Abstract
In Arizona during 1997–2013, coccidioidomycosis increased from 21 to 90 cases/100,000 population, but coccidioidomycosis-associated deaths remained stable at 3–6 deaths/million population. We used the capture-recapture method by using death certificates and hospital discharge data to more fully estimate the total number of coccidioidomycosis-attributable deaths and compared this with published estimates. Death certificates were included if any cause of death included coccidioidomycosis; hospital discharge data deaths were included if any discharge diagnosis included coccidioidomycosis and laboratory confirmation. Among deaths during 2008–2013, we identified 529 coccidioidomycosis-attributable deaths from death certificates and 560 from hospital discharge data, with 251 deaths identified in both databases. Capture-recapture estimated 1,178 total coccidioidomycosis-attributable deaths, compared with 164 deaths (underlying cause of death) or 529 deaths (any cause of death) on death certificates. Coccidioidomycosis-attributable deaths are underreported from two- to sevenfold on Arizona death certificates, demonstrating an education need for death certifiers to document coccidioidomycosis mortality.
Keywords: coccidioidomycosis, cause of death, epidemiology, surveillance, capture-recapture
Introduction
Coccidioidomycosis, or Valley fever, is a fungal respiratory disease caused by inhalation of Coccidioides species spores, which are found predominantly in the soil of arid environments in the southwestern United States and Central and South America.1 An estimated 150,000 annual infections occur in the United States2 and ~40% of these are thought to be symptomatic.1 Of the ~147,000 coccidioidomycosis cases reported to the Centers for Disease Control and Prevention (CDC) during 1998–2014, approximately two-thirds occurred among Arizona residents.3 In 2007 in Arizona, 1,735 hospital visits associated with coccidioidomycosis with an estimated cost of $86 million were reported.4
In Arizona, despite a >fourfold increase in incidence of reported coccidioidomycosis during 1997–2013 (from 21 cases/100,000 population to 90 cases/100,000 population),5 the death rate associated with coccidioidomycosis, calculated by using the death certificate underlying cause of death, had limited change during this period (range 3–6 deaths/million population).6 Similarly, a study estimating the coccidioidomycosis death rate by using underlying and secondary causes of death on death certificates reported a stable death rate in the United States of 0.59 deaths/million population during 1998–2008.7 Because of this discrepancy between reported cases and attributable deaths and the documented inaccuracies of cause of death data from death certificates,8–11 we used a capture-recapture method to more accurately estimate total number of deaths attributable to coccidioidomycosis and to calculate the sensitivity of death certificate data in capturing these deaths. We also conducted a case-control study to identify risk factors for omission of coccidioidomycosis as cause of death on the death certificate when it in fact contributed to death.
Methods
Data sources and case definitions
We used three databases to examine coccidioidomycosis cases and deaths as follows: the Arizona electronic death registry system (EDRS), the Arizona hospital discharge database (HDD), and Arizona’s statewide medical electronic disease surveillance intelligence system (MEDSIS).
EDRS captures data from death certificates, including demographics and causes of death. In Arizona, a medical examiner, physician, physician assistant, or nurse practitioner determines the chain of events that led to the patient’s death and other conditions that contributed to death and records them on the death certificate. EDRS includes the following three sections: (1) text fields for the causes of death; (2) associated International Classification of Diseases, Tenth Revision (ICD-10) codes; and (3) the underlying cause of death ICD-10 code as determined by algorithms performed by the National Center for Health Statistics.12 For our study, an EDRS coccidioidomycosis-attributable death was defined as any cause-of-death text field including “cocci” or “Valley fever,” or including a coccidioidomycosis ICD-10 record axis code (B38.0–B38.9). After review, we excluded deaths with cause-of-death text fields not related to coccidioidomycosis, including gram positive cocci, enterococci, and pneumococci.
Arizona’s HDD includes discharge records for all hospitals licensed by the Arizona Department of Health Services (ADHS); excluded are Veteran’s Administration hospitals, Department of Defense hospitals, and hospitals on tribal land. Discharge diagnoses were coded according to the International Classification of Diseases, Ninth Revision (ICD-9). For our study, an HDD coccidioidomycosis-attributable death was defined as a patient who died in the hospital; had an ICD-9 discharge diagnosis code for coccidioidomycosis (114.0–114.9); had a death certificate (to confirm patient was actually deceased); and had laboratory confirmation of coccidioidomycosis in MEDSIS. For both databases, we restricted the analysis to deaths during 2008–2013 among Arizona residents.
