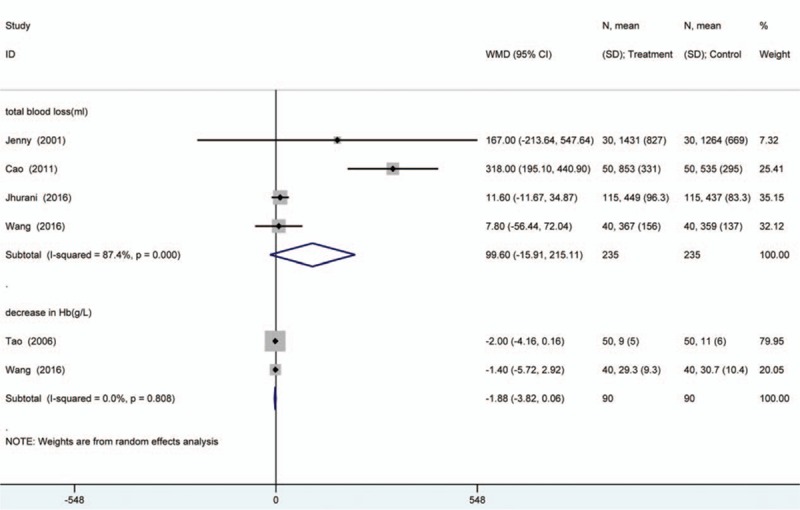
Postoperative total blood loss and hemoglobin drop between the drainage group and the nondrainage group.
Two[13,19] RCTs provided sufficient data accessible to calculate WMD and associated 95% CIs of hemoglobin drop between 2 groups. The summary estimate suggested that there was a trend toward more hemoglobin drop in the drainage group compared with the nondrainage group but the difference was not statistically significant, either (WMD = −1.88 g, 95% CI: −3.82 to 0.06, P = .057; P for heterogeneity = .808, I2 = 0%) (Fig. 3).
Ten[12,13,16,17,19–21,24,28,29] RCTs provided adequate data to calculate RR and associated 95% CIs of homologous transfusion rate between the drainage and the nondrainage groups. In this subgroup, the use of closed suction drains was correlated with a statistically increased rate of homologous transfusion (RR = 1.38, 95% CI: 1.04–1.83, P = .026; P for heterogeneity = .026, I2 = 52.3%) (Fig. 4). The significant heterogeneity across studies may result from the diverse standard to initiate transfusion.
Figure 4.
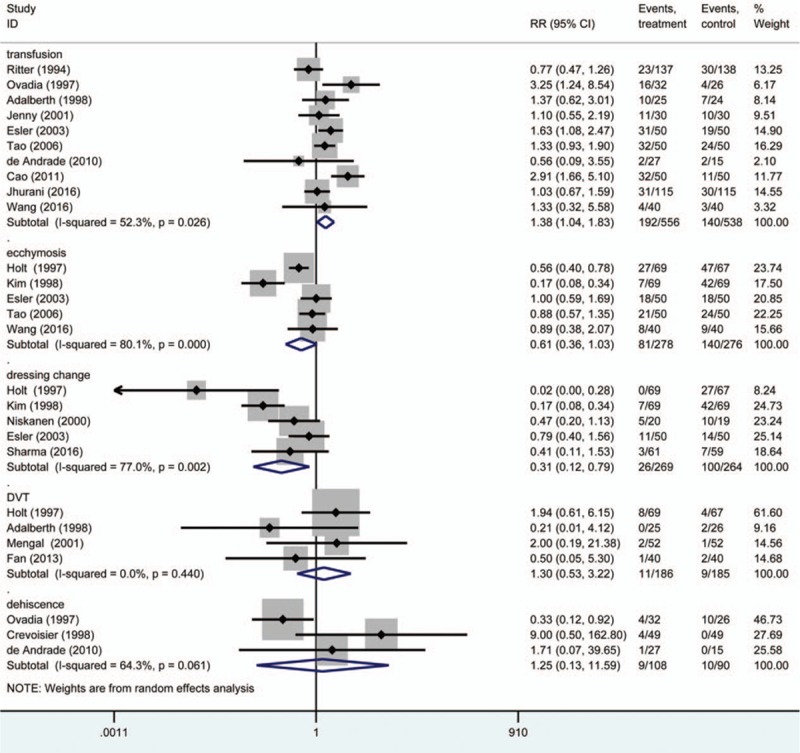
Incidence of postoperative homologous transfusion, ecchymosis, dressing change, DVT, and dehiscence between the drainage group and the nondrainage group.
