Abstract
Since the early 1800s vaccines have saved numerous lives by preventing lethal infections. However, during the past two decades, there has been growing awareness of possible adverse events associated with vaccinations, cultivating heated debates and leading to significant fluctuations in vaccination rates. It is therefore pertinent for the scientific community to seriously address public concern of adverse effects of vaccines to regain public trust in these important medical interventions. Such adverse reactions to vaccines may be viewed as a result of the interaction between susceptibility of the vaccinated subject and various vaccine components. Among the implicated mechanisms for these reactions is molecular mimicry. Molecular mimicry refers to a significant similarity between certain pathogenic elements contained in the vaccine and specific human proteins. This similarity may lead to immune crossreactivity, wherein the reaction of the immune system towards the pathogenic antigens may harm the similar human proteins, essentially causing autoimmune disease. In this review, we address the concept of molecular mimicry and its application in explaining post vaccination autoimmune phenomena. We further review the principal examples of the influenza, hepatitis B, and human papilloma virus vaccines, all suspected to induce autoimmunity via molecular mimicry. Finally, we refer to possible implications on the potential future development of better, safer vaccines.
Introduction (a brief history of molecular mimicry)
In 1962, Melvin Kaplan released his revolutionary article describing a case of an 11-year-old boy who died of heart failure due to rheumatic fever. Pathology revealed immunoglobulin deposits in the cardiac muscle of the patient, leading Kaplan to explore the role of these antibodies. He examined the reaction of sera from rabbits immunized with group A streptococcal cells to samples of human heart tissue, conjuring the first established description of what is today a well-accepted paradigm—that structural similarity between bacteria and human protein may lead to the development of cardiac injury in rheumatic fever.1
In another canonical article published that same year, Rowley and Jenkin2 described a novel theory, concerning a possible immune crossreaction between infectious agents and host antigens, causing the development of autoimmunity.
These two articles may be viewed as harbingers to a mass of scientific publications that followed, all exploring the concept of immune crossreactivity due to structural homology between pathogens and self-proteins, a concept commonly termed molecular mimicry.3,4,5,6
Molecular mimicry is a term originally referring to the ability of an organism to evade detection by its predator through assuming features of a non-edible object,7 yet the concept was expanded to address the significant homology between microbial agents and the human host. Interestingly, the theoretical consequences of such similarities may vary depending on the interpreter. Thus, almost simultaneous with the publication by Rowley and Jenkin,2 a fundamentally opposite view of molecular mimicry was presented by Damian.8 Damian addressed naturally occurring parasitic antigenic determinants that were found to elicit little or no immune reaction. He attributed this feature to the similarity of these determinants to host proteins, suggesting that molecular mimicry may facilitate immune tolerance rather than immune autoreactivity.
Nevertheless, these two seemingly rivaling hypotheses may actually coexist, explaining the ostensibly paradoxical induction of autoimmunity in the unique setting created by vaccination.
During the past two decades, the similarity of viral and bacterial proteins to the human proteome was extensively researched. Noteworthy are the papers of Kanduc9 and Kanduc and colleagues10 who described a massive overlap of the different proteomes, ranging up to 90% of viral pentapeptides, as well as an astonishing 99.7% of bacterial heptapeptides, which were shared by the human proteome. Kanduc11 suggested that this massive overlap supports the notion that microbial elements bearing similarity to human proteins would likely not elicit an immune response, owing to tolerogenic mechanisms inherent to our immune system. However, in the setting of impaired tolerogenicity, exposure to those similar elements may induce autoimmunity.
The importance of tolerogenic mechanisms in preventing autoimmunity has been widely explored. A prominent illustration is the process of stimulation and clonal expansion of lymphocytes upon exposure to antigens: both T cells and B cells exposed to foreign antigens depend on a second signal to generate an effective immune response. It is believed that the goal of this duplicity is to minimize immune reactiveness against self-antigens.12
A crucial question is therefore, what factors are involved in attenuating immune tolerance?
The answer, as may be expected, is comprised of two chief pillars: environmental and genetic.
With regards to the role of genetics in predisposing individuals to autoimmunity, the body of evidence is constantly expanding. One central example is the association between certain major histocompatibility complex (MHC) alleles and autoimmune diseases.13,14 The mechanisms behind this association are poorly understood as yet. However, it was suggested that aberrant presentation of antigens via MHC class II to autoreactive T cells may lead to breakdown of immune tolerance.15 In fact, it is hypothesized that this genetic susceptibility to autoimmunity represents a natural evolutionary toll, as it may have provided a survival advantage for those with an overactive immune system, which would be more effective in fighting infections.16,17
The second pillar in attenuation of immune response is environmental effects. The role of environmental factors in the pathogenesis of autoimmunity has supplied grounds to a vast body of research, with data accumulating on the contribution of various elements such as nutrition, sun exposure, exercise, smoking and gut microbiota.18,19,20,21 Nonetheless, attention is rarely drawn to a significant environmental factor applied regularly with the sole purpose of impairing immune tolerance—Adjuvants.
The term adjuvant refers to a variety of compounds used to stimulate immune response. In fact, research of immune responses is dependent on these compounds since inducing a significant ‘researchable’ immune response to pathogenic elements is possible almost solely when injecting these element along with an adjuvant.12
Kanduc11 suggested the need for adjuvants stems from the inherent tolerance of the human immune system to many pathogenic motifs, which are repeatedly shared with the human proteome. Therefore, she offered that upon exposure of the immune system to these shared motifs, while impairing immune tolerance (by adding an adjuvant), a reasonable outcome may be the development of crossreactivity and autoimmunity.11
This application of the molecular mimicry theory may serve to explain potential development of autoimmune phenomena post vaccination (as illustrated in Figure 1).
Figure 1.
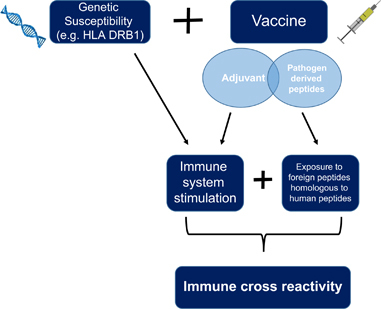
Schematic illustration of the process leading to the development of immune crossreactivity in genetically prone individuals upon exposure to vaccines.
Herein, we present principle examples of vaccines associated with autoimmunity, in which molecular mimicry has been implicated as a plausible mechanism.
Influenza (H1N1) vaccines: what pandemics may teach us
Since its initial isolation in the 1930s, the influenza A virus has justly been an important target for vaccine designers. Responsible for the Spanish flu in 1918, the H1N1 strain of the influenza virus took an estimated toll of 50–100 million deaths. No wonder then that as evidence began accumulating in mid-2009 of a new strain of A(H1N1) influenza virus rapidly spreading, health agencies worldwide alongside with vaccine manufacturing companies, enlisted to urgently develop suitable vaccinations.22 Several vaccines were marketed; however, the most prevalent vaccine, used across Europe as well as North America, was the AS03-adjuvanted A(H1N1) pandemic vaccine, with more the 30.5 million doses delivered.23 Such intense distribution of millions of doses over a rather short time frame allows the isolation of relatively rare potential adverse effects. And indeed, the 2009 influenza pandemic served as ground for extensive research of the influenza vaccine and its repercussions. Following the pandemic, a number of health concerns were raised regarding the vaccine, among those were a possible association with narcolepsy and Guillain-Barre syndrome.
