Abstract
Purpose:
The aim of the study was to report the occurrence of contamination/replacement of ophthalmic eye drops with liquids of acidic nature in patients treated for nonresponding scleritis.
Methods:
This was a retrospective interventional case series study.
Results:
Of the three patients (4 eyes) referred as necrotizing scleritis, two were found to have acid as the content in the bottle/s being used as eye drops, confirmed using biochemical tests. All four eyes had tarsal ischemia and tarsal conjunctival defect in addition to severe scleral ischemia involving the inferior bulbar area. All four eyes required tenonplasty with amniotic membrane transplant more than once for the ocular surface to heal. Two of the three patients were on systemic immunosuppressives including pulse cyclophosphamide for refractory necrotizing scleritis. Sulfuric and hydrochloric acid was isolated from the bottles of 2nd and 3rd patient using confirmatory biochemical tests.
Conclusion:
It is important to be aware of the possibility of contaminating or replacing contents of eye drops with harmful agents of acidic nature and should be considered in situations that resemble the clinical picture described herein.
Keywords: Acid, chemical injury, ocular chemical injury, tenonplasty
Chemical injuries of the eye are known to occur secondary to accidents, domestic or industrial, and vitriolage. Such injuries are in almost all cases accompanied by a history of the incident, and in most cases, the nature of the inciting agent, acid or alkali. Immediate primary care is usually provided at the site of the event before the patient seeks ophthalmic evaluation. The history being straightforward and chemical injuries being considered a condition of acute emergency in ophthalmic care, management is initiated at the earliest, realizing the perils of delay in doing so. A differential diagnosis is usually not sought for. Scleral ischemia is one of the features of severe chemical injuries requiring tenonplasty to address the same.[1,2]
In an acute setting, scleral ischemia can occur in chemical or thermal burns. Scleral ischemia can also occur when excessive beta irradiation or mitomycin C is used to treat pterygia or can develop secondary to systemic vasculitis and connective tissue disorders. Necrotizing scleritis is usually associated with collagen vascular disorders. The sclera can be affected and scleral ischemia with melt can be the presenting feature of the disease.[2] The palpebral conjunctiva and tarsal plate remain uninvolved except for a mild inflammatory reactive change except in chemical injuries.
This article brings forth three unusual cases with clinical features typical of chemical injury with severe scleral ischemia without a history suggestive of the same, steering the diagnosis toward necrotizing scleritis by ophthalmologists primarily treating the patients. Specific signs that did not agree with a diagnosis of scleritis along with a very high index of suspicion helped clinch the diagnosis of eye drops being contaminated with liquid of acidic nature in two of the three cases.
With an aim to create an awareness regarding such a possibility, we describe herein, in detail, the presentation features as well as the points that led us to the diagnosis in these cases.
Methods
This is a retrospective interventional study that adhered to the tenets of the Declaration of Helsinki approved by the Institutional Review and Ethics Board.
The case records of three patients who presented with being on treatment for necrotizing scleritis and later were diagnosed to be secondary to chemical injury were reviewed retrospectively. These were patients who presented to our tertiary eye care institute in the period between February 2015 and January 2017.
A complete ophthalmologic evaluation was done for each of them, and all patients underwent subsequent tenonplasty to address the scleral ischemia. The procedure was performed as described earlier and was repeated if required following retraction.
Results
Case 1
A 50-year-old female presented with irritation and pain in the left eye 2 weeks following clear corneal phacoemulsification. She was on tapering doses of topical steroids and topical antibiotic following surgery. In view of her redness and discomfort, the topical antibiotic was continued. She was referred to our tertiary eye care center for a possible diagnosis of surgically induced necrotizing scleritis.
Ocular examination revealed an inferior corneal epithelial defect with adjacent scleral ischemia and conjunctival defect. In addition, there was the presence of tarsal ischemia and tarsal palpebral conjunctival defect [Fig. 1a]. There was the presence of anterior chamber reaction and an inflammatory membrane in the pupillary plane. Her best-corrected visual acuity (BCVA) in the left eye was noted to be counting fingers at 1 m. Her workup for underlying systemic collagen disorders was negative.
