Abstract
Background
The aim of this study was to analyze daytime sleepiness in a sample of patients diagnosed with sarcoidosis.
Methods
A sample of 1197 German sarcoidosis patients was examined with the Epworth Sleepiness Scale (ESS), the Fatigue Assessment Scale, the Hospital Anxiety and Depression Scale, the Pittsburgh Sleep Quality Index, and the Short-Form Health Survey (SF-8). The patients' ESS mean scores were compared with those obtained from a large general population sample.
Results
Exactly 50% of the patients reached the criterion (ESS > 10) for excessive daytime sleepiness, compared with only 22.1% in the general population. The effect size for the mean score difference between both samples was d=0.62. The number of affected organs and the number of concomitant diseases proved to be significant independent predictors of daytime sleepiness. Sleepiness was associated with fatigue (r=0.45), anxiety (r=0.23), depression (r=0.28), sleep problems (r=0.23), and detriments in physical (r=−0.29) and mental (r=−0.28) quality of life.
Conclusions
The issue of excessive daytime sleepiness should be considered in the management of sarcoidosis.
1. Introduction
Sarcoidosis is a multisystem inflammatory disease, characterized by epitheloid granulomas [1]. Almost all organs of the body can be involved, but the lungs are the most frequently affected organ. Sarcoidosis patients suffer from a broad spectrum of symptoms such as muscle pain, weight loss, fever, night sweats, cough, breathlessness, and reduced exercise capacity, which results in reduced quality of life (QoL) [2, 3]. Fatigue is a symptom that is particularly prevalent in these patients [4]. This symptom is associated with poor sleep quality and excessive daytime sleepiness (EDS), which is defined as difficulty in maintaining an alert awake state in everyday situations [5]. EDS is associated with insomnia [6], obstructive sleep apnea [7], cognitive impairment [8, 9], cardiovascular diseases [10, 11], psychiatric disorders [12, 13], and low socioeconomic status [14]. The relationship between daytime sleepiness and QoL is less clear. A general population study [15] found small but consistent associations between daytime sleepiness and both physical and mental components of QoL, while among patients suffering from obstructive sleep apnea [16] daytime sleepiness was associated with physical but not mental QoL. Several studies have been performed to analyze fatigue [17, 18] and poor sleep quality [19] in patients suffering from sarcoidosis, but the role daytime sleepiness plays in sarcoidosis patients is largely unknown.
The instrument most often used for measuring daytime sleepiness is the Epworth Sleepiness Scale (ESS) [20]. Convergent, discriminant [21], and ecological validity [22] of the scale have been proved. The items of the ESS were included in the item banks of the Patient-Reported Outcomes Measurement Information System (PROMIS) “sleep disturbance and sleep-related” [23]. Using the ESS, a British study [24] compared sarcoidosis patients with healthy controls and found markedly elevated levels of daytime sleepiness among the sarcoidosis patients (M = 8.0 versus M = 4.7 in the ESS); however, the sample sizes were low (73 sarcoidosis patients and 82 controls), and the controls were not representative of the general population.
The aims of this study were (a) to determine the degree of EDS in sarcoidosis patients in comparison with the general population and to test psychometric properties of the ESS in a large sample of sarcoidosis patients, (b) to analyze the impact of affected organs and concomitant diseases on EDS, and (c) to investigate associations between daytime sleepiness and QoL.
2. Methods
2.1. Study Participants
All members of the German Sarcoidosis Society (n=4100) were invited to take part in the study and received a booklet with several questionnaires, along with the regular newsletter. Among other scales, the booklet included the ESS. The study was approved by the Ethics Committee of the Medical Faculty of the University of Leipzig. All participating individuals gave informed consent. The inclusion criteria were a diagnosis of sarcoidosis, age 18 years and above, and the willingness to take part in the study.
The scores of the general population were taken from a recent large normative study (n=9711) also performed in Germany [25]. We had access to the original data and selected a random subsample (n=7990) so that the gender distribution (65.5% women) and the mean age (M = 54.2 years) were nearly identical with the sample of the sarcoidosis patients.
