Summary
Introduction
In testicular torsion, ischemia time from pain onset impacts testicular salvage. A tunica albuginea fasciotomy to relieve compartment pressure followed by a tunica vaginalis flap (TVF) may enhance salvage.
Objective
To define the optimal window of ischemia time during which TVF may be most beneficial to avoid orchiectomy.
Study design
A retrospective cohort study of males presenting with testicular torsion at a single tertiary-care institution from January, 2003 to March, 2017. Ischemia time was defined as duration of pain from onset to surgery. Because TVF would be an option to orchiectomy, and it was found that ischemia time was longer in testicles that underwent orchiectomy, matching was performed. Cases of torsion treated with TVF were matched 1:1 with cases treated with orchiectomy on age at surgery, and ischemia time. Outcomes included postoperative viability, defined as palpable testicular tissue with normal consistency, and atrophy, defined as palpable decrease in size relative to contralateral testicle. Sensitivity analyses were performed restricting to the subgroups with postoperative ultrasound, >6 months’ follow-up, and additionally matching for degrees of twist.
Results
A total of 182 patients met eligibility criteria, of whom 49, 36, and 97 underwent orchiectomy, TVF, and septopexy alone, respectively. Median follow-up was 2.7 months; 26% of patients had postoperative ultrasound (61% of TVF group). In the orchiectomy, TVF, and septopexy groups, respectively, median ischemia times were 51, 11, and 8 hours, postoperative viability rates were 0, 86, and 95%, and postoperative atrophy rates were 0, 68, and 24%. After matching, 32 patients with TVF were matched to 32 patients who underwent orchiectomy. In the TVF group, postoperative viability occurred in 95% (19/20) vs 67% (8/12) of patients with ischemia times ≤24 and >24 hours, respectively (Summary table). Atrophy occurred in 67% (12/18) vs 83% (10/12) of these same respective patients. Sensitivity analysis by ultrasound and longer follow-up found similar viability results, although atrophy rates were higher. Additional matching for degrees of twist showed lower viability and higher atrophy rates for increasing ischemia times.
Discussion
Patients who presented with testicular torsion with ischemia times ≤24 hours and who were being considered for orchiectomy may have benefitted most from TVF, albeit at high risk of atrophy. However, for ischemia times >24 hours, TVF may still have preserved testicular viability in two-thirds of cases. A limitation was short follow-up.
Conclusion
A TVF was a valid alternative to orchiectomy for torsed testicles, albeit with high testicular atrophy rates.
Keywords: Testicular torsion, Testicular compartment syndrome, Tunica vaginalis flap, Testicular atrophy, Testicular viability
Introduction
Testicular torsion is a potentially devastating acute surgical emergency. With an annual incidence of 1 per 4000 males aged <25 years, torsion occurs when the testicular vessels twist [1]. Subsequent ischemia to the testicle makes torsion highly time-sensitive [1]. Rates of salvage decline rapidly the longer the duration of ischemia time from onset of pain, with orchiectomy rates inversely rising and nearing 80–90% when ischemia times exceed 24 hours [2].
Various techniques have been developed for enhancing salvage rates at the time of surgery, including: clinical pathways to expedite the process from emergency room admission to operating room [3]; manual detorsion while awaiting surgery [4]; and assessing for bleeding after a deep incision into the testicle [5] to assess possible viability. One innovation has been the conceptualization of torsion as a form of compartment syndrome, with fasciotomy through the tunica albuginea relieving the intra-compartmental pressure [6]. An adjacent tunica vaginalis flap (TVF) could be mobilized and used to cover the defect in the tunica albuginea rather than primarily closing the tunica albuginea, which recreates compartment syndrome [6]. While the success rate of TVF repair has been previously explored [7], defining the window of ischemia time for optimal utilization of this method has not yet been performed. In addition, a thorough time-stratified assessment of viability versus atrophy of the affected testicle is lacking.
The current study therefore sought to further characterize these gaps in knowledge of the utility of TVF repair for testicular torsion. It also shared a current clinical algorithm developed since the TVF repair was first described [6]. It was hypothesized that: of torsed testicles being considered for orchiectomy and not septopexy alone TVF repair may be optimally suited for ischemia times ≤24 hours.
