Abstract
Aim:
The aim of this study is to evaluate the marginal sealing ability of self-adhesive flowable composite resin when used as a liner in Class II composite restoration with and without aging.
Materials and Methods:
A total of 120 standardized Class II tooth preparations with gingival margins 1 mm coronal and apical to cementenamel junction (CEJ) were prepared on 60 extracted permanent mandibular molars and were randomly divided into eight equal Groups: Group 1: cavities coronal to CEJ and restored with Dyad flow liner + Herculite ultra, Group 2: same as Group 1 but cavities margins apical to CEJ, Group 5: cavities coronal to CEJ and restored with only Herculite ultra, and Group 6: same as Group 5 but cavities apical to CEJ. Groups 3,4,7,8 were similar to Groups 1,2,5,6, respectively, but were aged for 6 months. After thermocycling, microleakage testing was done using 0.5% basic fuchsin dye.
Result:
At cervical level, Group 5 exhibited statistically lower (P = 0.006) microleakage than Group 6, and Group 1 showed lesser microleakage than Group 5 (P = 0.162). Group 2 exhibited significantly less microleakage than Group 6 (P = 0.002). Increased microleakage was observed in aging Groups; however, the difference with nonaging Groups was not statistically significant (P > 0.005).
Conclusion:
Margins of the cavity in cementum can be better sealed by placing self-adhesive liner and is not affected by aging.
Keywords: Intermediate restorative material, microleakage, nanocomposite, self-adhesive flowable composite
INTRODUCTION
The advent of resin-based composites served as a viable tooth-colored alternative to amalgam restorations.[1] However, the most common shortcoming of composite was postoperative sensitivity due to gap formation as a result of polymerization shrinkage especially at the gingi-val cavosurface margin.[2]
To overcome this problem, use of resin-modified GIC and flowable composites as the intermediate restorative material between dentin and resin composites were suggested. Due to its low viscosity, increased elasticity, and wettability, the flowable resin composite may be useful in absorbing the stress caused by polymerization shrinkage.[3]
As a further advancement, recently, an innovative resin-based material, combining the properties of self-adhesion and flowability, was developed (Dyad Flow, Kerr, Orange, CA, USA), introducing a new category of restorative materials defined as “self-adhering composite resins” which eliminates the need for a separate bonding application step.
Hence, the hypothesis tested was that self-adhesive composite reduces microleakage in Class II composite restoration when used as a liner both above and below cementoenamel junction (CEJ).
MATERIALS AND METHODS
A total of 60 noncarious, freshly extracted human permanent mandibular molar teeth of similar dimensions with no cracks, decay, fracture, abrasion, previous restorations, or structural deformities (extracted for periodontal reasons) were selected. The teeth were thoroughly cleaned immediately after extraction, stored in 0.1%. Thymol solution for 1 week for disinfection (ISO/TS11405:2003 specifications) and then placed in distilled water until they were used to prevent dehydration (storage period <3 months). Standardized mesio-occlusal and disto-occlusal Class II tooth preparations were made (Occlusal box: depth 2 mm, buccolingual width 3 mm, mesiodistal width 4 mm. Proximal box: buccolingual width 3 mm, width of gingival seat = 1.5 mm). The tooth preparation was initiated with diamond round point #2 followed by straight fissure point #559. Subsequently, inverted cone diamond point #35 was used to create flat pulpal floor and gingival seat. About 30 samples were randomly selected, and cervical margin of the proximal box was placed 1-mm coronal to the CEJ in these samples, whereas in the remaining samples, the cervical margin was placed 1 mm apical to the CEJ. A sound tooth structure of 2 mm was left between the two cavity preparations in each tooth. The measurements were verified with a graduated Williams periodontal probe. The prepared teeth were randomly divided into eight groups on the basis of the restorative technique used. Group 1 (n = 15): cavities extending coronal to CEJ and restored with self-adhesive flowable composite liner + composite restoration (without aging), Group 2 (n = 15): cavities extending apical to CEJ and restored with self-adhesive flowable composite liner + composite restoration (without aging), Group 3 (n = 15): cavities extending coronal to CEJ and restored with self-adhesive flowable composite liner + composite restoration (with aging), Group 4 (n = 15): cavities extending apical to CEJ and restored with self-adhesive flowable composite liner + composite restoration (with aging), Group 5 (n = 15): cavities extending coronal to CEJ and restored with composite restoration without use of liner (without aging), Group 6 (n = 15): cavities extending apical to CEJ and restored with composite restoration without use of liner (without aging), Group 7 (n = 15): cavities extending coronal to CEJ and restored with composite restoration without use of liner (with aging), and Group 8 (n = 15): cavities extending apical to CEJ and restored with composite restoration without use of liner (with aging).