Figure 1.
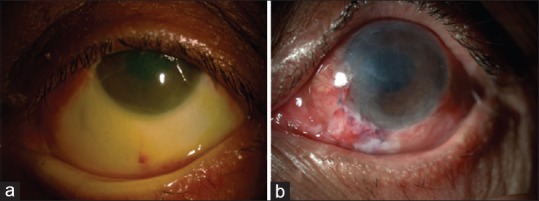
(a) Inferior large area of scleral ischemia with overlying conjunctival defect along with epithelial defect over the inferior one-third of the cornea. (b) Following tenonplasty for scleral ischemia
As the examination findings were typical of postchemical injury, a diagnosis of possible inadvertent chemical injury was made. The patient and attendants were repeatedly questioned regarding possibility of instilling some irritants to the eye secondary to mistaken identity of similar-looking bottles. This was denied and the patient consistently kept mentioning about a burning sensation on instillation of the antibiotic drop. She underwent tenonplasty with amniotic membrane transplantation twice [Fig. 1b]. Following minimal re-retraction of the Tenon's, scleral and corneal thinning was noted straddling the limbus for which cyanoacrylate glue was applied with a bandage contact lens (BCL). A month later the surface epithelized and the glue and BCL were removed. The inferior cornea showed signs of corneal decompensation. She required topical antiglaucoma medication to control the intraocular pressure. The inflammation in the eye subsided with no subsequent similar episodes over a 4-year period of follow-up, at which time a diffuse corneal haze with vascularization was noted with a healthy superior limbus.
Case 2
A 55-year-old female, on treatment for rheumatoid arthritis and hypothyroidism since 10 years, presented in February 2015 with scleral necrosis and pain 1 month after clear corneal cataract surgery done elsewhere. She was on systemic steroids and systemic methotrexate. The diagnosis of scleritis was concurred with at our institute and the patient continued to follow-up with her local ophthalmologist and rheumatologist. She underwent a clear corneal phacoemulsification in the right eye 3 months later, while on systemic immunosuppressives, following which she developed scleritis in the other eye with worsening of signs in the other eye. She was administered pulse methylprednisolone and cyclophosphamide twice by her treating ophthalmologist and referred to us for further management. She was on topical steroids, antibiotic, and lubricant in addition since the past 3 months.
Her BCVA was noted to be 6/36 in the right eye and counting fingers close to face in the left eye. Clinical features were similar to that noted in the previous patient with tarsal ischemia and ulceration and skin ulceration [Figs. 2a and b], all of which were not corroborating with the clinical diagnosis of scleritis. Her blood investigations revealed a normal erythrocyte sedimentation rate and C-reactive protein despite a worsening of the ocular condition. Clinical features were strongly suggestive of chemical injury and the patient as well as the attendants were questioned repeatedly about the instillation of anything other than the advised eye drops in the eye which was strongly refuted. The patient, however, complained of severe pain and discomfort during instillation of the antibiotic eye drop. Examination of the bottle with the antibiotic did not reveal anything amiss, though it appeared darker in color compared to the normal drop.
Figure 2.
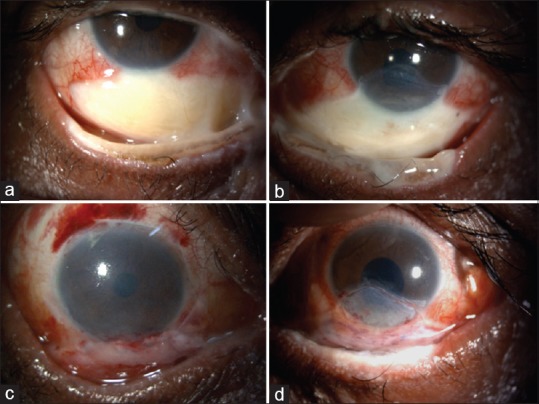
(a and b) Inferior large area of scleral ischemia with overlying conjunctival defect along with epithelial defect over the inferior one-third of the cornea in both eyes. The tarsal ischemia and lid margin damage are seen. (c and d) Following tenonplasty for scleral ischemiafor both eyes
When the content in the bottle was checked for pH using the pH strip, it turned acidic indicative of pH 1–2. The bottle was subsequently subjected to biochemical investigations that revealed the true nature of the liquid to be sulfuric acid [Fig. 3a].