Materials and Methods
Study design and setting
This was a retrospective cohort study of an Institutional Review Board-approved prospective patient registry of patients who presented with testicular torsion at a single tertiary referral center. Patients could have arrived by car, ambulance, or helicopter.
The institutional clinical pathway for acute scrotal pain in the Emergency department includes initial rapid assessment by the Emergency department team. Scrotal ultrasound is utilized depending on the clinical suspicion of the Emergency department team. Once Urology is consulted after diagnosis of acute torsion, time to the operating room is routinely within the hour.
Participants
All children aged ≤21 years who underwent surgery for testicular torsion between January, 2003 and March, 2017 were reviewed. Children were excluded from analysis if they had bilateral torsion, extravaginal torsion, intermittent torsion, torsion in an undescended testicle, were aged <5 years (due to potential heterogeneity in presentation compared to older children), or had no follow-up visit to document postoperative findings. Children who had an estimated ischemia time of >96 hours were further excluded because of the very low chance of viability.
Exposures
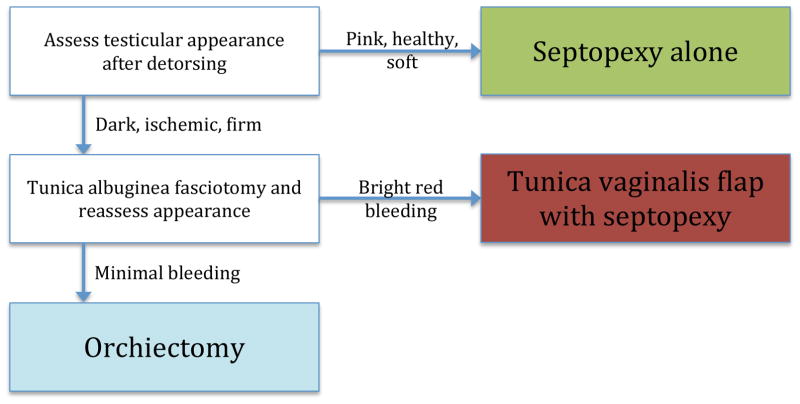
The primary exposure of interest was use of TVF. Three tunica vaginalis grafts were included, since the concept is the same. The surgery chosen – orchiectomy, TVF, or septopexy alone without TVF – was at the discretion of the operating surgeon. This decision was not based solely on estimated hours of ischemia, but rather on the appearance of the testicle once delivered onto the operative field, its subsequent appearance after reducing the torsion, and its subsequent appearance after a fasciotomy was made in the tunica albuginea. The intra-operative clinical algorithm is shown in Fig. 1. For patients who underwent TVF, the technique has been previously described [6]. Drains were placed as needed. The general follow-up protocol included a postoperative visit within the first 2–6 weeks after surgery, repeated every 2–3 months if needed. Scrotal ultrasound was obtained on a case-by-case basis.
Fig. 1.
Intraoperative algorithm for acute testicular torsion.
Outcomes
The primary outcome was testicular viability from the latest follow-up visit. For patients who underwent a scrotal ultrasound, viability was defined as having normal blood flow to the affected testicle, regardless of testicular size. For patients who did not undergo a scrotal ultrasound, viability was defined by the examining surgeon as palpable testicular tissue, regardless of size, of normal consistency and firmness in the affected testicle that would be thought to survive.
A secondary outcome was testicular atrophy from the latest follow-up visit. Atrophy was defined as smaller size of the affected testicle relative to the contralateral healthy testicle on scrotal ultrasound or on palpation. Because documentation was lacking on % size decrease on palpation, this outcome was dichotomized into any atrophy versus none. If no specific indication of the presence or absence of atrophy was noted for a patient on follow-up, it was kept as a missing value.
Covariates
Other characteristics that were collected included age at surgery (continuous), laterality, estimated ischemia time in hours from pain onset to surgery (<6, 6–12, 12–24, 24–48, 48–96), and degrees of twist found intra-operatively (<360, 360–720, >720, unknown).
Statistical analysis
Univariate analyses using Fisher’s exact and Kruskal-Wallis tests for categorical and continuous variables, respectively, were used to compare the orchiectomy, TVF, and detorsion alone groups. Because TVF would be considered if orchiectomy were considered (Fig. 1) and ischemia times were significantly longer in testicles that underwent orchiectomy than TVF, a matched analysis of TVF and orchiectomy patients was performed to explore viability and atrophy rates after TVF, given the same clinical characteristics that otherwise would have led to orchiectomy.
