Abstract
Background:
Optimal patient selection is key to the success of nonoperative treatment for rotator cuff tears.
Purpose:
To assess the predictors of pain and functional outcomes in a longitudinal cohort of patients undergoing nonoperative treatment.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A multicenter cohort of patients with rotator cuff tears undergoing nonoperative treatment was recruited from March 2011 to February 2015. Patients completed a detailed health questionnaire, completed standardized shoulder questionnaires including the Shoulder Pain and Disability Index (SPADI), and underwent magnetic resonance imaging. In addition to baseline assessments, patients received follow-up questionnaires at 3, 6, 12, and 18 months. Longitudinal mixed models were used to test predictors of the SPADI score, and interactions with time were assessed.
Results:
In our cohort of 70 patients, being married as compared with being single/divorced/widowed (P = .02), a shorter duration of symptoms (P = .02), daily shoulder use at work that included light or no manual labor versus moderate or heavy manual labor (P = .04), alcohol use of 1 to 2 times per week or more as compared with 2 to 3 times per month or less (P = .007), and absence of fatty infiltration (P = .0009) were significantly associated with decreased SPADI scores (improved shoulder pain and disability) over time. When interactions with time were assessed, having a college level of education or higher compared with less than a college education showed a differential effect over time, with those with a college level of education or more having lower SPADI scores (P = .004). Partial-thickness tear versus full-thickness tear also had an interaction with follow-up duration, such that those with a partial-thickness tear had lower SPADI scores (P = .0002).
Conclusion:
Longitudinal predictors of better outcomes of the nonoperative treatment of rotator cuff tears included being married, having at least a college education, shorter duration of symptoms, light or manual labor in daily work, alcohol use of 1 to 2 times per week or more, partial-thickness tear, and absence of fatty infiltration of the rotator cuff. Our results suggest that nonoperative treatment should be performed early for optimal outcomes. These data can be used to select optimal candidates for the nonoperative treatment of rotator cuff tears and to assist with patient education and expectations before treatment.
Keywords: rotator cuff, outcomes, physical therapy, rehabilitation, shoulder pain
Patients with symptomatic rotator cuff tears are typically offered either operative or nonoperative treatment. Studies indicate that patients undergoing nonoperative treatment for rotator cuff tears have improved pain and function at follow-up.3,4,7,11 Patient selection based on characteristics associated with better outcomes is key to the success of nonoperative treatment.
Most prior studies have focused on factors associated with outcomes after surgical treatment. As such, there are sparse data on longitudinal predictors of better pain and functional outcomes after nonoperative treatment. Prior studies have also assessed only a limited number of factors associated with the outcomes of nonoperative treatment. A comprehensive longitudinal analysis of the possible predictors of outcomes of nonoperative treatment is lacking. These data can be useful in clinical settings to optimize outcomes after nonoperative treatment. Information on factors predicting better outcomes of nonoperative treatment may also save expenses and time toward nonoperative treatment when it is not the optimal choice. In a cohort of patients with rotator cuff tears observed longitudinally, we assessed the predictors of better pain and functional outcomes with nonoperative treatment.
Methods
Patient Population
We recruited a prospective cohort of patients with symptomatic (for at least 4 weeks) rotator cuff tears undergoing nonoperative treatment in a multicenter longitudinal study termed the Rotator Cuff Outcomes Workgroup (ROW). Randomization to treatment was not performed in this study. Nonoperative treatment recommendations included physical therapy. As this was a pragmatic cohort study, the frequency and duration of physical therapy were not standardized. Patients could pursue corticosteroid injections or medications as per their preferences.
Patients aged 45 years and older were recruited from sports/shoulder clinics at 3 academic settings and 1 community setting between March 2011 and February 2015. Exclusion criteria were a current shoulder fracture, prior shoulder surgery (on the index shoulder), and active cervical radiculopathy (elicited as neck pain radiating to the shoulder/arm/hand). Patients who underwent rotator cuff surgery during follow-up (n = 7) or had missing information on the Shoulder Pain and Disability Index (SPADI), our primary outcome measure, were excluded from the analysis (n = 7). Patients provided informed consent, and the study was approved by our institutional review board.