3.3. Straight-leg raising and range of movement (ROM)
In 2[13,16] RCTs, investigators assessed the difference of time to regain straight-leg raising in the drainage group and nondrainage group. The WMD was 0.97 d (95% CI: 0.48–1.46, P < .001; P for heterogeneity = .701, I2 = 0%) (Fig. 5), which indicated that about one more day was needed to restore straight-leg raising for patients in the drainage group compared with those in the nondrainage group.
Figure 5.
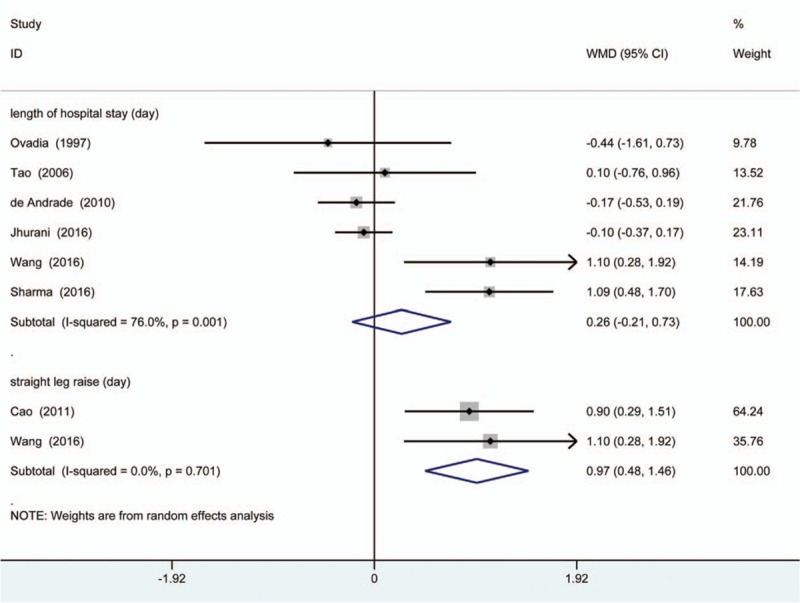
Duration of hospital stay and time to restore straight-leg raising between the drainage group and the nondrainage group.
Range of movement in 2 groups was available to be integrated and compared at postoperative day 1 (POD 7), POD 14, and long-term which was defined as more than 3 months after arthroplasty. There were 6,[14–17,19,21] 4,[15–17,19] and 6[13–17,19] RCTs provided adequate data to calculate WMDs and associated 95% CIs of ROM between 2 groups at 3 time points, respectively, which all did not make statistically significant difference (WMD = 1.12°, 95% CI: −1.92 to 4.16, P = .470; P for heterogeneity = .223, I2 = 28.2%; WMD = 1.58°, 95% CI: −3.29 to 6.45, P = .525; P for heterogeneity = .099, I2 = 52.1%; WMD = −0.31°, 95% CI: −0.10 to 1.55, P = .229; P for heterogeneity = .890, I2 = 0%, respectively) (Fig. 6).
Figure 6.