Capture-Recapture
Capture-recapture is a method used to estimate the total number of a population by using multiple sources13 and is often selected in public health to estimate the total incidence of a disease, including unreported cases, by using multiple incomplete surveillance data sources.14–17 We used a 2-source capture-recapture method by using EDRS and HDD to estimate the total number of coccidioidomycosis-attributable deaths in Arizona during 2008–2013.
We matched cases of coccidioidomycosis-attributable deaths in EDRS and HDD by using Link Plus 2.0 software18 by name, social security number, and date of birth. The software assigns a score to each potential pair of patients based on the probability of a true match. Lower scores with a lower probability were reviewed for final determination of a match. Patients who were identified in HDD but were missing from EDRS (e.g., had a death certificate that did not include coccidioidomycosis as a cause of death) were identified.
Total number of coccidioidomycosis-attributable deaths was estimated by the Chapman 2-source capture-recapture formula n = [(NEDRS+1)(NHDD+1)/(NBOTH+1)] − 1, where NEDRS = the number of deaths reported only in EDRS, NHDD = number of deaths reported only in HDD, and NBOTH = number of deaths reported in both databases;13,19 95% confidence intervals (CIs) were also determined.20,21 We calculated the sensitivity of coccidioidomycosis-attributable death estimates by using only EDRS and only HDD by comparing the number of coccidioidomycosis-attributable deaths reported from these sources with the capture-recapture estimate. We also calculated the sensitivity of coccidioidomycosis-attributable death estimates compared to the capture-recapture estimate using more narrow inclusion criteria, including only the underlying cause of death in EDRS, all ICD-10 cause of death codes on the death certificate not including text in EDRS, or only the primary diagnosis in HDD.
Case-Control
To determine risk factors for omitting coccidioidomycosis as a cause of death on the death certificate, we compared coccidioidomycosis-attributable deaths from HDD for which coccidioidomycosis was included as any cause of death (n = 251), including the text on the death certificate, with those for which coccidioidomycosis was not included as cause of death on the death certificate (n = 309) during 2008–2013. We compared demographics, disseminated versus pulmonary disease, and comorbidities by using discharge ICD-9 codes for disease classification. Disseminated disease includes patients with ICD-9 codes for coccidioidomycosis meningitis (114.2) and progressive coccidioidomycosis (114.3). Patients with ICD-9 codes for chronic coccidioidomycosis (114.4), unspecified pulmonary coccidioidomycosis (114.5), and unspecified coccidioidomycosis (114.9) were not included when comparing disseminated and pulmonary disease. Immunocompromised status and malignancy were classified according to the Agency for Healthcare Research and Quality definitions.22 Unadjusted odds ratios (ORs) and CIs were calculated; we calculated adjusted odds ratios (aORs) by using a multivariable logistic regression model that included age, race, and sex, in addition to variables with significant unadjusted ORs (human immunodeficiency virus [HIV] status and type of coccidioidomycosis). All analyses used SAS® Version 9.3 (SAS Institute, Incorporated, Cary, North Carolina, USA).
Medical record review and validation
To ensure that coccidioidomycosis contributed to the deaths identified in HDD for which coccidioidomycosis was not included as a cause of death on the death certificate (i.e., missed coccidioidomycosis-attributable deaths), medical records for all missed coccidioidomycosis-attributable deaths that occurred in Maricopa County residents in 2012 were reviewed. Maricopa County was chosen because it accounted for ~65% of hospital deaths during 2008–2013 (unpublished data, HDD, 2015). Two independent reviewers (epidemiologists trained in death certification and coccidioidomycosis) initially determined if coccidioidomycosis contributed to the death. Coccidioidomycosis was considered to have contributed to the patient’s death if it was listed in the death summary as a diagnosis, active coccidioidomycosis disease was described in the physician’s notes and appeared to contribute to death, and/or active disease was suggested by laboratory diagnosis and plausibly contributed to death (e.g., patient had a positive enzyme immunoassay (EIA) immunoglobulin (Ig) M and immunodiffusion tube precipitin and died of sepsis). A single positive EIA IgM in MEDSIS was considered insufficient for confirmation based on reports of false-positive results in the literature.23 Any discrepant results were reviewed by an infectious disease specialist trained in death certification for final determination. After excluding HDD deaths for which coccidioidomycosis could not be confirmed as a cause of death, we recalculated a capture-recapture estimate and compared this with the number of coccidioidomycosis-attributable deaths in EDRS and the HDD for deaths that occurred in Maricopa County residents during 2012.