2.2. Instruments
The ESS [20, 26] was designed to quantify a person's likelihood of falling asleep in several everyday situations and the degree to which sleepiness interferes with their daytime functioning. Eight items have to be answered on a four-point scale. The ESS total score is the sum of the ratings of the items, and it can range from 0 to 24. Scores of 11 and above are frequently considered indicative of EDS [27]. German normative values of the ESS are available [25].
In addition to the ESS, several other questionnaires were used in this study: the Pittsburgh Sleep Quality Index (PSQI) [28], the Fatigue Assessment Scale (FAS) [29], the Hospital Anxiety and Depression Scale (HADS) [30], and the quality of life instrument Short Form Health Survey (SF-8) [31]. Furthermore, self-reported clinical variables (affected organs, concomitant diseases, time since diagnosis, and therapy) were obtained.
2.3. Statistical Techniques
Because the proportion of females in the patients' sample was higher than in the normative study, we calculated weighted means for items and sum scores of the general population with the weights corresponding to the gender distribution of the patients' sample to enable unbiased comparisons. The resulting general population means are therefore slightly different from those reported for the total general population study. Group differences in ESS mean scores were statistically tested with t-tests. Effect sizes d were used to express the mean score difference, related to the pooled standard deviation [32]. A multiple regression analysis (method = enter) was performed to test the combined influence of several predictors of EDS. All calculations were performed with SPSS version 20.
3. Results
3.1. Sample Characteristics
Of the 4100 patients invited to participate, 1270 (31%) returned the questionnaire. 73 of these questionnaires could not be used because of missing data. In total, data from 1197 participants were ultimately included in the analysis. The sample consisted of 783 females (65.4%) and 414 males with an overall mean age of 54.3 ±11.6 years. The mean time since first diagnosis was 12.8 years (range, 0–64 years). 542 patients (45.3%) were receiving steroid therapy at the time of the survey. The most often affected organs were lungs (89.2%), followed by skin (24.5%) and lymphatic nodes (20.8%). In 39.7% of the patients, only one organ was affected, 28.2% had two affected organs, and 32.1% reported at least three affected organs.
3.2. EDS Mean Scores Compared with the General Population
Figure 1 shows ESS mean scores of the patients and the general population [25]. There was no consistent gender difference between the male and the female patients. In the first three age decades, female patients reported more EDS than male patients, while the trend was opposite for the age groups 60–69 years and ≥70 years.
Figure 1.
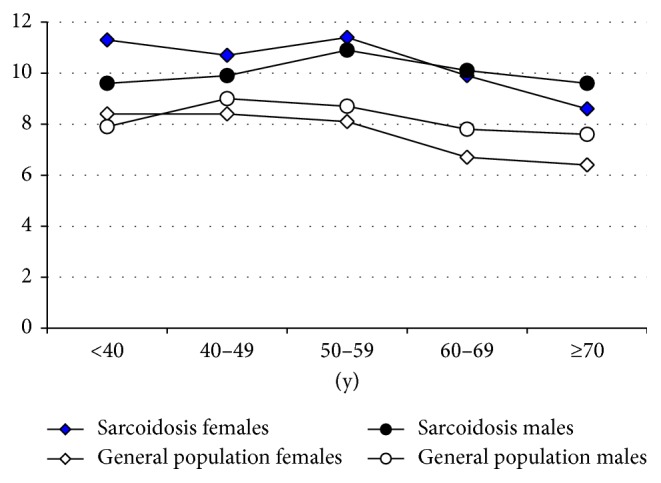
ESS mean scores for sarcoidosis patients and the general population, broken down by gender and age groups.
Every age group of sarcoidosis patients reported higher levels of EDS compared with the general population (Figure 1). The mean of the male patients was 10.18 ± 4.77, while the corresponding mean of the female patients was somewhat higher (10.56 ± 4.91), resulting in a total mean score of 10.43 ±4.87 of the patients. The corresponding mean scores of the general population were 8.26 ± 3.53 (males) and 7.55 ± 3.77 (females). This results in effect sizes of d = 0.45 (males) and d = 0.71 (females) for the comparison between sarcoidosis patients and the general population; the effect size of the total sample was d = 0.62.
