Abstract
We present the case of a 71 y/o man with chronic obstructive pulmonary disease (COPD) who presented with 3 weeks of cough, phlegm, fever, and failed outpatient antibiotic therapy for pneumonia. CT of the chest showed unilateral interstitial changes and bronchoscopic biopsies demonstrated primary lung papillary adenocarcinoma and extensive concentric psammomatous calcifications.
1. Case report
Lung cancer is associated with significant morbidity and mortality. Outcomes are usually dependent on tumour characteristics. Papillary adenocarcinoma is a rare subtype of lung adenocarcinoma with a distinct histopathological profile.
A 71-year-old male with 60 pack-years smoking history, active smoker, with moderate COPD (FEV 1, 60% predicted) presented with 3 weeks of cough, fevers, malaise and muco purulent phlegm. He had failed outpatient azithromycin, inhalers and prednisone with progressive symptoms and failure to thrive. Chest X Ray showed diffuse interstitial and airspace opacities throughout the right lung, a small right pleural effusion and a clear left lung (Fig. 1). A CT of the chest showed diffuse right sided interstitial reticulonodular changes which appear calcified, patchy consolidation with thickening of the peribronchovascular interstitium, no clear mass like density in the lungs and no thoracic lymphadenopathy. Differential included atypical infection versus lymphangitic carcinomatosis (Fig. 2).
Fig. 1.

CXR showing Right lung diffuse interstitial opacities.
Fig. 2.
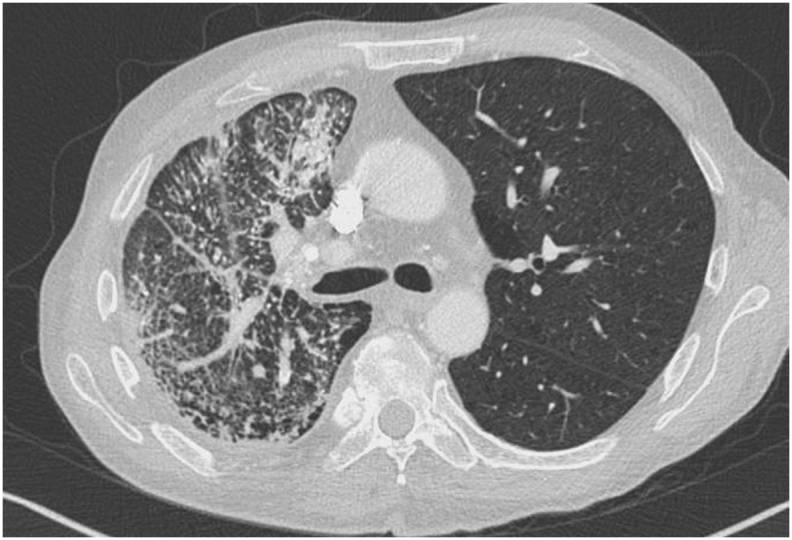
CT chest showing diffuse right sided interstitial reticulonodular changes.
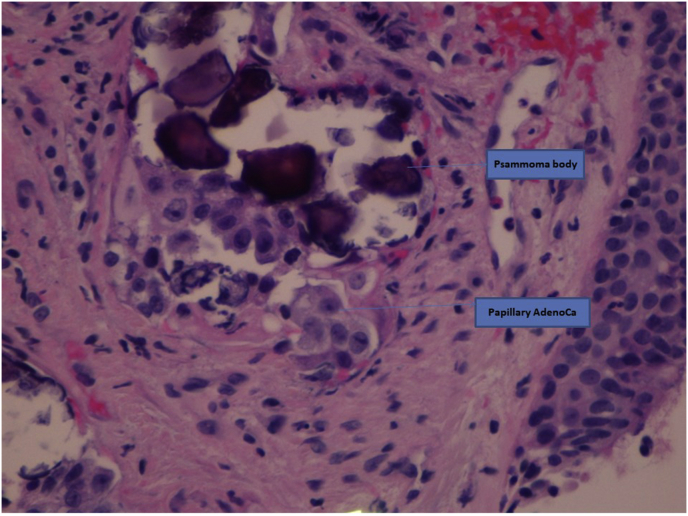
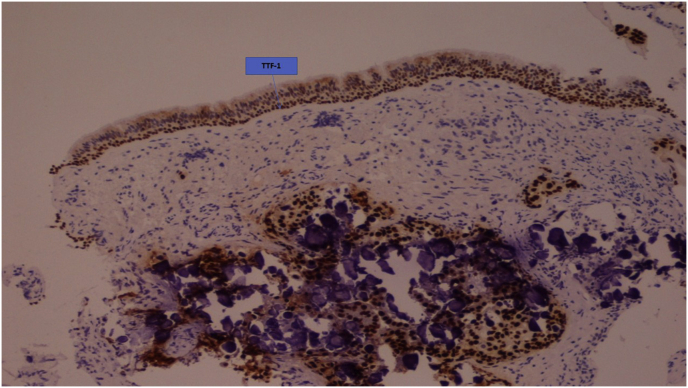
Bronchoscopy showed right lung airway erythema and minor mucosal irregularities in the right middle lobe and the right lower lobe but no endobronchial mass. Endobronchial biopsies showed poorly differentiated adenocarcinoma with papillary architecture (Fig. 3) and extensive concentric psammomatous calcifications but no lymphangitic spread on transbronchial specimens. Of note, clinical exam for lymph nodes and thyroid gland was non contributary. Immunohistochemistry was positive for cytokeratin, TTF-1, CK7 and focally for CK20(Fig. 4). It was negative for p63, calretinin and WT1 supporting a primary lung adenocarcinoma. Thyroglobulin was negative. Molecular studies were negative for KRAS, EGFR but had KRAS c.35G>A (G12D). Metastatic workup was negative and he was started on systemic chemotherapy.
