Abstract
The prevalence of fatty liver disease (FLD) is increasing. To clarify risk factors for developing FLD, we analyzed a database from healthy Japanese adults who had annual medical check-ups in 2004 and reexamined in 2009. We used the fatty liver index (FLI) to classify participants as FLD (FLI ≥60), borderline FLD (30≤ FLI <60), and normal liver (FLI <30). Subjects with hepatitis B or C virus infection and subjects with FLD at the baseline were excluded. The cumulative incidence of FLD from normal liver and from borderline FLD over five years were 0.65% (52/8,025) and 12.9% (244/1,888), respectively. After multiple adjustments, higher serum uric acid (SUA) (OR:1.92; 95% CI:1.40–2.63) and increased SUA change (OR:3.734; 95% CI:2.57–5.42) became risk factors for developing FLD from normal liver, as well as younger age and higher body mass index. The risk factors for developing FLD from borderline FLD were similar. Not only higher baseline SUA but also increased SUA change became independent risks for developing FLD.
Introduction
Fatty liver disease (FLD) is emerging now as the number one cause of chronic liver disease especially in developed countries1. Patients with FLD have been found to have increased morbidity and mortality compared to non-FLD patients. Of note, patients with FLD have a 2–6 fold risk of fatal and nonfatal CVD2–5, a 2–3 fold risk of developing diabetes6, and an overall increased mortality of 57%7. FLD will soon eclipse Hepatitis C as the number one indication for liver transplant8.
Early identification of those at risk for FLD is necessary in aiding timely discussions about the disease, screening, and prevention especially through life style modifications. Traditional risk factors such as central obesity, insulin resistance, western diet (high fructose, high fat, high salt), sedentary lifestyle, and genetics are well established as having roles in the development and progression of FLD9. Yet despite the recent expansion into our understanding of FLD, the pathological development of FLD has not been fully explained10. Besides traditional risk factors such as weight and diabetes, it is well known that serum uric acid (SUA) has also been found to associate with FLD11. Many studies have shown that SUA is a risk factor for developing FLD12–14. However, it is unclear how SUA change over time affects the risk for developing FLD. This study checked our hypothesis that not only a higher SUA at baseline, but also increase in SUA over time are risk factors for developing FLD.
Results
Demographics of this study subjects
Table 1 shows the demographics with normal liver and borderline FLD at the baseline (in 2004). Compared to men with normal liver group, borderline FLD group are older, higher male gender, higher body mass index (BMI), higher rate of smoking and drinking habits, and have a higher prevalence of hypertension, diabetes mellitus, dyslipidemia, and chronic kidney disease, along with higher liver enzyme levels, and higher SUA levels.
Table 1.
Demographics of study subjects.
| Number of subjects | Total | Normal liver | Borderline fatty liver | p |
|---|---|---|---|---|
| 9,914 | 8,025 | 1,889 | ||
| Age | 48.7 ± 10.6 | 48.1 ± 10.6 | 51.0 ± 10.4 | <0.001 |
| Male gender | 41.6% | 32.4% | 80.6% | <0.001 |
| Height (cm) | 163.0 ± 8.4 | 161.9 ± 8.1 | 167.7 ± 8.0 | <0.001 |
| Weight (kg) | 58.0 ± 10.2 | 55.3 ± 8.7 | 69.5 ± 7.9 | <0.001 |
| Body mass index (kg/m2) | 21.7 ± 2.6 | 21.0 ± 2.3 | 24.7 ± 2.0 | <0.001 |
| Waist circumference (cm) | 79.0 ± 7.9 | 77.0 ± 7.0 | 87.7 ± 5.1 | <0.001 |
| Smoking habits | 34.4% | 29.6% | 54.9% | <0.001 |
| Drinking habits | 41.0% | 37.6% | 55.3% | <0.001 |
| Hypertension | 8.9% | 6.7% | 18.2% | <0.001 |
| Diabetes mellitus | 1.5% | 0.9% | 3.9% | <0.001 |
| Dyslipidemia | 30.5% | 22.7% | 63.9% | <0.001 |
| Chronic kidney disease | 2.0% | 1.8% | 3.1% | 0.002 |
| Fatty liver index | 16.0 ± 15.3 | 9.63 ± 7.7 | 43.2 ± 8.5 | <0.001 |
| Triglyceride (mg/dL) | 85.6 ± 47.4 | 72.6 ± 32.8 | 140.8 ± 59.1 | <0.001 |
| Total protein (g/dL) | 7.13 ± 0.36 | 7.12 ± 0.36 | 7.21 ± 0.35 | <0.001 |
| Total bilirubin (mg/dL) | 0.83 ± 0.30 | 0.82 ± 0.30 | 0.84 ± 0.29 | 0.054 |
| Aspartate aminotransferase (IU/L) | 21.5 ± 6.5 | 20.8 ± 6.1 | 24.5 ± 7.4 | <0.001 |
| Alanine transaminase (IU/L) | 19.1 ± 10.9 | 16.9 ± 8.0 | 28.3 ± 15.5 | <0.001 |
| Gamma-glutamyl transferase (IU/L) | 29.0 ± 26.5 | 22.9 ± 16.2 | 55.2 ± 41.6 | <0.001 |
| Alkaline phosphatase (IU/L) | 190 ± 57 | 186 ± 56 | 208 ± 56 | <0.001 |
| Serum uric acid (mg/dL) | 5.13 ± 1.33 | 4.87 ± 1.21 | 6.22 ± 1.24 | <0.001 |
| Serum uric acid change (mg/dL) | −0.025 ± 0.708 | 0.008 ± 0.670 | −0.164 ± 0.835 | <0.001 |
p, probability.