Nonresearch determination was obtained since this was a public health response. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Results
Capture-Recapture
During 2008–2013, a total of 529 coccidioidomycosis-attributable deaths were recorded in EDRS. Among these, 164 (31%) had coccidioidomycosis coded as the underlying cause of death; 333 (63%) had a coccidioidomycosis ICD-10 code, but coccidioidomycosis was not listed as the underlying cause of death; and 32 (6%) had cocci or Valley fever in the text cause-of-death field but without a coccidioidomycosis ICD-10 code.
During 2008–2013, HDD included 651 patient deaths with a discharge diagnosis coccidioidomycosis ICD-9 code. Of these, 251 (39%) were also in EDRS. Of the 400 HDD deaths not in EDRS, 399 (100%) had an associated death certificate (to confirm death) that did not list coccidioidomycosis as a cause of death, and one had no death certificate. Laboratory confirmation of coccidioidomycosis in MEDSIS was identified for 309 (77%) of these 399 unique HDD deaths.
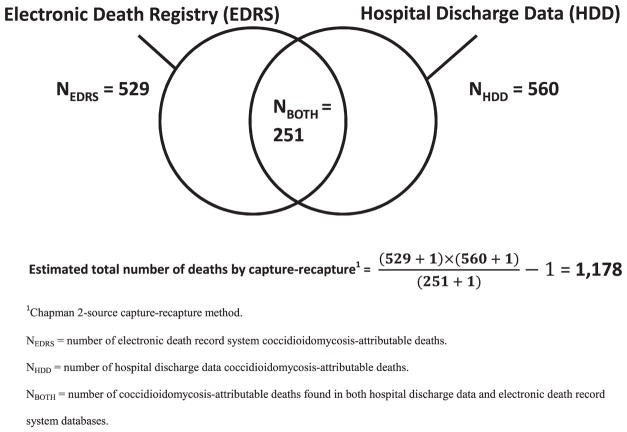
We identified 278 deaths in EDRS that were not in the HDD, and 309 deaths in the HDD that were not in EDRS. By using capture-recapture, we estimated 1,178 (95% CI: 1100–1256) total coccidioidomycosis-attributable deaths during 2008–2013 in Arizona (Fig. 1).
Figure 1.
Capture-recapture of Coccidioidomycosis Mortality — Arizona, 2008–2013.
The sensitivities of EDRS coccidioidomycosis-attributable death estimates varied by inclusion criteria. Compared with the capture-recapture estimate, the EDRS estimate using all causes of death and including text had a sensitivity of 45% (95% CI: 42%–48%) or a 2.2-fold underestimation (95% CI: 2.1–2.4). When the EDRS estimate using only the ICD-10 codes without including text was compared with the capture-recapture estimate, EDRS had a sensitivity of 42% (95% CI: 40%–45%) or a 2.4-fold underestimation (95% CI 2.2–2.5). Lastly, the EDRS estimate including only the single underlying cause of death ICD-10 code had a sensitivity of 14% (95% CI: 13%–15%) or a 7.2-fold underestimation (95% CI: 6.7–7.7), compared with the capture-recapture estimate (Table 1).
Table 1.
Number of coccidioidomycosis-attributable deaths and sensitivity of these methods compared with capture-recapture estimation by measurement method and by site and year.
| Measurement method | Arizona 2008–2013
|
Maricopa County 2012 with medical record validation1
|
||
|---|---|---|---|---|
| Number No. (95% CI) | Sensitivity compared with capture-recapture estimation % (95% CI) | Number No. (95% CI) | Sensitivity compared with capture-recapture estimation % (95% CI) | |
| Death Certificates | ||||
| Underlying cause of death alone | 164 | 14 (13–15) | 15 | 13 (11–15) |
| All cause of death ICD-10 codes | 497 | 42 (40–45) | 60 | 51 (42–62) |
| All cause of death ICD-10 codes and text fields2 | 529 | 45 (42–48) | 66 | 56 (48–68) |
| Hospital discharge data3 | ||||
| Primary diagnosis code only | 101 | 9 (8–9) | Not examined | - |
| All discharge codes | 560 | 47 (45–51) | 54 | 46 (39–56) |
| Capture-recapture estimate of total by using both death certificate and hospital discharge data4 | 1178 (1100–1256) | ref | 118 (98–138) | ref |
CI, confidence interval; ICD-10, International Classification of Diseases, Tenth Revision.