Figure 3.

(a) Confirmatory test for sulfuric acid in patient 2. In the presence of barium chloride, sulfuric acid gives milky white precipitate. The test also has same white precipitate, which indicates the presence of sulfuric acid in the test sample. (b) Confirmatory test for hydrochloric acid in patient 3. In presence of silver nitrate (AgNO3), hydrochloric acid gives white precipitate. Curd-like white precipitate of 7 test samples on the left similar to the standard on the right indicates the presence of hydrochloric acid. The tests for the other acids were negative for either of the test samples
The patient was informed of the same; the attendants were confronted though they continued to remain in denial. The patient care was continued with tenonplasty and amniotic membrane grafting done twice for both the eyes [Fig. 2c and d]. Only eye ointments were used postoperatively, and when patient was seen at the next follow-up 3 months later, the surface had healed with a BCVA of 6/9 in the right and 3/60 in the left eye.
Case 3
A 71-year-old male presented with pain and decrease of vision for 2 months, with clinical features exactly similar to the previous 2 cases [Fig. 4a and c]. He had been diagnosed as necrotizing scleritis elsewhere and was given three doses of intravenous cyclophosphamide and methylprednisolone. He complained of severe pain during instillation of the eye drops and refused to instill any drops in the eye, for which he had been referred to the psychiatric department that had initiated him on several antipsychotic medications. When the patient was seen at our institute for the 1st time, he was wheeled in on a stretcher and was heavily sedated.
Figure 4.
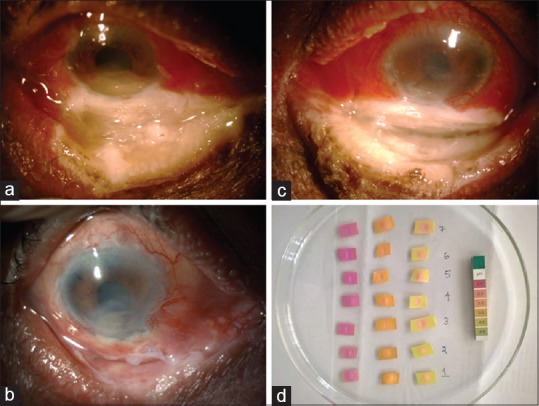
(a and c) Severe scleral and tarsal ischemia along with conjunctival congestion. The upper lid margin also shows excoriation changes due to contact with the acid following instillation. (b) Following healing of the ocular surface with inferior corneal and bulbar conjunctival scarring. (d) All seven eye drops showing a change in pH on the pH strip close to 2 on the pH indicator
He was on seven topical medications all of which appeared more yellow than normal [Fig. 5]. Without any delay, due to the very high index of suspicion this time, all the bottles were checked for pH using the pH strip that turned out to be <2 [Fig. 4d]. A fresh vial of each of the topical medications available at our pharmacy was obtained and checked for comparison that showed a near neutral pH. All seven bottles were subjected to biochemical investigations that revealed the nature of the liquid in all seven bottles to be hydrochloric acid (HCl) [Fig. 3b].
Figure 5.
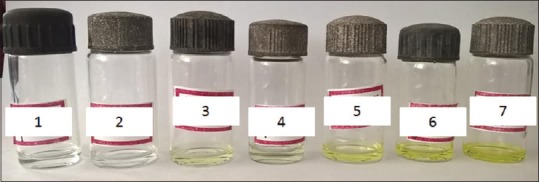
Contents of all seven eye drops were transferred to another sterile bottle. These topical medications included three different lubricating eye drops, a mydriatic, antibiotic, antiglaucoma, and steroid. Although the bottles 1 and 2 appear to have a colorless fluid and the others appear yellow, all the bottles tested positive for hydrochloric acid
The patient was accompanied by his family members who did not respond to any interrogation regarding the contents of the bottles. This time around, the nearest police station, was informed of the same who in turn referred it to the jurisdiction to which the patient belonged, which in this case was from a different state. The case was registered as medicolegal at our institute. The institutional authorities informed the DCGI. The medical care of the patient was continued. He required tenonplasty and amniotic membrane transplantation thrice in both the eyes [Fig. 4b]. All his systemic medications were stopped. Three months later, the patient walked in healthy into the clinic for a follow-up with a healed ocular surface, requiring cataract surgery later. His visual acuity in both eyes was counting fingers at 2 feet. He was accompanied by another attendant.