Each patient who underwent TVF was matched 1:1 with a patient who underwent orchiectomy. The study exactly matched on estimated ischemia time within each pair and then balanced the age at surgery by minimizing the Mahalanobis distance [8] between TVF and orchiectomy patients, using a caliper of 0.1 standard deviations. Matching was performed with replacement of patients who underwent orchiectomy, to ensure best matches and maximize analysis of TVF cases. All matches were performed first without viewing outcomes [9]. Balance after matching was assessed using standardized mean differences (SMD), which ignored sample sizes, with values <0.1 deemed as excellent [10].
Three sensitivity analyses were performed. The first restricted the matched cohort analysis to those patients who only completed a postoperative scrotal ultrasound. A second sensitivity analysis was performed where degrees of twist was included in the matching algorithm; the primary analysis had excluded degrees of twist because of missing data for this covariate. A third restricted the matched cohort to those with only >6 months of follow-up.
Given that data were sparse regarding viability and atrophy rates following TVF, no power calculations were performed; this was considered an exploratory and hypothesis-generating study. As such, no formal statistical tests were performed comparing TVF to orchiectomy outcomes in the matched analysis. All analyses were performed with Stata (v14, StataCorp, College Station, TX) with a two-tailed alpha of 0.05.
Results
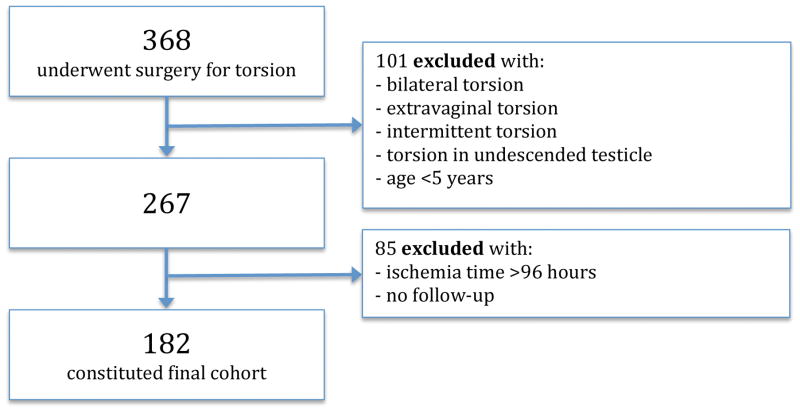
During the study time frame, 368 patients underwent surgery for testicular torsion. After applying exclusion criteria, 182 remained and constituted the study cohort (Fig. 2). Intra-operative assessment of degrees of twist was missing in 43 patients (24%); postoperative atrophy was missing in 46 patients (25%).
Fig. 2.
Study flowchart.
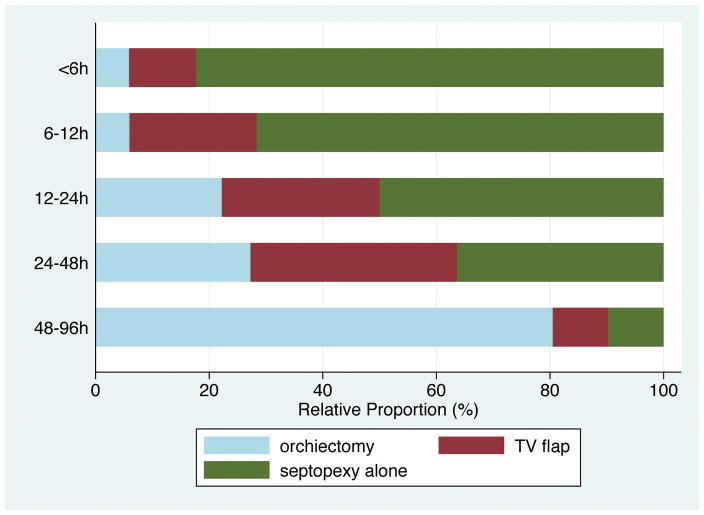
Of the 182 patients: 49, 36, and 97 underwent orchiectomy, TVF, and septopexy alone, respectively (Table 1). Median age at surgery was 14 years (range 5–18). Median overall follow-up was 2.7 months; in the TVF group, median follow-up was 4.5 months (interquartile range 2.1–12.5). In the orchiectomy, TVF, and septopexy alone groups, respectively, median ischemia times were 51, 11, and 7 hours; postoperative viability rates were 0, 86, and 95%; and postoperative atrophy rates were 0, 68, and 24%. Patients who only had septopexy had more right-sided torsions than the other groups. Of patients who had degrees of twist documented, orchiectomy patients had significantly higher degrees of twist compared to TVF and septopexy alone patients (median 540 vs 360 vs 315, respectively). Postoperative ultrasound was performed on 47 patients (26%); among TVF patients, 22 (61%) received a postoperative ultrasound. When stratified by estimated ischemia time, relative rates of orchiectomy increased with increasing ischemia time (Fig. 3). After successfully matching 32 patients with TVF to 32 patients with orchiectomy, excellent balance in age at surgery and ischemia time was achieved between the orchiectomy and TVF groups (Supplemental Table 1). In the TVF group, atrophy data were missing in two of the 32 (6%) patients.
