Abstract
Descending mediastinitis is a rare, life-threatening condition caused by contiguous spread of oropharyngeal or cervical infection into the mediastinum. Infectious mononucleosis generally results in a self-limited illness characterized by fever, pharyngitis and lymphadenopathy. We present an exceptional case of an 18-year-old with infectious mononucleosis complicated by progressive bacterial superinfection and fulminant descending mediastinitis. After resuscitation, broad spectrum antibiotics, critical care support and definitive surgical management, they made a full recovery.
INTRODUCTION
Contiguous spread of oropharyngeal or cervical infection into the mediastinum is termed descending mediastinitis (DM). Bacteria from the oral microflora spread into the mediastinum along the three fascial pathways of the neck: pretracheal, lateropharyngeal and retropharyngeal [1]. DM can present as a wide clinical spectrum, ranging from subacute to fulminant, with extensive fascial necrosis, abscesses and severe sepsis. Infectious mononucleosis (IM) is an acute illness caused by the Epstein-Barr herpes virus (EBV), characterized by fever, sore throat, fatigue, cervical lymphadenopathy, pharyngitis and splenomegaly [2]. Although IM ordinarily results in a mild self-limiting illness, we present an exceptional case of EBV infection complicated by life-threatening DM.
CASE PRESENTATION
A previously well 18-year-old male self-presented to the Emergency Department of an academic hospital with an 8 h history of shortness of breath and severe right-sided chest pain. He also had a 14-day history of fever, sore throat, dysphagia and fatigue, and had been admitted to hospital 6 days prior to presentation for symptomatic management of presumed tonsillitis, being discharged after 24 h observation with a 10-day course of Penicillin V. IM was subsequently confirmed by the detection of EBV specific antibodies (positive IgM and IgG anti-viral capsid antigens) at this attendance.
On examination the patient was noted to be in severe discomfort with right chest pain and tenderness. He was dyspnoeic with a respiratory rate of 30 breaths per minute and peripheral oxygen saturations of 94%. Temperature was 37.4°C, pulse rate 120 beats per minute and blood pressure 100/70 mmHg. Throat examination revealed bilateral symmetrical tonsillar swelling with white exudate, and bilateral cervical lymphadenopathy. Physical examination was otherwise unremarkable.
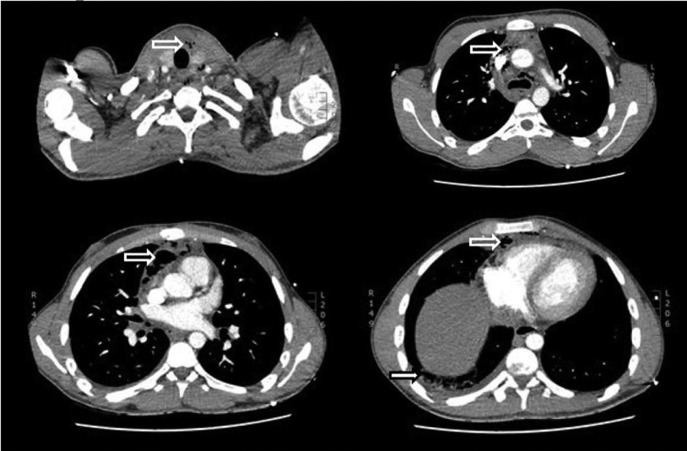
Initial laboratory investigations demonstrated: leucocytosis (11.8 × 109/l) with atypical lymphocytes; elevated C-reactive protein (346 mg/l); and elevated liver enzymes (alkaline phosphatase 147 IU/l, alanine aminotransferase 76 IU/l). Computed tomography imaging of the thorax and neck showed extensive pneumomediastinum with mediastinal fat stranding and pockets of fluid in the anterior mediastinum (Fig. 1). A small right pleural effusion, inflammatory consolidation in the right lung, reactive lymph nodes, splenomegaly and enlarged lymphoid tissue in the posterior nasopharynx were also noted. There was no evidence of oesophageal perforation; and peritonsillar or retropharyngeal abscesses were not present.
Figure 1:
CT scan of neck and thorax showing mediastinal/cervical emphysema (hollow white arrows) and right empyema (solid white arrow).
Initial management was commenced with IV opioid analgesia, fluid resuscitation, amoxicillin and clavulanic acid, and cardiothoracic surgery consultation. Over the next 4 h the patient deteriorated with increased chest pain and worsening physiology. Antibiotics were changed to a regimen of IV Piperacillin and tazobactam with clindamycin, and the patient underwent emergent video-assisted thoracoscopic surgery with drainage and decortication of a right pleural empyema, drainage of multiple mediastinal abscesses, debridement of mediastinal necrotic tissue, and insertion of a right-sided intercostal drain. Fusobacterium necrophorum, Dialister pneumosintes and Peptostreptococcus anaerobius were detected in mediastinal fluid. Post-operatively the patient was admitted to the intensive care unit for supportive care. After a 22-day period in the hospital, including 14 days of intensive care, the patient was discharged home well.
DISCUSSION
DM most commonly originates from odontogenic infection, retropharyngeal abscess, peritonsillar abscess or cervical lymphadenitis [1]. It is a very rare complication of IM, which has been reported only four times previously (Table S1, Supplementary File). Similar to previous patients, the current case was young and previously well. The marked chest pain and chest wall tenderness we observed appear to be novel presenting features. Mediastinitis was accompanied by pleural empyema in all reported cases, with thoracic wall abscesses, mediastinal collections and pericardial effusions/collection also observed as additional complications in individual cases. Gas forming anaerobic bacteria were predominantly causative in all patients, with the upper respiratory tract commensal Fusobacterium necrophorum a prominent pathogen.
It has been postulated that EBV infection results in transient immunosuppression due to a decrease in T cell-mediated immunity, which may predispose to a secondary bacterial superinfection, possibly resulting in peritonsillar abscess. DM could then arise by progressive infection, or following breakthrough of an abscess into the retropharyngeal or lateropharyngeal space [3]. Unlike previous cases, there was no evidence of peritonsillar abscess in our patient, suggesting secondary infection of the tonsils with progressive spread as the likely mechanism. Interestingly, the patient had taken 6 days of oral Penicillin V prior to presentation, which did not prevent development of DM.
DM is a life-threatening condition with reported mortality rates between 5 and 40% [1]. All reported EBV-associated cases of DM were promptly recognized with early definitive surgical management which may explain the 100% survival rate observed. Although the rarity of DM hinders accumulation of clinical experience, it is essential that the diagnosis is considered in patients with a recent diagnosis of IM presenting with shortness of breath, chest pain and sepsis enabling early recognition and treatment to facilitate a full recovery.
Supplementary Material
SUPPLEMENTARY MATERIAL
Supplementary material is available at the Journal of Surgical Case Reports online.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Lloyd T, Tran VK. Acute mediastinitis as a complication of Epstein-Barr virus. CJEM 2016;18:149–51. [DOI] [PubMed] [Google Scholar]
- 2. Geerts JW, van Driel EM, Janssen MJ. Descending mediastinitis in Epstein-Barr virus infection. J Clin Microbiol 2015;53:1781–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chandak TR, Wong P, Hussain E, Kim A Fulminant descending mediastinitis, bilateral empyema and respiratory failure: a rare complication of infectious mononucleosis (IM), 2011.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.