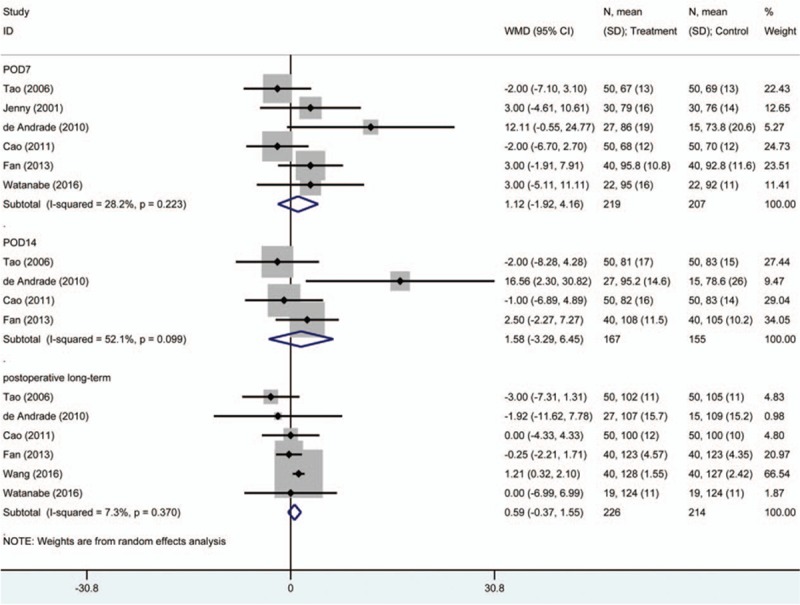
Postoperative range of movement between the drainage group and the nondrainage group.
3.4. Length of hospital stay, dressing reinforcement, and other complications
Six[11–13,17,19,28] studies provided enough data to assess the length of hospitalization in 2 groups and no statistically significant difference was found (WMD = 0.26 d, 95% CI: −0.21 to 0.73; P = .279; P for heterogeneity = .001, I2 = 76.0%) (Fig. 5).
Five[11,20,23,26,27] RCTs provided adequate data to calculate RR and corresponding 95% CIs of dressing reinforcement between the drainage and the nondrainage groups. In this subgroup, use of closed suction drains was associated with a decreased risk of dressing change (RR = 0.31, 95% CI: 0.12–0.79, P = .015; P for heterogeneity = .002, I2 = 77.0%) (Fig. 4).
Other complications, for instance, ecchymosis, DVT, and dehiscence were also analyzed in this study. There were 5,[13,19,20,26,27] 4,[15,22,24,27] and 3[17,25,28] RCTs provided adequate data to calculate RR and associated 95% CIs of ecchymosis, DVT, and dehiscence respectively between the drainage and the nondrainage groups. Statistical differences were not significant for all 3 outcome estimates (RR = 0.61, 95% CI: 0.36–1.03, P = .063 for ecchymosis; RR = 1.30, 95% CI: 0.53–3.22, P = .567 for DVT; and RR = 1.25, 95% CI: 0.13–11.59, P = .846 for dehiscence, respectively) (Fig. 4).
4. Discussion
Although placing closed suction drains after total knee arthroplasty is still a routine practice in the clinical setting, many orthopedists questions its value. The proposed benefits of drains include lower incidences of infection and wound complications, and possible shortcoming is more total blood loss. The former meta-analysis we performed focusing on this topic revealed several differences of outcome parameters between patients with and without closed suction drains.[8] However, due to the limited number of trials, some important indicators, such as total blood loss, hemoglobin drop, infection rate, range of movement, and length of hospital stay, were unavailable to be pooled or analyzed based on subgroups, which was specially emphasized in that article. Therefore, we conducted this updated systematic review and meta-analysis to further assess whether the application of closed suction drainage justified in patients undergoing total knee arthroplasty.
Infection after arthroplasty would bring catastrophic consequences and reducing the infection rate is the prime consideration for the application of closed suction drains. However, in the light of current evidence, no statistically significant correlation between drainage tube placement and infection (either superficial one or periprosthetic joint one) reduction could be detected. In a prospective investigation conducted by Willemen et al,[30] 41 patients receiving TKAs were randomly assigned to 2 groups according to the time of removing drains. Bacteria cultures of all drain tips cut off at postoperative 24 hours yielded negative results and surprisingly, Staphylococci were isolated from 5 of 21 drain tips indwelling for 48 hours after operation. These results indicated that closed suction drains did act as a source of retrograde infection and the risk increased with the extension of indwelling time.