Medical records were reviewed for deaths recorded by hospital discharge data and coccidioidomycosis was not listed as a cause of death on the death certificate; deaths for which coccidioidomycosis could not be confirmed as a cause of death were excluded.
Any cause of death text field including “cocci” or “valley fever” followed by review to ensure accuracy.
Hospital discharge data was defined as a patient who died at the hospital; had an ICD-9 discharge diagnosis code for coccidioidomycosis (114.0–114.9); had a death certificate that did not record coccidioidomycosis as a cause of death; and had laboratory confirmation of coccidioidomycosis in MEDSIS.
Estimated by the formula n = [(NEDRS+1)(NHDD+1)/(NBOTH+1)] − 1, where NEDRS = the number of deaths only found in the EDRS, NHDD = the number of deaths only found in the hospital discharge data, and NBOTH = the number of deaths found in both databases.
Case-Control
Patients identified in HDD with a death certificate that lists coccidioidomycosis as a cause of death were more likely to have a positive HIV test result (aOR: 2.4; 95% CI: 1.1–2.4) or have coccidioidomycosis meningitis or disseminated coccidioidomycosis (versus pulmonary coccidioidomycosis) (aOR: 1.7; 95% CI: 1.1–1.7), compared with patients in HDD with a death certificate that did not list coccidioidomycosis as a cause of death. Sex, race/ethnicity, diabetes, malignancy, immunocompromised status, and chronic obstructive pulmonary disease were not significantly associated with coccidioidomycosis being listed as a cause of death on the death certificate. Although not significant, decedents of younger age were more likely to have coccidioidomycosis listed as a cause of death on their death certificate (Table 2).
Table 2.
Factors associated with having coccidioidomycosis included as cause of death on death certificate among patients who died in hospital with discharge diagnosis of coccidioidomycosis—Arizona, 2008–2013.
| Factor | Coccidioidomycosis listed as cause of death | |||
|---|---|---|---|---|
| Yes (n = 251) | No (n = 309) | Unadjusted OR | Adjusted OR1 | |
| No. (%) | No. (%) | OR (95% CI) | OR (95% CI) | |
| Race/ethnicity | ||||
| Native American | 12 (5) | 23 (7) | 0.7 (0.3–1.4) | 0.6 (0.3–1.3) |
| Black | 20 (8) | 25 (8) | 1.0 (0.5–1.9) | 0.7 (0.4–1.4) |
| Hispanic | 51 (20) | 41 (13) | 1.6 (1.0–2.5) | 1.3 (0.8–2.1) |
| White | 160 (64) | 204 (66) | ref | ref |
| Other | 8 (3) | 16 (5) | 0.6 (0.3–1.5) | 0.7 (0.3–1.6) |
| Age (years) | ||||
| <25 | 14 (6) | 6 (2) | 2.7 (1.0–7.3) | 2.5 (0.9–6.9) |
| 25–64 | 123 (49) | 143 (47) | ref | ref |
| 65–84 | 102 (41) | 135 (44) | 0.9 (0.6–1.2) | 1.1 (0.8–1.7) |
| >85 | 12 (5) | 25 (8) | 0.6 (0.3–1.2) | 0.6 (0.3–1.4) |
| Female | 92 (37) | 114 (37) | 1.0 (0.7–1.4) | 1.3 (0.9–1.9) |
| HIV-positive2 | 31 (12) | 14 (5) | 3.0 (1.5–5.7) | 2.4 (1.1–5.0)4 |
| Immunocompromised2,3 | 130 (52) | 149 (48) | 1.2 (0.8–1.6) | . . . |
| Malignancy2,3 | 42 (17) | 74 (24) | 0.6 (0.4–1.0) | . . . |
| COPD2 | 55 (22) | 88 (28) | 0.7 (0.5–1.0) | . . . |
| Diabetes2 | 70 (28) | 95 (31) | 0.9 (0.6–1.3) | . . . |
| Types of coccidioidomycosis | ||||
| Pulmonary | 171 (68) | 221 (72) | ref | ref |
| Disseminated or meningitis | 68 (27) | 41 (13) | 2.1 (1.4–3.3) | 1.7 (1.1–2.8) |
| Chronic | 6 (2) | 14 (5) | 0.6 (0.2–1.5) | 0.5 (0.2–1.4) |
| Unspecified; | 6 (2) | 33 (11) | 0.2 (0.1–0.6) | 0.2 (0.1–0.5) |
Bold font style indicates significance with P < .05. aOR, adjusted odds ratio; 95% CI, 95% confidence interval; COPD, chronic obstructive pulmonary syndrome; HIV, human immunodeficiency virus; OR, odds ratio.