Narcolepsy
Narcolepsy is a debilitating neurological disorder characterized by uncontrollable rapid eye movement attacks, which are not preceded by a non-rapid eye movement stage as occurs normally. The disease classically manifests as excessive daytime sleepiness, which may be accompanied by disrupted nocturnal sleep, sleep paralysis, hallucinations and obesity.24,25 Narcoleptic patients are believed to suffer from selective destruction of hypothalamic neurons, which are responsible for producing Orexin, also termed Hypocretin (HCRT), a neurotransmitter involved in regulating sleep-wake states.26 Although a specific autoantigen has not been isolated yet, narcolepsy is highly suspected to be an autoimmune disease, as it presents several key autoimmune characteristics. Among those are the extremely high association of narcolepsy with the HLA DQB1*06:02, and perhaps most compelling—the induction of narcoleptic characteristics in mice injected with antibodies from narcoleptic patients.24,25,27,28
Following the 2009 H1N1 pandemic, reports surfaced of an increase in narcolepsy diagnoses. Two rather distinct populations presented this rise in narcolepsy incidence: the first was the population of Beijing, presenting with a threefold increase in narcolepsy diagnosis in 2010,29 which returned to prepandemic rates by 2011.30 The second population was revealed in various studies of children and adolescents vaccinated with the European AS03-adjuvanted A(H1N1) pandemic vaccine, reporting a significantly increased incidence of narcolepsy among subjects receiving the vaccine.31,32,33,34,35,36,37
Remarkably, the only vaccine reported to significantly induce an increase in narcolepsy incidence was the European Pandemrix—a vaccine containing inactivated split-virion particles, and the AS03 adjuvant—composed of dl-α-tocopherol, squalene and polysorbate 80.23 This led to the suggestion that the AS03 adjuvant may be the sole culprit responsible for the induction of disease. In contrast, the Canadian Arepanrix vaccine did not generate similar phenomena despite containing the exact same adjuvant. Furthermore, the Chinese population presented with increased disease incidence, although vaccination rates were extremely limited,38 eluding to a role of the virus itself in the pathogenesis of the disease.
A recent publication presented a well-rounded hypothesis elucidating the relationship between virus and disease39—the authors reported of similarity between a peptide sequence of the surface-exposed influenza nucleoprotein A (NP A) and an extracellular domain of the HCRT receptor, which may serve as the basis to the development of crossreaction and autoimmunity. Moreover, antibodies derived from vaccine-associated narcolepsy patients were demonstrated to crossreact with both NP and HCRT receptor 2. Interestingly, the authors report significantly higher amounts of NP were found in the Pandemrix and Arepanrix vaccines, compared to the Focetria vaccine, which was not associated with narcolepsy. They suggest that the higher levels of NP enabled sufficient MHC-binding and subsequent immune response and crossreaction. With regards to the discrepancy between Pandemrix and Arepanrix, they refer to the world distribution of the HLA DQB1*06:02 allele, which is found in ~90% of narcolepsy patients, and is believe to represent a significant genetic component in disease pathogenesis. As the Arepanrix vaccine was administered mainly in Canada, where the allele is rare, they suggest this may explain the lower incidence of narcolepsy among the Canadian vaccinated population.40
Guillain-Barre syndrome
Guillain-Barre syndrome (GBS) is the most common form of acquired flaccid paralysis, believed to result from an autoimmune assault to the peripheral nervous system. Patients commonly present with antibodies for gangliosides, which are important components of peripheral nerve fibers.41,42 Various environmental triggers were suggested to be involved in the pathogenesis, among them most notorious is infection with Campylobacter jejuni, demonstrated to precede as many as 30% of all reported GBS cases.42 Studies have demonstrated molecular similarity between a component of C. jejuni and GM1, one of the targets of the autoantibodies found in patients, suggesting a role of molecular mimicry in the pathogenesis of the disease.43
Additional infectious potential triggers include Mycoplasma pneumonia, cytomegalovirus, as well as influenza virus.44 It is therefore of no surprise that various associations have been reported between influenza vaccines and GBS.
The most staggering report of the relationship between the influenza vaccine and GBS dates back to 1976—during the mass influenza immunization in the United States prompted by a swine flu outbreak, there was a significant increase in GBS incidence among the vaccinated population, estimated later to represent a 4–8-fold increased risk attributed to the vaccine.45 The vaccination program was suspended, and nearly 30 years later it was demonstrated that mice immunized with the vaccine developed anti-GM1 antibodies, thus supporting the hypothesis that molecular mimicry was the link between vaccine and disease.46
Naturally, these events led to extensive scrutiny of the influenza vaccines produced during the 2009 pandemic, in search of a rise in GBS reports. Data obtained of more than 70 million vaccinated subjects, from over 10 countries, were analyzed and revealed a 2–3-fold increased risk of GBS in the 42 days following recipient of the 2009 influenza vaccines.47 The authors pointed out that despite the undeniable added risk, these numbers confer to an excess of 1–3 GBS cases per one million persons vaccinated. Since this risk is much smaller than the estimated risk of GBS following influenza illness, they concurred that vaccination is justified. However, these findings accentuate the importance of meticulous appraisal of the safety profile of new influenza vaccines as they emerge.
Hepatitis B Virus vaccines: potential mimickers of myelin components
Hepatitis B virus (HBV) infection is a significant cause of morbidity and mortality, with an estimated 30% of world population showing evidence of past or current infection.48 Infection with HBV was linked to various extrahepatic manifestations, among those several were believed to be autoimmune.49 Thus, it stands to reason that concern was raised of possible autoimmune repercussions of the HBV vaccines. In fact, the first suggestion of autoimmune ramifications of a possible vaccine yet to be developed was published in Nature as early as 1975, as a ‘note of caution’ urging for a ‘careful assessment of all vaccine effects on the immune system’.50
Indeed, HBV vaccines have stirred rigorous debates among the scientific community regarding their potential role in the development of autoimmunity. Of special note is the relationship between HBV vaccines and various neurological symptoms, particularly symptoms representing a possible assault to myelin, such as acute disseminating encephalomyelitis, certain variants of GBS, transverse myelitis and multiple sclerosis (MS).
MS and other demyelinating neuropathies
The first report of neurologic adverse events following HBV vaccines was produced in a postmarketing surveillance issued by the Center for Disease Control (CDC) and the manufacturer.51 The authors could not detect a conclusive association between any neurologic adverse event and the vaccine. Nevertheless, they relate to their significant limitations in calculating a precise relative risk for the various events reported, due to variations in diagnostic classification of the cases, estimates of the size of the vaccinated population, background incidence of the diseases and the definition of a hypothetical at-risk interval. They further refer to their inability to assess underreporting of adverse effects. Following this publication, several interesting case reports were published regarding central nervous system demyelination arising after HBV immunization. One noteworthy such report published in the Lancet dates back to 1991, when Herroelen et al.52 described two patients developing central nervous system demyelination 6 weeks after receiving the vaccine. In a similar case report published 4 years later,53 the author points to an intriguing common denominator of all three reported patients—all possessed the HLA haplotypes DR2 and B7, which represent genetic susceptibility to develop MS.54,55 This observation corresponds to the concept of the mosaic of autoimmunity devised by Shoenfeld and Isenberg,56 Shoenfeld and co-workers57 and Shoenfeld et al.58 suggesting that the development of autoimmunity is a process resulting from a complex web of attenuating factors—genetic (such as certain HLA haplotypes) as well as environmental (such exposure to infections as well as vaccinations).56,57,58
These three reports were followed by many others,59,60,61,62 among them five cases reported in a comprehensive review of major adverse reactions to HBV vaccines,61 and two additional cases reported in which peripheral nerve biopsies demonstrated axonal degradation, suggesting an autoimmune reaction against axonal components.62
These case reports accentuate the need for large-scale studies designed to ascertain whether HBV vaccination entails a risk for autoimmune neurological adverse events.