Discussion
To consider a diagnosis of chemical injury with no positive history requires a very high index of suspicion. A conclusive diagnosis could not be reached for the 1st case in our experience though a doubt of chemical injury kept lingering throughout the period of follow-ups, though biochemical confirmation of the acidic nature of the contents in the vial was possible for the other two cases.
Two of the three patients were on high-dose immunosuppression for a clinical diagnosis of necrotizing scleritis in these patients. Surgically induced necrotizing scleritis could have been one of the differential diagnoses. Both patients had undergone a clear corneal phacoemulsification and the location of the scleritis was inferior.[3] The important differentiating feature, however, was the presence of tarsal ischemia and tarsal conjunctival defect which would be absent in a case of scleritis. The inferior location, the relatively normal superior bulbar conjunctiva, and the patient giving a history of severe irritation on instillation of the drop/s are further indicators of the same. Telltale signs of ulceration or maceration of the skin of the lower lid and the lid margin are additional findings.
In the absence of a positive history, a nonresponding ischemic sclera in a symptomatic patient leads to a possible diagnosis of necrotizing scleritis. With no response to topical and systemic steroids, the next line of management for these eyes is to initiate systemic immunosuppression[4] and without any favorable results despite maximum immunosuppression for scleritis, it makes the condition very perplexing to the treating ophthalmologist.
The aim of this report is to create an awareness regarding the possibility of an intentional or accidental contamination of the ophthalmic vials. The identity of the medication vial/s has no bearing, since it was noted to have been possible with multiple preparations, though some by virtue of their packaging make it easier to contaminate.
Medications used in the eye in the form of ophthalmic drops have varying pH ranges, and it is important to be aware of the pH of commonly used medications. HCl or phosphoric acid is the commonly used acids in ophthalmic medications to adjust pH.
The normal physiological pH of the ocular surface in humans is noted to be 7.11 ± 1.5. An increase in ocular surface pH occurs early in the morning and a gradual increase in pH to more alkali levels during the day. In addition, 1 h of lid closure causes decrease in pH. Following instillation of one drop of tropicamide (pH 6.0) and one drop of phenylephrine (pH = 4.8), pH of the ocular surface shows a sudden decrease up to 4.6 and returns to the normal levels with flushing effect of normal tearing within 40 min. Among the other commonly used medications during ophthalmic evaluation, cyclopentolate hydrochloride eye drops 1.0% have a pH of 4.5 and tropicamide ophthalmic solution has a pH in the range of 4.0–5.8, often used for cycloplegia. Proparacaine hydrochloride ophthalmic solution (pH = 3.5–6.0) is often used as topical anesthetic drops. Moreover, formulations of antibiotic eye drops also contain HCl or phosphoric acid or sodium hydroxide to adjust pH. For example, ofloxacin ophthalmic solution is unbuffered and formulated with a pH of 6.4 (range: 6.0–6.8).[5,6] It, however, is unusual to have a pH of <3 or >9 in ophthalmic medications and a value beyond these on the pH strip is to be viewed with suspicion. Another simple method to compare the pH is to check the pH of the contents in the vial in question and compare it with the pH of a new vial of the same medication.
A simple litmus test paper in the clinic can help clinch a quick diagnosis in cases with a high index of suspicion. Biochemical confirmation of the nature of the acid by means of confirmatory tests was diagnostic of the content. Although HCl does form an ingredient to adjust pH in few ophthalmic medications, the pH cannot be in the range of 1–2 and the same acid was confirmed to be present in all bottles being instilled in the eyes of the 3rd patient. Although HCl has a pungent odor, it probably was not recognized by the patient as being abnormal or the very small quantity of the acid might not have been pungent enough to identify it. Sulfuric acid is not usually used to adjust pH in ophthalmic preparations.