Table 1.
Cohort characteristics by surgery type.
| Variable | Detorsion | TVF | Orchiectomy | P-value |
|---|---|---|---|---|
| Number (%) | 97 (53) | 36 (20) | 49 (27) | |
| Ischemia time, hours, median (IQR) | 7 (5–11) | 11 (6–26) | 51 (29–72) | <0.001 |
| Ischemia time, hours, n (%) | <0.001 | |||
| <6 | 28 (29) | 4 (11) | 2 (4) | |
| 6–12 | 48 (50) | 15 (42) | 4 (8) | |
| 12–24 | 9 (9) | 5 (14) | 4 (8) | |
| 24–48 | 8 (8) | 8 (22) | 6 (12) | |
| 48–96 | 4 (4) | 4 (11) | 33 (67) | |
| Age, years, median (IQR) | 15 (13–16) | 14 (13–15) | 14 (13–14) | 0.03 |
| Left laterality, n (%) | 47 (49) | 26 (72) | 32 (67) | 0.03 |
| Degrees of twist, median (IQR)* | 315 (180–540) | 360 (180–720) | 540 (360–720) | <0.001 |
| Ultrasound, n (%) | 21 (22) | 22 (61) | 4 (8) | <0.001 |
| Viability, n (%) | 90 (95) | 31 (86) | - | 0.14 |
| Atrophy, n (%) | 19 (24) | 23 (68) | - | <0.001 |
| Follow-up, months, median (IQR) | 2.2 (1.4–3.8) | 4.5 (2.1–12.5) | 2.6 (1.2–5.2) | 0.006 |
P-values from Kruskal-Wallis and Fisher’s exact tests for continuous and categorical variables, respectively.
Data on degrees of twist available for 38, 27, and 74 patients in orchiectomy, TVF, and detorsion groups, respectively.
IQR, interquartile range; TVF, tunica vaginalis flap
Fig. 3.
Relative rates of surgical type by ischemia time (in hours).
Within the matched cohort, clinical viability was 95% (19 of 20) using TVF until ischemia time was >24 hours (Table 2), at which point viability rates appeared to decrease. For ischemia times of 24–48 and 48–96 hours, respectively, 63% (five of eight) and 75% (three of four) of patients who underwent TVF were clinically viable; there was a cumulative viability rate of 67% (8 of 12) for ischemia time >24 hours. Clinical atrophy was common. For ischemia times ≤24 hours, the atrophy rate was 67% (12 of 18). For ischemia times >24 hours, the atrophy rate was 83% (10 of 12).
Table 2.