In fact, a significant number of such studies were conducted, yet the debate remains—while several large-scale studies found no significant association between HBV vaccines and central nervous system demyelinating conditions,63,64,65,66,67,68 others show a significantly increased risk, with an odds ratio ranging from 3 to 5 for developing multiple sclerosis following HBV vaccines compared with other vaccines.69,70 Two adamant articles by Girard60, 71 offer a thought-provoking explanation for these contradicting findings. The author pointed to significant flaws raised regarding some of the pivotal, which demonstrated no association between vaccine and adverse events,72 and eludes to substantial publication bias favoring studies that support vaccine safety.60,71
Regardless of the ongoing debate on the large-scale autoimmune consequences of HBV vaccines, the vast number of case reports evoked research into possible mechanisms for vaccine-induced autoimmunity. One fundamental study in this aspect set out to examine similarities between the small HBV surface antigen (SHBsAg) contained in vaccines, to the MS autoantigens myelin basic protein (MBP) and myelin oligodendrocyte glycoprotein (MOG), which could serve as targets of immunological crossreactivity.73 The authors reported five peptides shared between the SHBsAg and MBP/MOG. They tested these peptides against serum samples from 58 adults before and after receiving the HBV vaccine to examine the potential development of crossreactive antibodies, comparing these samples to 87 samples of anti-SHBsAg antibody-negative patients as controls. SHBsAg/MOG double reactivity was reported on at least one occasion in 60% of the vaccinated subjects, compared with none before vaccination, and 2% of the controls (P-value was 0.001 for both). This initial finding may provide a general proof of concept for the theory of molecular mimicry leading to autoimmunity among HBV-vaccinated subjects.
Additional preliminary evidence was provided in a simple experiment examining sera from a young girl who developed transverse myelitis 2 months following a HBV vaccine booster injection. The girl presented with high titers of antinuclear antibodies, and was diagnosed with neuro-lupus. Sera from this patient was mixed with various concentrations of HBV vaccine. ANA were completely absorbed at the highest level of HBV vaccine, partially absorbed at intermediate dosage and were not absorbed in the lowest concentration,74 suggesting that these typical lupus antibodies may crossreact with components of the HBV vaccine. This finding is of special interest as it potentially links HBV vaccine, crossreactive antinuclear antibodies and autoimmune myelitis, a possibility that should of course be assessed though larger controlled studies.
Finally, a comprehensive review of the evidence regarding significant molecular mimicry between HBV polymerase and MBP offers an additional possible culprit contained in various HBV vaccines, which may be responsible for the induction of immune crossreaction in susceptible individuals.75
The evidence supporting the possibility of molecular mimicry, along with the epidemiologic data suggesting a link between HBV vaccines and autoimmune phenomena, all imply to the need for further exploration of the potential relationship between the vaccines and autoimmunity. Considering the current body of knowledge regarding the pathogenesis of immune crossreactivity, it seems reasonable to assume that the risk for autoimmunity is mainly relevant for those with susceptibility for autoimmune diseases (such as individuals with a family history of autoimmunity, subjects known to have autoantibodies and those carrying a certain genetic profile).76 These populations may benefit from a personalized risk assessment before vaccination. However, research regarding the involvement of the HBV vaccines in the induction of autoimmunity should not diminish the importance of these vaccines for their role in worldwide prevention of a life-threatening infection.
Human papilloma virus vaccines: a veil of concern remains unsettled
Human papilloma viruses (HPV) are notorious for their ability to infect human epithelial cells, leading, upon persistent infection, to the development of carcinoma at the site of infection.77 There are currently three available vaccines against HPV, aimed to prevent infection and thus the development of malignancies. While considered effective in preventing infection,78,79,80 the vaccines raised fervent debates across the scientific community with regards to their safety profile, and specifically their suspected association with the development of autoimmune phenomena.81,82 Whereas some studies present no association between HPV vaccines and autoimmune adverse events,83,84,85,86 others have addressed the significant limitations of many of these analyses.87,88 The answer remains largely disputed, yet the attention drawn to HPV may be responsible for some intriguing discoveries regarding potential molecular mimicry between HPV and human proteins. In two comprehensive analyses Kanduc et al.9,89 exposes vast peptide overlap between peptides of HPV to the human proteome,90 thus laying the grounds for further research regarding HPV and autoimmunity. As with influenza and HBV, the potential for immune crossreactivity upon infection led to concern of a similar effect, which may be induced by vaccination with viral particles. Following are two central examples of diseases suspected to be associated with the vaccine, where molecular mimicry is a suggested mechanism.
Systemic lupus erythematosus
The association between systemic lupus erythematosus (SLE) and HPV infection has been widely demonstrated in several studies.91,92 This connection led to the conjecture that the relationship may be one of cause and effect. In two recent publications, Segal et al.93,94 raised the hypothesis that HPV may be an environmental trigger eliciting the development of SLE among genetically susceptible individuals. To assess the possible role of molecular mimicry in the relationship between virus and disease, viral peptides were examined for homology to human proteins involved in the pathogenesis of SLE. Significant overlap was found between viral and various potentially SLE-relevant peptides. Most noteworthy is the homology between certain HPV peptides and human peptides belonging to compliment components as well as natural killer cell receptors—both known to be dysregulated in SLE. Notably, the viral peptides examined are all present in the three available vaccines, suggesting that crossreactivity may follow HPV vaccination as well as infection.
While some of the aforementioned studies report no significant association between SLE and HPV vaccines, several case reports have been published describing disease onset following vaccination.95,96,97 Although case reports describing temporal association do not provide proof of causation, these reports are complemented by more recent publications relating to large-scale data.98,99 Of note, a case–control analysis of reports submitted to the US Vaccine adverse event reporting system compared 48 816 reports of SLE to 21 998 controls (reporting adverse events other than SLE). Subjects with SLE were significantly more likely to have received the HPV quadrivalent vaccine (odds ratio 7.626, 95% confidence interval: 3.385–19.366), with a median onset of symptoms ranging between 3 and 37 days post vaccination.99
Postural orthostatic tachycardia syndrome
Postural orthostatic tachycardia syndrome (POTS) is a heterogeneous disorder of the autonomic nervous system characterized by an inappropriately significant increase in heart rate upon changing from supine to upright position (defined as 30 b.p.m. within 10 min of standing or head-up tilt), accompanied by decreased blood flow to the brain, and leading to orthostatic intolerance.100 While the exact etiology of the disease is still largely unknown, findings suggest a significant subset of patients suffer from small fiber neuropathy leading to autonomic dysfunction.101,102 In this aspect the disease resembles fibromyalgia and complex regional pain syndrome, two distinct clinical conditions that some claim may represent a single spectrum alongside Postural orthostatic tachycardia syndrome.103,104 Although no specific autoantigen was discovered yet, several clues denote POTS may be a result of an autoimmune process.102,105,106
The first report of the development of POTS after HPV vaccination was published in 2010.107 It was followed by dozens of similar case reports of POTS following HPV vaccination, all within 2 months of receiving the vaccine.108,109,110,111,112,113,114 Among these were two case series, compiling a total of 88 women, all presenting no more than 2 months following vaccination, complaining of orthostatic intolerance, with additional complaints such as nausea, palpitations, fatigue and neuropathic pain. Out of the two series, a total of 49 (55%) fulfilled the diagnostic criteria for POTS.110,112 These reports provided grounds for a more thorough, large-scale investigation of the possible association between HPV vaccines and POTS. However, as mentioned, research regarding potential adverse effects of the HPV vaccines is contradicting and disputed.
Among the noted limitations of previous large-scale studies was the complexity of diagnosing POTS, which commonly presents with several months of nonspecific symptoms such as dizziness and fatigue,107,109 and thus may not appear within the evaluated time frame or adverse event definitions of many studies.