After cavity preparation, samples were restored with the respective restorative technique. In the group with liner, a layer of self-adhesive flowable composite (Dyad Flow) approximately 1 mm in thickness was placed to cover the entire gingival floor of the cavity. Subsequently, in all the groups, bonding agent (OptiBond All-In-One) was scrubbed with an applicator tip for 20 s on all the cavity wall surfaces. The application was repeated and air dried for 5 s followed by light curing for 10 s using LED-curing light in continuous mode. The cavities were then restored with a “nanohybrid” composite (Herculite ultra) using a horizontal incremental technique (1 mm thick) from the cervical to the occlusal surface. Each increment was cured for 20 s from the occlusal surface with a LED-curing light in continuous mode. Then, the metallic matrix was removed, and the restorations were light cured for 20 s from the buccal and lingual surfaces. Further, finishing and polishing were done with the super-snap kit in sequential manner as per manufacturer instructions.
The samples were placed in porous, cotton cloths of different colors, which helped in the identification of different groups. They were then subjected to thermocycling with 500 cycles in a customized thermocycling device and each cycle com-prised of specimens been subjected to 5°C, 37°C and 55°C temperature water bath with a transfer time of 15 s and a dwell time of 30 s between each cycle. Subsequently, in the half of the samples, two coats of nail paint were applied by applicator brush to coat the foramina and the entire sample surface except for the restoration and 1-mm area beyond the margins followed by sticky wax. Further, they were immersed in freshly prepared 0.5% basic fuchsin organic dye and sectioned mesiodistally from the center of the restorations. Samples were then evaluated under stereomicroscope, and microscopic observations were scored using the ISO microleakage scoring system (ISO/TS 11405:2003) according to which numerical values were assigned to represent the extent of dye penetration.
Occlusal microleakage scores
0 = No dye penetration
1 = Dye penetration into enamel
2 = Dye penetration into the dentine, not including the pulpal wall/gingival floor
3 = Dye penetration into the dentine including the pulpal wall.
Cervical Microleakage Scores
0 = No dye penetration
1 = Dye penetration into ½ of the cervical wall
2 = Dye penetration into all the cervical wall
3 = Dye penetration into the cervical and axial wall.
The remaining half of the specimens were subjected to aging in distilled water for 6 months after which they were tested for microleakage.
STATISTICAL ANALYSIS AND RESULTS
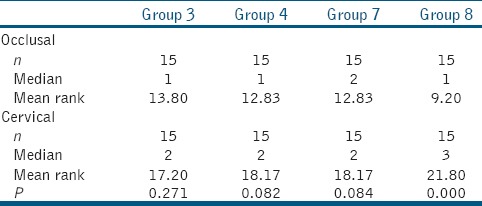
Microleakage values were compared using the “Mann–Whiney U-test.” At cervical level, Group 2 exhibited significantly less microleakage than Group 6 (P = 0.002). Group 5 exhibited statistically lower (P = 0.006) microleakage than Group 6, and Group 1 showed less microleakage than Group 5 (P = 0.162); however, the difference was not significant. Increased microleakage was observed in aging Groups (3, 4, 7, and 8); however, the difference with nonaging Groups (1, 2, 5, and 6) was not statistically significant. Microleakage scores were lower at the occlusal margins as compared to cervical margins in all the groups. It was also observed that there was no significant difference in occlusal scores among all the groups (Groups 1, 2, 5, and 6) [Tables 1–3 and Figures 1, 2].
Table 1.
Comparison of microleakage scores of occlusal and cervical margins among different groups (without aging)
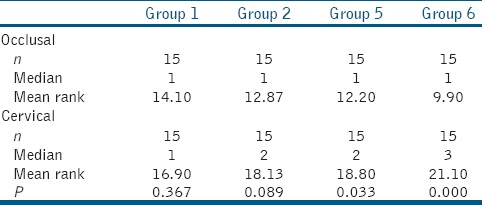
Table 3.