Outcomes in matched cohort of TVF and orchiectomy patients.
| Outcome | Ischemia time, hours | TVF, n (%) |
|---|---|---|
| Overall viability (n=32) | <6 | 0 (0) |
| 6–12 | 14/15 (93) | |
| 12–24 | 5/5 (100) | |
| 24–48 | 5/8 (63) | |
| 48–96 | 3/4 (75) | |
| Overall atrophy (n=32) | <6 | 0 (0) |
| 6–12 | 10/14 (71) | |
| 12–24 | 2/4 (50) | |
| 24–48 | 6/8 (75) | |
| 48–96 | 4/4 (100) |
TVF, tunica vaginalis flap
The viability results were similar on sensitivity analysis when restricted to radiographic follow-up; atrophy rates were worse (Supplemental Table 2). For ischemia times ≤24 hours, the viability and atrophy rates were 91% (10 of 11) and 91% (10 of 11), respectively. For ischemia times >24 hours, the viability and atrophy rates were 63% (five of eight) and 100% (eight of eight), respectively. Despite smaller sample size, the second sensitivity analysis that additionally matched on degrees of twist showed similar results – for the same degrees of twist, increasing ischemia time was associated with lower viability and higher atrophy rates (Supplemental Table 3). Upon restriction to testicles with >6-months follow-up, viability rates were 90% (9 of 10) for ischemia times ≤24 hours, compared to 60% (three of five) for ischemia >24 hours (Supplemental Table 4). Atrophy rates were, respectively, 80% (8 of 10) and 100% (five of five).
Discussion
The current findings from the overall cohort confirm that with increasing ischemia time from onset of pain, rates of orchiectomy rise while rates of septopexy alone fall. Repair with TVF offers a method through which to salvage certain testicles that otherwise would be removed. In the current matched cohort study, the use of TVF in testicles otherwise being considered for orchiectomy appeared to confer higher viability and lower atrophy if ischemia times were ≤24 hours vs >24 hours. For ischemia times >24 hours, testicles treated with TVF were viable in nearly two thirds of cases, albeit at higher risk of atrophy. The current results suggest a clinical niche for application of TVF in testicular torsion, but warrant tempering patient/parent expectations of full recovery.
The immediate benefit of TVF at time of initial detorsion is obvious: the testicle is preserved and not removed. It is important to note that TVF should not be considered when detorsion alone with septopexy is possible, which suggests less severe testicular injury, but rather when orchiectomy is the alternative (Fig. 1). Thus, TVF outcomes should not be compared directly to detorsion alone outcomes. Early series of the TVF technique have indicated promising results. The original description, in 2008, of TVF in three patients found symmetric clinical and radiographic salvage in two of three patients, with a third showing signs of radiographic atrophy but preserved blood flow [6]. Since this study others have shared their experience with TVF. In Toronto, 59 patients presented with acute torsion requiring surgical exploration over 10 years; of these, 11 underwent detorsion with TVF with a mean ischemia time of 31 hours [7]. The authors obtained scrotal ultrasound on follow-up for all 11 TVF patients, with 54% (6 of 11) meeting stringent criteria for salvage (normal blood flow with <50% relative atrophy) that otherwise would have been removed. Given differences in the definition of salvage by Figueroa et al., their salvage rate of 54% is comparable with the current viability rate of 63% for >24 hours on strictly radiographic assessment. Overall, both the findings by Figueroa et al. and the current results consisted of low numbers. Larger-sized studies with radiographic follow-up are warranted to be able to draw more definite conclusions about the benefits of TVF.
Less is known about the potential harms of TVF utilization in testicular torsion. Although the aims of the current study were not to examine the specific effects of TVF on fertility, it is necessary to discuss briefly. One study of men who had undergone orchiectomy for torsion noted abnormal semen analyses, though no different from other mono-orchid men [11]. Another study of boys who underwent septopexy versus orchiectomy for torsion noted lower serum inhibin B levels when compared to age-matched healthy controls, but normal levels of serum testosterone, follicle-stimulating hormone, and luteinizing hormone [12]. Concern for infertility may arise due to violation of the blood-testis barrier with the incision through tunica albuginea. However, levels of direct anti-sperm antibody in patients with septopexy or orchiectomy for torsion were not significantly different from those of normal controls [13]. Additionally, a study of prepubertal open testis biopsies showed no subsequent evidence of direct anti-sperm antibodies [14]. Of note, no studies have explicitly included patients with TVF repair; this remains a knowledge gap to be addressed by future studies.