Two noteworthy endeavors to overcome this limitation suggest that the occurrence of POTS post HPV vaccination may be higher than previously suspected. Both studies searched large-scale adverse event reporting systems for reports of various symptoms characteristic of POTS (such as syncope, dizziness, headaches, nausea, fatigue and palpitations), in an attempt to create a more accurate estimation of POTS incidence following HPV vaccine. The first, an analysis of reports from US Vaccine adverse event reporting system, demonstrated increased incidence of such reports following HPV vaccines compared with reports following Varivex.105 The second, a novel implementation of cluster analysis, conducted on an international database for adverse drug reactions, showed HPV vaccines to be associated with a significantly increased proportion of reports clinically consistent with the POTS, compared with other vaccines.115
These two publications stress the potential added value of appreciating POTS in the context of similar entities with substantial clinical overlap, such as chronic fatigue syndrome and fibromyalgia. However, while these findings suggest a possible association, which may have been missed due to limitations in adverse event definitions, they cannot substitute necessary future cohort studies.
Scant research is available regarding the potential mechanisms involved in vaccine-induced POTS; however, several thought-provoking publications may delineate a process of molecular mimicry as a possible explanation—an analysis of sera from 14 POTS patients demonstrated the presence of adrenergic receptor autoantibodies exerting agonistic effects, serving as a possible mechanism for the characteristic excessive tachycardia of POTS.116 The authors hypothesize that the antibodies may be induced by molecular mimicry, as similar findings were demonstrated in rats immunized with cardiac myosin, thus developing anti myosin antibodies which cross reacted with adrenergic receptors.117 The potential missing link to HPV is presented by Dahan et al.,105 who proposes an immune crossreaction in HPV-related POTS, ignited by specific HPV peptides, Shown to mimic human proteins potentially associated with arrhythmias, such as cardiac myosin.118
Discussion
The relationship between humans and potentially pathogenic microorganisms is no doubt intricate and complex, with new layers still unraveling. Such is our constantly evolving understanding of potential ramifications to the vast homology between viral and bacterial elements and the human proteome. While this affinity may exert protective effects, promoting immune tolerance (as attributed to the role of helminths in immunomodulation119), it may also serve to facilitate pathologic autoimmune processes. Molecular mimicry is a prototype of such processes, wherein an immune reaction directed against foreign pathogenic elements, bearing similarity to human proteins, may evolve into an autoimmune process targeting the homologous self-proteins.
Vaccines, perhaps the single most important contribution of modern medicine, serve as an essential and effective means of defense, protecting us of infectious diseases as well as potential induction of autoimmunity due to infection induced crossreactivity.
It seems somewhat ironic then that vaccines may induce the very same immune crossreactivity they serve to prevent. However, when considering the fact that vaccines inevitably contain infectious particles, it is rather expected.
In this review, we have addressed principle examples of vaccine-nduced molecular mimicry and autoimmunity (summarized in Table 1). Most of presented examples are subject to significant debate among the medical community, and unfortunately high-quality scientific data regarding these adverse events is lacking more often than not. Suspected associations are commonly deduced based on accumulating case reports and large-scale analyses of adverse event databases (such as US Vaccine adverse event reporting system). These are hardly sufficient to determine with certainty the nature of suggested correlations; however we believe such findings, viewed by some as a threat to the invaluable practice of vaccination, should instead serve as vital red flags, alerting for the need for constant investigation.
Table 1.
Examples of vaccines associated with immunological crossreaction and the suspected molecular elements implicated
| Vaccine | Autoimmune disease | Suspected viral element implicated | Suspected homologous human target | References |
|---|---|---|---|---|
| H1N1 | Narcolepsy | NP | HCRT receptor | 39 |
| GBS | HA | GM1 | 46 | |
| HBV | MS | SHBsAg | MOG | 73 |
| HBV polymerase | MBP | 75 | ||
| HPV | SLE | HPV L1 peptides | NK receptorsComplement components | 93, 94 |
| POTS | HPV L1 peptides | Cardiac myosin/adrenergic receptors | 105, 116, 118 |
Abbreviations: GBS, Guillain-Barre syndrome; GM1, ganglioside M1; HA, hemagglutinin; HBV, hepatitis B virus; HCRT, hypocretin; H1N1, strain of the influenza virus; HPV, human papilloma virus; MBP myelin binding protein; MOG, myelin oligodendrocyte glycoprotein; MS, multiple sclerosis; NK, natural killer cells; NP, influenza nucleoprotein; POTS, postural orthostatic tachycardia syndrome; SHBsAg, small hepatitis B surface antigen; SLE, systemic lupus erythematosus.
As history teaches us, vaccines, instrumental as they are in modern medicine, are subject to possible flaws in the same manner that all man-made developments are. Such were the cellular pertussis vaccine and the Rotashield vaccine—both products which were discontinued due to a high incidence of associated adverse events. Both were replaced by improved versions, leading to a significant decrease in reported side effects.
Indeed, the quest for safer vaccines in terms of immune crossreactivity is not a new one. As early as 1995, a seminal publication in Cell referred to the fact that ‘genetic modifications of viral vaccines that eliminate proven mimicry epitopes could make viral vaccines safer’.120 Nearly two decades later, Kanduc and Shoenfeld121 outlined a potential design for such vaccines, based on massive peptidome analyses and the isolation of sequences which are unique to pathogens, thus not bearing the potential for inducing immune crossreaction.
These suggestions represent a relatively recent and important trend, towards developing more accurate vaccines, which will potentially cause less adverse events, while still granting sufficient immunity. As with any important medical intervention, our duty as physicians is to eagerly advocate for vaccinations while still keeping a vigilant eye for potential risk, constantly striving to improve current medical practice and to minimize harm.
Conflict of interest
Prof. Yehuda Shoenfeld has served as an expert witness in cases involving adverse vaccine reaction in the no-fault US National Vaccine Injury Compensation Program.
References
- 1.Kaplan M, Meyeserian M. An immunological cross-reaction between group—a streptococcal cells and human heart tissue. Lancet. 1962;279:706–710. doi: 10.1016/s0140-6736(62)91653-7. [DOI] [PubMed] [Google Scholar]
- 2.Rowley D, Jenkin CR. Antigenic cross-reaction between host and parasite as a possible cause of pathogenicity. Nature. 1962;193:151–154. doi: 10.1038/193151a0. [DOI] [PubMed] [Google Scholar]
- 3.Oldstone MB. Molecular mimicry and immune-mediated diseases. FASEB J. 1998;12:1255–1265. doi: 10.1096/fasebj.12.13.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanduc D, Stufano A, Lucchese G, Kusalik A. Massive peptide sharing between viral and human proteomes. Peptides. 2008;29:1755–1766. doi: 10.1016/j.peptides.2008.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanduc D. The self/nonself issue. Self Nonself. 2010;1:255–258. doi: 10.4161/self.1.3.11897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agmon-Levin N, Blank M, Paz Z, Shoenfeld Y. Molecular mimicry in systemic lupus erythematosus. Lupus. 2009;18:1181–1185. doi: 10.1177/0961203309346653. [DOI] [PubMed] [Google Scholar]
- 7.Carpenter GDH. Mimicry, as viewed by Professor Shull. Science. 1937;85:356–359. doi: 10.1126/science.85.2206.356. [DOI] [PubMed] [Google Scholar]
- 8.Damian RT. Molecular mimicry: antigen sharing by parasite and host and its consequences. Am Nat. 1964;98:129–149. [Google Scholar]
- 9.Kanduc D. Quantifying the possible cross-reactivity risk of an HPV16 vaccine. ResearchGate. 2009;8:65–76. [PubMed] [Google Scholar]
- 10.Trost B, Lucchese G, Stufano A, Bickis M, Kusalik A, Kanduc D. No human protein is exempt from bacterial motifs, not even one. Self Nonself. 2010;1:328–334. doi: 10.4161/self.1.4.13315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanduc D. Peptide cross-reactivity: theoriginal sin of vaccines. Front Biosci School Ed. 2012;4:1393–1401. doi: 10.2741/s341. [DOI] [PubMed] [Google Scholar]
- 12.Janeway CA. Approaching the asymptote? Evolution and revolution in immunology. Cold Spring Harb Symp Quant Biol. 1989;54((Part 1)):1–13. doi: 10.1101/sqb.1989.054.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Arango M-T, Perricone C, Kivity S, Cipriano E, Ceccarelli F, Valesini G et al. HLA-DRB1 the notorious gene in the mosaic of autoimmunity. Immunol Res 2016, 1–17. [DOI] [PubMed]
- 14.Sønderstrup G, McDevitt HO. DR, DQ, and you: MHC alleles and autoimmunity. J Clin Invest. 2001;107:795–796. doi: 10.1172/JCI12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernando MMA, Stevens CR, Walsh EC, De Jager PL, Goyette P, Plenge RM et al. Defining the role of the MHC in autoimmunity: a review and pooled analysis. PLoS Genet [Internet] 2008; 4: e1000024. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2291482/. [DOI] [PMC free article] [PubMed]
- 16.Matzaraki V, Kumar V, Wijmenga C, Zhernakova A. The MHC locus and genetic susceptibility to autoimmune and infectious diseases. Genome Biol. 2017;18:76. doi: 10.1186/s13059-017-1207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taneja V, Mangalem A, David CS. Genetic predisposition to autoimmune diseases conferred by the major histocompatibility complex: utility of animal models. In: Mackay IR, Rose NR (eds). The Autoimmune Diseases. Academic Press: New York, NY, 2013; pp 365–377.