Expressed in terms of patients with scores above the cutoff point for excessive daytime sleepiness (ESS > 10), the percentages were 48.1% for the male patients and 51.0% for the female patients. The corresponding percentages from the general population were 25.0% (males) and 20.6% (females) [25]. In the total sample of the sarcoidosis patients, 598 (50.0%) of the 1197 patients had scores above the cutoff point, while the corresponding percentage in the general population was 22.1%.
3.3. Item Analyses
Item mean scores are presented in Table 1. As in the general population, the afternoon is the situation with the highest chance to fall asleep. In all eight items, the patients reported more sleepiness than the general population. All items positively contributed to the ESS total score. The reliability (Cronbach's alpha) of the ESS was 0.82.
Table 1.
ESS items and global mean scores.
| Patients | General population | d | p | r it | Alpha del. | |||
|---|---|---|---|---|---|---|---|---|
| M | (SD) | M | (SD) | |||||
| 1 Sitting/reading | 1.43 | (1.01) | 1.09 | (0.89) | 0.36 | <0.001 | 0.63 | 0.78 |
| 2 Watching TV | 1.97 | (0.99) | 1.77 | (0.93) | 0.21 | <0.001 | 0.49 | 0.81 |
| 3 Public place | 1.21 | (0.97) | 0.92 | (0.82) | 0.32 | <0.001 | 0.66 | 0.78 |
| 4 Car passenger | 1.21 | (1.05) | 0.81 | (0.92) | 0.41 | <0.001 | 0.56 | 0.80 |
| 5 Afternoon | 2.41 | (0.85) | 2.06 | (0.91) | 0.40 | <0.001 | 0.36 | 0.82 |
| 6 Sitting/talking to someone | 0.39 | (0.60) | 0.13 | (0.40) | 0.52 | <0.001 | 0.58 | 0.80 |
| 7 After lunch | 1.45 | (1.02) | 1.01 | (0.87) | 0.47 | <0.001 | 0.61 | 0.79 |
| 8 Traffic | 0.32 | (0.62) | 0.14 | (0.41) | 0.35 | <0.001 | 0.48 | 0.81 |
| ESS total score | 10.43 | (4.87) | 7.95 | (3.73) | 0.58 | <0.001 | – | 0.82 |
Note. M: mean; SD: standard deviation; d: effect size; p: significance; rit: part-whole-corrected test-item correlation; alpha del.: Cronbach's alpha if item is deleted.
3.4. Effect of Clinical Variables on ESS
Table 2 shows the impact of the affected organs on EDS, expressed in univariate analyses. The sequence of the organs is arranged according to the frequency with which they were affected by the disease. Muscles and bones are the organs with the highest effect sizes. Among the concomitant diseases, sleep apnea was most strongly associated with EDS (d = 0.61). There was no statistical significant association between time since diagnosis and daytime sleepiness. Participants receiving steroid therapy were significantly more affected by daytime sleepiness than participants without that therapy.
Table 2.
The association between clinical variables and daytime sleepiness.