Adjusted for race/ethnicity, age, sex, HIV status, and type of coccidioidomycosis.
Presence of qualifying discharge diagnosis International Classification of Diseases, 9th Revision (ICD-9) code compared to no presence of qualifying ICD-9 code.
Classified according to the Agency for Healthcare Research and Quality definitions (20).
Adjusted for race/ethnicity, age, sex, and type of coccidioidomycosis but not for HIV.
Medical record review and validation
We identified 33 potential coccidioidomycosis-attributable deaths in Maricopa County residents during 2012 from HDD by reviewing death certificates that did not list coccidioidomycosis as a cause of death. After medical records review, 24 (73%) were confirmed as coccidioidomycosis-attributable deaths; of these 24 deaths, 11 (46%) had coccidioidomycosis listed as a diagnosis on the death summary; 12 (50%) had physician notes or laboratory results confirming active coccidioidomycosis disease; and one (4%) had multiple positive laboratory tests for coccidioidomycosis in MEDSIS within 6 months of the patient’s death. On the 24 death certificates confirmed to be coccidioidomycosis-attributable deaths, 96 different causes of death were listed; the most common causes of death and associated ICD-10 codes were respiratory failure, un-specified (J96.9) (6 %), cardiac arrest, cause unspecified (I46.9) (5%), and atherosclerotic heart disease of native coronary artery (I25.1) (5%). Nine (27%) of the 33 deaths could not be confirmed as coccidioidomycosis-attributable deaths relying on available medical records; when reviewing MEDSIS records within six months of the patient’s death, seven had only one positive EIA IgM, and two had no laboratory confirmation.
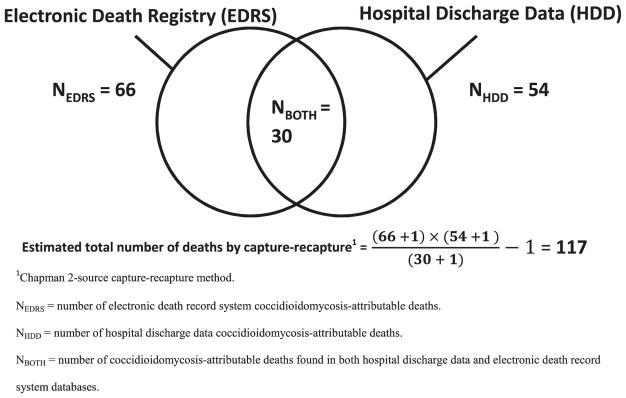
After restricting the analysis to coccidioidomycosis-attributable deaths in Maricopa County residents in 2012 reported in EDRS or verified by review of the medical records, we found 30 deaths in both databases, 36 in EDRS alone, and 24 in the HDD alone (Fig. 2). By using capture-recapture, we estimated a total of 117 (95% CI: 97–137) coccidioidomycosis-attributable deaths. Compared with the capture-recapture estimation, EDRS using all causes of death including text had a sensitivity of 56% (66/117; 95% CI: 48–68%) or a 1.8-fold underestimation (95% CI: 1.5–2.1). EDRS including only the ICD-10 codes without using text had a sensitivity of 51% (60/117; 95% CI: 44–62%) or a 2.0-fold underestimation (95% CI: 1.5–2.1). Finally, EDRS using only the single underlying cause of death ICD-10 code had a sensitivity of 13% (15/117; 95% CI: 11–15%) or a 7.8-fold underestimation (95% CI: 6.5–9.1) (Table 1).
Figure 2.
Capture-Recapture of Coccidioidomycosis Mortality — Maricopa County, Arizona, 2012.
Discussion
By using the capture-recapture methodology, we estimated that 1,178 total coccidioidomycosis-attributable deaths occurred during 2008–2013 in Arizona. Methods of measuring the coccidioidomycosis mortality rate by using death certificate data underestimate the mortality burden from two- to sevenfold. For example, ADHS uses the underlying or secondary cause of death ICD-10 codes from death certificates in their Valley Fever Annual Report,24 resulting in an approximate twofold underestimate of the mortality burden. A national coccidioidomycosis mortality study also used this method.7 The method used by the ADHS Bureau of Public Health Statistics,25 which reports the coccidioidomycosis mortality rate only based on underlying cause of death ICD-10 code, underestimates the total burden approximately sevenfold.