Structured History Questionnaire and Outcome Measures
Patients completed a structured shoulder and general health questionnaire at baseline. An abbreviated version of this questionnaire (without questions on comorbidities and social history) was completed by patients at each of the follow-up time points. This questionnaire assessed patient demographics, comorbidities, symptoms, smoking/alcohol habits, and patient expectations after treatment about the magnitude of improvement expected. Daily shoulder use at work was assessed by asking patients about manual labor at their current job. If patients were not working, they were instructed to answer the question for their past job. The Fear-Avoidance Beliefs Questionnaire (FABQ) was administered to patients. The FABQ was designed by Waddell et al16 to assess fear-avoidance beliefs about physical activity and work in patients with low back pain. We modified the FABQ (4 items that contribute toward scoring) to state “shoulder” instead of “back” for our study. The scale has 24 possible points, with a higher score indicating worse fear-avoidance behavior. Mental health was assessed using the Mental Health Inventory (MHI-5),2 a component of the 36-item Short-Form Health Survey.17 MHI-5 scores range from 0 to 100. A score of ≤68 on the MHI-5 is indicative of a probable mood disorder (including depression).10,15
Patients also completed shoulder pain and function questionnaires including the SPADI,14 a standardized 13-item questionnaire. The SPADI has a pain scale (5 items) and a disability scale (8 items) that elicit information on pain and functional limitations with activities of daily living. The composite SPADI score ranges from 0 to 100, with higher scores reflecting worse pain and function. The minimal clinically important difference for the SPADI is 10 points. If a patient was missing more than 2 items of the SPADI, the SPADI score was assigned a missing value.
Strength Testing
Strength testing was performed using a handheld dynamometer in abduction, external rotation, and internal rotation by trained research assistants only at baseline. A clinical examination including strength testing was not performed at follow-up. Both the affected and contralateral shoulders were assessed, and an average of 2 consecutive measurements that were at least 10 seconds apart were used in our analysis. Our detailed protocol for standardized strength testing has been previously described.9,13 Strength testing using a dynamometer has good intrarater and interrater reliability.6 We used a ratio of affected shoulder strength versus contralateral shoulder strength in the analysis. There were 2 patients with a strength ratio above 3. These patients were given a value of 3 for the strength ratio to avoid outlying values in the analysis.
Diagnostic Imaging
Shoulder magnetic resonance imaging (MRI) scans were read in a blinded fashion by consensus of 2 shoulder experts (L.D.H. and N.B.J. or J.E.K. and N.B.J.). Although this was a pragmatic cohort with no specific requirements for MRI, most patients underwent MRI on a 1.5-T or 3.0-T magnet with a dedicated shoulder coil. The following sequences were usually obtained: coronal oblique fast-spin echo (FSE) proton density–weighted images, coronal oblique FSE short tau inversion recovery images, sagittal FSE proton density– or T2-weighted images with fat suppression, sagittal FSE T1-weighted images, axial T1-weighted images, and axial T2-weighted gradient echo images. Previous work has shown good interrater and intrarater reliability for these MRI readings as compared with a reading by a musculoskeletal radiologist.8 Kappa values ranged from 0.75 to 0.90 for tear presence, tear size, and tear thickness.8 MRI features including tear thickness, tear size in the longitudinal and transverse planes, fatty infiltration of the rotator cuff muscles, tendon retraction, and rotator cuff muscle atrophy were assessed. Criteria for each of these measurements follow standard nomenclature and have been previously described.8
Diagnosis of Rotator Cuff Tear
Rotator cuff tears were diagnosed based on the clinical impression of a sports/shoulder fellowship–trained attending physician and evidence of structural deficits on MRI (when available). In cases where an MRI scan was available, both of these conditions had to be met for a patient to be diagnosed with a rotator cuff tear. If an MRI scan was unavailable (because it was not clinically indicated; n = 14), the diagnosis was based on the clinician’s impression.