Data are presented as mean ± standard deviation.
Cumulative incidences of FLD from normal liver or from borderline FLD over five years
Cumulative incidence of FLD from normal liver or from borderline FLD over five years were 0.65% (52/8,025) and 12.9% (244/1,888), respectively.
Risk factors for developing FLD
We checked the risk factors for developing FLD from normal liver or from borderline FLD over 5 years, separately. First, we checked the risk factors for developing FLD from normal liver. In crude analysis, younger age, male gender, higher BMI, smoking habits, drinking habits, dyslipidemia, higher SUA levels, and increased SUA change over 5 years are risk factors for developing FLD from normal liver. After multiple adjustments for age, sex, BMI, smoking and drinking habits, dyslipidemia, SUA levels, and SUA change, the risk factors for developing FLD from normal liver are younger age (odds ratio (OR):0.94 per 1 year increased; 95% confidence interval (CI), 0.90–0.97), higher BMI (OR:1.75 per 1 kg/m2 increased; 95% CI, 1.55–2.00), higher SUA levels (OR:1.92 per 1 mg/dL increased; 95% CI, 1.40–2.63), and increased SUA change (OR: 3.73 per 1 mg/dL increased; 95% CI, 2.57–5.42) (Table 2).
Table 2.
Risk factors for developing fatty liver from normal liver function (FLI <30) over five years.
| Normal liver | Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | ||
| Age | per 1 year increased | 0.947 | 0.919–0.975 | <0.001 | 0.936 | 0.904–0.968 | <0.001 |
| Male gender | versus female gender | 3.360 | 1.918–5.886 | <0.001 | 0.592 | 0.249–1.405 | 0.23 |
| Body mass index | per 1 kg/m2 increased | 1.731 | 1.545–1.939 | <0.001 | 1.750 | 1.534–1.996 | <0.001 |
| Smoking | positive versus negative | 2.399 | 1.390–4.140 | 0.002 | 1.564 | 0.849–2.882 | 0.15 |
| Drinking habits | positive versus negative | 1.944 | 1.125–3.360 | 0.017 | 1.591 | 0.846–2.991 | 0.15 |
| Hypertension | positive versus negative | 1.497 | 0.593–3.780 | 0.39 | 0.913 | 0.327–2.549 | 0.86 |
| Diabetes mellitus | positive versus negative | — | — | — | — | — | — |
| Dyslipidemia | positive versus negative | 1.814 | 1.022–3.220 | 0.042 | 1.791 | 0.962–3.335 | 0.066 |
| Chronic kidney disease | positive versus negative | — | — | — | — | — | — |
| Serum uric acid | per 1 mg/dL increased | 1.766 | 1.448–2.155 | <0.001 | 1.920 | 1.400–2.634 | <0.001 |
| Serum uric acid change | per 1 mg/dL increased | 3.413 | 2.383–4.889 | <0.001 | 3.734 | 2.574–5.416 | <0.001 |
OR, odds ratio; CI, confidence interval; p, probability.
There is no subject with diabetes mellitus or chronic kidney disease at the baseline who developed fatty liver over 5 years.
*Data adjusted for age, sex, body mass index, smoking and drinking habits, hypertension, diabetes mellitus, dyslipidemia, chronic kidney disease, serum uric acid and serum uric acid change over 5 years.
Second, we checked the risk factors for developing FLD from borderline FLD. In crude analysis, younger age, higher BMI, and increased SUA change are risk factors for developing FLD from borderline FLD. After multiple adjustments for age and BMI, the risk factors for developing FLD from borderline FLD are younger age (OR:0.95 per 1 year increased; 95% CI, 0.94–0.97), higher BMI (OR:1.15 per 1 kg/m2 increased; 95% CI, 1.08–1.23), smoking (OR: 1.37; 95% CI, 1.01–1.87), higher SUA levels (OR: 1.17 per 1 mg/dL increased; 95% CI, 1.02–1.35), and increased SUA change (OR: 1.76 per 1 mg/dL increased; 95% CI, 1.47–2.11) (Table 3).
Table 3.
Risk factors for developing fatty liver from borderline fatty liver (30 < FLI < 60) over five years.