Intragroup comparison of microleakage
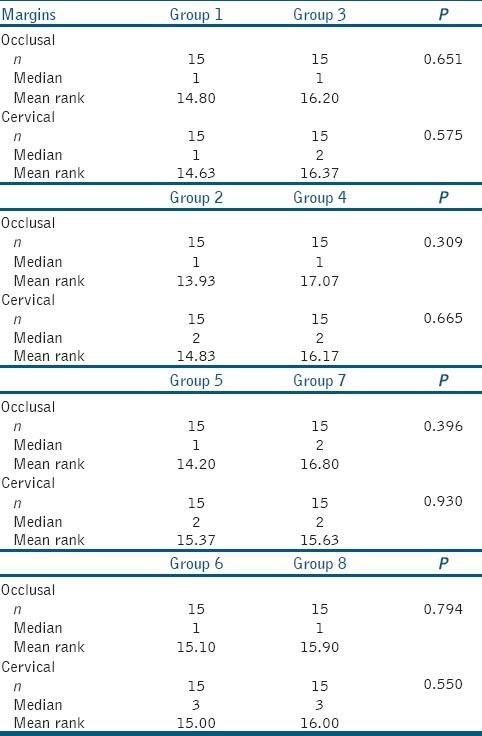
Figure 1.
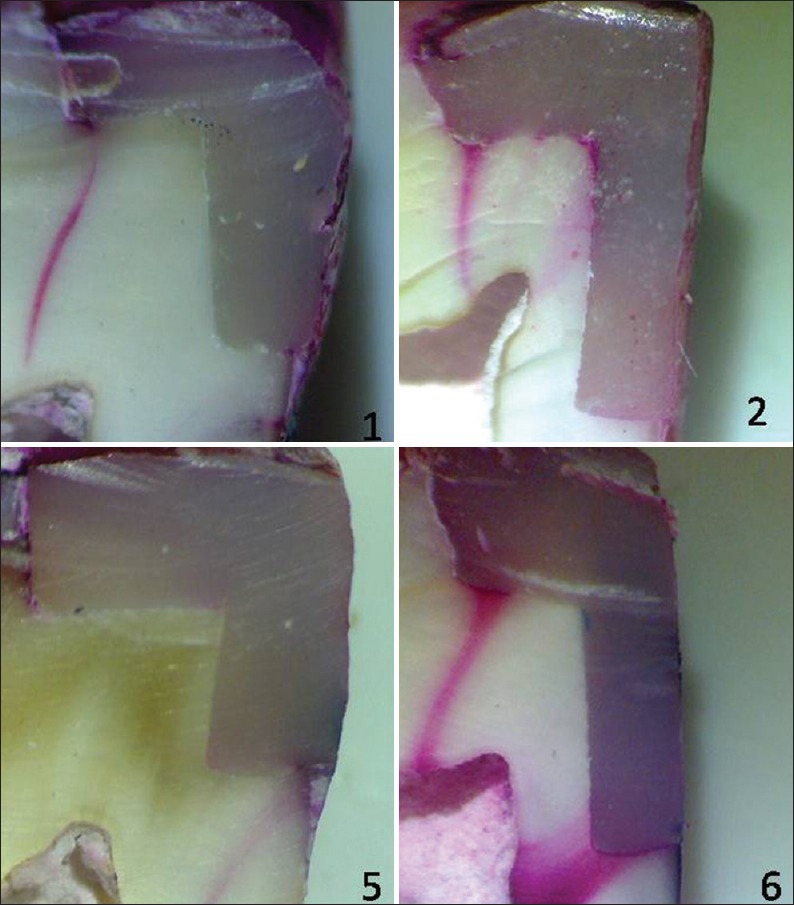
Stereomicroscopic images of groups 1, 2, 5, and 6
Figure 2.
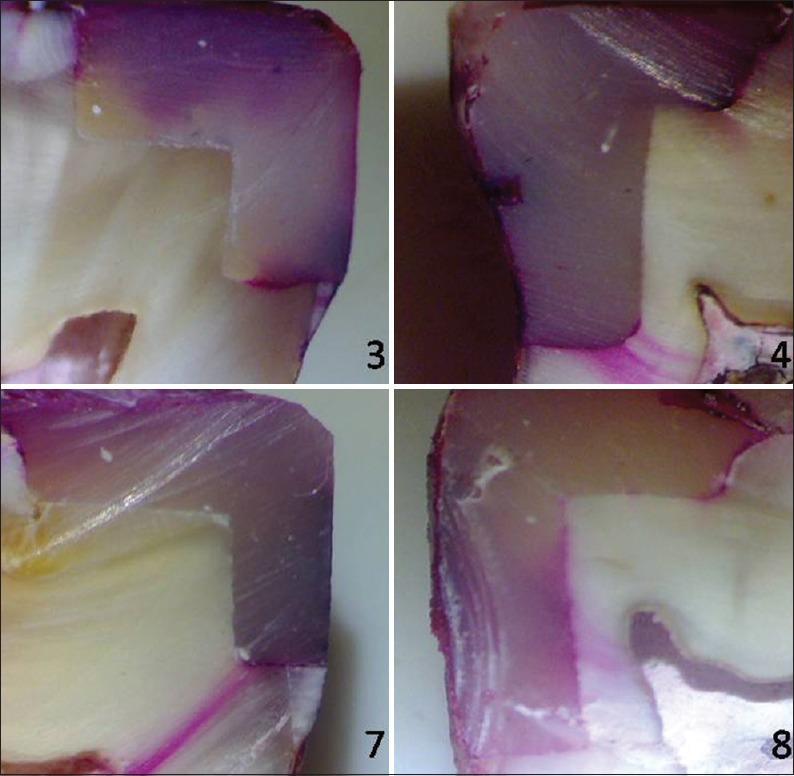
Stereomicroscopic images of groups 3, 4, 7, and 8
Table 2.