The diagnosis of a biceps tendon lesion was based on the physician, indicating that the patient had clinical signs and symptoms corresponding to biceps disease (a “yes/no” question).
Longitudinal Follow-up
Patients were assessed at approximately 3, 6, 12, and 18 months after the baseline visit for this analysis. Follow-up was performed via mail, and patients received telephone or email reminders if they did not return the questionnaires. All 70 patients had at least 1 follow-up from baseline, although full responses were unavailable at all of the follow-up time points (responses received: n = 59 at 3 months, n = 48 at 6 months, n = 45 at 12 months, and n = 41 at 18 months).
Statistical Analysis
We report covariate effects on the SPADI measured over 18 months of follow-up. A total of 21 variables and their interactions with time were assessed, including demographics, patient symptoms, comorbidities, personal habits, shoulder strength, and patient expectations. An a priori sample size calculation was not performed. Tear size was not used as a predictor variable because there were patients in whom MRI was not clinically indicated. Race could not be used in the analysis because of very few patients in categories except non-Hispanic white. Continuous variables were summarized using the interquartile range, median, mean, and standard deviation.
All models were estimated using a weighted linear mixed model incorporating a first-order autoregressive (AR(1)) covariance structure with time modeled as 4 dummy variables at 5 time points (baseline, 3 months, 6 months, 12 months, and 18 months). Our statistical model used all available follow-up time points for a given patient, thus increasing the power of the analysis. Results of standard goodness-of-fit and residual analyses were unremarkable. Variable interactions with time were tested independently, but the full model (including interactions regardless of statistical significance) was used to test and estimate model-based (least squares) mean contrasts. Univariate P values are presented for each variable based on the global test for the variable and interactions with time. If desired, the 21 univariate models can be interpreted, adjusting for multiplicity by the reader, using the Bonferroni adjustment (0.05/21 = 0.002).
Results
Of the 70 patients who underwent nonoperative treatment in our ROW cohort, 50% of patients were female (Table 1). The median age of participants was 64.3 years, and a majority of patients were non-Hispanic white (83%; n = 58). The median duration of symptoms was 6.0 months (mean, 21.1 ± 38.1 months). A concomitant biceps lesion was present in 30% (n = 21) of patients.
TABLE 1.
Baseline Characteristics of Patients (N = 70)a
| Sex | |
| Female | 35 (50) |
| Male | 35 (50) |
| Age, y | |
| Median (IQR) | 64.3 (59.1-68.4) |
| Mean ± SD | 63.4 ± 8.2 |
| Race/ethnicity | |
| Non-Hispanic white | 58 (83) |
| Other | 9 (13) |
| Missing | 3 (4) |
| Highest level of education | |
| Less than college | 23 (33) |
| College or above | 46 (66) |
| Missing | 1 (1) |
| Marital status | |
| Single/divorced/widowed | 19 (27) |
| Married | 49 (70) |
| Missing | 2 (3) |
| Duration of symptoms, mo | |
| Median (IQR) | 6.0 (4.0-18.0) |
| Mean ± SD | 21.1 ± 38.1 |
| Daily shoulder use at work | |
| Heavy/moderate manual labor | 12 (17) |
| Light/no manual labor | 58 (83) |
| Dominant shoulder affected | |
| No | 16 (23) |
| Yes | 50 (71) |
| Missing | 4 (6) |
| Tear as a result of trauma | |
| No | 39 (56) |
| Yes | 27 (39) |
| Missing | 4 (6) |
| External rotation strength ratiob | |
| Median (IQR) | 0.77 (0.61-0.99) |
| Mean ± SD | 0.86 ± 0.46 |
| Isolated abduction strength ratiob | |
| Median (IQR) | 0.94 (0.82-1.00) |
| Mean ± SD | 0.89 ± 0.18 |
| No. of comorbidities | |
| ≤1 | 30 (43) |
| >1 | 40 (57) |
| Smoking | |
| Never | 34 (49) |
| Past/current | 35 (50) |
| Missing | 1 (1) |
| Alcohol use | |
| 2-3 times per month or less | 40 (57) |
| 1-2 times per week or more | 29 (41) |
| Missing | 1 (1) |
| FABQ score | |
| Median (IQR) | 18.0 (12.0-21.0) |
| Mean ± SD | 16.4 ± 6.2 |
| MHI-5 score | |
| Median (IQR) | 85.0 (75.0-90.0) |
| Mean ± SD | 80.0 ± 15.0 |
| Patient expectations after treatment | |
| Great improvement | 48 (69) |
| Moderate/little/no improvement or quality of life will be worse | 20 (29) |
| Missing | 2 (3) |
| Presence of associated biceps tendon lesion | |
| No | 49 (70) |
| Yes | 21 (30) |
aData are shown as n (%) unless otherwise indicated. Missing values: duration of symptoms, n = 4; external rotation strength ratio, n = 4; isolated abduction strength ratio, n = 3; and FABQ score, n = 5. FABQ, Fear-Avoidance Beliefs Questionnaire; IQR, interquartile range; MHI-5, Mental Health Inventory.