Fig. 3.
High resolution papillary lung adenocarcinoma with psammomatous calcifications.
Fig. 4.
Immunohistochemistry positive for TTF-1.
The patient completed six cycles of carboplatin, pemetrexed and cetuximab. He is currently on maintenance pemetrexed and cetuximab.
He developed odynophagia and dysphagia after his first cycle of maintenance chemotherapy.
The patient had minor improvement in his radiological findings and has clinical stability at 4 months post diagnosis. No further hospitalizations were reported.
2. Discussion
Lung cancer is the leading cause of cancer mortality worldwide. Primary lung carcinoma and metastasis are often diagnosed late and vary widely in symptoms, pathology, immunohistochemistry, and prognosis [1]. Primary papillary adenocarcinoma (PA) is a rare subtype of lung adenocarcinoma [2]. The World Health Organization classification defines PA as adenocarcinoma with predominance of papillary structures that replace the underlying alveolar architecture [3]. Overall, less than 10% of lung adenocarcinoma will fit this description. PA is often seen in non-smokers and is associated with aggressive intrapulmonary metastasis/lymph node involvement [4] and overall worse prognosis. Radiologically it most commonly presents as ill-defined lung nodules and can be initially confused with atypical infections [5,6]. PA has a distinct immunohistochemistry profile that has prognostic implications [7].
Presence of psammoma bodies is rare in lung adenocarcinoma (5–7% of all lung adenocarcinomas) and it may predict a good response to tyrosine kinase inhibitors [8]. Our patient with unilateral lung disease with papillary lung adenocarcinoma with extensive psammoma bodies makes this an even more usual presentation.
3. Conclusions
Persistent pulmonary symptoms often warrant invasive testing especially in the right clinical context. Papillary lung adenocarcinoma is an uncommon subtype of adenocarcinoma with poorer prognosis. Psammoma bodies, although rarely see, can predict response to certain chemotherapy.
Conflict of interest
*The author(s) declare(s) that there is no conflict of interest regarding the publication of this paper. All the authors have approved the manuscript. Dr Gupta is the corresponding author.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.rmcr.2018.07.004.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Palkar A.V., Gupta A., Greenstein Y., Gottesman E. Primary cardiac angiosarcoma: a rare cause of diffuse alveolar haemorrhage. BMJ Case Rep. 2018 Jun 4;2018 doi: 10.1136/bcr-2018-225365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karmakar S., Nath A., Neyaz Z. Primary papillary adenocarcinoma of the lung: report of two cases. Lung India. 2017 May-Jun;34(3):299–302. doi: 10.4103/lungindia.lungindia_467_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miyoshi T., Satoh Y., Okumura S. Early-stage lung adenocarcinomas with a micropapillary pattern, a distinct pathologic marker for a significantly poor prognosis. Am. J. Surg. Pathol. 2003;27:101–109. doi: 10.1097/00000478-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Kerr K.M. Pulmonary adenocarcinomas: classification and reporting. Histopathology. 2009;54:12–27. doi: 10.1111/j.1365-2559.2008.03176.x. [DOI] [PubMed] [Google Scholar]
- 5.Noguchi M., Morikawa A., Kawasaki M. Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer. 1995;75:2844–2852. doi: 10.1002/1097-0142(19950615)75:12<2844::aid-cncr2820751209>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 6.Gupta A., Gulati S. Mesalamine induced eosinophilic pneumonia. Respir. Med. Case Rep. 2017 Apr 12;21:116–117. doi: 10.1016/j.rmcr.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chao L., Yi-Sheng H., Yu C. Relevance of EGFR mutation with micropapillary pattern according to the novel IASLC/ATS/ERS lung adenocarcinoma classification and correlation with prognosis in Chinese patients. Lung Canc. 2014 Nov;86(2):164–169. doi: 10.1016/j.lungcan.2014.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Miyake A., Okudela K., Matsumura M. Update on the potential significance of psammoma bodies in lung adenocarcinoma from a modern perspective. Histopathology. 2018 Mar;72(4):609–618. doi: 10.1111/his.13397. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.