Because HDD is an administrative database and the accuracy depends on the skill of coders, we took multiple steps to ensure that coccidioidomycosis actually contributed to the death of patients identified in this database. Even when restricting our analysis to deaths included in HDD with either a death certificate listing coccidioidomycosis as a cause of death or an available medical record that confirmed coccidioidomycosis as contributing to death, death certificates underestimated mortality at approximately the same amount (1.8-fold with medical record validation versus 2.2-fold without medical record validation). This study reveals that when performing capture-recapture to estimate total coccidioidomycosis mortality by using EDRS and HDD, medical record validation (the most resource-intensive step of this study) might be unnecessary to calculate an accurate estimate.
Death certificate data assist in monitoring health trends, determining public health goals, and prioritizing which medical conditions receive research funding.26 However, cause of death information is frequently inaccurate or incomplete.8–11 Although this is the first study to document this problem for coccidioidomycosis, multiple studies have reported similar results when evaluating cause of death accuracy concerning death certificate data for other diseases, including cancer,27,28 heart disease,29 and drug overdose.30 Concerns have been raised that methodologies of tabulating death certificate data underestimate the mortality burden of infectious diseases.31 Multiple studies have reported heart disease to be overreported as a cause of death.32–35 The inaccuracies of death certificate data might be attributable to a lack of formal training in death certification of healthcare providers.11,35,36 Additional training of medical residents has been demonstrated to be effective in improving the accuracy of death certification.11,35,37
In this study, patients diagnosed with HIV or disseminated coccidioidomycosis were more likely to have coccidioidomycosis included as a cause of death on the death certificate. HIV is a well-established risk factor for disseminated coccidioidomycosis38 and is known to increase the risk of dying because of the disease.2 Disseminated disease is also recognized as an AIDS-defining condition. Death certifiers are likely more aware of the risk for disease among persons who are HIV-positive in endemic regions and might be more likely to include coccidioidomycosis as a cause of death on the death certificate of a person infected with HIV.
Multiple limitations are notable, including the following three assumptions made when conducting capture-recapture analyses. First, sources should be independent of each other and dependence of sources leads to underestimation.13 EDRS and HDD likely have a level of dependence because patients who die in the hospital are likely to have a death certificate; therefore, our capture-recapture estimate is likely an underestimate. Second, deaths should have equal probability of being ascertained by each source and differences in ascertainment probabilities can lead to overestimation.13 The probability of ascertainment among sources in this study might differ because every death should have a death certificate, whereas only persons who died in a hospital licensed by ADHS are included in HDD; this could inflate our capture-recapture calculation. Third, the population should be closed to the outside; migration of persons in or out of population can lead to an overestimate.13 An estimated 5% of Arizona’s population resides in the state only during the winter months,39 but winter residents would not affect our study because we only included residents of Arizona; Arizona residents who died in out-of-state hospitals would not have been included in the HDD but should have been included in EDRS. This might also have inflated our capture-recapture calculation. We did not adjust our calculations for these limitations, which is consistent with other published public health capture-recapture analyses.15,16 Fourth, medical record validation was performed on a subset of deaths and the results might not represent the general study population. Lastly, the possibility exists that coccidioidomycosis did actually contribute to the cause of death for a portion of the 27% of patients whose medical records lacked confirmation of coccidioidomycosis as a contributing cause of death, but the information was not included among available medical records. This can also lead to an underestimate of missed deaths.
In summary, estimates of coccidioidomycosis-attributable deaths that are based solely on death certificate data likely underestimate the true burden by at least twofold. Because unreliable death certificate data limit accurate mortality estimates for diseases of public health importance, medical education policy makers should consider incorporating death certification training into medical school and residency curricula and medical board certification requirements. ADHS offers online continuing medical education regarding death certification to all providers; however, this training is not mandatory. Public health agencies in coccidioidomycosis endemic areas should consider using HDD in addition to death certificate data to more accurately estimate coccidioidomycosis mortality. More accurate coccidioidomycosis mortality estimates might assist policy makers with prioritizing resources to support research regarding treatment and prevention of coccidioidomycosis to lessen the public health effects of the disease.
Acknowledgments
This work was supported by the Centers for Disease Control and Prevention.
Footnotes
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and the writing of the paper.