bStrength ratio is measured as affected shoulder versus unaffected shoulder.
Imaging characteristics could be determined in 56 patients who underwent MRI. A majority of patients had a full-thickness tear (54%; n = 30) (Table 2). There was no fatty infiltration of the rotator cuff tendons in 61% (n = 34) of patients.
TABLE 2.
MRI Characteristics of Rotator Cuff Tearsa
| Longitudinal size of tear,b cm | |
| Median (IQR) | 1.0 (0.0-2.5) |
| Mean ± SD | 2.1 ± 2.9 |
| Transverse size of tear,b cm | |
| Median (IQR) | 0.75 (0.00-1.58) |
| Mean ± SD | 1.32 ± 1.8 |
| Cross-sectional area of tear,b cm2 | |
| Median (IQR) | 0.64 (0.00-3.96) |
| Mean ± SD | 7.75 ± 15.6 |
| Thickness of tearc | |
| Partial-thickness | 26 (46) |
| Full-thickness | 30 (54) |
| Fatty infiltrationd | |
| Grade 0 | 34 (61) |
| Grade 1 or greater | 15 (27) |
| Missing | 7 (12) |
| Muscle atrophyd | |
| None/mild | 43 (77) |
| Moderate/severe | 6 (11) |
| Missing | 7 (12) |
| No. of tendons torn | |
| 1 | 41 (73) |
| 2 or 3 | 15 (27) |
| Tendon retraction | |
| Stage 1 or not applicablee | 44 (79) |
| Stage 2 or more | 12 (21) |
aData are shown as n (%) unless otherwise indicated. MRI information was available for 56 patients; percentages reflect a total of 56 patients (100%). Fatty infiltration and muscle atrophy were determined by computed tomography in 2 patients, who were included in the analysis but not in the table. IQR, interquartile range; MRI, magnetic resonance imaging.
bTear size was determined by the sum of supraspinatus and infraspinatus tears in the longitudinal or transverse planes for full-thickness tears only; missing values: longitudinal, n = 3; transverse, n = 6; and cross-sectional, n = 6.
cIf any of the tendons had a full-thickness tear, the tear was classified as full-thickness.
dGrading was reported for the muscle most severely affected.
eBecause the tear was partial thickness.
In unadjusted multiple comparisons, being married as compared with being single/divorced/widowed (P = .02) (Table 3), a shorter duration of symptoms (P = .02), daily shoulder use at work that included light or no manual labor versus moderate or heavy manual labor (P = .04), and alcohol use of 1 to 2 times per week or more as compared with 2 to 3 times per month or less (P = .007) were significantly associated with decreased SPADI scores (improved shoulder pain and disability) over time. Among structural characteristics of a rotator cuff tear, absence of fatty infiltration (P = .0009) was significantly associated with decreased SPADI scores over time. The variables of sex (lower SPADI scores in male vs female patients), MHI-5 score (lower SPADI scores with increasing MHI-5 scores), and tendon retraction (lower SPADI scores with stage 1 or not applicable vs stage 2 or more) were not significant (all P < .10).