| Borderline fatty liver | Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | ||
| Age | per 1 year increased | 0.950 | 0.937–0.963 | <0.001 | 0.956 | 0.941–0.971 | <0.001 |
| Male gender | versus female gender | 0.984 | 0.702–1.381 | 0.93 | 0.656 | 0.420–1.025 | 0.064 |
| Body mass index | per 1 kg/m2 increased | 1.188 | 1.112–1.268 | <0.001 | 1.178 | 1.096–1.265 | <0.001 |
| Smoking | positive versus negative | 1.196 | 0.911–1.570 | 0.20 | 1.369 | 1.005–1.866 | 0.047 |
| Drinking habits | positive versus negative | 1.202 | 0.915–1.578 | 0.19 | 1.305 | 0.953–1.786 | 0.097 |
| Hypertension | positive versus negative | 0.981 | 0.691–1.391 | 0.98 | 1.152 | 0.791–1.677 | 0.46 |
| Diabetes mellitus | positive versus negative | 0.373 | 0.135–1.032 | 0.057 | 0.502 | 0.174–1.447 | 0.20 |
| Dyslipidemia | positive versus negative | 0.843 | 0.640–1.110 | 0.22 | 0.986 | 0.734–1.323 | 0.92 |
| Chronic kidney disease | positive versus negative | 0.480 | 0.172–1335 | 0.16 | 0.970 | 0.333–2.821 | 0.95 |
| Serum uric acid | per 1 mg/dL increased | 1.056 | 0.948–1.177 | 0.32 | 1.173 | 1.023–1.346 | 0.022 |
| Serum uric acid change | per 1 mg/dL increased | 1.658 | 1.398–1.965 | <0.001 | 1.762 | 1.468–2.114 | <0.001 |
OR, odds ratio; CI, confidence interval; p, probability.
There is no subject with diabetes mellitus or chronic kidney disease at the baseline who developed fatty liver over 5 years.
*Data adjusted for age, sex, body mass index, smoking and drinking habits, hypertension, diabetes mellitus, dyslipidemia, chronic kidney disease, serum uric acid and serum uric acid change over 5 years.
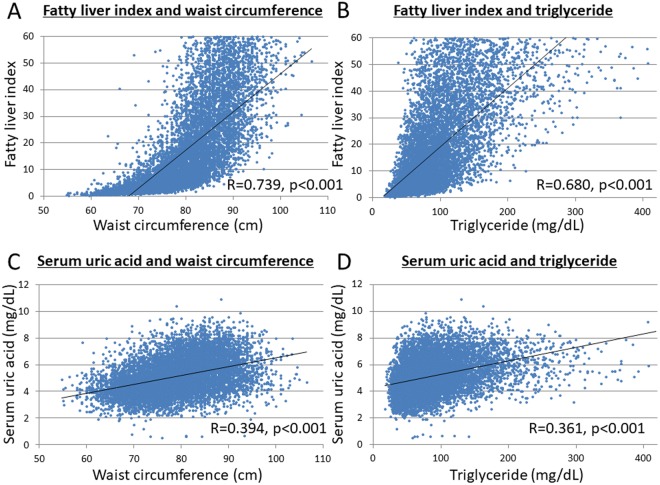
Correlation between SUA levels and fatty liver index (FLI)
We checked the correlation between SUA levels and FLI using all the study subjects’ data (9,914 subjects) in 2004. There is significantly positive correlation between SUA levels and FLI by Pearson’s correlation coefficient (R = 0.513, p < 0.001) (Fig. 1). However, FLI is also influenced by other components of the metabolic syndrome, like waist circumference and triglyceride. We conducted additional analyses of the correlation between FLI and waist circumference (Fig. 2A), between FLI and triglyceride (Fig. 2B), between SUA and waist circumference (Fig. 2C), and between SUA and TG (Fig. 2D). The results showed FLI was more correlated to abdominal circumference (R = 0.739, p < 0.001) or triglyceride (R = 0.680, p < 0.001) than SUA (R = 0.513, p < 0.001). However, the correlations between SUA and waist circumference (R = 0.394, p < 0.001) or between SUA and TG (R = 0.361, p < 0.001) were not as strong (R < 0.4).
Figure 1.
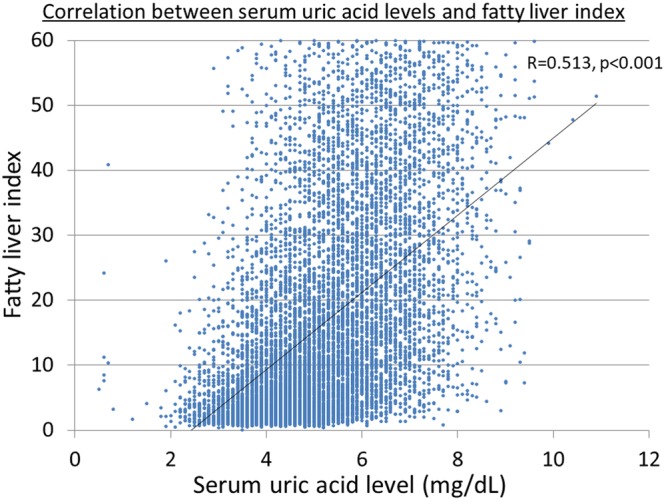
Correlation between serum uric acid levels and fatty liver index. There is significantly positive correlation between serum uric acid levels and fatty liver index by Pearson’s correlation coefficient (R = 0.513, p < 0.001).
Figure 2.
Correlation between fatty liver index, serum uric acid levels, waist circumference, and triglyceride. (A) Correlation between fatty liver index and waist circumference There is significantly positive correlation (R = 0.739, *p < 0.001). (B) Correlation between fatty liver index and triglyceride There is significantly positive correlation (R = 0.680, *p < 0.001). (C) Correlation between serum uric acid levels and waist circumference There is significantly positive correlation (R = 0.394, *p < 0.001). (D) Correlation between serum uric acid levels and triglyceride There is significantly positive correlation (R = 0.361, **p < 0.001). All the analyses were conducted by Pearson’s correlation coefficient (R = 0.513, p < 0.001).