References
- 1.Twarog M, Thompson GR., 3rd Coccidioidomycosis: recent updates. Semin Respir Crit Care Med. 2015;36:746–755. doi: 10.1055/s-0035-1562900. [DOI] [PubMed] [Google Scholar]
- 2.Galgiani JN, Ampel NM, Blair JE, et al. Coccidioidomycosis. Clin Infect Dis. 2005;41:1217–1223. doi: 10.1086/496991. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. [Accessed May 27, 2016];Valley fever (coccidioidomycosis) statistics. 2015 http://www.cdc.gov/fungal/diseases/coccidioidomycosis/statistics.html.
- 4.Tsang CA, Anderson SM, Imholte SB, et al. Enhanced surveillance of coccidioidomycosis, Arizona, USA, 2007–2008. Emerg Infect Dis. 2010;16:1738–1744. doi: 10.3201/eid1611.100475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arizona Department of Health, Office of Infectious Disease Services. [Accessed May 27, 2016];Valley fever 2013 annual report. 2014 http://www.azdhs.gov/documents/preparedness/epidemiology-disease-control/valley-fever/reports/valley-fever-2013.pdf.
- 6.Arizona Department of Health, Population Health and Vital Statistics. [Accessed May 27, 2016];Arizona Health Status and Vital Statistics 2013 Annual Report. 2014 http://www.azdhs.gov/plan/report/ahs/ahs2013/index.php.
- 7.Huang JY, Bristow B, Shafir S, et al. Coccidioidomycosis-associated deaths, United States, 1990–2008. Emerg Infect Dis. 2012;18:1723–1728. doi: 10.3201/eid1811.120752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoff CJ, Ratard R. Louisiana death certificate accuracy: a concern for the public’s health. J La State Med Soc. 2010;162:350, 352–353. [PubMed] [Google Scholar]
- 9.Johansson LA, Westerling R. Comparing Swedish hospital discharge records with death certificates: implications for mortality statistics. Int J Epidemiol. 2000;29:495–502. [PubMed] [Google Scholar]
- 10.Johns LE, Madsen AM, Maduro G, et al. A case study of the impact of inaccurate cause-of-death reporting on health disparity tracking: New YorkCity premature cardiovascular mortality. Am J Public Health. 2013;103:733–739. doi: 10.2105/AJPH.2012.300683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ong P, Gambatese M, Begier E, et al. Effect of cause-of-death training on agreement between hospital discharge diagnoses and cause of death reported, inpatient hospital deaths, New York City, 2008–2010. Prev Chronic Dis. 2015;12:E04. doi: 10.5888/pcd12.140299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. [Accessed May 27, 2016];About the mortality medical data system. 2015 http://www.cdc.gov/nchs/nvss/mmds/about_mmds.htm%5C.
- 13.Hook EB, Regal RR. Capture-recapture methods in epidemiology: methods and limitations. Epidemiol Rev. 1995;17:243–264. doi: 10.1093/oxfordjournals.epirev.a036192. [DOI] [PubMed] [Google Scholar]
- 14.Boden LI, Ozonoff A. Capture-recapture estimates of nonfatal workplace injuries and illnesses. Ann Epidemiol. 2008;18:500–506. doi: 10.1016/j.annepidem.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Giambrone GP, Zansky SM, Eidson M, et al. Guillain-Barré syndrome surveillance during National Influenza Vaccination Campaign, New York, U.S.A., 2009. Emerg Infect Dis. 2013;19:1956–1962. doi: 10.3201/eid1912.130643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gignoux E, Idowu R, Bawo L, et al. Use of capture-recapture to estimate underreporting of Ebola virus disease, Montserrado County, Liberia. Emerg Infect Dis. 2015;21:2265–2267. doi: 10.3201/eid2112.150756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.La Ruche G, Dejour-Salamanca D, Bernillon P, et al. Capture-recapture method for estimating annual incidence of imported dengue, France, 2007–2010. Emerg Infect Dis. 2013;19:1740–1748. doi: 10.3201/eid1911.120624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. [Accessed May 27, 2016];National program of cancer registries (NPCR) 2016 http://www.cdc.gov/cancer/npcr/
- 19.Chapman DG. Some Properties of the Hypergeometric Distribution with Applications to Zoological Sample Censuses. Berkeley, CA: University of California Press; 1951. [Google Scholar]
- 20.Wittes J, Sidel VW. A generalization of the simple capture-recapture model with applications to epidemiological research. J Chronic Dis. 1968;21:287–301. doi: 10.1016/0021-9681(68)90038-6. [DOI] [PubMed] [Google Scholar]
- 21.Kiakalayeh AD, Mohammadi R, Stark Ekman D, et al. Estimating drowning deaths in Northern Iran using capture-recapture method. Health Policy. 2011;100:290–296. doi: 10.1016/j.healthpol.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality. [Accessed May 27, 2016];Patient safety indicators technical specifications. 2015 http://www.qualityindicators.ahrq.gov/Modules/PSI_TechSpec.aspx.