- 18.Dahan S, Segal Y, Shoenfeld Y. Dietary factors in rheumatic autoimmune diseases: a recipe for therapy? Nat Rev Rheumatol. 2017;13:348–358. doi: 10.1038/nrrheum.2017.42. [DOI] [PubMed] [Google Scholar]
- 19.Perricone C, Versini M, Ben-Ami D, Gertel S, Watad A, Segel MJ, et al. Smoke and autoimmunity: The fire behind the disease. Autoimmun Rev. 2016;15:354–374. doi: 10.1016/j.autrev.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Shoenfeld N, Amital H, Shoenfeld Y. The effect of melanism and vitamin D synthesis on the incidence of autoimmune disease. Nat Clin Pract Rheumatol. 2009;5:99–105. doi: 10.1038/ncprheum0989. [DOI] [PubMed] [Google Scholar]
- 21.Brusca SB, Abramson SB, Scher JU. Microbiome and mucosal inflammation as extra-articular triggers for rheumatoid arthritis and autoimmunity. Curr Opin Rheumatol. 2014;26:101–107. doi: 10.1097/BOR.0000000000000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neumann G, Noda T, Kawaoka Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature. 2009;459:931–939. doi: 10.1038/nature08157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed SS, Schur PH, MacDonald NE, Steinman L. Narcolepsy, 2009A(H1N1) pandemic influenza, and pandemic influenza vaccinations: what is known and unknown about the neurological disorder, the role for autoimmunity, and vaccine adjuvants. J Autoimmun. 2014;50:1–11. doi: 10.1016/j.jaut.2014.01.033. [DOI] [PubMed] [Google Scholar]
- 24.Arango M-T, Kivity S, Shoenfeld Y. Is narcolepsy a classical autoimmune disease? Pharmacol Res. 2015;92:6–12. doi: 10.1016/j.phrs.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Partinen M, Kornum BR, Plazzi G, Jennum P, Julkunen I, Vaarala O. Narcolepsy as an autoimmune disease: the role of H1N1 infection and vaccination. Lancet Neurol. 2014;13:600–613. doi: 10.1016/S1474-4422(14)70075-4. [DOI] [PubMed] [Google Scholar]
- 26.Sakurai T, Mieda M, Tsujino N. The orexin system: roles in sleep/wake regulation. Ann NY Acad Sci. 2010;1200:149–161. doi: 10.1111/j.1749-6632.2010.05513.x. [DOI] [PubMed] [Google Scholar]
- 27.Katzav A, Arango MT, Kivity S, Tanaka S, Givaty G, Agmon-Levin N, et al. Passive transfer of narcolepsy: anti-TRIB2 autoantibody positive patient IgG causes hypothalamic orexin neuron loss and sleep attacks in mice. J Autoimmun. 2013;45:24–30. doi: 10.1016/j.jaut.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 28.Singh AK, Mahlios J, Mignot E. Genetic association, seasonal infections and autoimmune basis of narcolepsy. J Autoimmun. 2013;43:26–31. doi: 10.1016/j.jaut.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Han F, Lin L, Warby SC, Faraco J, Li J, Dong SX, et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Ann Neurol. 2011;70:410–417. doi: 10.1002/ana.22587. [DOI] [PubMed] [Google Scholar]
- 30.Picchioni D, Hope CR, Harsh JR. A case–control study of the environmental risk factors for narcolepsy. Neuroepidemiology. 2007;29:185–192. doi: 10.1159/000111581. [DOI] [PubMed] [Google Scholar]
- 31.Stowe J, Andrews N, Kosky C, Dennis G, Eriksson S, Hall A, et al. Risk of narcolepsy after AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine in adults: a case-coverage study in England. Sleep. 2016;39:1051–1057. doi: 10.5665/sleep.5752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lakemedelsverket M. Occurrence of narcolepsy with cata-plexy among children and adolescents in relation to the H1N1 pandemic and Pandemrix vaccinations: results of a case inventory study by the MPA in Sweden during 2009–2010. 2011; 1: 1–20.
- 33.Heier MS, Gautvik KM, Wannag E, Bronder KH, Midtlyng E, Kamaleri Y, et al. Incidence of narcolepsy in Norwegian children and adolescents after vaccination against H1N1 influenza A. Sleep Med. 2013;14:867–871. doi: 10.1016/j.sleep.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 34.Dauvilliers Y, Arnulf I, Lecendreux M, Monaca Charley C, Franco P, Drouot X, et al. Increased risk of narcolepsy in children and adults after pandemic H1N1 vaccination in France. Brain. 2013;136:2486–2496. doi: 10.1093/brain/awt187. [DOI] [PubMed] [Google Scholar]
- 35.Department of Health (DoH). Investigation of an increase in the incidence of narcolepsy in children and adolescents in 2009 and 2010 Final Report of National Narcolepsy Study Steering Committee [Internet]. 2012 Apr (cited 13 August 2017). Available at: http://www.lenus.ie/hse/handle/10147/219671.