Discussion
The primary goal of our study was to identify risk factors for developing FLD in a general healthy Japanese population. In the subjects both with normal liver and borderline FLD at the baseline, not only higher SUA levels but also increased SUA change over 5 years became independent risk factors for developing FLD over 5 years, as well as younger age and higher BMI. Moreover, increased SUA change was the highest OR for developing FLD after multiple adjustments. Our study also showed significantly positive correlation between baseline SUA levels and FLI.
The key finding in our study is that, not only does baseline SUA predict the development of FLD in a healthy population independent of several other traditional risk factors, but increased SUA change over 5 years also becomes a strong risk for developing FLD. There are many studies that clarified the association between SUA and FLD, but this is the first study that assessed SUA change over 5years as a risk factor for developing FLD. While several studies have found elevated SUA associated with presence or severity of FLD11,15–22, others have not including in an adolescent and adult female population23,24. Some have contended that SUA elevations seen in metabolic syndrome are a result of the pathology rather than a cause of the pathology25–28. Also, some contend that hyperinsulinemia decreases renal uric acid excretion and that uric acid is an innocent bystander26. Yet our findings are consistent with other longitudinal cohort studies that did find SUA levels were a predictor of FLD development in Korean and Chinese adult populations12–14. In addition, SUA is associated with more advanced FLD in adolescent and adult populations17,18,29, and elevated baseline SUA predicted cirrhosis related hospitalization or death even after adjustment for causes or risk factors of chronic liver disease in 5,518 patients during a 12.9 year median follow up15.
There is also data that supports a role in lower SUA levels leading to improvement in FLD. Animal FLD models have shown use of allopurinol or febuxostat improves markers of inflammation as well as in a human liver line (HepG2)30,31. In addition, a small study in humans found allopurinol improved levels of cytokeratin 18 (marker for hepatocyte apoptosis), AST, ALT, total cholesterol, and Triglycerides32. Finally, a longitudinal cohort found lower SUA levels at baseline predicted resolution of FLD33. A recent study by Cicero, A. F. G. et al. showed that SUA and FLI were also related to pulse wave velocity34. The study suggested that arterial stiffness might be associated with not only high SUA levels, but also FLD.
An interesting finding is that for patients with borderline FLD, SUA is smaller risk than the normal liver population. As noted in Table 1, borderline FLD patients are older, weigh more with greater waist circumference, and have more features of metabolic syndrome (dyslipidemia, higher blood pressure, and presence of diabetes) compared to the normal liver group. SUA has been strongly linked to playing a role in the development of metabolic syndrome35 and therefore it is possible that SUA leads to FLD through indirect mechanism such as insulin resistance than direct effects on liver pathology. As of note, our normal liver population had few features of metabolic syndrome, and even after adjustment for traditional risk factors, found SUA to strongly associate with the development of FLD. It has been shown that uric acid directly drives oxidative stress in HepG2 cells and this further activates endoplasmic reticulum (ER) stress along with activating genes involved in lipogenesis36,37. Another study found an association of SUA with lean FLD38. Thus, SUA level at baseline and increases in SUA highlight a population at risk for FLD particularly in a relative healthy appearing population compared to borderline FLD group. Evidence supports uric acid’s role in FLD, both via direct means on ER stress and lipogenesis as well as indirect means such as weight gain, and insulin resistance39, which drive free fatty acid shunting to the liver and de-novo lipogenesis40. Our study does not clarify, which mechanism could potentially be playing the more prominent role.
We found that a younger age at baseline predicted the development of FLD. Dietary habits in younger patients compared to older patients are likely more of a Western diet than traditional Japanese food41,42. In addition, it may be that older patients who already have FLD were excluded since they had FLI ≥ 60 and those (of the older patients) who had a FLI <60 are not as likely to develop FLD if they have factors (ie healthier diet) placing them at less risk for development of FLD. In addition, for both groups, BMI was found to be risk factor for development of FLD.
Our study has several limitations. First, this study is a retrospective single center study, which may have introduced selection bias. However, single center studies have some advantages of the similarity of methodology. Second, we did not exclude for elevated bilirubin and other liver enzymes at the baseline, which might suggest another liver disorder and could affect SUA levels as there is association between jaundice and hypouricemia43. However, this study population was done in a generally healthy population. Data from Table 1 shows average bilirubin and other liver enzymes were normal for this population. In our multivariable analysis, we used a category of dyslipidemia which included triglyceride. However, we did not include abdominal circumference because we included BMI. BMI is strongly correlated with abdominal circumference, and we used only BMI in the multiple adjustment models to exclude confounding bias. Third, the FLI is designed to identify those with low likelihood of FLD. Use of FLI is a limitation since it is an indirect measurement of FLD. It is possible some patients in the borderline FLD already had FLD and maybe possible that even some with healthy liver may have FLD while some with an FLI ≥ 60 do not, though, as stated before, a FLI < 30 strongly rules out likelihood of FLD disease, while an FLI ≥ 60 strongly indicates likely FLD. FLI has been validated in Asian populations (Korean cohort)44 and recent research has shown FLI to accurately predict steatosis when compared to MR Spectroscopy (MRS)45. Fourth, our study did not separate out alcoholic FLD (AFLD) from nonalcoholic FLD (NAFLD). We adjusted for drinking habits though, and found both baseline SUA and changes in SUA still to be risk factors for the development of FLD suggesting SUA plays a role in NAFLD, though it could likely play a role in AFLD as well. Of note, drinking habits was not associated with risk of FLD development. In addition, there is likely coexistence of AFLD and NAFLD in the population46. Finally, this is an observation study, and it cannot show the causal relationships between SUA and FLD. Intervention studies are needed to clarify whether the treatments for hyperuricemia in subjects with normal liver are useful to prevent the development of FLD.