- 23.Malo J, Luraschi-Monjagatta C, Wolk DM, et al. Update on the diagnosis of pulmonary coccidioidomycosis. Ann Am Thorac Soc. 2014;11:243–253. doi: 10.1513/AnnalsATS.201308-286FR. [DOI] [PubMed] [Google Scholar]
- 24.Arizona Department of Health Services, Office of Infectious Disease Services. [Accessed May 27, 2016];Valley fever 2014 annual report. 2015 http://www.azdhs.gov/documents/preparedness/epidemiology-disease-control/valley-fever/reports/valley-fever-2014.pdf.
- 25.Arizona Department of Health Services. Population Health and Vital Statistics. [Accessed May 27, 2016];Arizona health Status and vital statistics annual reports. 2015 http://www.azdhs.gov/plan/report/ahs/
- 26.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed May 27, 2016];Instructions for completing cause-of-death section of death certificate. 2004 http://www.cdc.gov/nchs/data/dvs/blueform.pdf.
- 27.Hinchliffe SR, Abrams KR, Lambert PC. The impact of under and over-recording of cancer on death certificates in a competing risks analysis: a simulation study. Cancer Epidemiol. 2013;37:11–19. doi: 10.1016/j.canep.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 28.Chow WH, Devesa SS. Underreporting and misclassification of urinary tract cancer cases on death certificates. Epidemiology. 1996;7:517–520. [PubMed] [Google Scholar]
- 29.Lloyd-Jones DM, Martin DO, Larson MG, et al. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–1026. doi: 10.7326/0003-4819-129-12-199812150-00005. [DOI] [PubMed] [Google Scholar]
- 30.Mertz KJ, Janssen JK, Williams KE. Underrepresentation of heroin involvement in unintentional drug overdose deaths in Allegheny County, PA. J Forensic Sci. 2014;59:1583–1585. doi: 10.1111/1556-4029.12541. [DOI] [PubMed] [Google Scholar]
- 31.Govindan S, Shapiro L, Langa KM, et al. Death certificates underestimate infections as proximal causes of death in the U.S. PLoS One. 2014;9:e97714. doi: 10.1371/journal.pone.0097714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lakkireddy DR, Gowda MS, Murray CW, et al. Death certificate completion: how well are physicians trained and are cardiovascular causes overstated? Am J Med. 2004;117:492–498. doi: 10.1016/j.amjmed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 33.Agarwal R, Norton JM, Konty K, et al. Overreporting of deaths from coronary heart disease in New York City hospitals, 2003. Prev Chronic Dis. 2010;7:A47. [PMC free article] [PubMed] [Google Scholar]
- 34.Coady SA, Sorlie PD, Cooper LS, et al. Validation of death certificate diagnosis for coronary heart disease: the atherosclerosis risk in communities (ARIC) study. J Clin Epidemiol. 2001;54:40–50. doi: 10.1016/s0895-4356(00)00272-9. [DOI] [PubMed] [Google Scholar]
- 35.Lakkireddy DR, Basarakodu KR, Vacek JL, et al. Improving death certificate completion: a trial of two training interventions. J Gen Intern Med. 2007;22:544–548. doi: 10.1007/s11606-006-0071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wexelman BA, Eden E, Rose KM. Survey of New York City resident physicians on cause-of-death reporting, 2010. Prev Chronic Dis. 2013;10:E76. doi: 10.5888/pcd10.120288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Myers KA, Farquhar DR. Improving the accuracy of death certification. CMAJ. 1998;158:1317–1323. [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Revised surveillance case definition for HIV infection—United States, 2014. MMWR Recomm Rep. 2014;63(RR-03):1–10. [PubMed] [Google Scholar]
- 39.Happel SK, Hogan TD. Counting snowbirds: the importance of and the problems with estimating seasonal populations. Population Research and Policy Review. 2002;21:227–240. [Google Scholar]