| Organs/comorbidity | N | M ± SD | d | t | p | |
|---|---|---|---|---|---|---|
| Organs | ||||||
| Lungs | Yes | 1086 | 10.5 ± 4.8 | 0.12 | 1.08 | 0.279 |
| No | 111 | 9.9 ± 5.0 | ||||
|
| ||||||
| Skin | Yes | 293 | 10.9 ± 4.9 | 0.13 | 1.85 | 0.065 |
| No | 904 | 10.3 ± 4.8 | ||||
|
| ||||||
| Lymphatic nodes | Yes | 249 | 11.0 ± 4.9 | 0.14 | 2.06 | 0.040 |
| No | 948 | 10.3 ± 4.9 | ||||
|
| ||||||
| Eyes | Yes | 191 | 10.4 ± 5.0 | 0.00 | 0.25 | 0.804 |
| No | 1006 | 10.4 ± 4.8 | ||||
|
| ||||||
| Liver | Yes | 141 | 11.1 ± 5.0 | 0.16 | 1.87 | 0.062 |
| No | 1056 | 10.3 ± 4.8 | ||||
|
| ||||||
| Muscles | Yes | 113 | 12.1 ± 5.1 | 0.37 | 3.87 | <0.001 |
| No | 1084 | 10.3 ± 4.8 | ||||
|
| ||||||
| Nerves | Yes | 108 | 11.0 ± 5.3 | 0.12 | 1.29 | 0.196 |
| No | 1089 | 10.4 ± 4.8 | ||||
|
| ||||||
| Bones | Yes | 105 | 12.0 ± 5.2 | 0.34 | 3.39 | 0.001 |
| No | 1092 | 10.3 ± 4.8 | ||||
|
| ||||||
| Heart | Yes | 95 | 10.9 ± 4.8 | 0.10 | 1.08 | 0.281 |
| No | 1102 | 10.4 ± 4.9 | ||||
|
| ||||||
| Kidneys | Yes | 60 | 10.7 ± 5.2 | 0.06 | 0.49 | 0.622 |
| No | 1037 | 10.4 ± 4.8 | ||||
|
| ||||||
| Number of organs | <3 | 813 | 10.1 ± 4.8 | 0.23 | 3.81 | <0.001 |
| ≥3 | 384 | 11.2 ± 4.9 | ||||
|
| ||||||
| Comorbidity | ||||||
| Arterial hypertensiona | Yes | 452 | 10.6 ± 5.0 | 0.06 | 1.02 | 0.306 |
| No | 738 | 10.3 ± 4.8 | ||||
|
| ||||||
| Disease of thyroid glanda | Yes | 320 | 10.6 ± 5.0 | 0.06 | 0.99 | 0.323 |
| No | 869 | 10.3 ± 4.8 | ||||
|
| ||||||
| Obesity (BMI ≥30)a | Yes | 320 | 11.3 ± 5.0 | 0.24 | 3.87 | <0.001 |
| No | 875 | 10.1 ± 4.8 | ||||
|
| ||||||
| Restless legs syndromea | Yes | 186 | 11.4 ± 5.2 | 0.24 | 3.00 | 0.003 |
| No | 998 | 10.2 ± 4.8 | ||||
|
| ||||||
| Diabetes mellitusa | Yes | 134 | 10.9 ± 5.2 | 0.10 | 1.26 | 0.209 |
| No | 1060 | 10.4 ± 4.8 | ||||
|
| ||||||
| Sleep apneaa | Yes | 104 | 13.1 ± 5.0 | 0.61 | 5.95 | <0.001 |
| No | 1084 | 10.1 ± 4.8 | ||||
|
| ||||||
| Pulmonary hypertensiona | Yes | 38 | 10.9 ± 5.5 | 0.10 | 0.67 | 0.503 |
| No | 1138 | 10.4 ± 4.8 | ||||
|
| ||||||
| Number of concomitant diseases | <3 | 1002 | 10.1 ± 4.8 | 0.40 | 4.30 | <0.001 |
| ≥3 | 195 | 12.1 ± 5.1 | ||||
|
| ||||||
| Time since diagnosis and therapy | ||||||
| Time since diagnosisa | ≤10 y | 625 | 10.7 ± 4.8 | 0.10 | 1.72 | 0.086 |
| >10 y | 566 | 10.2 ± 5.0 | ||||
|
| ||||||
| Steroid therapy | Yes | 542 | 10.8 ± 4.9 | 0.14 | 2.62 | 0.009 |
| No | 655 | 10.1 ± 4.8 | ||||
Note. d: effect size; t: t value of the t-test; p: significance; acase numbers not added to 1197 due to missing values.
The results of the multivariate analysis are presented in Table 3. The number of affected organs as well as the number of concomitant diseases proved to be independent factors for predicting EDS. The multiple r of this analysis was 0.21.
Table 3.