In conclusion, not only higher baseline SUA, but also increased SUA change over 5 years become independent risks for developing FLD both from normal liver and borderline liver, as well as younger age and higher BMI. Therefore, in a relative healthy population we should pay attention to both baseline SUA and SUA change as risk factors for developing FLD. Further research and especially clinical trials are needed to evaluate whether SUA lowering can impede the development of FLD.
Methods
Study design
This is a retrospective, single-center, cohort study in Japan to clarify the risk factors for developing FLD. The database was from the Center for Preventive Medicine, St. Luke’s International Hospital, Tokyo, Japan. The study analyzed 13,201 Japanese subjects who underwent annual medical examinations at the center in 2004 and were reevaluated five years later. We used FLI to assess FLD47. This is a well established algorithm based upon BMI, waist circumference, triglycerides, and gamma-glutamyl-transferase (GGT) that is shown to have an accuracy of 84% with a cutoff value of <30 to rule out hepatic steatosis (sensitivity of 87% and a negative likelihood ratio of 0.2) and FLI ≥ 60 to rule in (Specificity 86%, positive likelihood ratio 4.3). We included the subjects between the ages 20 and 75 years old at the baseline (2004) given this was the age cutoffs in the validation study47. We excluded the subjects with hepatitis B (HBs antigen positive) and C (HCV antibody positive) virus infection and subjects with FLD (FLI ≥ 60) at the baseline. We also excluded the subjects on medication for hypertension, dyslipidemia, diabetes mellitus, and hyperuricemia and/or gout. When the subjects had more than one annual examination, we only used the first examination of that year to avoid counting the individual twice. Every subject had the same work-up, including medical history, routine physical examination, and blood tests collected in this database and detailed in previous publications48–51. We evaluated the cumulative incidence of FLD from normal liver (FLI < 30) and borderline FLD (30 ≤ FLI < 60) at baseline. Moreover, we evaluated risk factors for developing FLD both from normal liver and from borderline FLD over five years and calculated ORs. Finally we prefer to use the term FLD over NAFLD even though we adjusted for drinking habits given total intake was not assessed nor were other rare causes of FLD such as celiac or certain medications eliminated from analysis52.
Fatty liver index (FLI)
FLI is calculated by this formula47.
GGT, Gamma-glutamyl transferase
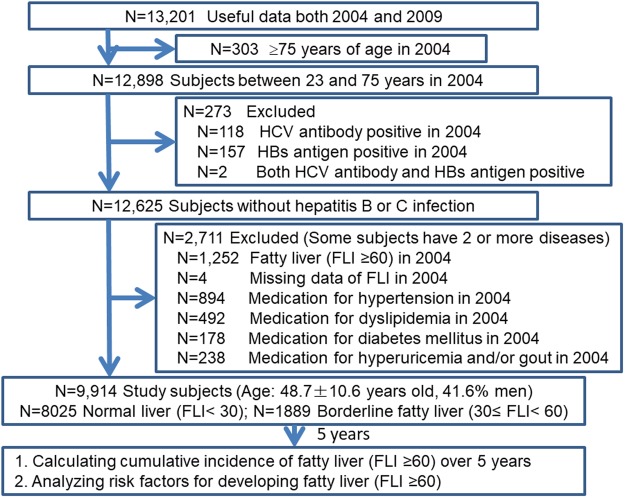
Study subjects
Out of the 13,201 subjects, no subject was less than 20 years old (23 years old is the youngest in this study) and 303 subjects were 75 years old and above in 2004. Of 12,898 subjects, 118 subjects were HCV positive and 157 subjects were HBs antigen positive (2 subjects had both). Of 12,625 subjects without hepatitis virus infection, we excluded 1,252subjects with FLD, 4 subjects with missing data of FLI, 894 subjects on medication for hypertension, 492 subjects on medication for dyslipidemia, 178 subjects on medication for diabetes mellitus, and 238 subjects on medication for hyperuricemia and/or gout. Finally, we analyzed 9,914 subjects (age: 48.7 ± 10.6 years old, 41.6% men) (Fig. 3).
Figure 3.
Flow diagram of study enrollment N: number of subjects; FLI, fatty liver index.
Patient involvement
No patients were involved in setting the research question or outcome measures, nor were they involved in the design and implementation of the study. There are no plans to involve patients in dissemination.