TABLE 3.
Predictors of SPADI Score at 18 Monthsa
| P Value for Variable | P Value for Variable Duration of Follow-upb | |
|---|---|---|
| Highest level of education | — | .004 |
| Marital status | .02 | .15 |
| Sex | .095 | .22 |
| Age | .18 | .39 |
| Duration of symptoms | .02 | .75 |
| Daily shoulder use at work | .04 | .29 |
| Tear as a result of trauma | .46 | .55 |
| Dominant shoulder affected | .79 | .84 |
| External rotation strength ratio | .18 | .60 |
| Isolated abduction strength ratio | .33 | .68 |
| Alcohol use | .007 | .77 |
| No. of comorbidities | .23 | .50 |
| Smoking | .26 | .51 |
| FABQ score | .13 | .09 |
| MHI-5 score | .065 | .75 |
| Patient expectations after treatment | .87 | .10 |
| Presence of associated biceps tendon lesion | .42 | .75 |
| Fatty infiltration | .0009 | .12 |
| Thickness of tear | — | .0002 |
| Tendon retraction | .08 | .11 |
| No. of torn tendons | .19 | .83 |
aVariables significant at P < .05 are boldfaced. FABQ, Fear-Avoidance Beliefs Questionnaire; MHI-5, Mental Health Inventory; SPADI, Shoulder Pain and Disability Index.
bIf the interaction is significant, the P value for the variable is not reported.
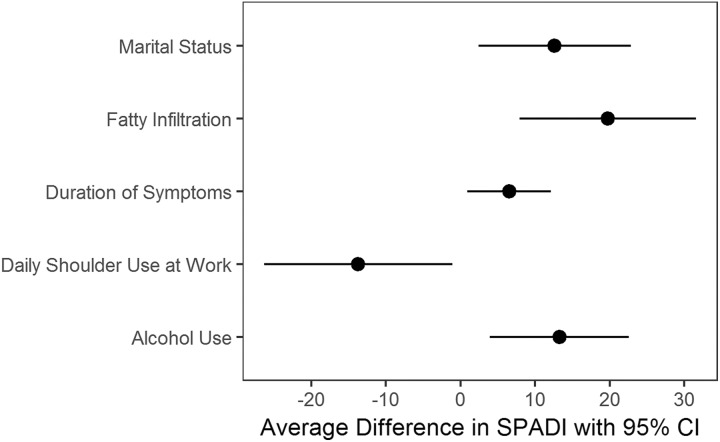
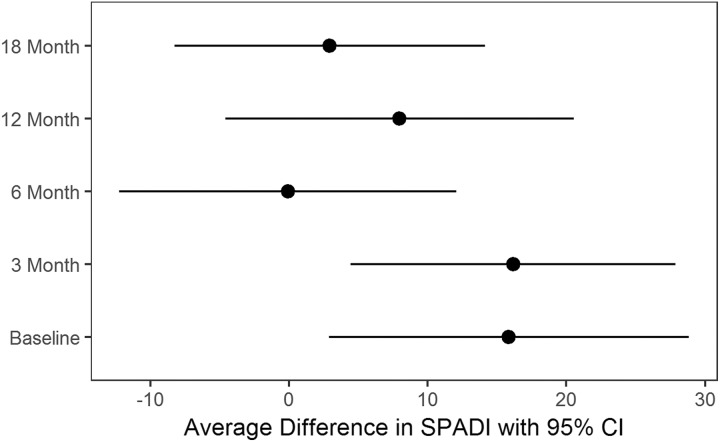
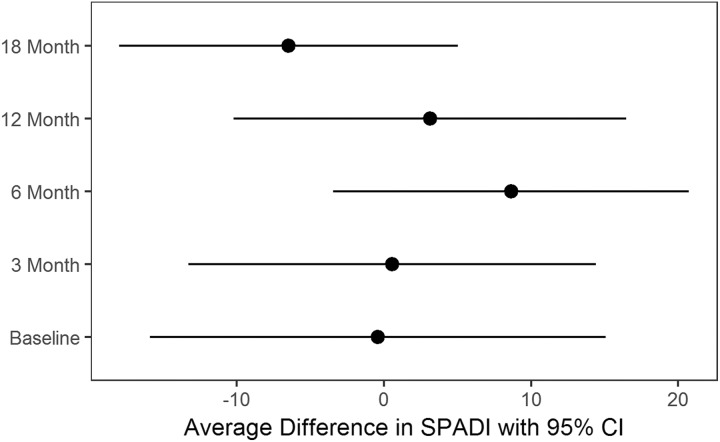
When interactions with time were assessed, having a college level of education or more versus less than a college education showed a differential effect over time, with those with a college level of education or more having lower SPADI scores (P = .004). Partial-thickness tear versus full-thickness tear also had an interaction with time, such that those with a partial-thickness tear had lower SPADI scores (P = .0002). We present a visual representation of differences in SPADI scores between groups for significant variables (Figures 1 -3).