Homologous blood transfusion may generate issues like hematogenous infections (i.e., hepatitis B, hepatitis C, and acquired immune deficiency syndrome), hemolytic reaction, anaphylactic reaction, and cardiopulmonary diseases. Some authors proposed that due to the lack of “self-tamponade” effect, the use of drains might be associated with an elevated amount of total blood loss; meanwhile, blood perfusion around the wound reactively increases within hours after operation and therefore the drain tubes were advised to be clamped for about 4 to 6 hours.[31,32] Although we did not observe a significant difference in calculating blood loss or hemoglobin drop between the drainage group and the nondrainage group, elevated rate of postoperative homologous blood transfusion did correlate with the insertion of closed suction drains. The plausible reason is the heterogeneous and sometimes subjective criteria for transfusion. These results were consistent with those of a noncontrolled trial conducted by Mardian et al.[33]
A drainage tube would obstruct physiotherapy in the early postoperative period[20]; at the same time, theoretically for patients without drains, hematoma formation, and organization in joint cavities may hinder early exercise, generate loads of scars, and reduce ROM. In the short run, closed suction drainage appears to interfere with the ability to regain straight-leg raising; however, similar ROM was obtained in both groups at 3 time points after operation. One possible explanation is that the early and arduous exercise in patients without drains help to prevent the scar adhesion and therefore maintain a satisfactory ROM.
Ecchymosis and dressing changing reflect the amount of fluid oozing out of the joint cavity to soft tissue or surgical dressing. As the blood and other fluids were evacuated, less dressing reinforcement in the short term after the operation was reported in the drainage group; meanwhile, the extent of ecchymosis of drainage group was greater than that in the nondrainage group.[26,27] However, short-term complications such as DVT and dehiscence appear to be irrelevant to the application of closed suction drains. Length of hospital stay, which comprehensively represents the occurrence of postoperative events, is also similar in 2 groups. In Watanabe et al's study[14] with a mean follow-up of 5.5 years, no differences in radiographic manifestations such as radiolucent lines around endoprostheses between those with and without drains was observed.
Results of meta-analysis should be interpreted cautiously. Although homologous transfusion rates between 2 groups showed a statistically significant difference, it was noted that lower limit of the 95% CIs of this summary estimate was close to invalid line, which represented a limited clinical value of this result. Meanwhile, closed suction drains do result in approximately one additional day to regain active straight-leg raising and one-third the need to conduct dressing change compared with those without drains. Except for these clinical parameters aforementioned, use of closed suction drains brings issues of nonnegligible material cost and labor burden. In Yin et al's prospective studies,[2] conservative estimates showed that approximately 31.87 dollars per patient were needed for drain use. Meanwhile, placement of closed suction drains extends operation time and as drains were removed at postoperative 24 hours or longer, it would increase the workloads of orthopedists and nurses.
Several limitations existed in this investigation. Firstly, number of analyzed studies in each subgroup analyses were small. Secondly, heterogeneity across studies could not be fully expounded, which indicated existence of unnoticed biased factors such as surgical operation, mental state, kinds of prosthesis, and so on. Last but not least, some demographic and methodological data were not reported in original studies. In spite of these concerns, limited value of closed suction drains in primary total knee arthroplasty was found in current meta-analysis.
5. Conclusions
Our investigations revealed that the placing closed suction drains after total knee arthroplasty proven to be ineffective for infection prevention, blood loss control, or functional recovery. Although drain usage could decrease the need for dressing reinforcement, it was also associated with an elevated rate of homologous transfusion and delayed time to regain the straight-leg raising. In conclusion, based on this analysis, the use of closed suction drains after total knee arthroplasty is probably not superior to no drains for most outcome measures and therefore surgeons may wish to reconsider the routine use of this empirical practice until there is further evidence.
Author contributions
Conceptualization: Wei Sun.
Data curation: Fuqiang Gao, Qidong Zhang.
Formal analysis: Fuqiang Gao, Liming Cheng, Zirong Li.
Funding acquisition: Wei Sun.
Investigation: Qingyu Zhang, Lihua Liu.
Methodology: Qingyu Zhang, Lihua Liu.