Definition of hypertension, diabetes mellitus, dyslipidemia, and chronic kidney disease
Hypertension is defined as a condition when subjects are on current antihypertensive medication and/or systolic blood pressure of greater than or equal to 140 mmHg and/or diastolic blood pressure of greater than or equal to 90 mmHg53,54 blood pressure readings were obtained using an automatic brachial sphygmomanometer (OMRON Corporation, Kyoto, Japan), which were upper arm blood pressure measurements that had passed validation. Two blood pressure examinations were taken after the participants were seated and rested quietly for more than five minutes with their feet on the ground and their back supported. The mean systolic and diastolic blood pressure of each of the subjects were calculated from the recorded measurements. Diabetes mellitus is defined as current diabetes mellitus on medication use and/or HbA1c (National Glycohemoglobin Standardization Program) greater than or equal to 6.5%, according to International Expert Committee55. Dyslipidemia is defined as current medication use for dyslipidemia and/or low-density lipoprotein cholesterol greater than or equal to 140 mg/dl, high-density lipoprotein cholesterol less than 40 mg/dL, and/or triglycerides greater than or equal to 150 mg/dL, according to Japan Atherosclerosis Society guidelines56. Chronic kidney disease is defined as estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m2. We calculated eGFR using the Japanese GFR equation: eGFR (mL/min/1.73 m2) = 194 × serum creatinine−1.094 × age−0.287 (×0.739 if woman)57. Smoking habits included past smoking and current smoking. Drinking habits were defined as drinking alcohol every day or not.
Statistical analysis
Statistically significance was set at a probability (p) value < 0.05 (two sided). Data are expressed as mean ± standard derivation or as percent frequency unless otherwise specified. Comparisons between two groups were performed with student t-tests for normally distributed variables, and χ2 analyses for categorical data. The risk factors for developing FLD from normal liver or borderline FLD in the period of over five years were evaluated both by non-adjusted (crude) models and by multivariable logistic regression models. We checked risk factors for developing FLD with age, sex, body mass index (BMI), smoking and drinking habits, hypertension, diabetes mellitus, dyslipidemia, chronic kidney disease, baseline SUA levels, and SUA change over 5 years (calculated by SUA in 2009 – SUA in 2004) by crude models and multivariable adjusted models, and odds ratios (ORs) were analyzed in each group. We also checked the correlation between SUA levels and FLI by Pearson’s correlation coefficient. All the statistical analyses were performed using the SPSS Statistics software (IBM SPSS Statistics version 22 for Windows; IBM, New York, USA).
Ethical considerations
We adhered to the principles of the Declaration of Helsinki. All data were collected and compiled in a protected computer database. Individual data were anonymous without identifiable personal information. Informed consent was obtained from all subjects by a comprehensive agreement method provided by St. Luke’s International Hospital. St. Luke’s International Hospital Ethics Committee approved the protocol for this study.
Acknowledgements
All the authors of this paper fulfill the criteria of authorship. The authors thank the patients and all staff in Center for Preventive Medicine, St. Luke’s International Hospital, for assistance with data collection. Dr. Kuwabara reports the grant for studying abroad from Federation of National Public Service Personnel Mutual Aid Association in Japan.
Author Contributions
T.J. and M.Kuwabara designed the study and wrote the manuscript. K.N. and M.Kuwabara provided research data. M.Kuwabara performed data analyses and data interpretation. T.J., K.N., I.H., M.Kanbay, M.O., M.A.L., R.J.J. and M.Kuwabara contributed to the discussion and supervised the study designed. All the authors reviewed and edited the manuscript. All authors have approved the final article.
Competing Interests
Dr. Johnson has equity with XORT Therapeutics that is developing novel xanthine oxidase inhibitors and with Colorado Research Partners LLC that is developing inhibitors of fructose metabolism. In addition, Dr. Johnson is an inventor on several patents licensed to XORT Therapeutics. (US Patent No 7,799,794, US Patent No. 8,557,831).
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ray K. NAFLD-the next global epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:621. doi: 10.1038/nrgastro.2013.197. [DOI] [PubMed] [Google Scholar]
- 2.Haring R, et al. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum gamma-glutamyl transpeptidase levels. Hepatology. 2009;50:1403–1411. doi: 10.1002/hep.23135. [DOI] [PubMed] [Google Scholar]
- 3.Jepsen P, et al. Prognosis of patients with a diagnosis of fatty liver–a registry-based cohort study. Hepatogastroenterology. 2003;50:2101–2104. [PubMed] [Google Scholar]
- 4.Targher G, et al. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabetes Care. 2007;30:2119–2121. doi: 10.2337/dc07-0349. [DOI] [PubMed] [Google Scholar]
- 5.Treeprasertsuk S, et al. The Framingham risk score and heart disease in nonalcoholic fatty liver disease. Liver Int. 2012;32:945–950. doi: 10.1111/j.1478-3231.2011.02753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekstedt M, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 7.Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43:617–649. doi: 10.3109/07853890.2010.518623. [DOI] [PubMed] [Google Scholar]