- 36.Nohynek H, Jokinen J, Partinen M, Vaarala O, Kirjavainen T, Sundman J, et al. AS03 adjuvanted AH1N1 vaccine associated with an abrupt increase in the incidence of childhood narcolepsy in Finland. PLoS ONE. 2012;7:e33536. doi: 10.1371/journal.pone.0033536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller E, Andrews N, Stellitano L, Stowe J, Winstone AM, Shneerson J, et al. Risk of narcolepsy in children and young people receiving AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine: retrospective analysis. BMJ. 2013;346:f794. doi: 10.1136/bmj.f794. [DOI] [PubMed] [Google Scholar]
- 38.Wang X, Yang P, Seale H, Zhang Y, Deng Y, Pang X, et al. Estimates of the true number of cases of pandemic (H1N1) 2009, Beijing, China. Emerg Infect Dis. 2010;16:1786–1788. doi: 10.3201/eid1611.100323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmed SS, Volkmuth W, Duca J, Corti L, Pallaoro M, Pezzicoli A, et al. Antibodies to influenza nucleoprotein cross-react with human hypocretin receptor 2. Sci Transl Med. 2015;7:294ra105. doi: 10.1126/scitranslmed.aab2354. [DOI] [PubMed] [Google Scholar]
- 40.Ahmed SS, Steinman L. Mechanistic insights into influenza vaccine-associated narcolepsy. Hum Vaccines Immunother. 2016;12:3196–3201. doi: 10.1080/21645515.2016.1171439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shoenfeld Y, George J, Peter JB. Guillain-Barré as an autoimmune disease. Int Arch Allergy Immunol. 1996;109:318–326. doi: 10.1159/000237258. [DOI] [PubMed] [Google Scholar]
- 42.Yuki N, Hartung H-P. Guillain-Barré syndrome. N Engl J Med. 2012;366:2294–2304. doi: 10.1056/NEJMra1114525. [DOI] [PubMed] [Google Scholar]
- 43.Yuki N, Taki T, Inagaki F, Kasama T, Takahashi M, Saito K, et al. A bacterium lipopolysaccharide that elicits Guillain-Barré syndrome has a GM1 ganglioside-like structure. J Exp Med. 1993;178:1771–1775. doi: 10.1084/jem.178.5.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wakerley BR, Yuki N. Infectious and noninfectious triggers in Guillain-Barré syndrome. Expert Rev Clin Immunol. 2013;9:627–639. doi: 10.1586/1744666X.2013.811119. [DOI] [PubMed] [Google Scholar]
- 45.Schonberger LB, Bregman DJ, Sullivan-Bolyai JZ, Keenlyside RA, Ziegler DW, Retailliau HF, et al. Guillain-Barre syndrome following vaccination in the National Influenza Immunization Program, United States, 1976–1977. Am J Epidemiol. 1979;110:105–123. doi: 10.1093/oxfordjournals.aje.a112795. [DOI] [PubMed] [Google Scholar]
- 46.Nachamkin I, Shadomy SV, Moran AP, Cox N, Fitzgerald C, Ung H, et al. Anti-ganglioside antibody induction by swine (A/NJ/1976/H1N1) and other influenza vaccines: insights into vaccine-associated Guillain-Barré syndrome. J Infect Dis. 2008;198:226–233. doi: 10.1086/589624. [DOI] [PubMed] [Google Scholar]
- 47.Salmon DA, Vellozzi C, Chen RT, Halsey NA. Did the influenza A (H1N1) 2009 monovalent inactivated vaccines increase the risk for Guillain-Barré syndrome? Expert Rev Clin Immunol. 2013;9:795–797. doi: 10.1586/1744666X.2013.824686. [DOI] [PubMed] [Google Scholar]
- 48.Trépo C, Chan HLY, Lok A. Hepatitis B virus infection. Lancet Lond Engl. 2014;384:2053–2063. doi: 10.1016/S0140-6736(14)60220-8. [DOI] [PubMed] [Google Scholar]
- 49.Maya R, Gershwin ME, Shoenfeld Y. Hepatitis B virus (HBV) and autoimmune disease. Clin Rev Allergy Immunol. 2008;34:85–102. doi: 10.1007/s12016-007-8013-6. [DOI] [PubMed] [Google Scholar]
- 50.Zuckerman AJ. Hepatitis vaccine: a note of caution. Nature. 1975;255:104–105. [Google Scholar]
- 51.Shaw FE, Graham DJ, Guess HA, Milstien JB, Johnson JM, Schatz GC, et al. Postmarketing surveillance for neurologic adverse events reported after hepatitis B vaccination. Experience of the first three years. Am J Epidemiol. 1988;127:337–352. doi: 10.1093/oxfordjournals.aje.a114808. [DOI] [PubMed] [Google Scholar]
- 52.Herroelen L, de Keyser J, Ebinger G. Central-nervous-system demyelination after immunisation with recombinant hepatitis B vaccine. Lancet Lond Engl. 1991;338:1174–1175. doi: 10.1016/0140-6736(91)92034-y. [DOI] [PubMed] [Google Scholar]
- 53.Kaplanski G, Retornaz F, Durand J, Soubeyrand J. Central nervous system demyelination after vaccination against hepatitis B and HLA haplotype. J Neurol Neurosurg Psychiatry. 1995;58:758–759. doi: 10.1136/jnnp.58.6.758-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gyódi E, Benczur M, Pálffy G, Tálas M, Petrányi G, Földes I, et al. Association between HLA B7, DR2 and dysfunction of natural- and antibody-mediated cytotoxicity without connection with the deficient interferon production in multiple sclerosis. Hum Immunol. 1982;4:209–217. doi: 10.1016/0198-8859(82)90036-2. [DOI] [PubMed] [Google Scholar]
- 55.Dyment DA, Ebers GC, Sadovnick AD. Genetics of multiple sclerosis. Lancet Neurol. 2004;3:104–110. doi: 10.1016/s1474-4422(03)00663-x. [DOI] [PubMed] [Google Scholar]
- 56.Shoenfeld Y, Isenberg DA. The mosaic of autoimmunity. Immunol Today. 1989;10:123–126. doi: 10.1016/0167-5699(89)90245-4. [DOI] [PubMed] [Google Scholar]
- 57.Perricone C, Agmon-Levin N, Shoenfeld Y. Novel pebbles in the mosaic of autoimmunity. BMC Med. 2013;11:101. doi: 10.1186/1741-7015-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shoenfeld Y, Gilburd B, Abu-Shakra M, Amital H, Barzilai O, Berkun Y, et al. The mosaic of autoimmunity: genetic factors involved in autoimmune diseases—2008. Isr Med Assoc J. 2008;10:3–7. [PubMed] [Google Scholar]
- 59.Gout O. Vaccinations and multiple sclerosis. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2001;22:151–154. [PubMed] [Google Scholar]
- 60.Girard M. Autoimmune hazards of hepatitis B vaccine. Autoimmun Rev. 2005;4:96–100. doi: 10.1016/j.autrev.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 61.Grotto I, Mandel Y, Ephros M, Ashkenazi I, Shemer J. Major adverse reactions to yeast-derived hepatitis B vaccines—a review. Vaccine. 1998;16:329–334. doi: 10.1016/s0264-410x(97)00214-4. [DOI] [PubMed] [Google Scholar]
- 62.Vital C, Vital A, Gbikpi-Benissan G, Longy-Boursier M, Climas M-T, Castaing Y, et al. Postvaccinal inflammatory neuropathy: peripheral nerve biopsy in 3 cases. J Peripher Nerv Syst. 2002;7:163–167. doi: 10.1046/j.1529-8027.2002.02010.x. [DOI] [PubMed] [Google Scholar]
- 63.Belloni C, Avanzini MA, De Silvestri A, Martinetti M, Pasi A, Coslovich E, et al. No evidence of autoimmunity in 6-year-old children immunized at birth with recombinant hepatitis B vaccine. Pediatrics. 2002;110((Part 1)):e4. doi: 10.1542/peds.110.1.e4. [DOI] [PubMed] [Google Scholar]
- 64.Monteyne P, André FE. Is there a causal link between hepatitis B vaccination and multiple sclerosis? Vaccine. 2000;18:1994–2001. doi: 10.1016/s0264-410x(99)00533-2. [DOI] [PubMed] [Google Scholar]
- 65.Langer-Gould A, Qian L, Tartof SY, Brara SM, Jacobsen SJ, Beaber BE, et al. Vaccines and the risk of multiple sclerosis and other central nervous system demyelinating diseases. JAMA Neurol. 2014;71:1506–1513. doi: 10.1001/jamaneurol.2014.2633. [DOI] [PubMed] [Google Scholar]