Demographic and medical factors as predictors of EDS.
| B | SE (B) | Beta | T | p | |
|---|---|---|---|---|---|
| Affected organs (sum) | 0.399 | 0.102 | 0.116 | 3.933 | <0.001 |
| Comorbidity (sum) | 0.545 | 0.117 | 0.141 | 4.652 | <0.001 |
| Age | −0.054 | 0.012 | −0.128 | 4.294 | <0.001 |
| Sex (female) | 0.030 | 0.296 | 0.003 | 0.101 | 0.920 |
3.5. Associations between Daytime Sleepiness and Other Scales
The correlations between the ESS and other scales are given in Table 4. The strongest association was found for fatigue (r=0.44). All the coefficients were statistically significant with p < 0.001.
Table 4.
Correlations between the ESS and other scales.
| Scale | r |
|---|---|
| PSQI | |
| Sleep problems | 0.23 |
|
| |
| FAS | |
| Fatigue | 0.44 |
|
| |
| HADS | |
| Anxiety | 0.23 |
| Depression | 0.28 |
|
| |
| SF-8 | |
| Physical functioning | −0.28 |
| Role-physical | −0.32 |
| Bodily pain | −0.25 |
| General health | −0.25 |
| Vitality | −0.27 |
| Social functioning | −0.30 |
| Role-emotional | −0.32 |
| Mental health | −0.26 |
| Physical component score | −0.29 |
| Mental component score | −0.28 |
4. Discussion
Excessive daytime sleepiness is common among patients suffering from sarcoidosis. Exactly 50% of the sarcoidosis patients fulfilled the criterion of EDS, while only 22.1% of the adult general population reported experiencing EDS. The effect size of the mean score difference was d = 0.62. Half a standard deviation (d = 0.50) is a frequently used criterion for clinical relevance [33]. The burden of EDS is prevalent in all age groups to a similar degree. Female patients were slightly more affected by EDS than males, though most normative studies [25,34–36] found higher degrees of sleepiness among males.
The ESS proved to be a reliable instrument for measuring EDS in sarcoidosis patients, and the alpha coefficient (0.82) was even higher than the coefficients obtained in other studies [37, 38]. All items contributed positively to the total score, and all items showed a statistically significant difference between the patients and the general population.
If the burden of patients is to be assessed in relation to the burden perceived by healthy controls, it is possible to examine a specifically selected sample of healthy controls or to refer to normative values. We used the second approach, which is more convenient and which provides more profound comparisons. The study with sarcoidosis and idiopathic pulmonary fibrosis patients [24], for example, included a control group of 82 persons with an ESS mean score of 4.7 and a HADS depression mean score of 2.1 which are markedly below the normative scores obtained in larger general population studies. Using such healthy controls can lead to an overestimation of the differences to the patient groups and to an imprecise estimation of the disease burden.
Among the affected organs, muscles and bones were seen to have the highest impact on EDS. A compromised musculoskeletal system may lead to physical inactivity and lack of exercise [39], and a low degree of physical fitness may be associated with EDS. Sarcoidosis patients experience improvements in fatigue levels when they participate in physical exercise programs [40], and they should be encouraged to be physically active even when they are bothered by EDS. However, it should be taken into account that patients whose muscles or bones are affected often have other affected organs too, and that the mean number of concomitant diseases is higher in these patient subgroups.
Concomitant diseases have an impact on EDS, in particular sleep apnea (effect size d = 0.61). This corresponds to the findings of other studies [41–43]. Sleep apnea is an interruption of sleep due to the collapse of upper airways, and it can lead to hypoxic episodes. This reduced sleep quality is also associated with daytime sleepiness. The number of affected organs as well as the number of comorbidities proved to be independent prognostic factors for EDS in the multiple regression analysis. This indicates that there are additive effects of the affected organs and concomitant diseases which should be taken into account when treating this patient population. The frequency of several concomitant diseases in the patients' sample was higher than in the general population. Therefore, it is difficult to clarify which proportion of the heightened EDS level is due to sarcoidosis itself and which proportion can be attributed to comorbidity. However, even if the causal relationship between sarcoidosis and comorbidity is unclear, clinicians should know that patients with sarcoidosis experience heightened levels of daytime sleepiness. The clinicians should advise their patients to maintain correct sleep hygiene.