- 8.Pais R, et al. NAFLD and liver transplantation: Current burden and expected challenges. J Hepatol. 2016;65:1245–1257. doi: 10.1016/j.jhep.2016.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Younossi Z, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 10.Yu J, Marsh S, Hu J, Feng W, Wu C. The Pathogenesis of Nonalcoholic Fatty Liver Disease: Interplay between Diet, Gut Microbiota, and Genetic Background. Gastroenterol Res Pract. 2016;2016:2862173. doi: 10.1155/2016/2862173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou Y, Wei F, Fan Y. High serum uric acid and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. Clin Biochem. 2016;49:636–642. doi: 10.1016/j.clinbiochem.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Lee JW, et al. Serum uric Acid as a predictor for the development of nonalcoholic Fatty liver disease in apparently healthy subjects: a 5-year retrospective cohort study. Gut Liver. 2010;4:378–383. doi: 10.5009/gnl.2010.4.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryu S, Chang Y, Kim SG, Cho J, Guallar E. Serum uric acid levels predict incident nonalcoholic fatty liver disease in healthy Korean men. Metabolism. 2011;60:860–866. doi: 10.1016/j.metabol.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Xu C, Yu C, Xu L, Miao M, Li Y. High serum uric acid increases the risk for nonalcoholic Fatty liver disease: a prospective observational study. PLoS One. 2010;5:e11578. doi: 10.1371/journal.pone.0011578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afzali A, Weiss NS, Boyko EJ, Ioannou GN. Association between serum uric acid level and chronic liver disease in the United States. Hepatology. 2010;52:578–589. doi: 10.1002/hep.23717. [DOI] [PubMed] [Google Scholar]
- 16.Liu Z, Que S, Zhou L, Zheng S. Dose-response Relationship of Serum Uric Acid with Metabolic Syndrome and Non-alcoholic Fatty Liver Disease Incidence: A Meta-analysis of Prospective Studies. Sci Rep. 2015;5:14325. doi: 10.1038/srep14325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mosca A, et al. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. J Hepatol. 2017;66:1031–1036. doi: 10.1016/j.jhep.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 18.Sertoglu E, et al. The relationship of serum uric acid with non-alcoholic fatty liver disease. Clin Biochem. 2014;47:383–388. doi: 10.1016/j.clinbiochem.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 19.Kuo CF, et al. Gout and risk of non-alcoholic fatty liver disease. Scand J Rheumatol. 2010;39:466–471. doi: 10.3109/03009741003742797. [DOI] [PubMed] [Google Scholar]
- 20.Li Y, Xu C, Yu C, Xu L, Miao M. Association of serum uric acid level with non-alcoholic fatty liver disease: a cross-sectional study. J Hepatol. 2009;50:1029–1034. doi: 10.1016/j.jhep.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 21.Petta S, Camma C, Cabibi D, Di Marco V, Craxi A. Hyperuricemia is associated with histological liver damage in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2011;34:757–766. doi: 10.1111/j.1365-2036.2011.04788.x. [DOI] [PubMed] [Google Scholar]
- 22.Vos MB, et al. Correlation of vitamin E, uric acid, and diet composition with histologic features of pediatric NAFLD. J Pediatr Gastroenterol Nutr. 2012;54:90–96. doi: 10.1097/MPG.0b013e318229da1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cardoso AS, Gonzaga NC, Medeiros CC, Carvalho DF. Association of uric acid levels with components of metabolic syndrome and non-alcoholic fatty liver disease in overweight or obese children and adolescents. J Pediatr (Rio J) 2013;89:412–418. doi: 10.1016/j.jped.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Fan N, et al. Sex-Specific Association between Serum Uric Acid and Nonalcoholic Fatty Liver Disease in Type 2 Diabetic Patients. J Diabetes Res. 2016;2016:3805372. doi: 10.1155/2016/3805372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferrara LA, et al. Serum uric acid does not predict incident metabolic syndrome in a population with high prevalence of obesity. Nutr Metab Cardiovasc Dis. 2014;24:1360–1364. doi: 10.1016/j.numecd.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sluijs I, et al. A Mendelian Randomization Study of Circulating Uric Acid and Type 2 Diabetes. Diabetes. 2015;64:3028–3036. doi: 10.2337/db14-0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dai X, et al. Association between serum uric acid and the metabolic syndrome among a middle- and old-age Chinese population. Eur J Epidemiol. 2013;28:669–676. doi: 10.1007/s10654-013-9829-4. [DOI] [PubMed] [Google Scholar]
- 28.McKeigue PM, et al. Bayesian methods for instrumental variable analysis with genetic instruments (‘Mendelian randomization’): example with urate transporter SLC2A9 as an instrumental variable for effect of urate levels on metabolic syndrome. Int J Epidemiol. 2010;39:907–918. doi: 10.1093/ije/dyp397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jaruvongvanich V, Ahuja W, Wirunsawanya K, Wijarnpreecha K, Ungprasert P. Hyperuricemia is associated with nonalcoholic fatty liver disease activity score in patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017;29:1031–1035. doi: 10.1097/MEG.0000000000000931. [DOI] [PubMed] [Google Scholar]
- 30.Nakatsu Y, et al. The xanthine oxidase inhibitor febuxostat suppresses development of nonalcoholic steatohepatitis in a rodent model. Am J Physiol Gastrointest Liver Physiol. 2015;309:G42–51. doi: 10.1152/ajpgi.00443.2014. [DOI] [PubMed] [Google Scholar]
- 31.Wang W, et al. Quercetin and allopurinol reduce liver thioredoxin-interacting protein to alleviate inflammation and lipid accumulation in diabetic rats. Br J Pharmacol. 2013;169:1352–1371. doi: 10.1111/bph.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sylvia, S., Sedhom, O. A. B., Salwa, H. S. & Mohamad, A. Mokhles. Assessment of the therapeutic effect of allopurinol in patients with non-alcoholic fatty liver disease associated with hyperuricemia by cytokeratin 18. In 9th Euro Global Gastroenterology Conference (Valenica Spain, 2016).