- 66.Demicheli V, Rivetti A, Pietrantonj CD, Clements CJ, Jefferson T. Hepatitis B vaccination and multiple sclerosis: evidence from a systematic review. J Viral Hepat. 2003;10:343–344. doi: 10.1046/j.1365-2893.2003.00423.x. [DOI] [PubMed] [Google Scholar]
- 67.DeStefano F, Verstraeten T, Jackson LA, Okoro CA, Benson P, Black SB, et al. Vaccinations and risk of central nervous system demyelinating diseases in adults. Arch Neurol. 2003;60:504–509. doi: 10.1001/archneur.60.4.504. [DOI] [PubMed] [Google Scholar]
- 68.Ascherio A, Zhang SM, Hernán MA, Olek MJ, Coplan PM, Brodovicz K, et al. Hepatitis B vaccination and the risk of multiple sclerosis. N Engl J Med. 2001;344:327–332. doi: 10.1056/NEJM200102013440502. [DOI] [PubMed] [Google Scholar]
- 69.Geier DA, Geier MR. A case–control study of serious autoimmune adverse events following hepatitis B immunization. Autoimmunity. 2005;38:295–301. doi: 10.1080/08916930500144484. [DOI] [PubMed] [Google Scholar]
- 70.Hernán MA, Jick SS, Olek MJ, Jick H. Recombinant hepatitis B vaccine and the risk of multiple sclerosis: a prospective study. Neurology. 2004;63:838–842. doi: 10.1212/01.wnl.0000138433.61870.82. [DOI] [PubMed] [Google Scholar]
- 71.Girard M. When evidence-based medicine (EBM) fuels confusion: multiple sclerosis after hepatitis B vaccine as a case in point. Med Veritas. 2007;4:1436–1451. [Google Scholar]
- 72.Bégaud B, Alpérovitch A. Vaccinations and multiple sclerosis. N Engl J Med. 2001;344:1793–1796. [PubMed] [Google Scholar]
- 73.Bogdanos D-P, Smith H, Ma Y, Baum H, Mieli-Vergani G, Vergani D. A study of molecular mimicry and immunological cross-reactivity between hepatitis B surface antigen and myelin mimics. Clin Dev Immunol. 2005;12:217–224. doi: 10.1080/17402520500285247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Poirriez J. A preliminary experiment of absorption of antinuclear antibodies by the hepatitis B vaccine components, in a case of neurolupus. Vaccine. 2004;22:3166–3168. doi: 10.1016/j.vaccine.2004.01.056. [DOI] [PubMed] [Google Scholar]
- 75.Faure E. Multiple sclerosis and hepatitis B vaccination: could minute contamination of the vaccine by partial hepatitis B virus polymerase play a role through molecular mimicry? Med Hypotheses. 2005;65:509–520. doi: 10.1016/j.mehy.2005.02.044. [DOI] [PubMed] [Google Scholar]
- 76.Soriano A, Nesher G, Shoenfeld Y. Predicting post-vaccination autoimmunity: who might be at risk? Pharmacol Res. 2015;92:18–22. doi: 10.1016/j.phrs.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 77.Tommasino M. The human papillomavirus family and its role in carcinogenesis. Semin Cancer Biol. 2014;26:13–21. doi: 10.1016/j.semcancer.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 78.Iversen O-E, Miranda MJ, Ulied A, Soerdal T, Lazarus E, Chokephaibulkit K, et al. Immunogenicity of the 9-valent HPV vaccine using 2-dose regimens in girls and boys vs a 3-dose regimen in women. JAMA. 2016;316:2411–2421. doi: 10.1001/jama.2016.17615. [DOI] [PubMed] [Google Scholar]
- 79.Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow S-N, Apter D, et al. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet Lond Engl. 2009;374:301–314. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- 80.Garland SM, Hernandez-Avila M, Wheeler CM, Perez G, Harper DM, Leodolter S, et al. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356:1928–1943. doi: 10.1056/NEJMoa061760. [DOI] [PubMed] [Google Scholar]
- 81.Pellegrino P, Carnovale C, Pozzi M, Antoniazzi S, Perrone V, Salvati D, et al. On the relationship between human papilloma virus vaccine and autoimmune diseases. Autoimmun Rev. 2014;13:736–741. doi: 10.1016/j.autrev.2014.01.054. [DOI] [PubMed] [Google Scholar]
- 82.Baker B, Eça Guimarães L, Tomljenovic L, Agmon-Levin N, Shoenfeld Y. The safety of human papilloma virus-blockers and the risk of triggering autoimmune diseases. Expert Opin Drug Saf. 2015;14:1387–1394. doi: 10.1517/14740338.2015.1073710. [DOI] [PubMed] [Google Scholar]
- 83.Slade BA, Leidel L, Vellozzi C, Woo EJ, Hua W, Sutherland A, et al. Postlicensure safety surveillance for quadrivalent human papillomavirus recombinant vaccine. JAMA. 2009;302:750–757. doi: 10.1001/jama.2009.1201. [DOI] [PubMed] [Google Scholar]
- 84.Cramon C, Poulsen CL, Hartling UB, Holden IK, Johansen IS. Possible adverse effects of the quadrivalent human papillomavirus vaccine in the Region of Southern Denmark: a retrospective, descriptive cohort study. Dan Med J 2017; 64. [PubMed]
- 85.Klein NP, Hansen J, Chao C, Velicer C, Emery M, Slezak J, et al. Safety of quadrivalent human papillomavirus vaccine administered routinely to females. Arch Pediatr Adolesc Med. 2012;166:1140–1148. doi: 10.1001/archpediatrics.2012.1451. [DOI] [PubMed] [Google Scholar]
- 86.Grönlund O, Herweijer E, Sundström K, Arnheim-Dahlström L. Incidence of new-onset autoimmune disease in girls and women with pre-existing autoimmune disease after quadrivalent human papillomavirus vaccination: a cohort study. J Intern Med. 2016;280:618–626. doi: 10.1111/joim.12535. [DOI] [PubMed] [Google Scholar]
- 87.Jefferson T, Jørgensen L. Human papillomavirus vaccines, complex regional pain syndrome, postural orthostatic tachycardia syndrome, and autonomic dysfunction—a review of the regulatory evidence from the European Medicines Agency. Indian J Med Ethics. 2017;2:30–37. doi: 10.20529/IJME.2017.006. [DOI] [PubMed] [Google Scholar]
- 88.Dahan S, Shoenfeld Y. Letter to the editor—HPV vaccine and autoimmunity Incidence of new-onset autoimmune disease in girls and women with pre-existing autoimmune disease after quadrivalent human papillomavirus vaccination: a cohort study. J Intern Med. 2017;281:313–315. doi: 10.1111/joim.12575. [DOI] [PubMed] [Google Scholar]
- 89.Kanduc D. Penta- and hexapeptide sharing between HPV16 and Homo sapiens proteomes. Int J Med Med Sci. 2009;1:383–387. [Google Scholar]
- 90.Natale C, Giannini T, Lucchese A, Kanduc D. Computer-assisted analysis of molecular mimicry between human papillomavirus 16 E7 oncoprotein and human protein sequences. Immunol Cell Biol. 2000;78:580–585. doi: 10.1046/j.1440-1711.2000.00949.x. [DOI] [PubMed] [Google Scholar]
- 91.Klumb EM, Pinto AC, Jesus GR, Araujo M, Jascone L, Gayer CR, et al. Are women with lupus at higher risk of HPV infection? Lupus. 2010;19:1485–1491. doi: 10.1177/0961203310372952. [DOI] [PubMed] [Google Scholar]
- 92.Lyrio LDC, Grassi MFR, Santana IU, Olavarria VG, Gomes A, do N, CostaPinto L, et al. Prevalence of cervical human papillomavirus infection in women with systemic lupus erythematosus. Rheumatol Int. 2013;33:335–340. doi: 10.1007/s00296-012-2426-0. [DOI] [PubMed] [Google Scholar]