Figure 1.
Estimated differences with 95% CIs in Shoulder Pain and Disability Index (SPADI) scores for significant variables. Estimated differences represent the following comparisons with a positive difference, indicating that the first group in the comparison has higher SPADI scores (worse shoulder pain and disability): (A) marital status: single/divorced/widowed versus married; (B) duration of symptoms (months): 75th percentile (2.89 months, log-transformed) versus 25th percentile (1.39 months, log-transformed); (C) daily shoulder use at work: moderate to heavy versus no or light; (D) alcohol use: 2-3 times per month or less versus 1-2 times per week or more; and (E) fatty infiltration: grade 0 versus grade 1 or more.
Figure 2.
Estimated differences with 95% CIs in Shoulder Pain and Disability Index (SPADI) scores for patients with less than a college education versus those with at least a college education. Estimated differences at each of the time points are presented given the significant interaction of highest level of education with time.
Figure 3.
Estimated differences with 95% CIs in Shoulder Pain and Disability Index (SPADI) scores for patients with a full-thickness versus partial-thickness tear. Estimated differences at each of the time points are presented given the significant interaction of tear thickness with time.
Discussion
We assessed the predictors of outcomes after nonoperative treatment in patients with rotator cuff tears in a well-characterized longitudinal cohort. Treatment outcomes were measured using the SPADI, which is a pain and functional assessment. The SPADI was used as the primary outcome for our analysis because it is reliable, validated, and shoulder specific. It also has multiple items that assess pain. The predictors of better outcomes included being married, a shorter duration of symptoms, light or no manual labor in daily work, alcohol use of 1 to 2 times per week or more, and absence of fatty infiltration of the rotator cuff. Education had an interaction with duration of follow-up in that there was a greater improvement in patients with at least a college level of education with a shorter duration of follow-up. Tear thickness also had an interaction with time in that those with partial-thickness tears had better shoulder pain and function. All of these differences were significant. It is possible that these factors are also associated with better outcomes of operative treatment. Our study did not report on a comparison of outcomes of operative versus nonoperative treatments.
Nonoperative treatment is one of the standards of care for patients with rotator cuff tears. Often, nonoperative treatment is the first line of treatment before surgery is considered. Rehabilitation with physical therapy is the mainstay of nonoperative treatment, although other options/adjuvant therapies such as watchful waiting, acupuncture, iontophoresis, phonophoresis, transcutaneous electrical nerve stimulation, pulsed electromagnetic field, ultrasound, pharmacological management with analgesics or anti-inflammatories, and corticosteroid injections are available. Patients undergoing physical therapy are shown to improve over time.3,4,7,11 However, nonoperative treatment including physical therapy is expensive, requires a substantial time commitment from the patient, and uses health care resources. In some instances, nonoperative treatment is unsuccessful and thus can be an unneeded step toward operative treatment. An assessment of the predictors of better outcomes after nonoperative treatment can possibly save time and resources spent on patients who may not benefit from such treatments. Our study accomplishes this goal in a well-characterized longitudinal cohort. We performed a longitudinal analysis and assessed factors possibly associated with the outcomes of nonoperative treatment in a single study.