Comparison of microleakage scores of occlusal and cervical margins among different groups (with aging)
DISCUSSION
Failure is usually seen in the Class II composite restorations with the cervical margin below the CEJ, due to a gap which usually forms along the cervical wall, which could be due to shrinkage of the composite during polymerization (of up to 2.0%)[4] or from mismatches between either the coefficients of thermal expansion of the tooth and the composite or between the elastic moduli of the tooth and the composite. This phenomenon leads to microleakage.[5]
Cervical lining restoration techniques (Sandwich technique) were developed to overcome this disadvantage of resin composites. Some in vitro studies[6,7] have shown that the use of flowable composites as a liner reduces restoration microleakage, and the occurrence of voids was due to their low viscosity, increased elasticity, and wettability.
With the introduction of self-adhering flowable composite (Dyad Flow, Kerr, Orange, CA, USA), which combines the properties of self-adhesion and flowability, the technique of application was further simplified. These resins are based on the bonding technology that uses glycerophosphate dimethacrylate (GPDM) to etch enamel and dentin, and hydroxyethyl methacrylate to enhance wetting and penetration by resin into dentin. This resin bonds chemically between the phosphate groups of a GPDM monomer and the hydroxyapatite of tooth structure and also micromechanically between the polymerized monomers of the self-adhering flowable composite resin and the collagen fibers and smear layer of dentin.[8]
Varying the filler particles helps prevent microleakage, increase the modulus of elasticity, and rigidity for the adhesive system. This means that the filler size and content play an important role in the clinical performance of adhesive systems.[5] Hence, a new category of resin composite was developed and named as nanofilled composites. The microfilled composites present nearly 37%–40% volume of filler loading while the nanofilled resins have approximately 60% volume filler loading, making the nanofilled resins as strong as the hybrid and microhybrid resins.[9]
A variety of different techniques for assessing microleakage have been developed and utilized. The most modern techniques utilize different principles involving biological, chemical, electrical, physical, or radioactive components. These include the use of dyes, radioactive isotopes, air pressure, bacteria, neutron activation analysis, artificial caries, scanning electron microscopy, calcium hydroxide, and other methods.[10,11]
The use of organic dyes is one of the most popular techniques using this principle. It is also one of the oldest and time-tested methods. Some of the organic dyes used including basic fuchsin, methylene blue, eosin, aniline blue, crystal violet, drawing ink, and erythrosine The basic fuchsin dye is one of the most commonly used dyes today.[12] Percentage concentration currently in use ranges from 0.5% to 2.0%.[13] Hence, the samples were immersed in 0.5% basic fuchsin for 24 h. This is the most commonly used and advocated organic dye in the literature[9,14] for dye penetration scores due to its low-molecular size of 1–2 nm. The sectioned teeth were observed under a stereomicroscope at 12× magnification and scored for the degree of dye penetration by two blindfolded examiners. Microleakage scores were independently assigned by two examiners, and in case of disagreement between their evaluations, the worst score was considered for statistical analysis. Microscopic observations were scored using the ISO microleakage scoring system (ISO/TS 11405:2003).[15]
In the current study, all specimens were stored in distilled water for 6 months which was periodically changed to prevent bacterial growth. To simulate the oral environment, the samples were kept in the incubator at 37°C. Various methods of aging composites artificially have been described in the literature, for example, storage of the dry material at 37°C in acids, immersion in distilled water, hot water or artificial saliva, and accelerated artificial aging by thermocycling at different temperatures. In the present study, we have used thermocycling and storage in distilled water for artificial aging. Saliva was not used because of the possibility of growth of microorganisms over a period.