Patients receiving steroid therapy were more strongly affected by EDS than patients without that therapy (Table 2). However, even the patients not receiving steroid therapy had markedly higher daytime sleepiness scores (M = 10.1) than people from the general population (M = 7.95). This means that sarcoidosis itself (and not the therapy) is the main reason for the heightened levels of sleepiness.
All correlations between the ESS scores and the QoL and mental health scales were statistically significant and clinically meaningful. The strongest association was found with fatigue (r=0.45) which underlines the impact of EDS on symptoms such as fatigue. Consistent with the Chinese [15] and the German [25] general population study, daytime sleepiness was associated with both physical and mental components of QoL, and the correlations with the physical component score (r=−0.28) and the mental component score (r=−0.29) were nearly identical. This might help explain the strong association with fatigue, a concept which also consists of both physical and mental components. This cross-sectional study does not allow for drawing conclusions about causality. EDS might cause fatigue and vice versa.
Some limitations of the study should be noted. The presence of sarcoidosis in the sample was not determined by clinical diagnosis, and all clinical data were self-reported. The representativeness of the patients' sample is difficult to assess, thus possibly introducing a selection bias. The univariate analyses presented in Table 2 do not take into account the combined effects of affected organs and concomitant diseases.
In summary, EDS is a problem for one out of every two sarcoidosis patients. Not only sleep quality and depression but also daytime sleepiness should be considered when treating patients suffering from sarcoidosis.
Acknowledgments
The authors thank the German Sarcoidosis Association for its support to the study. The authors also acknowledge the support from the Universität Leipzig within the program of Open Access Publishing.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Valeyre D., Prasse A., Nunes H., et al. Sarcoidosis. The Lancet. 2014;383(9923):1155–1167. doi: 10.1016/s0140-6736(13)60680-7. [DOI] [PubMed] [Google Scholar]
- 2.de Vries J., Drent M. Quality of life and health status in sarcoidosis: a review of the literature. Clinics in Chest Medicine. 2008;29(3):525–532. doi: 10.1016/j.ccm.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Judson M. A. Quality of life in sarcoidosis. Seminars in Respiratory and Critical Care Medicine. 2017;38(4):546–558. doi: 10.1055/s-0037-1602589. [DOI] [PubMed] [Google Scholar]
- 4.de Kleijn W. P. E., de Vries J., Lower E. E., et al. Fatigue in sarcoidosis: a systematic review. Current Opinion in Pulmonary Medicine. 2009;15(5):499–506. doi: 10.1097/mcp.0b013e32832d0403. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd. Darien, IL, USA: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 6.Drake C. L., Vargas I., Roth T., et al. Quantitative measures of nocturnal insomnia symptoms predict greater deficits across multiple daytime impairment domains. Behavioral Sleep Medicine. 2015;13(1):73–87. doi: 10.1080/15402002.2014.880345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cvengros J. A., Rodríguez V. M., Snyder S., et al. An adaptive treatment to improve positive airway pressure (PAP) adherence in patients with obstructive sleep apnea: a proof of concept trial. Behavioral Sleep Medicine. 2017;15(5):345–360. doi: 10.1080/15402002.2015.1135292. [DOI] [PubMed] [Google Scholar]
- 8.Jaussent I., Bouyer J., Ancelin M. L., et al. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep. 2012;35(9):1201–1207. doi: 10.5665/sleep.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Byun E., Kim J., Riegel B. Associations of subjective sleep quality and daytime sleepiness with cognitive impairment in adults and elders with heart failure. Behavioral Sleep Medicine. 2017;15(4):302–317. doi: 10.1080/15402002.2015.1133418. [DOI] [PubMed] [Google Scholar]