Previous literature on the predictors of outcomes of nonoperative treatment is limited. A few single-institution studies that have addressed this issue have analyzed a limited number of factors associated with treatment outcomes.1,4,7 We assessed a variety of potential factors that could be expected to be associated with treatment outcomes.
Bartolozzi et al1 observed 136 patients with impingement syndrome and rotator cuff disease and assessed outcomes using the University of California, Los Angeles (UCLA) shoulder rating system at a mean follow-up of 20 months. A tear size ≥1 cm2 (as compared with tendon lesions without a tear, a partial-thickness tear, and a tear size <1 cm2), duration of symptoms >1 year (as compared with ≤1 year). and greater functional impairment at initial presentation were associated with worse outcomes. Our results also showed that a longer duration of symptoms was associated with worse outcomes. It is possible that some patients improved over a period of time with no treatment, and these patients were not included in our cohort because they did not seek care, leading to a selection bias in our cohort. Although tear size could not be analyzed in our study, tear thickness was significantly associated with the outcomes of nonoperative treatment and showed an interaction with time. Most of the effect was seen at 6 months, in which patients with partial-thickness tears had better outcomes as compared with those with full-thickness tears.
There are data to suggest that tears increase in size over time.12 If this hypothesis is applied to the progression of partial-thickness tears to full-thickness tears, early nonoperative treatment may be advised because the progression of a tear may lead to worse outcomes in the future, especially in younger patients. The presence of fatty infiltration, which is likely a sign of a chronic rotator cuff tear, was associated with worse outcomes in our study. The presence of fatty infiltration, along with a longer chronicity of symptoms that predicts worse outcomes in our analysis, possibly indicates that nonoperative treatment is most efficacious in patients with a shorter duration of symptoms and absence of fatty infiltration.
Goldberg et al4 reported in 46 patients that younger age and tears in the dominant extremity were associated with patients experiencing improvement after the nonoperative treatment of rotator cuff tears. Neither of these variables was associated with outcomes in our analysis, which are similar to the results from the study of Itoi and Tabata.7 However, daily shoulder use at work was associated with outcomes in our study. Patients working in no or light manual labor jobs had significantly better outcomes as compared with those working in moderate or heavy manual labor jobs. It is likely that daily job demands in those performing moderate or heavy labor do not allow recovery in shoulder pain and function because of repetitive use/trauma.
Abduction strength and range of motion at initial presentation have been significantly associated with improvement in shoulder pain, motion, and strength at follow-up in 23 patients at over 5 years of follow-up.7 Shoulder strength was not a significant predictor of outcomes in our study. However, we performed strength testing using a handheld dynamometer as opposed to the manual muscle strength testing that was performed by Itoi and Tabata.7
Harris et al5 reported on a large cohort of 389 patients who underwent nonoperative treatment for symptomatic, atraumatic, full-thickness rotator cuff tears. Outcomes were assessed using the Western Ontario Rotator Cuff Index (WORC) and American Shoulder and Elbow Surgeons (ASES) score. Their study assessed factors associated with outcome scores at baseline and not at follow-up. Hence, data from that study cannot be used to determine the predictors of outcomes of nonoperative treatment. A higher education, active abduction range of motion, and strength in forward elevation and abduction were associated with better outcome scores at baseline. Male sex, supraspinatus atrophy, infraspinatus atrophy, and presence of scapulothoracic dyskinesia were associated with worse outcome scores at baseline.
Social demographic determinants such as level of highest education and marital status were predictors of outcomes in our study. A married status and higher level of education may indicate better social support, better compliance with nonoperative treatment, or better pain-coping mechanisms, leading to better treatment outcomes. The association of alcohol use with treatment outcomes in our study is puzzling. It is possible that alcohol use is a proxy for another variable that was not measured in our cohort.