Project administration: Qingyu Zhang, Lihua Liu.
Supervision: Wei Sun, Qidong Zhang, Zirong Li.
Validation: Wei Sun.
Writing – original draft: Qingyu Zhang, Lihua Liu.
Writing – review & editing: Fuqiang Gao, Qidong Zhang, Liming Cheng.
Footnotes
Abbreviations: CI = confidence interval, CONSORT = Consolidated Standards of Reporting Trials, DVT = deep vein thrombosis, PRISMA = the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCT = randomized controlled trial, ROM = range of motion, RR = risk ratio, WMD = weighted mean difference.
Funding: This study was supported by the Natural Science Foundation of Beijing Municipality (7174346, 7182146), National Natural Science Foundation of China (81372013, 81672236), and Graduate Innovation Foundation of Peking Union Medical College (2017-1002-2-26).
QZ and LL contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Waugh TR, Stinchfield FE. Suction drainage of orthopaedic wounds. J Bone Joint Surg Am 1961;43-A:939–46. [PubMed] [Google Scholar]
- [2].Yin D, Delisle J, Banica A, et al. Tourniquet and closed-suction drains in total knee arthroplasty. No beneficial effects on bleeding management and knee function at a higher cost. Orthop Traumatol Surg Res 2017;103:583–9. [DOI] [PubMed] [Google Scholar]
- [3].Parker MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am 2004;86-A:1146–52. [DOI] [PubMed] [Google Scholar]
- [4].Chandratreya A, Giannikas K, Livesley P. To drain or not drain: literature versus practice. J R Coll Surg Edinb 1998;43:404–6. [PubMed] [Google Scholar]
- [5].Beer KJ, Lombardi AJ, Mallory TH, et al. The efficacy of suction drains after routine total joint arthroplasty. J Bone Joint Surg Am 1991;73:584–7. [PubMed] [Google Scholar]
- [6].Li N, Liu M, Wang D, et al. Comparison of complications in one-stage bilateral total knee arthroplasty with and without drainage. J Orthop Surg Res 2015;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Quinn M, Bowe A, Galvin R, et al. The use of postoperative suction drainage in total knee arthroplasty: a systematic review. Int Orthop 2015;39:653–8. [DOI] [PubMed] [Google Scholar]
- [8].Zhang QD, Guo WS, Zhang Q, et al. Comparison between closed suction drainage and nondrainage in total knee arthroplasty: a meta-analysis. J Arthroplasty 2011;26:1265–72. [DOI] [PubMed] [Google Scholar]
- [9].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 2011;9:672–7. [DOI] [PubMed] [Google Scholar]
- [11].Sharma GM, Palekar G, Tanna DD. Use of closed suction drain after primary total knee arthroplasty—an overrated practice. SICOT J 2016;2:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jhurani A, Shetty GM, Gupta V, et al. Effect of closed suction drain on blood loss and transfusion rates in simultaneous bilateral total knee arthroplasty: a prospective randomized study. Knee Surg Relat Res 2016;28:201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wang D, Xu J, Zeng WN, et al. Closed suction drainage is not associated with faster recovery after total knee arthroplasty: a prospective randomized controlled study of 80 patients. Orthop Surg 2016;8:226–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Watanabe T, Muneta T, Yagishita K, et al. Closed suction drainage is not necessary for total knee arthroplasty: a prospective study on simultaneous bilateral surgeries of a mean follow-up of 5.5 years. J Arthroplasty 2016;31:641–5. [DOI] [PubMed] [Google Scholar]
- [15].Fan Y, Liu Y, Lin J, et al. Drainage does not promote post-operative rehabilitation after bilateral total knee arthroplasties compared with nondrainage. Chin Med Sci J 2013;28:206–10. [DOI] [PubMed] [Google Scholar]
- [16].Li Cao, Nijat A, Askar M. No clear advantage to use of wound drains after unilateral total knee arthroplasty: a prospective randomized, controlled trial. J Arthroplasty 2011;26:519–22. [DOI] [PubMed] [Google Scholar]