At cervical level, composite exhibited significantly more microleakage at the cementum margin when compare to the enamel margin. This may be because of the better bonding of composite to enamel since dentin exhibit less reliable bonding due to its complex structure.[16] Within the enamel margin, flowable composite liner exhibited less microleakage than without flowable composite liner although the difference was not statistically significant (P = 0.162). It appears that the influence of low elastic modulus on stress development of flowable composites is surpassed by their high contraction strain, resulting in stress levels that are equivalent to those obtained with nonflowable material.[17] Flowable composite liner exhibited more microleakage at the cementum margin when compare to the enamel margin (P = 0.493). The low modulus of elasticity of flowable composite allows for plastic deformation, which acts as an elastic buffer and increases the flexibility of the bonded assembly and might act as a shock absorber, and thus, compensates for contraction shrinkage stress when used as a liner.[18] In self-adhesive flowable composite, there is a high hygroscopic expansion of the hydrophilic acidic phosphate Group and a short spacer Group in the adhesive monomer (GPDM). The hygroscopic expansion and relatively low polymerization shrinkage might be the reason for this high-sealing performance.[18] Within the cementum margin, flowable composite liner exhibited significantly less microleakage than without flowable composite liner (P = 0.002). Composites have a relatively high modulus of elasticity and employing an intermediate layer of flowable composite liner may provide better adaptation. Due to their relative flexibility, these liners help relieve stresses during polymerization shrinkage of the composite restorations. The use of flowable materials as a liner underneath the resin composites may reduce the effects of the C-factor. Lowering the C-factor may lower the internal stresses within the placed restoration.[19]
Microleakage scores were lower at the occlusal margins as compared to cervical margins in all the Groups. This is due to the lesser thickness of enamel at the cavo surface margin of the proximal aspect which requires adhesion of the restorative materials to greater proportion of dentin. An additional reason may be the bonding of composite to a more complex substrate (cementum/dentin) than enamel.[16] Another reason for increased gingival microleakage when compared to occlusal relates to the distance of light source from the material at the proximal box especially the gingival floor as compared to occlusal surfaces.[16] It was also observed that there was no significant difference in occlusal scores among all the Groups. The reason could be that the same materials and techniques were used in all the Groups at the occlusal level.
At 6 months, aging increased microleakage in all the Group although the difference was statistically nonsignificant. This showed that aging had no significant effect on the microleakage of both nanofilled and flowable composites in the enamel and cementum margins. Microleakage in the aging Groups followed the same pattern as that of the nonaging Groups. Previous studies[20,21] have also assessed the effect of aging on microleakage of composites and have concluded that aging pronounced produces no significant effect. Gonulol et al.[22] concluded that when the composite Groups were compared for 5000 and 15,000 thermal cycles, no significant differences were detected for both enamel and cementum microleakage scores. In contrast, Naga et al.[8] in his study found increased microleakage of the tested materials with aging. However, the study assessed the effect of aging regarding cyclic loading which may have led to a difference in the results.
The limitations of this study were sample size and relatively lesser aging period (6 months) was observed. Hence, further studies are required to demonstrate the effect of aging.