The risk of subsequent testicular atrophy for preserved testicles can be substantial. The current study found that for testicles that had been twisted for >24 hours, the rate of clinical atrophy was 83% with the TVF technique. Even for ischemia times ≤24 hours, atrophy occurred in 67% of TVF testicles. However, two points must be clarified regarding atrophy: first, presence of atrophy does not equal loss of complete testicular function, which would result from orchiectomy; second, atrophy likely results not from interventions at time of initial scrotal exploration, but rather from the cumulative ischemic injury to the testicle. Evidence of the latter is that atrophy may result from simple detorsion alone. An older study of 64 boys who underwent detorsion alone for testicular torsion during 1979–1991, with follow-up in 25 boys, found a 100% atrophy rate for testicles twisted beyond 24 hours [15]. Another study of over 500 torsed testicles that underwent detorsion alone showed an atrophy rate of 80% for ischemia times >24 hours [2]. In the current overall cohort, detorsion alone for torsions with >24 hours of ischemia time yielded an atrophy rate of 60% (6 of 10) (data not shown). As stated previously, the decision to perform detorsion alone (versus TVF or orchiectomy) is not solely dependent on the ischemia time, but rather a stepwise algorithm of clinical appearance, as shown in Fig. 1. For some testicles twisted >24 hours, intra-operative recovery after simple detorsion might be substantial enough to require no more than straightforward septopexy. However, for other testicles twisted >24 hours orchiectomy may be the gold standard. It is in this latter group, not the former, that TVF for decompression of testicular compartment syndrome is advocated for consideration.
The current study had several limitations. First, follow-up protocols were not standardized with a scrotal ultrasound. Thus, 61% of TVF patients had radiographic documentation of viability and atrophy, which was based on surgeon preference and may have introduced selection bias. However, the results for viability were similar when restricted only to the subgroup that had radiographic follow-up (95 vs 91% for ischemia times ≤24 hours, and 67 vs 63% for >24 hours, respectively). Second, as with all observational studies, the study faced potential unobserved confounding, misclassification of ischemia time or outcomes, and other sources of selection bias. However, it tried to address these shortcomings by applying stringent exclusion criteria, separating the outcomes of viability from atrophy, and using a matching methodology to pair TVF and orchiectomized testicles with similar ischemia times. Additionally, the possibility of conducting a randomized trial regarding testicular torsion is likely very low, leaving observational studies as the best possible type of study. Third, the study was derived from a single institution and hence limited in generalizability. It is unclear whether national practice patterns reflect the utilization of TVF as much as at the current institution. However, with at least one other major tertiary referral center publishing their early experience with TVF [7], it is hoped that others will follow suit. Lastly, the follow-up period was short and fertility effects of TVF repair were unknown. Longer-term reassessment of testicular viability and atrophy is currently ongoing. It is hoped that multi-institutional prospective cohorts can be formed and followed with formal semen analyses collected once puberty is completed.
In conclusion, the TVF technique allows select torsed testicles otherwise destined for orchiectomy to be preserved, albeit at risk of subsequent atrophy. The optimal clinical setting for TVF may be those rare testicles with ischemia times ≤24 hours where orchiectomy is being considered. However, for ischemia times >24 hours where orchiectomy rates are higher, TVF still may be a valid option. This study offered a clinical algorithm for utilization of TVF, and encourages others to follow and modify as needed. Though a promising technique for one of the true pediatric urological emergencies, TVF requires further long-term large-scale study into its benefits and potential harms.
Supplementary Material
Summary table.
Outcomes in matched cohort of TVF and orchiectomy patients.
| Outcome | Ischemia time, hours | TVF, n (%) |
|---|---|---|
| Overall viability (n=32) | <6 | 0 (0) |
| 6–12 | 14/15 (93) | |
| 12–24 | 5/5 (100) | |
| 24–48 | 5/8 (63) | |
| 48–96 | 3/4 (75) | |
| Overall atrophy (n=32) | <6 | 0 (0) |
| 6–12 | 10/14 (71) | |
| 12–24 | 2/4 (50) | |
| 24–48 | 6/8 (75) | |
| 48–96 | 4/4 (100) |
TVF, tunica vaginalis flap
Acknowledgments
Funding source: This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (grant number T32-DK007785-14 to DIC). The NIDDK had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily represent the official view of the NIDDK.
Footnotes
Ethical approval: This protocol was reviewed and approved by the Institutional Review Board.