- [17].de Andrade MA, de Oliveira CT, Silva BF, et al. Six month follow-up of patients submitted to total knee arthroplasty with and without placement of suction drainage devices. Rev Bras Ortop 2010;45:549–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Omonbude D, El MM, O’Connor PJ, et al. Measurement of joint effusion and haematoma formation by ultrasound in assessing the effectiveness of drains after total knee replacement: a prospective randomised study. J Bone Joint Surg Br 2010;92:51–5. [DOI] [PubMed] [Google Scholar]
- [19].Tao K, Wu HS, Li XH, et al. The use of a closed-suction drain in total knee arthroplasty: a prospective, randomized study. Zhonghua Wai Ke Za Zhi 2006;44:1111–4. [PubMed] [Google Scholar]
- [20].Esler CN, Blakeway C, Fiddian NJ. The use of a closed-suction drain in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br 2003;85:215–7. [DOI] [PubMed] [Google Scholar]
- [21].Jenny JY, Boeri C, Lafare S. No drainage does not increase complication risk after total knee prosthesis implantation: a prospective, comparative, randomized study. Knee Surg Sports Traumatol Arthrosc 2001;9:299–301. [DOI] [PubMed] [Google Scholar]
- [22].Mengal B, Aebi J, Rodriguez A, et al. A prospective randomized study of wound drainage versus non-drainage in primary total hip or knee arthroplasty. Rev Chir Orthop Reparatrice Appar Mot 2001;87:29–39. [PubMed] [Google Scholar]
- [23].Niskanen RO, Korkala OL, Haapala J, et al. Drainage is of no use in primary uncomplicated cemented hip and knee arthroplasty for osteoarthritis: a prospective randomized study. J Arthroplasty 2000;15:567–9. [DOI] [PubMed] [Google Scholar]
- [24].Adalberth G, Bystrom S, Kolstad K, et al. Postoperative drainage of knee arthroplasty is not necessary: a randomized study of 90 patients. Acta Orthop Scand 1998;69:475–8. [DOI] [PubMed] [Google Scholar]
- [25].Crevoisier XM, Reber P, Noesberger B. Is suction drainage necessary after total joint arthroplasty? A prospective study. Arch Orthop Trauma Surg 1998;117:121–4. [DOI] [PubMed] [Google Scholar]
- [26].Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total knee arthroplasties. Clin Orthop Relat Res 1998;347:188–93. [PubMed] [Google Scholar]
- [27].Holt BT, Parks NL, Engh GA, et al. Comparison of closed-suction drainage and no drainage after primary total knee arthroplasty. Orthopedics 1997;20:1121–4. 1124–1125. [DOI] [PubMed] [Google Scholar]
- [28].Ovadia D, Luger E, Bickels J, et al. Efficacy of closed wound drainage after total joint arthroplasty. A prospective randomized study. J Arthroplasty 1997;12:317–21. [DOI] [PubMed] [Google Scholar]
- [29].Ritter MA, Keating EM, Faris PM. Closed wound drainage in total hip or total knee replacement. A prospective, randomized study. J Bone Joint Surg Am 1994;76:35–8. [DOI] [PubMed] [Google Scholar]
- [30].Willemen D, Paul J, White SH, et al. Closed suction drainage following knee arthroplasty. Effectiveness and risks. Clin Orthop Relat Res 1991;264:232–4. [PubMed] [Google Scholar]
- [31].Senthil KG, Von Arx OA, Pozo JL. Rate of blood loss over 48 hours following total knee replacement. Knee 2005;12:307–9. [DOI] [PubMed] [Google Scholar]
- [32].Sa-ngasoongsong P, Chanplakorn P, Wongsak S, et al. An in vivo study of low-dose intra-articular tranexamic acid application with prolonged clamping drain method in total knee replacement: clinical efficacy and safety. Biomed Res Int 2015;2015:164206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Mardian S, Matziolis G, Schwabe P. Influence of wound drainage in primary total knee arthroplasty without tourniquet. Int Orthop 2015;39:435–40. [DOI] [PubMed] [Google Scholar]