- 10.Newman A. B., Spiekerman C. F., Enright P., et al. Daytime sleepiness predicts mortality and cardiovascular disease in older adults: the Cardiovascular Health Study Research Group. Journal of the American Geriatrics Society. 2000;48(2):115–123. doi: 10.1111/j.1532-5415.2000.tb03901.x. [DOI] [PubMed] [Google Scholar]
- 11.Jaussent I., Empana J. P., Ancelin M. L., et al. Insomnia, daytime sleepiness and cardio-cerebrovascular diseases in the elderly: a 6-year prospective study. PLoS One. 2013;8(2) doi: 10.1371/journal.pone.0056048.e56048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaussent I., Bouyer J., Ancelin M. L., et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep. 2011;34(8):1103–1110. doi: 10.5665/sleep.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ng T. H., Chung K.-F., Lee C.-T., et al. Eveningness and its associated impairments in remitted bipolar disorder. Behavioral Sleep Medicine. 2016;14(6):650–664. doi: 10.1080/15402002.2015.1065407. [DOI] [PubMed] [Google Scholar]
- 14.Jarrin D. C., McGrath J. J., Silverstein J. E., et al. Objective and subjective socioeconomic gradients exist for sleep quality, sleep latency, sleep duration, weekend oversleep, and daytime sleepiness in adults. Behavioral Sleep Medicine. 2013;11(2):144–158. doi: 10.1080/15402002.2011.636112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu S., Wang R., Ma X., et al. Excessive daytime sleepiness assessed by the Epworth Sleepiness Scale and its association with health related quality of life: a population-based study in China. BMC Public Health. 2012;12(1):p. 849. doi: 10.1186/1471-2458-12-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee W., Lee S.-A., Ryu H. U., et al. Quality of life in patients with obstructive sleep apnea: relationship with daytime sleepiness, sleep quality, depression, and apnea severity. Chronic Respiratory Disease. 2016;13(1):33–39. doi: 10.1177/1479972315606312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drent M., Lower E. E., Vries J. D. Sarcoidosis-associated fatigue. European Respiratory Journal. 2012;40(1):255–263. doi: 10.1183/09031936.00002512. [DOI] [PubMed] [Google Scholar]
- 18.Strookappe B., de Vries J., Elfferich M., et al. Predictors of fatigue in sarcoidosis: the value of exercise testing. Respiratory Medicine. 2016;116:49–54. doi: 10.1016/j.rmed.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 19.Bosse-Henck A., Wirtz H., Hinz A. Subjective sleep quality in sarcoidosis. Sleep Medicine. 2015;16(5):570–576. doi: 10.1016/j.sleep.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 20.Johns M. W. A new method for measuring daytime sleepiness–the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 21.Kaambwa B., Mpundu-Kaambwa C., Adams R., et al. Suitability of the Epworth Sleepiness Scale (ESS) for economic evaluation: an assessment of its convergent and discriminant validity. Behavioral Sleep Medicine. 2016 doi: 10.1080/15402002.2016.1228647. In press. [DOI] [PubMed] [Google Scholar]
- 22.Broderick J. E., Junghaenel D. U., Schneider S., et al. Pittsburgh and Epworth sleep scale items: accuracy of ratings across different reporting periods. Behavioral Sleep Medicine. 2013;11(3):173–188. doi: 10.1080/15402002.2012.654549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu L., Buysse D. J., Germain A., et al. Development of short forms from the PROMIS™ sleep disturbance and Sleep-Related Impairment item banks. Behavioral Sleep Medicine. 2011;10(1):6–24. doi: 10.1080/15402002.2012.636266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Atkins C. P., Gilbert D., Brockwell C., et al. Fatigue in sarcoidosis and idiopathic pulmonary fibrosis: differences in character and severity between diseases. Sarcoidosis Vasculitis and Diffuse Lung Diseases. 2016;33:130–138. [PubMed] [Google Scholar]
- 25.Sander C., Hegerl U., Wirkner K., et al. Normative values of the Epworth Sleepiness Scale (ESS), derived from a large German sample. Sleep and Breathing. 2016;20(4):1337–1345. doi: 10.1007/s11325-016-1363-7. [DOI] [PubMed] [Google Scholar]