Inadvertent instillation of contents from a similar-looking bottle which could contain an irritant should be borne in mind and asked for, though this would probably be a one-time event.
Based on available facts in our series, we suspect replacement of eye drop bottle contents with acid and its implications could be manifold. There were no existing guidelines regarding the steps to be taken, this being an unprecedented situation, and hence we followed the course that was most appropriate, as discussed above, labeling the case as medicolegal, and the ophthalmic care required was proceeded with as required.
The severity of scleral ischemia determines the course of treatment and all three patients (four eyes) required a tenonplasty along with amniotic membrane transplantation to heal the damaged surface. Placing amniotic membrane on a severely ischemic sclera without a tenonplasty does not lead to epithelization. The authors have reported earlier their outcome following tenonplasty in severe chemical injuries.[7] Discussing other therapeutic options for scleral ischemia would be beyond the scope of this article that primarily aims to highlight the pitfalls in the diagnosis of such occurrences.
Late occurring peripheral ulcerative sclerokeratitis can occur years after chemical injury[8] though the clinical picture would resemble that of necrotizing scleritis without tarsal involvement with a definite past history of chemical injury.
The ocular morbidity leading to a permanent impairment of varying severity, both anatomical and functional, and more importantly, the daily psychological and physical trauma caused by the entire process of being subjected to instillation of acid as drops into the eye and the associated delay in diagnosis and management pertaining to a different condition, are all beyond measure. The ease of availability of acids over the counter in many shops and its physical similarity to water or eye drops makes this an easy choice to use. It might not be a very common situation or there could have been instances when the diagnosis was missed. Under such circumstances, as ophthalmologists, it is our responsibility to be aware of such a possibility to prevent the delay in diagnosis.
Conclusion
Though very unusual and rare, it is important to be aware of and have a high index of suspicion for the possibility of an underlying chemical injury in eyes that present with features suggestive of necrotising scleritis, especially when associated with tarsal ischemia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kuckelkorn R, Redbrake C, Reim M. Tenonplasty: A new surgical approach for the treatment of severe eye burns. Ophthalmic Surg Lasers. 1997;28:105–10. [PubMed] [Google Scholar]
- 2.Casas VE, Kheirkhah A, Blanco G, Tseng SC. Surgical approach for scleral ischemia and melt. Cornea. 2008;27:196–201. doi: 10.1097/ICO.0b013e31815ba1ae. [DOI] [PubMed] [Google Scholar]
- 3.Watson PG. The diagnosis and management of scleritis. Ophthalmology. 1980;87:716–20. doi: 10.1016/s0161-6420(80)35177-4. [DOI] [PubMed] [Google Scholar]
- 4.O'Donoghue E, Lightman S, Tuft S, Watson P. Surgically induced necrotising sclerokeratitis (SINS) – Precipitating factors and response to treatment. Br J Ophthalmol. 1992;76:17–21. doi: 10.1136/bjo.76.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coles WH, Jaros PA. Dynamics of ocular surface pH. Br J Ophthalmol. 1984;68:549–52. doi: 10.1136/bjo.68.8.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim LT, Ah-Kee EY, Collins CE. Common eye drops and their implications for pH measurements in the management of chemical eye injuries. Int J Ophthalmol. 2014;7:1067–8. doi: 10.3980/j.issn.2222-3959.2014.06.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iyer G, Srinivasan B, Agarwal S, Barbhaya R. Visual rehabilitation with keratoprosthesis after tenonplasty as the primary globe-saving procedure for severe ocular chemical injuries. Graefes Arch Clin Exp Ophthalmol. 2012;250:1787–93. doi: 10.1007/s00417-012-2030-8. [DOI] [PubMed] [Google Scholar]
- 8.Iovieno A, Anand S, Dart JK. Late-onset peripheral ulcerative sclerokeratitis associated with alkali chemical burn. Am J Ophthalmol. 2014;158:1305–90000. doi: 10.1016/j.ajo.2014.08.038. [DOI] [PubMed] [Google Scholar]