CONCLUSION
Within the limitations of this study, it can be concluded that self-adhesive flowable composite, when used as a liner below composite in open sandwich restorations, can significantly decrease the microleakage and hence provide better marginal sealing ability when the cervical margin is in cementum. In addition, the marginal sealing ability of nanofilled composite with or without the use of a self-adhesive flowable liner is not significantly affected over a period of 6 months.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Saraswati MV, Jacob G, Ballal NV. Evaluation of the influence of flowable liner and two different adhesive systems on the microleakage of packable composite resin. J Interdiscip Dent. 2012;2:98–103. [Google Scholar]
- 2.Eunice C, Margarida A, Joao CL, Filomena B, Anabela P, Pedro A, et al. Evaluation of microleakage of composite resin restorations with SonicFill. An in vitro experimental model. J Stomatol. 2012;2:1–9. [Google Scholar]
- 3.Vichi A, Goracci C, Ferrari M. Clinical study of the self-adhering flowable composite resin Vertise flow in class II restoration: Six month follow-up. Int Dent SA. 2012;12:14–23. [Google Scholar]
- 4.Feilzer AJ, De Gee AJ, Davidson CL. Curing contraction of composites and glass-ionomer cements. J Prosthet Dent. 1988;59:297–300. doi: 10.1016/0022-3913(88)90176-x. [DOI] [PubMed] [Google Scholar]
- 5.Narayana V, Ashwathanarayana S, Nadig G, Rudraswamy S, Doggalli N, Vijai S, et al. Assessment of microleakage in class II cavities having gingival wall in cementum using three different posterior composites. J Int Oral Health. 2014;6:35–41. [PMC free article] [PubMed] [Google Scholar]
- 6.Attar N, Tam LE, McComb D. Flow, strength, stiffness and radiopacity of flowable resin composites. J Can Dent Assoc. 2003;69:516–21. [PubMed] [Google Scholar]
- 7.Qin M, Liu H. Clinical evaluation of a flowable resin composite and flowable compomer for preventive resin restorations. Oper Dent. 2005;30:580–7. [PubMed] [Google Scholar]
- 8.Naga AA, Yousef M, Ramadan R, Fayez Bahgat S, Alshawwa L. Does the use of a novel self-adhesive flowable composite reduce nanoleakage? Clin Cosmet Investig Dent. 2015;7:55–64. doi: 10.2147/CCIDE.S80462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadeghi M. Influence of flowable materials on microleakage of nanofilled and hybrid class II composite restorations with LED and QTH LCUs. Indian J Dent Res. 2009;20:159–63. doi: 10.4103/0970-9290.52891. [DOI] [PubMed] [Google Scholar]
- 10.Crisp S, Wilson AD. Radioactive tracer technique for monitoring of microleakage: An interim report. J Biomed Mater Res. 1980;14:373–82. doi: 10.1002/jbm.820140404. [DOI] [PubMed] [Google Scholar]
- 11.Trowbridge HO. Model systems for determining biologic effects of microleakage. Oper Dent. 1987;12:164–72. [PubMed] [Google Scholar]
- 12.Taylor MJ, Lynch E. Microleakage. J Dent. 1992;20:3–10. doi: 10.1016/0300-5712(92)90002-t. [DOI] [PubMed] [Google Scholar]
- 13.Mente J, Ferk S, Dreyhaupt J, Deckert A, Legner M, Staehle HJ, et al. Assessment of different dyes used in leakage studies. Clin Oral Investig. 2010;14:331–8. doi: 10.1007/s00784-009-0299-8. [DOI] [PubMed] [Google Scholar]
- 14.Poggio C, Chiesa M, Scribante A, Mekler J, Colombo M. Microleakage in class II composite restorations with margins below the CEJ:In vitro evaluation of different restorative techniques. Med Oral Patol Oral Cir Bucal. 2013;18:e793–8. doi: 10.4317/medoral.18344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.International Standards Organization. Dental Materials-testing of Adhesion to Tooth Structure ISO Standard 11405. Geneva: ISO-TS; 2003. [Google Scholar]
- 16.Simi B, Suprabha B. Evaluation of microleakage in posterior nanocomposite restorations with adhesive liners. J Conserv Dent. 2011;14:178–81. doi: 10.4103/0972-0707.82631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lokhande NA, Padmai AS, Rathore VP, Shingane S, Jayashankar DN, Sharma U, et al. Effectiveness of flowable resin composite in reducing microleakage - an in vitro study. J Int Oral Health. 2014;6:111–4. [PMC free article] [PubMed] [Google Scholar]
- 18.Charlton DG, Moore BK, Swartz ML. An in vitro evaluation of the use of resin liner to reduce microleakage and improve retention of amalgam restorations. Oper Dent. 1992;17:112–9. [PubMed] [Google Scholar]
- 19.Reddy SN, Jayashankar DN, Nainan M, Shivanna V. The effect of flowable composite lining thickness with various curing techniques on microleakage in class II composite restorations: An in vitro study. J Contemp Dent Pract. 2013;14:56–60. doi: 10.5005/jp-journals-10024-1270. [DOI] [PubMed] [Google Scholar]
- 20.Khoroushi M, Mansoori M. Marginal sealing durability of two contemporary self-etch adhesives. ISRN Dent. 2012;2012:204813. doi: 10.5402/2012/204813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mousavinasab SM, Atai M, Alavi B. To compare the microleakage among experimental adhesives containing nanoclay fillers after the storages of 24 hours and 6 months. Open Dent J. 2011;5:52–7. doi: 10.2174/1874210601105010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gonulol N, Ertas E' Yılmaz A, Soner C. Effect of thermal aging on microleakage of current flowable composite resins. J Dent Sci. 2015;10:376–82. [Google Scholar]