- 26.Bloch K. E., Schoch O. D., Zhang J. N. N., et al. German version of the Epworth Sleepiness Scale. Respiration. 1999;66(5):440–447. doi: 10.1159/000029408. [DOI] [PubMed] [Google Scholar]
- 27.Johns M., Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20(10):844–847. doi: 10.1093/sleep/20.10.844. [DOI] [PubMed] [Google Scholar]
- 28.Buysse D. J., Reynolds C. F., Monk T. H., et al. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14(4):331–338. doi: 10.1093/sleep/14.4.331. [DOI] [PubMed] [Google Scholar]
- 29.Vries J. D., Michielsen H., van Heck G. L., et al. Measuring fatigue in sarcoidosis: the Fatigue Assessment Scale (FAS) British Journal of Health Psychology. 2004;9(3):279–291. doi: 10.1348/1359107041557048. [DOI] [PubMed] [Google Scholar]
- 30.Zigmond A. S., Snaith R. P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 31.Ware J. E., Kosinski M., Dewey J. E., et al. How to Score and Interpret Single-Item Health Status Measures: A Manual For Users of The SF-8TM Health Survey. Lincoln, RI, USA: QualityMetric Incorporated; 2001. [Google Scholar]
- 32.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ, USA: Erlbaum; 1988. [Google Scholar]
- 33.Norman G. R., Sloan J. A., Wyrwich K. W. Interpretation of changes in health-related quality of life—the remarkable universality of half a standard deviation. Medical Care. 2003;41(5):582–592. doi: 10.1097/00005650-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Pallesen S., Nordhus I. H., Omvik S., et al. Prevalence and risk factors of subjective sleepiness in the general adult population. Sleep. 2007;30(5):619–624. doi: 10.1093/sleep/30.5.619. [DOI] [PubMed] [Google Scholar]
- 35.Tsuno N., Jaussent I., Dauvilliers Y., et al. Determinants of excessive daytime sleepiness in a French community-dwelling elderly population. Journal of Sleep Research. 2007;16(4):364–371. doi: 10.1111/j.1365-2869.2007.00606.x. [DOI] [PubMed] [Google Scholar]
- 36.Gander P. H., Marshall N. S., Harris R., et al. The Epworth Sleepiness Scale: Influence of age, ethnicity, and socioeconomic deprivation. Epworth sleepiness scores of adults in New Zealand. Sleep. 2005;28(2):249–253. doi: 10.1093/sleep/28.2.249. [DOI] [PubMed] [Google Scholar]
- 37.Chen N. H., Johns M. W., Li H. Y., et al. Validation of a Chinese version of the Epworth sleepiness scale. Quality of Life Research. 2002;11(8):817–821. doi: 10.1023/a:1020818417949. [DOI] [PubMed] [Google Scholar]
- 38.Beaudreau S. A., Spira A. P., Stewart A., et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Medicine. 2012;13(1):36–42. doi: 10.1016/j.sleep.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spruit M. A., Thomeer M. J., Gosselink R., et al. Skeletal muscle weakness in patients with sarcoidosis and its relationship with exercise intolerance and reduced health status. Thorax. 2005;60(1):32–38. doi: 10.1136/thx.2004.022244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marcellis R., van der Veeke M., Mesters I., et al. Does physical training reduce fatigue in sarcoidosis? Sarcoidosis Vasculitis and Diffuse Lung Diseases. 2015;32(1):53–62. [PubMed] [Google Scholar]
- 41.Patterson K. C., Huang F., Oldham J. M., et al. Excessive daytime sleepiness and obstructive sleep apnea in patients with sarcoidosis. Chest. 2013;143(6):1562–1568. doi: 10.1378/chest.12-1524. [DOI] [PubMed] [Google Scholar]
- 42.Spira A. P., Beaudreau S. A., Stone K. L., et al. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. Journals of Gerontology Series A—Biological Sciences and Medical Sciences. 2012;67(4):433–439. doi: 10.1093/gerona/glr172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sauter C., Asenbaum S., Popovic R., et al. Excessive daytime sleepiness in patients suffering from different levels of obstructive sleep apnoea syndrome. Journal of Sleep Research. 2000;9(3):293–301. doi: 10.1046/j.1365-2869.2000.00211.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