- 33.Zhou Z, et al. Associations between Serum Uric Acid and the Remission of Non-Alcoholic Fatty Liver Disease in Chinese Males. PLoS One. 2016;11:e0166072. doi: 10.1371/journal.pone.0166072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cicero, A.F.G. et al. Fatty liver index is associated to pulse wave velocity in healthy subjects: Data from the Brisighella Heart Study. Eur J Intern Med (2018). [DOI] [PubMed]
- 35.Kanbay M, et al. Uric acid in metabolic syndrome: From an innocent bystander to a central player. Eur J Intern Med. 2016;29:3–8. doi: 10.1016/j.ejim.2015.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lanaspa MA, et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: potential role in fructose-dependent and -independent fatty liver. J Biol Chem. 2012;287:40732–40744. doi: 10.1074/jbc.M112.399899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choi YJ, et al. Uric acid induces fat accumulation via generation of endoplasmic reticulum stress and SREBP-1c activation in hepatocytes. Lab Invest. 2014;94:1114–1125. doi: 10.1038/labinvest.2014.98. [DOI] [PubMed] [Google Scholar]
- 38.Zheng X, et al. Serum uric acid and non-alcoholic fatty liver disease in non-obesity Chinese adults. Lipids Health Dis. 2017;16:202. doi: 10.1186/s12944-017-0531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johnson RJ, et al. Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes. 2013;62:3307–3315. doi: 10.2337/db12-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kotronen A, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–872. doi: 10.1053/j.gastro.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 41.Akter S, Nanri A, Pham NM, Kurotani K, Mizoue T. Dietary patterns and metabolic syndrome in a Japanese working population. Nutr Metab (Lond) 2013;10:30. doi: 10.1186/1743-7075-10-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miyagi S, Iwama N, Kawabata T, Hasegawa K. Longevity and diet in Okinawa, Japan: the past, present and future. Asia Pac J Public Health. 2003;15(Suppl):S3–9. doi: 10.1177/101053950301500S03. [DOI] [PubMed] [Google Scholar]
- 43.Schlosstein L, Kippen I, Bluestone R, Whitehouse MW, Klinenberg JR. Association between hypouricaemia and jaundice. Ann Rheum Dis. 1974;33:308–312. doi: 10.1136/ard.33.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim JH, Kwon SY, Lee SW, Lee CH. Validation of fatty liver index and lipid accumulation product for predicting fatty liver in Korean population. Liver Int. 2011;31:1600–1601. doi: 10.1111/j.1478-3231.2011.02580.x. [DOI] [PubMed] [Google Scholar]
- 45.Cuthbertson DJ, et al. External validation of the fatty liver index and lipid accumulation product indices, using 1H-magnetic resonance spectroscopy, to identify hepatic steatosis in healthy controls and obese, insulin-resistant individuals. Eur J Endocrinol. 2014;171:561–569. doi: 10.1530/EJE-14-0112. [DOI] [PubMed] [Google Scholar]
- 46.Mehta M, et al. Can Alcoholic Liver Disease and Nonalcoholic Fatty Liver Disease Co-Exist? J Clin Exp Hepatol. 2017;7:121–126. doi: 10.1016/j.jceh.2017.01.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bedogni G, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33. doi: 10.1186/1471-230X-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuwabara M, et al. Low frequency of toothbrushing practices is an independent risk factor for diabetes mellitus in male and dyslipidemia in female: A large-scale, 5-year cohort study in Japan. J Cardiol. 2017;70:107–112. doi: 10.1016/j.jjcc.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 49.Kuwabara M, et al. Asymptomatic Hyperuricemia Without Comorbidities Predicts Cardiometabolic Diseases: Five-Year Japanese Cohort Study. Hypertension. 2017;69:1036–1044. doi: 10.1161/HYPERTENSIONAHA.116.08998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kuwabara M, et al. Elevated Serum Uric Acid Level Predicts Rapid Decline in Kidney Function. Am J Nephrol. 2017;45:330–337. doi: 10.1159/000464260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuwabara M, et al. Increased Serum Sodium and Serum Osmolarity Are Independent Risk Factors for Developing Chronic Kidney Disease; 5 Year Cohort Study. PLoS One. 2017;12:e0169137. doi: 10.1371/journal.pone.0169137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kneeman JM, Misdraji J, Corey KE. Secondary causes of nonalcoholic fatty liver disease. Therap Adv Gastroenterol. 2012;5:199–207. doi: 10.1177/1756283X11430859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shimamoto K, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014) Hypertens Res. 2014;37:253–390. doi: 10.1038/hr.2013.80. [DOI] [PubMed] [Google Scholar]
- 54.Black HR, et al. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 6: Hypertension: A Scientific Statement from the American Heart Association and the American College of Cardiology. Circulation. 2015;132:e298–302. doi: 10.1161/CIR.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 55.International Expert, C. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care32, 1327–1334 (2009). [DOI] [PMC free article] [PubMed]
- 56.Teramoto T, et al. Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan–2012 version. J Atheroscler Thromb. 2013;20:517–523. doi: 10.5551/jat.15792. [DOI] [PubMed] [Google Scholar]
- 57.Matsuo S, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–992. doi: 10.1053/j.ajkd.2008.12.034. [DOI] [PubMed] [Google Scholar]