Limitations of our study include a relatively small sample size, missing MRI information in 14 patients and hence the noninclusion of tear size as one of the predictor variables, and unavailability of complete data at all of the outcome time points. We also did not have physical examination information or repeat MRI during follow-up, which was limited to 18 months. Patients with missing MRI information were included in the analysis. It is important to include patients without MRI scans in the analysis to avoid a spectrum bias in patients undergoing nonoperative treatment, who in many cases do not need imaging unless surgery is indicated. A follow-up physical examination and longer term follow-up were also unavailable. The analysis could also not be stratified by tear thickness because of the relatively small sample size. However, this is one of the few studies to longitudinally assess prognostic factors in patients undergoing nonoperative treatment with a comprehensive set of potential predictor variables.
In our prospective cohort study, the longitudinal predictors of better outcomes of nonoperative treatment during 18 months of follow-up included being married, having a college level of education or more, a shorter duration of symptoms, light or manual labor in daily work, alcohol use of 1 to 2 times per week or more, partial-thickness tears, and absence of fatty infiltration of the rotator cuff. Our results suggest that nonoperative treatment should be performed early for optimal outcomes. These data can be used to optimize patient selection for the nonoperative treatment of rotator cuff tears.
Acknowledgment
The authors thank the entire ROW team for their efforts. They also thank the clinical staff at the Orthopaedic & Arthritis Center at Brigham and Women’s Hospital, the Shoulder Service at Massachusetts General Hospital, and the Vanderbilt Orthopaedic Institute for their efforts and cooperation.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This project was supported by the Clinical and Translational Science Awards program (CTSA No. UL1TR000445) from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health. N.B.J. is supported by funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (1K23AR059199 and 1U34AR069291). K.B. has received consulting fees from Wright Medical Group and educational support from Arthrex. E.M. has received educational support from NuVasive and Smith & Nephew. L.D.H. has received educational support from Arthrex and Ethicon.
Ethical approval for this study was obtained from Partners HealthCare and the Vanderbilt University Institutional Review Board.
References
- 1. Bartolozzi A, Andreychik D, Ahmad S. Determinants of outcome in the treatment of rotator cuff disease. Clin Orthop Relat Res. 1994;(308):90–97. [PubMed] [Google Scholar]
- 2. Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. [DOI] [PubMed] [Google Scholar]
- 3. Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993;(294):103–110. [PubMed] [Google Scholar]
- 4. Goldberg BA, Nowinski RJ, Matsen FA., 3rd Outcome of nonoperative management of full-thickness rotator cuff tears. Clin Orthop Relat Res. 2001;(382):99–107. [DOI] [PubMed] [Google Scholar]
- 5. Harris JD, Pedroza A, Jones GL, Group MS. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med. 2012;40(2):359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg. 2002;11(1):33–39. [DOI] [PubMed] [Google Scholar]
- 7. Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1992;(275):165–173. [PubMed] [Google Scholar]
- 8. Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R. 2015;7(3):245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jain NB, Wilcox RB, 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R. 2013;5(1):45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kelly MJ, Dunstan FD, Lloyd K, Fone DL. Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: a comparison of five different methods. BMC Psychiatry. 2008;8:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22(10):1371–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mall NA, Kim HM, Keener JD, et al. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92(16):2623–2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Miller JE, Higgins LD, Dong Y, et al. Association of strength measurement with rotator cuff tear in patients with shoulder pain: the Rotator Cuff Outcomes Workgroup study. Am J Phys Med Rehabil. 2016;95(1):47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a Shoulder Pain and Disability Index. Arthritis Care Res. 1991;4(4):143–149. [PubMed] [Google Scholar]
- 15. Thorsen SV, Rugulies R, Hjarsbech PU, Bjorner JB. The predictive value of mental health for long-term sickness absence: the Major Depression Inventory (MDI) and the Mental Health Inventory (MHI-5) compared. BMC Med Res Methodol. 2013;13:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. [DOI] [PubMed] [Google Scholar]
- 17. Ware JE, Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]