Conflicts of interest: The authors declare no conflicts of interest.
Data statement: All research data used in this study are confidential and unable to be shared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159:1167–71. doi: 10.1001/archpedi.159.12.1167. [DOI] [PubMed] [Google Scholar]
- 2.Visser AJ, Heyns CF. Testicular function after torsion of the spermatic cord. BJU Int. 2003;92:200–3. doi: 10.1046/j.1464-410x.2003.04307.x. [DOI] [PubMed] [Google Scholar]
- 3.Afsarlar CE, Ryan SL, Donel E, Baccam TH, Jones B, Chandwani B, et al. Standardized process to improve patient flow from the Emergency Room to the Operating Room for pediatric patients with testicular torsion. J Pediatr Urol. 2016;12:233e1–4. doi: 10.1016/j.jpurol.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 4.Dias Filho AC, Oliveira Rodrigues R, Riccetto CL, Oliveira PG. Improving Organ Salvage in Testicular Torsion: Comparative Study of Patients Undergoing vs Not Undergoing Preoperative Manual Detorsion. J Urol. 2017;197:811–7. doi: 10.1016/j.juro.2016.09.087. [DOI] [PubMed] [Google Scholar]
- 5.Arda IS, Ozyaylali I. Testicular tissue bleeding as an indicator of gonadal salvageability in testicular torsion surgery. BJU Int. 2001;87:89–92. doi: 10.1046/j.1464-410x.2001.00021.x. [DOI] [PubMed] [Google Scholar]
- 6.Kutikov A, Casale P, White MA, Meyer WA, Chang A, Gosalbez R, et al. Testicular compartment syndrome: a new approach to conceptualizing and managing testicular torsion. Urology. 2008;72:786–9. doi: 10.1016/j.urology.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Figueroa V, Pippi Salle JL, Braga LH, Romao R, Koyle MA, Bagli DJ, et al. Comparative analysis of detorsion alone versus detorsion and tunica albuginea decompression (fasciotomy) with tunica vaginalis flap coverage in the surgical management of prolonged testicular ischemia. J Urol. 2012;188:1417–22. doi: 10.1016/j.juro.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 8.Silber JH, Rosenbaum PR, Trudeau ME, Even-Shoshan O, Chen W, Zhang X, et al. Multivariate matching and bias reduction in the surgical outcomes study. Med Care. 2001;39:1048–64. doi: 10.1097/00005650-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Rubin DB. The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med. 2007;26:20–36. doi: 10.1002/sim.2739. [DOI] [PubMed] [Google Scholar]
- 10.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferreira U, Netto NR, Junior, Esteves SC, Rivero MA, Schirren C. Comparative study of the fertility potential of men with only one testis. Scand J Urol Nephrol. 1991;25:255–9. doi: 10.3109/00365599109024555. [DOI] [PubMed] [Google Scholar]
- 12.Romeo C, Impellizzeri P, Arrigo T, Antonuccio P, Valenzise M, Mirabelli S, et al. Late hormonal function after testicular torsion. J Pediatr Surg. 2010;45:411–3. doi: 10.1016/j.jpedsurg.2009.10.086. [DOI] [PubMed] [Google Scholar]
- 13.Arap MA, Vicentini FC, Cocuzza M, Hallak J, Athayde K, Lucon AM, et al. Late hormonal levels, semen parameters, and presence of antisperm antibodies in patients treated for testicular torsion. J Androl. 2007;28:528–32. doi: 10.2164/jandrol.106.002097. [DOI] [PubMed] [Google Scholar]
- 14.Patel RP, Kolon TF, Huff DS, Carr MC, Zderic SA, Canning DA, et al. Testicular microlithiasis and antisperm antibodies following testicular biopsy in boys with cryptorchidism. J Urol. 2005;174:2008–10. doi: 10.1097/01.ju.0000176480.93985.37. discussion 10. [DOI] [PubMed] [Google Scholar]
- 15.Tryfonas G, Violaki A, Tsikopoulos G, Avtzoglou P, Zioutis J, Limas C, et al. Late postoperative results in males treated for testicular torsion during childhood. J Pediatr Surg. 1994;29:553–6. doi: 10.1016/0022-3468(94)90090-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.