- 93.Segal Y, Dahan S, Calabrò M, Kanduc D, Shoenfeld Y. HPV and systemic lupus erythematosus: a mosaic of potential crossreactions. Immunol Res. 2017;65:564–571. doi: 10.1007/s12026-016-8890-y. [DOI] [PubMed] [Google Scholar]
- 94.Segal Y, Calabrò M, Kanduc D, Shoenfeld Y. Human papilloma virus and lupus: the virus, the vaccine and the disease. Curr Opin Rheumatol. 2017;29:331–342. doi: 10.1097/BOR.0000000000000398. [DOI] [PubMed] [Google Scholar]
- 95.Gatto M, Agmon-Levin N, Soriano A, Manna R, Maoz-Segal R, Kivity S, et al. Human papillomavirus vaccine and systemic lupus erythematosus. Clin Rheumatol. 2013;32:1301–1307. doi: 10.1007/s10067-013-2266-7. [DOI] [PubMed] [Google Scholar]
- 96.Soldevilla HF, Briones SFR, Navarra SV. Systemic lupus erythematosus following HPV immunization or infection? Lupus. 2012;21:158–161. doi: 10.1177/0961203311429556. [DOI] [PubMed] [Google Scholar]
- 97.Ito H, Noda K, Hirai K, Ukichi T, Furuya K, Kurosaka D. A case of systemic lupus erythematosus (SLE) following human papillomavirus (HPV) vaccination. Nihon Rinsho Meneki Gakkai Kaishi. 2016;39:145–149. doi: 10.2177/jsci.39.145. [DOI] [PubMed] [Google Scholar]
- 98.Wang B, Shao X, Wang D, Xu D, Zhang J-A. Vaccinations and risk of systemic lupus erythematosus and rheumatoid arthritis: a systematic review and meta-analysis. Autoimmun Rev. 2017;16:756–765. doi: 10.1016/j.autrev.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 99.Geier DA, Geier MR. Quadrivalent human papillomavirus vaccine and autoimmune adverse events: a case–control assessment of the vaccine adverse event reporting system (VAERS) database. Immunol Res. 2016;65:46–54. doi: 10.1007/s12026-016-8815-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Grubb BP, Kanjwal Y, Kosinski DJ. The postural tachycardia syndrome: a concise guide to diagnosis and management. J Cardiovasc Electrophysiol. 2006;17:108–112. doi: 10.1111/j.1540-8167.2005.00318.x. [DOI] [PubMed] [Google Scholar]
- 101.Haensch C-A, Tosch M, Katona I, Weis J, Isenmann S. Small-fiber neuropathy with cardiac denervation in postural tachycardia syndrome. Muscle Nerve. 2014;50:956–961. doi: 10.1002/mus.24245. [DOI] [PubMed] [Google Scholar]
- 102.Low PA, Sandroni P, Joyner M, Shen W-K. Postural Tachycardia Syndrome (POTS) J Cardiovasc Electrophysiol. 2009;20:352–358. doi: 10.1111/j.1540-8167.2008.01407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Martínez-Lavín M. Hypothesis: human papillomavirus vaccination syndrome—small fiber neuropathy and dysautonomia could be its underlying pathogenesis. Clin Rheumatol. 2015;34:1165–1169. doi: 10.1007/s10067-015-2969-z. [DOI] [PubMed] [Google Scholar]
- 104.Üçeyler N. Small fiber pathology—a culprit for many painful disorders? Pain. 2016;157((Suppl 1)):S60–S66. doi: 10.1097/j.pain.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 105.Dahan S, Tomljenovic L, Shoenfeld Y. Postural orthostatic tachycardia syndrome (POTS)—a novel member of the autoimmune family. Lupus. 2016;25:339–342. doi: 10.1177/0961203316629558. [DOI] [PubMed] [Google Scholar]
- 106.Wang X-L, Chai Q, Charlesworth MC, Figueroa JJ, Low P, Shen W-K, et al. Autoimmunoreactive IgGs from patients with postural orthostatic tachycardia syndrome. Proteomics Clin Appl. 2012;6:615–625. doi: 10.1002/prca.201200049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Blitshteyn S. Postural tachycardia syndrome after vaccination with Gardasil. Eur J Neurol. 2010;17:e52. doi: 10.1111/j.1468-1331.2010.03021.x. [DOI] [PubMed] [Google Scholar]
- 108.Blitshteyn S. Postural tachycardia syndrome following human papillomavirus vaccination. Eur J Neurol. 2014;21:135–139. doi: 10.1111/ene.12272. [DOI] [PubMed] [Google Scholar]
- 109.Tomljenovic L, Colafrancesco S, Perricone C, Shoenfeld Y. Postural orthostatic tachycardia with chronic fatigue after HPV vaccination as part of the ‘autoimmune/auto-inflammatory syndrome induced by adjuvants’: case report and literature review. J Investig Med High Impact Case Rep. 2014;2:1–8. doi: 10.1177/2324709614527812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Brinth LS, Pors K, Theibel AC, Mehlsen J. Orthostatic intolerance and postural tachycardia syndrome as suspected adverse effects of vaccination against human papilloma virus. Vaccine. 2015;33:2602–2605. doi: 10.1016/j.vaccine.2015.03.098. [DOI] [PubMed] [Google Scholar]
- 111.Hendrickson JE, Tormey CA. Human papilloma virus vaccination and dysautonomia: considerations for autoantibody evaluation and HLA typing. Vaccine. 2016;34:4468. doi: 10.1016/j.vaccine.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 112.Brinth L, Theibel AC, Pors K, Mehlsen J. Suspected side effects to the quadrivalent human papilloma vaccine. Dan Med J. 2015;62:A5064. [PubMed] [Google Scholar]
- 113.Palmieri B, Poddighe D, Vadalà M, Laurino C, Carnovale C, Clementi E. Severe somatoform and dysautonomic syndromes after HPV vaccination: case series and review of literature. Immunol Res. 2017;65:106–116. doi: 10.1007/s12026-016-8820-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kafaie J, Kim M, Krause E. Small fiber neuropathy following vaccination. J Clin Neuromuscul Dis. 2016;18:37–40. doi: 10.1097/CND.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 115.Chandler RE, Juhlin K, Fransson J, Caster O, Edwards IR, Norén GN. Current safety concerns with human papillomavirus vaccine: a cluster analysis of reports in VigiBase®. Drug Saf. 2017;40:81–90. doi: 10.1007/s40264-016-0456-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Li H, Yu X, Liles C, Khan M, Vanderlinde-Wood M, Galloway A, et al. Autoimmune basis for postural tachycardia syndrome. J Am Heart Assoc. 2014;3:e000755. doi: 10.1161/JAHA.113.000755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Li Y, Heuser JS, Cunningham LC, Kosanke SD, Cunningham MW. Mimicry and antibody-mediated cell signaling in autoimmune myocarditis. J Immunol. 2006;177:8234–8240. doi: 10.4049/jimmunol.177.11.8234. [DOI] [PubMed] [Google Scholar]
- 118.Kanduc D. Potential cross-reactivity between HPV16 L1 protein and sudden death-associated antigens. J Exp Ther Oncol. 2011;9:159–165. [PubMed] [Google Scholar]
- 119.Versini M, Jeandel P-Y, Bashi T, Bizzaro G, Blank M, Shoenfeld Y. Unraveling the hygiene hypothesis of helminthes and autoimmunity: origins, pathophysiology, and clinical applications. BMC Med. 2015;13:81. doi: 10.1186/s12916-015-0306-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wucherpfennig KW, Strominger JL. Molecular mimicry in T cell-mediated autoimmunity: viral peptides activate human T cell clones specific for myelin basic protein. Cell. 1995;80:695–705. doi: 10.1016/0092-8674(95)90348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kanduc D, Shoenfeld Y. From HBV to HPV: designing vaccines for extensive and intensive vaccination campaigns worldwide. Autoimmun Rev. 2016;15:1054–1061. doi: 10.1016/j.autrev.2016.07.030. [DOI] [PubMed] [Google Scholar]


